Abstract
Introduction
The aim of this work is to determine the interocular differences in peripapillary retinal nerve fiber layer (p-RNFL) thickness and its associations among school children in Hong Kong.
Methods
We conducted a population-based study including 4034 children aged 6–8 years from the Hong Kong Children Eye Study (HKCES). All participants received comprehensive ocular examinations where p-RNFL thickness was measured using spectral-domain optical coherence tomography (SD-OCT). The degree of symmetry between both eyes was analyzed and represented by intraclass correlation coefficient (ICC) values. Multivariable linear regression analysis was used to investigate the associations between ocular and systemic factors with p-RNFL thickness difference.
Results
The study included 4034 children with a mean age of 7.61 ± 0.98 years. The mean global p-RNFL thickness was 106.60 ± 9.41 μm in right eyes and 105.99 ± 9.30 μm in left eyes. The ICC for global p-RNFL difference was 0.866 (95% CI 0.858–0.873, p < 0.001). The symmetry displayed the largest values in nasal inferior quadrant with the ICC value of 0.736 (95% CI 0.721–0.749); and the smallest degree of symmetry was found to be in the superior temporal quadrant with the ICC value of 0.567 (95% CI 0.546–0.588). Axial length (AL) difference was found to have more pronounced correlation to interocular symmetry in p-RNFL thickness with the coefficient of 0.514 (p < 0.001).
Conclusions
Normal variation in interocular symmetry exists in children. Our results can contribute to the establishment of a standard reference for interocular differences in OCT parameters in children. The interocular differences in AL should be considered in the interpretation of RNFL symmetry, in terms of identifying children at risk of developing glaucoma or other ocular disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is currently limited research on interocular symmetry specifically in the thickness of the retinal nerve fiber layer (RNFL) among Chinese children. Therefore, it is crucial to assess the normal range of interocular variation and its potential associations. This information will aid eye care professionals in enhancing diagnostic accuracy in pediatric populations. |
The aim of this study was to determine the interocular differences in p-RNFL thickness and its associated factors among school children in Hong Kong. |
Our study findings demonstrate the presence of normal variation in interocular symmetry among children. These results have significant implications for establishing a standard reference for interocular differences in optical coherence tomography (OCT) parameters in this population. It is crucial to consider the interocular differences in axial length (AL) when interpreting RNFL symmetry, as this has important implications for assessing ocular health and diagnosing various ocular conditions. |
Our study contributes valuable insights to enhance the accuracy and interpretation of OCT measurements in children, further advancing ocular health assessment and disease diagnosis. |
Introduction
Interocular asymmetry could be an abnormal sign necessitating further investigation [1,2,3]. In addition, some disease entities preferentially affect one eye [4]. While our vital organs are not perfectly symmetrical due to inherent physiological asymmetries, it is important to note that a certain degree of asymmetry can be a typical variation in healthy eyes. Hence, understanding the range of this asymmetry in normal eyes is crucial.
Optical coherence tomography (OCT) is firmly established as a vital tool for structural imaging in the diagnosis and management of ophthalmic diseases [5]. Its rapid, non-invasive, and non-contact nature makes it particularly valuable in evaluating children with various ocular pathologies. However, interpreting pediatric tomograms presents unique challenges compared to those of adults, given the growth of the eyeball, changes in axial lengths, and the continuous development of the retina and optic nerve. As such, additional adjustments are essential for the precise interpretation of pediatric tomograms.
To date, in adult populations, the peripapillary retinal nerve fiber layer (p-RNFL) thickness has been well documented, with several studies establishing norms for interocular symmetry [6, 7]. However, there remain limited data specific to pediatric populations. Notably, while previous studies have examined RNFL asymmetry in children, the majority have focused on non-Asian cohorts [8, 9], leaving a noticeable gap in data specific to Chinese children. Moreover, there has been a marked increase in myopia in East Asian regions such as Hong Kong and an elongated axial length (AL) associated with myopia can influence the RNFL thickness. Given the heightened prevalence of myopia in this demographic, understanding the variations of AL and asymmetries in RNFL thickness becomes even more vital. Recognizing the normal variations and asymmetries in RNFL thickness among children can guide clinicians in distinguishing between physiological variations and pathological changes. This study aims to fill the knowledge gap by investigating the interocular symmetry of RNFL thickness and the associated factors in Chinese children, providing a foundation for future clinical and research applications in this demographic.
