Abstract
Introduction
This study investigates factors associated with recurrent rhegmatogenous retinal detachment (RRD), macular complications, and visual outcomes after pars plana vitrectomy (PPV) without perfluorocarbon liquids (PFCLs) for primary RRD.
Methods
A longitudinal cohort study included consecutive patients with RRD who underwent PFCL-free PPV. Postoperative visual acuity and spectral-domain optical coherence tomography findings [cystoid macular edema (CME), epiretinal membrane (ERM), ellipsoid zone/interdigitation zone (EZ/IZ) damage] were collected. Logistic regression and linear mixed models analyzed rates and risk factors for RRD recurrence, CME, ERM, EZ/IZ damage, and visual acuity at 12 months.
Results
346 eyes with RRD were studied. Single-operation success rates were 96% and 93% for uncomplicated (n = 274 eyes) and complicated (n = 72 eyes) RRD, respectively. Factors associated with RRD recurrence were posterior retinal breaks [odds ratio (OR) = 10.7 compared to peripheral retinal breaks, p = 0.008], silicone oil tamponade (OR = 5.66 compared to gas, p = 0.01), and sectorial laser retinopexy (OR = 4.34 compared to 360° laser retinopexy, p = 0.007). The prevalence of CME, ERM, and EZ/IZ damage at 12 months was 10%, 9%, and 6%, respectively. Eyes with EZ/IZ defects had worse postoperative visual acuity in both uncomplicated and complicated RRD. Proliferative vitreoretinopathy (OR = 2.95, p = 0.03) and silicone oil tamponade (OR = 3.70 compared to gas, p = 0.05) were associated with EZ/IZ damage.
Conclusions
PFCL-free PPV demonstrated satisfactory single-operation success rates for uncomplicated and complicated RRD, with a low prevalence of macular complications. Analyzing factors associated with RRD recurrence can provide provisional recommendations for PFCL-free approaches in the absence of randomized trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Retinal reattachment surgeries using perfluorocarbon liquids (PFCLs) have potential risks and complications. There is a need for safer and more cost-effective techniques in retinal reattachment surgeries. |
The study aimed to evaluate the efficacy and outcomes of PFCL-free pars plana vitrectomy (PPV) in uncomplicated and complicated rhegmatogenous retinal detachment (RRD). |
What was learned from the study? |
PFCL-free PPV demonstrated satisfactory single-operation success rates for both uncomplicated and complicated RRD cases. |
Macular complications were infrequent and mainly observed in complex RRD cases. Outer retinal damage emerged as a critical predictor of postoperative vision, emphasizing the importance of careful assessment of macular morphology. |
The study suggests the need for further research to explore alternative surgical strategies and refine treatment approaches for complex RRD cases. |
Introduction
Rhegmatogenous retinal detachment (RRD) is a sight-threatening condition affecting a significant number of individuals, with an annual incidence of 10 to 20 cases per 100,000 population in high-income countries [1, 2]. Pars plana vitrectomy (PPV) is a widely performed surgical procedure for RRD repair, with advancements in surgical techniques and tools leading to improved visual outcomes and long-term anatomical success [3].
Perfluorocarbon liquids (PFCLs) have historically played a critical role in vitreoretinal surgery, facilitating retina flattening, subretinal fluid (SRF) drainage, macular protection, and intraocular foreign body removal. However, the use of PFCLs has been associated with rare but severe complications, including inflammation, subretinal migration, and toxicity to the inner retina or retinal pigment epithelium (RPE) [4]. In recent years, PFCL-free PPV techniques, involving direct SRF aspiration through retinal breaks or surgical retinotomy, have gained popularity [5]. These techniques have demonstrated comparable visual outcomes and single-operation success rates to PFCL-assisted PPV for uncomplicated RRD [6,7,8,9,10,11,12,13]. Nevertheless, data on PFCL-free PPV in complicated RRD cases are limited [14], and little is known about factors associated with RRD recurrence in this approach.
