Abstract
Introduction
The purpose of this study was to report the success and long-term outcomes of cyanoacrylate tissue adhesive (CTA) application in the management of corneal perforation disorders.
Methods
This retrospective case series describes the profile and outcomes of eyes that underwent CTA for corneal perforation over an 11-year period from January 2009 until January 2020 at a tertiary eye centre in the United Kingdom.
Results
In total, 25 eyes underwent CTA application during the study period. Non-traumatic sterile corneal melt was responsible in more than half of the cases (56.0%; n = 14) followed by infection (32.0%; n = 8) and trauma (12.0%; n = 3). Median size of perforation was 2.0 mm (interquartile range, IQR 1.0–3.0). The most common anatomical location of corneal perforation was central (56.0%; n = 14). Ocular surface disease was seen in almost all eyes except two (92.0%; n = 23) with dry eye disease being the most common (48.0%; n = 12). Amongst 23 eyes that completed follow-up (median 27 months; IQR 9.5–46.5), single CTA application was successful in achieving intact globe in 13 (56.5%) eyes and repeat gluing sealed total of 20 (86.9%) eyes. Survival analysis showed cumulative success of 71.0% and 51.2% at 90 and 250 days, respectively. The CTA was retained in the eyes for median of 94.0 days (IQR 30.0–140.5). A total of five patients developed adverse events, including endophthalmitis (n = 2), following CTA application.
Conclusions
CTA was highly effective in sealing corneal perforations in acute setting and showed moderate long-term success. However, multiple applications are often required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There is a lack of studies reporting long-term outcomes of cyanoacrylate tissue adhesive (CTA) following corneal perforation. |
In this study we have tried to report long-term outcomes and safety of CTA. |
What was learned from the study? |
We observed that CTA is not only an effective treatment modality in restoring globe anatomy in acute setting, but also that it has favourable long-term outcomes with an acceptable safety profile. |
Introduction
Corneal perforation is an ophthalmic emergency and requires urgent management to prevent disastrous outcomes [1,2,3]. Timely intervention is required to seal the perforation and restore the anterior chamber anatomy, which may otherwise lead to profound visual loss, endophthalmitis, and even loss of the eye [2]. Several different methods have been described in the literature to acutely seal the perforation including: (i) bandage contact lens (BCL) insertion [4], (ii) tissue adhesives [5, 6], (iii) conjunctival flaps [7], (iv) multi-layered amniotic membrane transplantation (AMT) [8], (v) Tenon’s patch graft [9], and (vi) lamellar or penetrating tectonic corneal grafts [10]. The choice of intervention depends on the size and location of the perforation, sterility status of the wound, availability of donor tissue and surgeon experience.
Tissue adhesives are commonly used in repair of small to medium size (≤ 3.0 mm) corneal perforations [2, 6, 11]. Their ease of use and effectiveness have made them a popular choice in acute setting where urgent intervention is required to restore the ocular anatomy. Although both types of tissue adhesives – biologic (fibrin adhesive) and synthetic (cyanoacrylate derivatives) – can be used to seal corneal perforations, the latter is more frequently used due to its prolonged retention time and cost-effectiveness [6, 12].
There are several studies that have reported use of cyanoacrylate tissue adhesives (CTA) in the acute management of corneal perforations with variable success rate in re-establishing globe integrity [11, 13,14,15,16,17,18]. However, there is paucity of evidence highlighting long-term outcomes of CTA application and factors influencing treatment success. To our knowledge, only one study to date has reported long-term survival outcomes of CTA application and analysed the factors determining treatment failure [3]. Therefore, in this study we aimed to report long-term outcomes of CTA gluing performed in a tertiary ophthalmic unit in the United Kingdom (UK).
Methods
In this retrospective single-centre case series, we reviewed clinical records of all consecutive patients who underwent CTA application for corneal perforation due to any aetiology from January 2009 until January 2020 at the Ophthalmology Department, Royal Victoria infirmary, Newcastle upon Tyne, UK. The study was conducted following the principles of the Declaration of Helsinki and was registered for retrospective data collection with the Clinical Governance Department of the Newcastle upon Tyne Hospitals NHS Foundation Trust (ref: 10,323). Informed consent was obtained from all patients.