Methods
Study Design and Population
The Hong Kong Children Eye Study (HKCES) is a population-based cross-sectional study targeting primary school children from 6 to 8 years old in Hong Kong who were invited to visit the Hong Kong Eye Centre for comprehensive ophthalmological examinations [10,11,12,13,14,15,16]. It aims to evaluate various eye conditions among children in this age group and to determine the prevalence of different eye diseases. The sample selection was based on a stratified and clustered randomized sampling frame. Further details on sample size calculation and the study protocol were mentioned in previous reports. The participants were invited to attend in comprehensive ophthalmic examinations, physical examinations, and standardized interviews [10]. This study excluded children with congenital malformations, previous ocular trauma, a history of ocular surgery, or any ocular disorders other than refractive errors. Additionally, children with systemic diseases, except for obesity, or those who were unable to cooperate were also excluded from the study. The project adhered strictly to the Declaration of Helsinki, and approval was obtained from the Ethics Committee Board of the Chinese University of Hong Kong. Participating children and their parents gave informed consent prior to their participation in the study. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
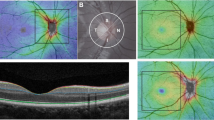
OCT Imaging
OCT imaging was performed with the Spectralis SD-OCT (Heidelberg Engineering, Heidelberg, Germany) system by a well-trained ophthalmic photographer. All the averaged B-scans in this study had a signal quality of at least 15 dB [15]. Imaging of the peripapillary retinal nerve fiber layer (p-RNFL) was performed at a central wavelength of 870 nm. For each participant, a scan circle with a diameter of approximately 3.45 mm (consisting of 1536 A-scans) was manually positioned at the center of the optic disc, with the eye-tracking system activated. Fifteen B-scans were captured at the same location and automatically averaged using the built-in software (Heidelberg Eye Explorer, version 1.6.1.0; Heidelberg Engineering) to enhance the signal-to-noise ratio of the images. The software’s automatic segmentation feature was employed to delineate the p-RNFL on each averaged B-scan. The measurements obtained from the SD-OCT scans included the mean circumpapillary p-RNFL thickness as well as the sectorial peripapillary p-RNFL thickness in six specific regions: nasal, temporal, superonasal, inferonasal, inferotemporal, and supratemporal. These measurements were derived from the segmented p-RNFL using the aforementioned built-in software. To ensure high-quality scans, all averaged B-scans included in this study had a signal quality of ≥ 15 dB, as per the manufacturer's recommendation.
Ocular Examinations
Visual acuity was measured by using a logarithm of the minimum angle of resolution (log MAR) chart (Nidek Inc., Gamagori, Aichi, Japan). Cycloplegic autorefraction was performed using an autorefractor (ARK-510A, Nidek, Gamagori, Japan) after a cycloplegic regime, which consisted of at least two cycles of eye drops. At the first cycle, two separate eye drops, cyclopentolate 1% (Cyclogyl, Alcon-Convreur, Rijksweg, Belgium) and tropicamide 1% (Santen, Osaka, Japan), were administered to both eyes 5 min apart. A second cycle of the same cycloplegic drops would be administered 10 min after the first cycle. A third cycle of the same cycloplegic eye drops would be given 30 min after the second cycle if pupillary light reflex was still present or the pupil size was less than 6.0 mm. Further cycles of cycloplegic eye drops would be administered if necessary to ensure the pupils are well dilated. Five readings, all of which had to be less than 0.25 D apart, were obtained and averaged. Ocular axial length (AL) was measured on a Zeiss IOL Master unit (Carl Zeiss Meditec Inc., Dublin, CA, USA) using noncontact partial coherence interferometry. A non-contact tonometer, Corvis ST (Corvis ST; Oculus, Arlington, WA, USA) was used to measure the subjects’ intro-ocular pressure (IOP) and central corneal thickness. Trained ophthalmologists conducted complete ocular examinations for each participant, including examinations of the anterior segment, posterior segment, and ocular motility [13,14,15,16]. Spherical equivalent refraction (SER) was defined as spherical diopters (D) plus one-half of the value for cylindrical diopters.
Other Examinations
Blood pressure (BP) was measured in the seated position after a 5-min rest using a digital autonomic BP monitor (Vital Signs Monitor; Heal Force Bio-Meditech, Shanghai, China). Body height and weight were measured using a professional integrated set (seca; Hamburg, Germany). A tape measure was used to measure the child’s waist and head circumference, the most prominent part of the forehead-1 to 2 fingers above the eyebrows and to the widest part of the back of the head. Three measurements were taken, with the average result taken for subsequent analysis. Body mass index (BMI) was calculated as body weight (in kilograms) divided by the square of body height (in meters).