While previous studies, including the ELLIPSOID study, have explored macular complications associated with different SRF drainage techniques in PPV for primary RRD, none have specifically evaluated factors linked to outer retinal damage, cystoid macular edema (CME), and other macular complications in PFCL-free PPV [12]. At our center, PFCL-free PPV has been routinely performed for uncomplicated RRD since 2015, and this study aims to investigate factors related to RRD recurrence in PFCL-free PPV for both complicated and uncomplicated RRD cases. Additionally, the study seeks to estimate the prevalence of macular complications detected by spectral-domain optical coherence tomography (SD-OCT) and their associations with visual outcomes at 12 months.
The findings from this study are expected to serve as a valuable reference for surgeons adopting PFCL-free PPV approaches and provide provisional treatment recommendations for uncomplicated and complicated RRD cases. By shedding light on the factors influencing RRD recurrence and macular complications, this research contributes to a broader understanding and refinement of surgical strategies for managing RRD.
Methods
This longitudinal cohort study was conducted at a tertiary referral center, San Gerardo Hospital, Monza, Italy, from March 2017 to June 2021. The study included patients with RRD repaired using PFCL-free PPV. To be eligible, patients had to have at least one postoperative SD-OCT scan and a minimum follow-up duration of 6 months. Exclusion criteria comprised previous intraocular surgery (except uncomplicated phacoemulsification), other retinal or optic nerve diseases, ocular trauma, or prior retinal detachment.
Patients were categorized into two groups: complicated RRD and uncomplicated RRD. Complicated RRD encompassed cases with high myopia (≤ − 6.00 diopters or axial length > 26.5 mm) prior to cataract extraction, RRD originating from a macular hole or macular schisis, giant retinal tears, choroidal detachment, or proliferative vitreoretinopathy (PVR) worse than grade A [14, 15]. The remaining eyes were classified as uncomplicated RRD. The study adhered to the Declaration of Helsinki and received approval from the local Institutional Review Board (CE-MILAN-V1, approval date 01/28/2022).
Data, including patient demographics, concomitant cataract extraction, surgery duration, macular involvement, retinal break characteristics (e.g., presence of multiple breaks, location, and size), PVR grade, tamponading agent used, preoperative and postoperative visual acuity (converted into LogMAR), RRD recurrences, and complications, were extracted from the hospital’s electronic medical records. All available preoperative and postoperative SD-OCT scans were evaluated by a retina specialist (MVC).
Surgical Procedure
All surgeries were performed by a single vitreoretinal surgeon (MC). Simultaneous phacoemulsification with aspheric intraocular lens implantation (RayOne Aspheric RAO 600 C) was performed when lens opacity was considered visually impairing. At the end of phacoemulsification, 0.1 ml of intracameral cefuroxime (1 mg/0.1 ml) was injected.
A three-port PPV was performed using the Constellation vitrectomy system (Alcon, Fort Worth, TX) and a binocular indirect ophthalmo-microscope for a non-contact, wide-angle view. Core vitrectomy and peripheral vitreous shaving were performed, and retinal breaks were identified with scleral depression. If no tear could be seen, a small retinotomy was performed. Subretinal fluid was evacuated through retinal breaks under air, followed by laser retinopexy around the breaks. Laser photocoagulation was extended to 360° at the surgeon’s discretion. In cases of PVR, proliferative membrane peeling was performed, with surgical retinotomy if necessary. No episcleral buckle was used.
The eye was filled with a tamponade agent [C3F8 16%, SF6 20%, or silicone oil (100% polydimethylsiloxane, PDMS, 1000 cS)] based on the surgeon’s clinical judgment. Sclerotomies were sutured with 8/0 Vicryl, and a combination of 2 mg dexamethasone/1 mg gentamycin was injected into the subconjunctival space. Patients received a fixed steroid/antibiotic combination for the first month after surgery. Face-down posturing was maintained for the first postoperative day, followed by 10 days of positioning based on retinal break location.
Imaging Evaluation
SD-OCT scans were obtained using the Spectralis OCT (Heidelberg Engineering GmbH, Heidelberg, Germany). An SD-OCT raster macular volume of 26 scans centered on the fovea was evaluated. Additional SD-OCT scans were inspected if available. Parameters assessed on postoperative SD-OCT included:
-
CME (defined as a central subfield macular thickness increase of at least 10% from the baseline, together with cystoid changes at the fovea)
-
Epiretinal membrane (ERM) involving the fovea
-
Ellipsoid zone/interdigitation zone (EZ/IZ) damage, defined as a focal optical attenuation or interruption of the EZ and/or the IZ under the fovea or juxtafoveally
-
Residual SRF
-
Full-thickness retinal folds
-
Outer retinal folds (ORF), seen as hyperreflective partial thickness folds created by EZ/IZ infolding [16]
-
Macular hole.