A total of 25 eyes of 25 subjects were identified from theatre entries during the study period. Two patients were lost to follow-up after corneal gluing, and they were excluded from final outcome analysis. The remaining 23 patients had at least 3 months of follow-up data. All cases had Seidel-positive test on presentation. The information extracted from clinical case records included demographics, past medical and ophthalmic history, ocular co-morbidities, aetiology of perforation, best-corrected distance visual acuity (BCDVA), intraocular pressure (IOP), presence of ocular surface disease (OSD), location (central versus peripheral) and size of the perforation, status of BCL post-CTA, number of CTA applications, subsequent complications, additional interventions required, and final outcomes.
Outcomes of the study were recorded as primary and secondary successes. Primary success after CTA was defined as intact globe with no leak without need for repeat CTA or any other intervention. Secondary success implied intact globe with no leak with repeat CTA but no other intervention post-CTA. Essentially, secondary success included a subset of cases that required repeat gluing to achieve water-tight non-leaking globe.
Surgical Technique
All cases underwent the same technique of CTA application. It involved punching of a small disc (i.e. 3.0–5.0 mm depending on the perforation size) from a thin non-adhesive part of the transparent surgical plastic drape and placing a tiny drop of adhesive over one side of the disc. The disc was then gently placed over the perforation site with the CTA facing down using Paton Titanium Spatula (D&K 9-820, UK). The adhesive polymerised within seconds, forming a firm water-tight seal underneath the non-abrasive surfaced plastic disc. Soft BCL (D&N Novartis, UK®) was applied at the end of the procedure. All patients were commenced on prophylactic topical antibiotic following CTA.
Statistical Analysis
IBM® SPSS version 23 for Windows was used to conduct statistical analysis. The normality of data was assessed using histograms and Shapiro–Wilk test. Skewed numerical data were presented as median with interquartile range (IQR), and frequencies with percentages were calculated for categorical variables.
Kaplan–Meier survival curves were plotted to represent CTA success over time. Each CTA application was considered as a case and any subsequent intervention including repeat CTA application was considered as an event. Univariate and multivariable analysis were performed to analyse factors associated with outcome failure. Further, point-biserial analysis was used to determine strength of correlation. Odds ratios (OR) with confidence intervals (CI) were calculated and p-values of less than 0.05 were considered statistically significant.
Results
A total of 25 (12 right and 13 left) eyes of 25 patients were included in this series with a median age of 70 (range 20–93) years. Over half (56.0%; 14) were male. All patients were Caucasian. Demographic and clinical characteristics are described in Table 1.
The causes of corneal perforation were characterised into three groups (Table 2). Non-traumatic sterile corneal melt accounted for more than half of the cases (56.0%; n = 14) of perforation; followed by infection (32.0%; n = 8) and trauma (12.0%; n = 3). Information on original pathologies is summarised under respective cause categories in Table 2.
Amongst cases with underlying bacterial infection, two cases were due to Pseudomonas aeruginosa and one was culture-positive for Haemophilus influenzae. All cases except two had significant OSD (92.0%; n = 23). Dry eye disease (DED) was most common (48.0%; n = 12), followed by neurotrophic keratopathy (24.0%; n = 6), meibomian gland dysfunction (MGD, 20.0%; n = 5), limbal stem cell deficiency (LSCD, 12.0%; n = 3), allergic eye disease (4.0%; n = 1), and exposure keratopathy due to ectropion (4.0%; n = 1).
In the majority of cases, the cornea perforated centrally (56.0%; n = 14). The remaining five (20.0%) were paracentral and four (16.0%) perforated in the peripheral cornea. In two cases site of perforation was not clearly documented. Median diameter of perforation was 2.0 (IQR 1.0–3.0) mm. BCL was inserted in all cases, and it was retained for median 50.0 (IQR 17.8–92.3) days.