Statistical Analysis
Stata Version 14.0 (StataCorp LLC, College Station, TX, USA) was used for all statistical analyses. Confidence intervals (CIs) and p values (significant at the < 0.05 level) were derived for difference estimates. Mean differences for all parameters were calculated by subtracting the left eye parameters from the right eye parameters, and their respective p values were reported using the paired sample t test. Therefore, mean differences were stated as positive when right eyes had higher values than left eyes, and vice versa. To measure interocular correlation, intraclass correlation coefficients (ICCs) were computed. Absolute interocular differences were log-transformed due to the skewed distribution. Univariable and multiple linear regression analyses were conducted to determine associations, if any, between systemic, demographic, and ocular variables (as independent variables) with log-transformed absolute interocular p-RNFL thickness differences (as dependent variables). We interpreted the effect of each independent variable on the outcome and reported the result as the unstandardized correlation coefficients (β). We also calculated the standardized regression coefficients (sβ) for each independent variable. The dataset utilized in the current study was sourced from the same dataset as our previous studies [15], emphasizing different research questions. Any data with a p value < 0.05 were considered as statistically significant.
Results
Study Population
Among the 4273 children who participated in the study, 159 either declined later or were not able to complete the OCT examination, and another 80 children were also excluded due to suboptimal imaging quality. Consequently, 8068 eyes from 4034 children were included in the final analysis, including 2067 boys (51.2%) and 1967 girls (48.8%), with a mean age of 7.61 ± 0.98 years. Among them, 1009 had myopia with the mean SER of − 1.95 ± 1.33 D (Table 1).
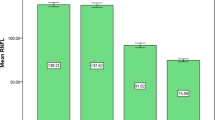
Interocular Symmetry of p-RNFL Thickness
The means for global p-RNFL thickness of right and left eyes were, respectively, 106.60 ± 9.41 μm and 105.99 ± 9.30 μm, with ICC 0.866 (95% CI 0.858 to 0.873, p < 0.001) (Table 2). The absolute difference of global p-RNFL thickness was difference was 3.58 ± 3.84 μm (Table 3).
Among the differences of p-RNFL in various quadrants, the temporal superior quadrant had the largest degree of asymmetry, with an ICC value of 0.567 (95% CI 0.546–0.588) and an absolute mean difference of 13.30 μm; while the least asymmetry was found to be in the nasal inferior quadrant, with a ICC being 0.736 (95% CI 0.721–0.750) and an absolute mean difference of 12.89 μm (Tables 2, 3).
Associations of p-RNFL Thickness Differences with AL
After adjusting for confounders such as age, sex, BMI, systolic and diastolic BP, waist and head circumference, VA, IOP, CCT, and central macular thickness, we found greater axial length differences was significantly associated with increased absolute global p-RNFL thickness difference (β = 0.514; 95% CI = [0.342, 0.687]; p < 0.001). This association with AL was significant across all subfields except temporal superior region (β from 0.051 to 0.649; p < 0.001 to 0.039) (Table 4). The univariable analysis echoed these observations, pinpointing axial length and SE differences as the predominant factors influencing the absolute global p-RNFL thickness difference, whereas variables such as age, sex, and IOP did not exhibit significant associations (Supplementary Table 1).
Discussion
In this population-based study, we established a normative database of p-RNFL thickness difference among Chinese children aged 6–8 years old in Hong Kong. We observed the differences in global and all six quadrants of the p-RNFL thickness between two eyes, indicating a discernible level of asymmetry. Notably, the disparity in axial length demonstrated a robust association with p-RNFL thickness difference: a greater variation in axial length corresponded to increased p-RNFL symmetry between eyes. Our study has clinical implications that when evaluating the nature of p-RNFL asymmetry—whether it is physiological or pathological—it is imperative to factor in the influence of axial length differences. This insight can refine diagnostic precision in pediatric patients.
We found that the ICC value of the global p-RNFL thickness was 0.872. In line with our findings, prior studies also observed the asymmetry in p-RNFL thickness between eyes [8, 9, 17]. In the Sydney Childhood Eye Study, which involved 1765 children aged 6 years, an interocular correlation of 0.7 was observed for average RNFL thickness [8]. Another study, which focused on the degree of symmetry among healthy adults of different ethnicities, showed a symmetry value of 86.7% in the mean p-RNFL thickness among Chinese [18]. This supported our data in terms of the representativeness of the ethnic Chinese populations.