Statistical Analysis
Statistical analyses were performed with the open-source programming language R [16]. Descriptive statistics for continuous data were presented as mean ± standard deviation (SD) or median and interquartile range (IQR). Baseline characteristics were compared between uncomplicated and complicated RRD eyes using logistic regression models.
The rate of RRD recurrence was determined using Kaplan–Meier statistics. Logistic regression models were employed to investigate factors associated with RRD recurrences, CME, ERM, EZ/IZ loss, residual SRF, and ORF. The reported results included odds ratios (ORs) and 95% confidence intervals (CIs). Significant covariates were included in the multivariable models. Factors related to visual acuity at 12 months were examined using linear regression models, incorporating available data beyond the minimum 6 months follow-up period. Regression estimates and standard errors (SE) were calculated. Recurrent RRD eyes were excluded from this analysis to avoid confounding, and missing data on visual acuity were addressed using the last observation carried forward approach.
All the models were corrected for a history of phacoemulsification at the time of PPV or during follow-up to account for potentially worse vision in eyes developing postoperative lens opacity. Statistical significance was set at p = 0.05 unless specified otherwise.
Results
A total of 346 eyes from 333 patients who underwent PFCL-free PPV for primary RRD were included in the study. Among them, 274 eyes (79%) had uncomplicated RRD, while 72 eyes (21%) had complicated RRD. The complicated RRD group comprised eyes with various complicating factors, including pathologic myopia (39 eyes, 54%), PVR grade B or worse (15 eyes, 21%), giant tears (15 eyes, 21%), RRD starting from a macular hole (11 eyes, 15%), and choroidal detachment (3 eyes, 4%). Notably, some patients with complicated RRD had multiple complicating factors. Peripheral schisis-associated RRD was not observed.
The clinical characteristics of the patients are summarized in Table 1. Sixty-five eyes (24%) with uncomplicated RRD and 25 eyes (35%) with complicated RRD had macula-off RRD (p = 0.06). Eyes with complicated RRD were more myopic (− 8.60 ± 3.73 vs. − 2.40 ± 2.22 diopters, p < 0.001) and had longer PPV surgery durations (49.6 ± 17.8 vs. 43.3 ± 11.9 min, p = 0.005) than eyes with uncomplicated RRD. Silicone oil was used more frequently as a tamponading agent in complicated RRD cases (10% vs. 4%, p = 0.04), while 360° laser retinopexy was performed more often in uncomplicated RRD cases (88% vs. 75%, p = 0.005). There were no significant differences in other characteristics.
The mean postoperative follow-up duration was similar for uncomplicated and complicated patients with RRD (p = 0.8): 11 ± 2.0 months (range 6–44). A higher percentage of complicated RRD eyes underwent cataract extraction during follow-up (21% vs. 9%, p = 0.01).
RRD Recurrences
RRD recurrences were observed in 15 eyes (4%). Among these, 10 eyes (4%) belonged to the uncomplicated RRD group and 5 eyes (7%) belonged to the complicated RRD group (p = 0.2). In the complicated RRD group, recurrent RRD occurred in 2 out of 39 patients with pathologic myopia (5%), 1 out of 15 eyes with PVR grade B or worse (7%), none of the 15 eyes with giant tears (0%), 2 out of 11 eyes with RRD starting from a macular hole (18%), and 2 out of 3 eyes with choroidal detachment (67%). It is important to note that one patient had concurrent myopia and a macular hole, and another patient had myopia and choroidal detachment.
Among the eyes with recurrent RRD, 12 eyes underwent one surgery, while 3 eyes required two surgeries for RRD repair. Median time to RRD recurrence was 31 days (interquartile range: 15.5 to 75.5), with similar median values observed for uncomplicated RRD (24.5 days, interquartile range: 15 to 83.4) and complicated RRD (31 days, interquartile range: 24 to 36).
Due to the small number of events, a subset analysis for risk factor analysis between complicated and uncomplicated RRD was not feasible. Logistic regression analysis in the entire cohort revealed that eyes with posterior retinal breaks (OR = 10.7 vs. peripheral retinal breaks, 95% CI 1.43 to 55.6, p = 0.008), silicone oil tamponade (OR = 5.66 vs. gas, 95% CI 1.19 to 20.41, p = 0.01), and an absence of 360° laser retinopexy (OR = 4.34, 95% CI 1.40 to 12.66, p = 0.007) had a higher likelihood of RRD recurrence.
The presence of a macular hole or choroidal detachment was associated with a high risk of RRD recurrence, though with wide confidence intervals due to the small numbers (95% CI 1.78 to 224.2, p = 0.045 for a macular hole; 95% CI 4.59 to 1,135, p = 0.001 for choroidal detachment). Longer surgeries (OR = 2.08 for each 30 min increase, 95% CI 0.85 to 4.76, p = 0.07) showed an association with a higher risk of RRD recurrence at a confidence level of α = 0.1.
Prevalence of SD-OCT Features
The prevalence of SD-OCT features was also evaluated. Cystoid macular edema was the most common finding, occurring in 36 eyes (10%). Older age (61.9 ± 10.7 vs. 57.7 ± 10.6, p = 0.02), posterior retinal tears (8% vs. 2%, p = 0.04), preoperative presence of PVR (17% vs. 3% for grade B-D PVR, p < 0.001), silicone oil tamponade (17% vs. 4%, p = 0.002), and RRD recurrence (19% vs. 3%, p < 0.001) were associated with postoperative CME. Postoperative SD-OCT scans revealed an association between CME and EZ/IZ damage (17% vs. 5%, p = 0.01) as well as ERM (32% vs. 11%, p = 0.003) (Supplementary Material Table 1, Fig. 1).
Clinical example of macular complications after rhegmatogenous retinal detachment repair. A Optical coherence tomography (OCT) structural B-scan of a patient 5 days after perfluorocarbon-liquid-free vitrectomy for superior RRD. The OCT shows diffuse disruption of the ellipsoid zone (EZ) and the interdigitation zone (IZ) (white arrow), and intraretinal cysts (asterisk). The co-registered near-infrared image shows the shadow from the gas bubble superiorly. B OCT structural B-scan acquired 3 months after vitrectomy shows an epiretinal membrane (white arrowhead), increased intraretinal cysts (white asterisk), and a focal interruption in the EZ/IZ under the fovea (white arrow). C Blue-light fundus autofluorescence (FAF) shows a hyper-FAF signal corresponding to intraretinal cysts. D Late-frame fluorescein angiography shows dye leakage in the macula and late pooling corresponding to the intraretinal cysts
Epiretinal membrane was the second most common finding, detected in 32 eyes (9%). The use of larger-gauge instruments (19% vs. 3% for 23-gauge, p = 0.001) and the presence of giant tears (13% vs. 4%, p = 0.02) and preoperative PVR (13% vs. 4% for grade B–D PVR, p = 0.03) were associated with ERM detection during follow-up. Multivariable logistic regression analysis identified the presence of giant tears (OR = 5.88, 95% CI 1.10 to 28.4, p = 0.03) and the use of 23-gauge vitrectomy probes (OR = 5.18, 95% CI 1.03 to 31.11, p = 0.045) as independent associations with ERM (Supplementary Material Table 2).
EZ/IZ damage was observed in 21 eyes (6%). The presence of PVR (14% vs. 3% for grade A PVR, OR = 2.95, 95% CI 1.10 to 8.75, p = 0.03) and silicone oil tamponade (14% vs. 4%, OR = 3.70, 95% CI 0.80 to 12.57, p = 0.05) were associated with postoperative EZ/IZ damage (Supplementary Material Table 3).
Outer retinal folds were seen in 17 eyes (5%), with the development of ERM after the surgery (35% vs. 13%, OR = 3.80, 95% CI 1.22 to 10.90, p = 0.01) being the only associated factor (Fig. 2). Residual fluid was observed in 14 eyes (4%), but no cases persisted at the last available SD-OCT, and no significant associations were found. No ORF or residual SRF was found at the fovea.