We established a normative database of p-RNFL thickness in Hong Kong. In our study, the observed mean and median differences in global p-RNFL thickness were 3.85 and 2.83 μm, respectively, with the 95th percentile marked at 11 μm. This falls within the interocular differences range observed in prior studies on healthy populations. A study involving 357 healthy children determined that the typical interocular disparity in average RNFL should not surpass 13 μm for normal individuals [9]. Similarly, research conducted among adults highlighted that standard variations between the two eyes generally stay within the limits of 9–12 μm [17]. It was further posited that variations exceeding these identified thresholds could potentially be indicative of the early stages of optic neuropathy, such as glaucoma [17]. Given our findings, the majority of the studied children remains within these established norms. This emphasizes the importance of understanding these baseline variations for pediatric eye care practitioners, as discerning physiological variances from potential pathological markers is crucial. Therefore, in a clinical setting, when children present with interocular differences beyond the recognized range, further in-depth evaluation might be warranted to rule out potential pathological conditions.
Prior research has consistently indicated an inverse relationship between axial length and p-RNFL thickness, suggesting that eyes with longer axial lengths tend to have thinner p-RNFLs and vice versa [7, 19, 20]. However, few studies established the correlation of differences in axial length with variations in p-RNFL thickness. Our study is pioneering in highlighting this significant association between variances in axial length and p-RNFL thickness symmetry between the eyes. These findings carry substantial implications for interpreting axial length and p-RNFL thickness symmetry in the pediatric population, especially in the context of Hong Kong. Furthermore, when differentiating physiological from pathological asymmetry, clinicians should consider the influence of axial length differences.
In our study, the variation in p-RNFL thickness across different quadrants appeared more pronounced than that in global p-RNFL thickness. The ICC for the six quadrants ranged from 0.567 to 0.736, and the mean absolute differences extended from 7.43 to 14.82 μm. Moreover, the disparity in AL influenced p-RNFL thickness across most quadrants in varying degrees. It remains unclear how AL differences might distinctly impact different p-RNFL quadrants. Historical research observed AL correlated negatively with sectoral p-RNFL thickness in all non-temporal quadrants, but correlated positively with the temporal quadrant in both adults and children [21, 22]. There is likely redistribution of retinal nerve fiber with increasing AL, in which the retinal thickness in the most central area—the temporal sector of the RNFL—is preserved, but the peripheral retina becomes thinner since it is less resistant to traction and stretch [23]. As axial length increases, the retina is dragged towards the temporal horizon, and consequently the RNFL thickens in the temporal quadrant [24]. Although this theory provides insights, it does not entirely elucidate the phenomenon our study observed—where AL differences exert varying impacts on distinct p-RNFL quadrants. Nonetheless, it highlights the intricacy underlying the influence of AL on the quadrants of p-RNFL thickness.
The strength of this study includes its large-scale population-based setting, with its standardized random sampling method. In addition, the study had well-experienced ophthalmologists and optometrists who carried out comprehensive ophthalmoscopic examinations for the subject group in a well-equipped eye center. Meanwhile, several limitations of the study were noted. First, we did not include the optic disc parameters such as cup disk ratio (CDR) value. Second, we did not evaluate tilted disc. Also, the cyclotorsion in the tilted disc might influence the RNFL symmetry measurement, potentially resulting in under or overestimation. Third, the causal relationship between symmetry and its associated factors cannot be inferred because of the cross-sectional nature of our data. Fourth, this study included a narrow age range, from 6 to 8 years. As a result, the findings might not extend to a more diverse age group. Future studies including a broader age spectrum could provide more information on the asymmetry of p-RNFL thickness and will be warranted.
Conclusions
In conclusion, we established a normative database of p-RNFL thickness difference among Chinese children aged 6–8 years old in Hong Kong. Asymmetry in p-RNFL thickness was observed among children, with a notable association between this asymmetry and the difference in axial length between the two eyes. Our study highlights the importance of considering axial length differences when assessing the nature of p-RNFL asymmetry, whether physiological or pathological. Incorporating this understanding can enhance diagnostic accuracy in pediatric populations.
Data Availability
Deidentified participant data are available upon reasonable request from JCSY, ORCID: 0000-0002-5835-208X.