Occurrence and follow-up of an outer retinal fold (ORF) after rhegmatogenous retinal detachment (RRD) repair. A Optical coherence tomography (OCT) structural B-scan of a patient with superior rhegmatogenous retinal detachment showing subretinal fluid superiorly. B OCT structural B-scan of the same patient after perfluorocarbon-liquid-free vitrectomy, showing a partial-thickness hyperreflective roundish lesion in the outer retina due to the EZ/IZ infold (white arrowhead). C, D Repeated OCT structural B-scan in the first 12 postoperative months, showing progressive flattening of the outer retinal fold. E OCT structural B-scan showing resolution of the outer retinal fold (white arrowhead); the patient also developed an epiretinal membrane (white arrow)
Macular hole development occurred in 10 eyes (3%), with 60% associated with macular hole-associated RRD and 10% with preoperative ERM. Three eyes (1%) developed a full-thickness macular fold.
Visual Acuity at 12 Months
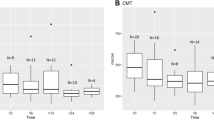
Visual acuity at 12 months showed improvements from baseline (1.25 ± 1.17 LogMAR) to month 3 (0.46 ± 0.58 LogMAR, p < 0.001), month 6 (0.34 ± 0.38 LogMAR, p < 0.001), and month 12 (0.39 ± 0.45 LogMAR, p < 0.001). At 12 months, uncomplicated RRD eyes had significantly better visual acuity compared to complicated RRD eyes (0.29 ± 0.31 vs. 0.51 ± 0.65 LogMAR, p = 0.002). Multivariable analysis showed that in the uncomplicated RRD group, eyes with EZ/IZ damage had significantly worse vision [regression estimate (SE) = 0.35 (0.09) LogMAR, p = 0.002], while in the complicated RRD group, the use of silicone oil as tamponading agent [regression estimate (SE) = 1.28 (0.30) LogMAR vs. gas, p = 0.001] and EZ/IZ damage [regression estimate (SE) = 0.64 (0.40) LogMAR, p = 0.02] were independently associated with worse visual acuity at 12 months (Table 2).
Discussion
The present study adds to the increasing body of evidence supporting the adoption of PFCL-free techniques in vitreoretinal surgery for retinal reattachment. PFCL-free procedures have gained popularity among vitreoretinal surgeons due to several potential advantages, such as avoiding retinal toxicity, reducing surgery times and costs, and minimizing intraoperative manipulations. Furthermore, procedures involving PFCLs carry a notable risk of accidental PFCL migration into the subretinal space, a potentially serious event that can lead to decreased visual acuity and scotomata. This global trend is evident in reports from various countries, including Canada [12], the United States [11], Italy [10], Israel [7], India [13], China [8], and Japan [9], all of which have shown widespread adoption of PFCL-free techniques.
This study contributes to the existing literature by presenting one of the largest series (n = 346) of PFCL-free PPV surgeries for both uncomplicated and complicated RRD. Previous studies have reported favorable outcomes with PFCL-free PPV, showing high single-operation success rates. For instance, Chen et al. conducted a small prospective study on uncomplicated RRD eyes managed with PPV and partial PFCL-free subretinal fluid drainage, achieving a single-operation success rate of 91.6% at 3 months [8]. Subsequent retrospective case series have further supported the positive outcomes of PFCL-free PPV. Additionally, it is important to consider the impact of surgeons’ experience and skills over time as well as the thoughtful selection of cases when analyzing surgical outcomes.
The main objective of this study was to investigate factors associated with RRD recurrence. In the analysis of uncomplicated RRD eyes, previous studies indicated that intraoperative 360° prophylactic laser photocoagulation was linked to a reduced risk of re-detachment [17, 18], suggesting its potential to prevent re-detachment from overlooked breaks. However, due to the small number of events, we could not perform a subset analysis of uncomplicated and complicated RRD regarding the role of 360° prophylactic laser photocoagulation. We acknowledge that 360° retinopexy was more commonly performed in cases perceived to have a higher risk of re-detachment compared to eyes where focal laser was used, leading to a potential selection bias that might have influenced the observed association between 360° retinopexy and a lower re-detachment rate. Moreover, the drawbacks of intraoperative 360° laser retinopexy include increased total operating time and the need for scleral depression to coagulate peripheral retinal locations. A navigated pattern laser (Navilas) could also have been used postoperatively [19]. A higher rate of RRD recurrence was observed in eyes filled with silicone oil, but this could also be attributed to a selection bias, as silicone oil is typically used in eyes perceived to be at a higher risk of re-detachment.
In cases of complicated RRD, including traumatic RRD, high myopia, choroidal detachment, recurrent RRD, a macular hole, high-grade PVR, and giant tears, the recurrence rate was estimated to be 7%, which aligns with a previous study by Bai et al. reporting a recurrence rate of 13% in complicated RRD managed with PFCL-free PPV [14]. While certain subgroups of complicated RRD, such as pathologic myopia, PVR, and giant tears, showed single-operation success rates similar to uncomplicated RRD, poorer outcomes were observed in cases with posterior retinal breaks, a macular hole, or concurrent choroidal detachment. These findings suggest that alternative surgical strategies may be necessary for such cases.
Optical coherence tomography imaging was utilized to assess postoperative outcomes in this study. Common findings after retinal reattachment surgery, as observed in previous studies [20], include residual pockets of SRF, CME, ORF, a macular hole, ERM, and EZ/IZ damage [21, 22]. The prevalence rates of these complications in PFCL-free PPV eyes were estimated to be 4% for SRF, 5% for ORF, 6% for EZ/IZ damage, and 3% for a macular hole. These rates are in line with previous reports, although caution should be exercised when comparing studies due to potential variations in the timing of OCT assessments [7,8,9,10]. Nevertheless, these findings underscore the importance of vigilant postoperative monitoring and timely intervention to address macular complications in PFCL-free PPV cases.
The ELLIPSOID study, which included 300 eyes with RRD that underwent PPV with different SRF drainage techniques, reported a lower proportion of EZ/IZ damage at 12 months in eyes undergoing PFCL-free PPV [12]. These findings support the idea that PFCL-free PPV may be associated with less retinal turbulence, SRF currents, and forced retinal repositioning compared to PFCL-assisted PPV [23]. However, it is important to note that the occurrence of CME, ERM, and EZ/IZ damage together suggests that outer retinal damage is multifactorial, and epiretinal traction may also contribute to outer retinal disruption. The dynamic changes in EZ/IZ reflectivity after retinal reattachment and the timing of SD-OCT assessment can influence the rate of EZ/IZ damage [21].
The presence of PVR preoperatively and RRD recurrence were identified as risk factors for CME, consistent with previous studies [24]. ERM was found more frequently in eyes with giant tears, likely due to the higher chances of RPE dispersion and vitreous hemorrhage in these cases [25]. ERM was also associated with the use of large-caliber vitrectomy probes (23-gauge), which may be related to the complexity of the cases operated using these probes [26]. ORF was more frequently observed in association with ERM, suggesting that epiretinal traction could impede retinal relaxation after reattachment, favoring ORF formation.
Visual acuity significantly improved from baseline to 12 months in this study, and final VA scores were comparable to those reported in other PFCL-free cohorts [7, 11]. Postoperative EZ/IZ damage was associated with worse vision after adjusting for confounding variables such as cataract extraction during or after PPV. These results align with previous studies, indicating a link between functional outcomes of RRD repair and the integrity of photoreceptors on SD-OCT [27, 28].
The present study has several strengths, including a relatively large sample size and the comprehensive availability of SD-OCT data for all study eyes, allowing for objective and repeatable functional and prognostic assessments. However, there are some limitations that need to be acknowledged. The retrospective design of the study may introduce selection bias due to loss to follow-up, favoring more complicated or recurrent RRD cases. Additionally, the dropout rate limited the use of more sophisticated statistical analyses, and certain functional and anatomical outcomes, such as metamorphopsia and retinal vessel displacement, were not evaluated. The analysis focused on a 26-scan macular volume, potentially underestimating extra-macular pathology. Clinically relevant details, including the time elapsed between RRD and repair surgery, were missing, and this factor could have influenced visual outcomes, especially in cases with macular detachment at the time of surgery. The classification of pseudophakic eyes based on refraction status prior to cataract surgery was not possible for all patients due to unavailable data. Furthermore, postoperative SD-OCT data were analyzed at different postoperative times, which may have led to an underestimation of some postoperative complications, such as ERM or CME development.