References
Lee SY, Jeoung JW, Park KH, Kim DM. Macular ganglion cell imaging study: interocular symmetry of ganglion cell-inner plexiform layer thickness in normal healthy eyes. Am J Ophthalmol. 2015;159(2):315 e2-323 e2.
Quigley HA, Enger C, Katz J, Sommer A, Scott R, Gilbert D. Risk factors for the development of glaucomatous visual field loss in ocular hypertension. Arch Ophthalmol. 1994;112(5):644–9.
Cartwright MJ, Anderson DR. Correlation of asymmetric damage with asymmetric intraocular pressure in normal-tension glaucoma (low-tension glaucoma). Arch Ophthalmol. 1988;106(7):898–900.
Yüksel D, Orban de Xivry JJ, Lefèvre P. Review of the major findings about Duane retraction syndrome (DRS) leading to an updated form of classification. Vis Res. 2010;50(23):2334–47.
Menke MN, Feke GT, Trempe CL. OCT measurements in patients with optic disc edema. Investig Ophthalmol Vis Sci. 2005;46(10):3807–11.
Li H, Healey PR, Tariq YM, Teber E, Mitchell P. Symmetry of optic nerve head parameters measured by the Heidelberg Retina Tomograph 3 in healthy eyes: the Blue Mountains Eye Study. Am J Ophthalmol. 2013;155(3):518 e1-523 e1.
Mwanza JC, Durbin MK, Budenz DL, Cirrus OCTNDSG. Interocular symmetry in peripapillary retinal nerve fiber layer thickness measured with the Cirrus HD-OCT in healthy eyes. Am J Ophthalmol. 2011;151(3):514 e1-521 e1.
Huynh SC, Wang XY, Burlutsky G, Mitchell P. Symmetry of optical coherence tomography retinal measurements in young children. Am J Ophthalmol. 2007;143(3):518–20.
Altemir I, Oros D, Elía N, Polo V, Larrosa JM, Pueyo V. Retinal asymmetry in children measured with optical coherence tomography. Am J Ophthalmol. 2013;156(6):1238.e1-1243.e1.
Yam JC, Tang SM, Kam KW, Chen LJ, Yu M, Law AK, et al. High prevalence of myopia in children and their parents in Hong Kong Chinese population: the Hong Kong Children Eye Study. Acta Ophthalmol. 2020;98(5):e639–48.
Yuan N, Li J, Tang S, Li FF, Lee CO, Ng MPH, et al. Association of secondhand smoking exposure with choroidal thinning in children aged 6 to 8 years: the Hong Kong Children Eye Study. JAMA Ophthalmol. 2019;137(12):1406–14.
Wong ES, Zhang XJ, Yuan N, Li J, Pang CP, Chen L, et al. Association of optical coherence tomography angiography metrics with detection of impaired macular microvasculature and decreased vision in amblyopic eyes: the Hong Kong Children Eye Study. JAMA Ophthalmol. 2020;138(8):858–65.
Zhang XJ, Wong PP, Wong ES, Kam KW, Yip BHK, Zhang Y, et al. Delayed diagnosis of amblyopia in children of lower socioeconomic families: the Hong Kong Children Eye Study. Ophthalmic Epidemiol. 2022;29(6):621–8.
Zhang XJ, Lau YH, Wang YM, Kam KW, Ip P, Yip WW, et al. Prevalence of strabismus and its risk factors among school aged children: the Hong Kong Children Eye Study. Sci Rep. 2021;11(1):13820.
Zhang XJ, Lau YH, Wang YM, Chan HN, Chan PP, Kam KW, et al. Thicker retinal nerve fiber layer with age among schoolchildren: the Hong Kong Children Eye Study. Diagnostics (Basel, Switzerland). 2022;12(2):500
Zhang XJ, Zhang Y, Kam KW, Tang F, Li Y, Ng MPH, et al. Prevalence of myopia in children before, during, and after COVID-19 restrictions in Hong Kong. JAMA Netw Open. 2023;6(3): e234080.
Budenz DL. Symmetry between the right and left eyes of the normal retinal nerve fiber layer measured with optical coherence tomography (an AOS thesis). Trans Am Ophthalmol Soc. 2008;106:252–75.
Tao Y, Tham YC, Chee ML, Majithia S, Thakur S, Soh ZD, et al. Profile of retinal nerve fibre layer symmetry in a multiethnic Asian population: the Singapore Epidemiology of Eye Diseases study. Br J Ophthalmol. 2020;104(6):836–41.
Chen CY, Huang EJ, Kuo CN, Wu PL, Chen CL, Wu PC, et al. The relationship between age, axial length and retinal nerve fiber layer thickness in the normal elderly population in Taiwan: the Chiayi eye study in Taiwan. PLoS ONE. 2018;13(3): e0194116.
Savini G, Barboni P, Parisi V, Carbonelli M. The influence of axial length on retinal nerve fibre layer thickness and optic-disc size measurements by spectral-domain OCT. Br J Ophthalmol. 2012;96(1):57–61.
Kang MT, Li SM, Li H, Li L, Li SY, Zhu BD, et al. Peripapillary retinal nerve fibre layer thickness and its association with refractive error in Chinese children: the Anyang Childhood Eye Study. Clin Exp Ophthalmol. 2016;44(8):701–9.
Kang SH, Hong SW, Im SK, Lee SH, Ahn MD. Effect of myopia on the thickness of the retinal nerve fiber layer measured by Cirrus HD optical coherence tomography. Investig Ophthalmol Vis Sci. 2010;51(8):4075–83.
Chen L, Huang J, Zou H, Xue W, Ma Y, He X, et al. Retinal nerve fiber layer thickness in normal Chinese students aged 6 to 17 years. Investig Ophthalmol Vis Sci. 2013;54(13):7990–7.
Zhang X, Li EY, Leung CK, Musch DC, Tang X, Zheng C, et al. Prevalence of visual impairment and outcomes of cataract surgery in Chaonan, South China. PLoS ONE. 2017;12(8): e0180769.
Acknowledgements
We thank all the children and their families for their participation in the Hong Kong Children Eye Study. We also thank our colleagues and volunteers for all their hard work and dedication in data collection for this study. We are very grateful to Ms. Mandy P.H. Ng from the Department of Ophthalmology and Visual Sciences, the Chinese University of Hong Kong for her overall coordination efforts and logistic arrangements.
Funding
This study was supported in part by the General Research Fund (GRF), Research Grants Council, Hong Kong (14111515 and 14103419 [JCY]); Collaborative Research Fund (C7149-20G [JCY]); Health and Medical Research Fund (HMRF), Hong Kong (07180826 [XJZ], 09202466 [XJZ] and 10210246 [XJZ]), National Natural Science Foundation of China (8217040098 [JCY]); and the Direct Grants of the Chinese University of Hong Kong, (4054193 [LJC] and 4054121 and 4054199 [JCY] and 178662514 [JCY] and 4054634 [XJZ] and 2022.061 [XJZ]), the Innovation and Technology Fund (7010590 [JCY]), the UBS Optimus Foundation Grant 8984 (JCY); the Centaline Myopia Fund [JCY]; Start-up Grant of CUHK (no Grant no., [XJZ]), the CUHK Jockey Club Children’s Eye Care Programme (no Grant no., [JCY]); and the CUHK Jockey Club Myopia Prevention Programme (no Grant no., [JCY]). The funding from JCY paid the journal’s Rapid Service fee.
Author information
Authors and Affiliations
Contributions
Conceptualization: Jason C Yam and Xiujuan Zhang; Data collection: Xiujuan Zhang, Yumeng Wang, Hei-Nga Chan, Yi Han Lau, Wei Zhang, Ka Wai Kam, Patrick Ip, Alvin L Young; Formal analysis and investigation: Xiujuan Zhang and Zhenzhen Jue; Writing—original draft preparation: Xiujuan Zhang, Yumeng Wang and Yi Han Lau; Writing—review and editing: all authors; Funding acquisition: Jason C Yam and Xiujuan Zhang; Resources: Jason C Yam; Supervision: Jason C Yam and Chi Pui Pang.
Corresponding author
Ethics declarations
Conflict of Interest
All named authors confirm they have no conflicts of interest to declare.
Ethical Approval
The project adhered strictly to the Declaration of Helsinki, and approval was obtained from the Ethics Committee Board of the Chinese University of Hong Kong. Participating children and their parents gave informed consent prior to their participation in the study. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhang, X.J., Wang, Y.M., Jue, Z. et al. Interocular Symmetry in Retinal Nerve Fiber Layer Thickness in Children: The Hong Kong Children Eye Study. Ophthalmol Ther 12, 3373–3382 (2023). https://doi.org/10.1007/s40123-023-00825-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00825-7