Conclusion
In conclusion, the study contributes valuable insights into the efficacy of PFCL-free PPV for both uncomplicated and complicated RRD. The prevalence of macular complications was low, and they were predominantly observed in complicated RRD cases. Outer retinal damage was identified as a crucial predictor of postoperative vision. The analysis of risk factors for RRD recurrence provided provisional recommendations for PFCL-free approaches, suggesting that heavy liquid retinal reattachment may be necessary in cases with posterior retinal breaks, macular holes, and concurrent choroidal detachment. The use of SD-OCT imaging allowed for an objective assessment of postoperative outcomes and confirmed the association between EZ/IZ damage and visual outcomes. However, the retrospective design and limitations of the study warrant further prospective investigations to validate these findings and explore additional functional and anatomical outcomes.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Madi HA, Keller J. Increasing frequency of hospital admissions for retinal detachment and vitreo-retinal surgery in England 2000–2018. Eye (Lond). 2022;36(8):1610–4.
Mitry D, Charteris DG, Yorston D, et al. The epidemiology and socioeconomic associations of retinal detachment in Scotland: a two-year prospective population-based study. Invest Ophthalmol Vis Sci. 2010;51(10):4963–8.
Sodhi A, Leung LS, Do DV, et al. Recent trends in the management of rhegmatogenous retinal detachment. Surv Ophthalmol. 2008;53(1):50–67.
Yu Q, Liu K, Su L, et al. Perfluorocarbon liquid: its application in vitreoretinal surgery and related ocular inflammation. Biomed Res Int. 2014;2014: 250323.
Hahn P. ASRS 2022 preferences and trends membership survey. Chicago: American Society of Retina Specialists; 2022.
Coppola M, Marchese A, Cicinelli MV, et al. Letter to the editor: Perfluorocarbon-free vitrectomy for rhegmatogenous retinal detachment: feasibility and outcomes in the small-gauges era. Curr Eye Res. 2019;44(8):925–6.
Vidne O, Blum Meirovitch S, Rabina G, et al. Perfluorocarbon liquid vs. subretinal fluid drainage during vitrectomy for the primary repair of rhegmatogenous retinal detachment: a comparative study. Curr Eye Res. 2018;43(11):1389–94.
Chen X, Zhang Y, Yan Y, et al. Complete subretinal fluid drainage is not necessary during vitrectomy surgery for macula-off rhegmatogenous retinal detachment with peripheral breaks: a prospective, nonrandomized comparative interventional study. Retina. 2017;37(3):487–93.
Yamaguchi M, Ataka S, Shiraki K. Subretinal fluid drainage via original retinal breaks for rhegmatogenous retinal detachment. Can J Ophthalmol. 2014;49(3):256–60.
Chelazzi P, Azzolini C, Bellina C, et al. Efficacy and safety of vitrectomy without using perfluorocarbon liquids and drainage retinotomy associated with postoperative positioning based on residual subretinal fluid for rhegmatogenous retinal detachment. J Ophthalmol. 2021;2021:5588479.
Vo LV, Ryan EH, Ryan CM, et al. Posterior retinotomy vs perfluorocarbon liquid to aid drainage of subretinal fluid during primary rhegmatogenous retinal detachment repair (PRO study report no. 10). J Vitreoretin Dis. 2020;4(6):494–8.
McKay BR, Bansal A, Kryshtalskyj M, et al. Evaluation of subretinal fluid drainage techniques during pars plana vitrectomy for primary rhegmatogenous retinal detachment—ELLIPSOID study. Am J Ophthalmol. 2022;241:227–37.
Kumari N, Surve A, Kumar V, et al. Comparative evaluation of outcomes of drainage techniques in vitrectomy for rhegmatogenous retinal detachment. Retina. 2022;42(1):27–32.
Bai Y, Song Q, Liu J, et al. Vitrectomy for complicated retinal detachment without the use of perfluorocarbon liquid: a real-world data and retrospective study. Ophthalmol Ther. 2022;11(2):857–68.
Machemer R, Aaberg TM, Freeman HM, et al. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1991;112(2):159–65.
Muni RH, Darabad MN, Oquendo PL, et al. Outer retinal corrugations in rhegmatogenous retinal detachment: the retinal pigment epithelium-photoreceptor dysregulation theory. Am J Ophthalmol. 2022. https://doi.org/10.1016/j.ajo.2022.08.019.
He Y, Zeng S, Zhang Y, Zhang J. Risk factors for retinal redetachment after silicone oil removal: a systematic review and meta-analysis. Ophthalmic Surg Lasers Imaging Retina. 2018;49(6):416–24.
Dirani A, Antaki F, Rheaume MA, et al. 360-Degree intra-operative laser retinopexy for the prevention of retinal re-detachment in patients treated with primary pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2020;258(2):249–56.
Kulikov AN, Maltsev DS, Boiko EV. Navigated pattern laser system versus single-spot laser system for postoperative 360-degree laser retinopexy. J Ophthalmol. 2016;2016:9871976.
Coppola M, Marchese A, Cicinelli MV, et al. Macular optical coherence tomography findings after vitreoretinal surgery for rhegmatogenous retinal detachment. Eur J Ophthalmol. 2020;30(4):805–16.
Figueiredo N, Sarraf D, Gunnemann F, et al. Longitudinal assessment of ellipsoid zone recovery using en face optical coherence tomography after retinal detachment repair. Am J Ophthalmol. 2022;236:212–20.
Baudin F, Deschasse C, Gabrielle PH, et al. Functional and anatomical outcomes after successful repair of macula-off retinal detachment: a 12-month follow-up of the DOREFA study. Acta Ophthalmol. 2021;99(7):e1190–7.
Muni RH, Felfeli T, Sadda SR, et al. Postoperative photoreceptor integrity following pneumatic retinopexy vs pars plana vitrectomy for retinal detachment repair: a post hoc optical coherence tomography analysis from the pneumatic retinopexy versus vitrectomy for the management of primary rhegmatogenous retinal detachment outcomes randomized trial. JAMA Ophthalmol. 2021;139(6):620–7.
Starr MR, Cai L, Obeid A, et al. Risk factors for presence of cystoid macular edema following rhegmatogenous retinal detachment surgery. Curr Eye Res. 2021;46(12):1867–75.
Glaser BM. Treatment of giant retinal tears combined with proliferative vitreoretinopathy. Ophthalmology. 1986;93(9):1193–7.
Pan Q, Gao Z, Hu X, et al. Risk factors for epiretinal membrane in eyes with primary rhegmatogenous retinal detachment that received silicone oil tamponade. Br J Ophthalmol. 2022. https://doi.org/10.1136/bjophthalmol-2021-320121.
Malosse L, Rousseau H, Baumann C, et al. Prevalence and risk factors for outer retinal layer damage after macula-off retinal detachment. Br J Ophthalmol. 2020;104(5):660–5.
Gharbiya M, Grandinetti F, Scavella V, et al. Correlation between spectral-domain optical coherence tomography findings and visual outcome after primary rhegmatogenous retinal detachment repair. Retina. 2012;32(1):43–53.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
All the authors (Maria Vittoria Cicinelli, Eleonora Benatti, Vincenzo Starace, Francesco Nadin, Edoardo di Nisi, Francesco Bandello, Michele Coppola) contributed to the conception or design of the work, the acquisition, analysis, and interpretation of data, drafting the work, and revising it critically for important intellectual content. Each of the co-authors has seen and agrees with each of the changes made to this manuscript in the revision, and to the way his or her name is listed.
Corresponding author
Ethics declarations
Conflict of Interest
The authors (Maria Vittoria Cicinelli, Eleonora Benatti, Vincenzo Starace, Francesco Nadin, Edoardo di Nisi, Francesco Bandello, Michele Coppola) have no competing interest in publishing the present work.
Ethical Approval
The Institutional Review Board of San Gerardo (Monza, Italy) granted ethical approval and exempted the study from written informed consent due to its retrospective and non-interventional design. The study adhered to the Declaration of Helsinki and received approval from the local Institutional Review Board (CE-MILAN-V1, approval date 01/28/2022).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cicinelli, M.V., Benatti, E., Starace, V. et al. Recurrences and Macular Complications after Perfluorocarbon-Liquid-Free Vitrectomy for Primary Rhegmatogenous Retinal Detachment. Ophthalmol Ther 12, 3219–3232 (2023). https://doi.org/10.1007/s40123-023-00811-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00811-z