Outcome Analysis
Out of 23 eyes that completed follow-up (median 27 months; IQR 9.5–46.5 months) after CTA application, 13 (56.5%) accomplished primary success (Table 3).
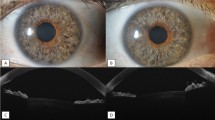
Eight out of remaining ten eyes underwent repeat gluing, of which seven eyes sealed achieving secondary success (n = 20; 86.9%), and only one eye failed, which eventually did seal after third attempt, but it was combined with AMT. Two eyes with primary failure underwent further surgical intervention without repeat gluing. One had AMT, and the other was known as phthisical eye which was eviscerated following failure to seal with single CTA application. The CTA was retained in the eyes for median of 94.0 (IQR 30.0–140.5) days. Survival analysis of total 31 CTA applications (including 8 repeat) showed cumulative success of 80.6% at 30 days post-gluing. It gradually diminished to 71.0% at 90 days, and 51.2% at 250 days (Fig. 1). On further stratifying data, perforations with history of infection observed better long-term CTA survival compared with sterile causes. This trend, however, was statistically not significant (p = 0.13) (Fig. 2).
Central perforations were observed to have higher probability of CTA failure compared with paracentral and peripheral, although the differences were not statistically significant (OR 1.60, CI 0.42–6.60, p = 0.49). Similarly, the size of perforation showed negative correlation to the CTA success, but again the association did not reach statistical significance (rpb = −0.21, p = 0.35). Amongst OSD underlying DED seemed to have the most negative impact on the CTA success, but statistically results remained trivial (OR 1.39, CI 0.27–7.04, p = 0.51). Other variables including age, gender and cause of perforation remained statistically insignificant in regression analysis (Table S1 Supplementary Material).
In total, six eyes underwent further surgical intervention in the form of penetrating keratoplasty (n = 2), AMT (n = 2), and evisceration (n = 2) (Table 3). We observed adverse events in a total of five patients. Two had acute IOP rise in the immediate post-operative period, one eye suffered from microbial keratitis and two eyes developed endophthalmitis.
Discussion
CTA remains an effective method of managing corneal perforations since it was first described in the 1960s by Refojo et al. [19] and Webster et al. [20] Amongst cyanoacrylate derivatives N-butyl-2-cyanoacrylate tissue adhesive is the most suitable due to its optimum polymerization rate and lower toxicity [6]. In addition to tectonic support, CTA is also found to have anti-keratolytic and anti-bacterial properties, mainly against Gram-positive organisms [19, 21, 22]. The latter attribute can be of advantage in patients with active infection when the cornea is melting/impending perforation. However, authors recommend in such setting to aggressively treat the infection first before gluing, as the infective process may get concealed by the opaqueness and inflammation incited by CTA itself. Furthermore, use of BCL following CTA application can promote microbial colonisation, and therefore, increased risk of endophthalmitis.
In our study, sterile non-traumatic corneal perforation was the leading indication for CTA (56.0%; n = 14). This is in contrast to most published studies in which higher proportion of corneal perforations that underwent gluing had an underlying infective aetiology [3, 6, 14, 16, 23]. We postulate that this disparity may be due to lower incidence of infected corneal ulcers in our region compared with referenced studies [24, 25]. Nevertheless, at our tertiary referral centre we have set robust protocols to deal with corneal infections [26]. We have low threshold for admitting patients to a dedicated ophthalmology ward where they receive intensive anti-microbial treatment with daily review. This standardised care may be the reason for lower incidence of corneal perforations due to infective aetiology [27, 28]. For survival outcome analysis, we grouped our cases into infected versus non-infected due to smaller sample size and found better success of CTA in the infected group. Although our results were not statistically significant, a similar trend was observed by Yin et al. [3] as well. Amongst infective aetiology, studies have observed lower success rates of tissue adhesives in herpes-related perforations (37.0%) [17] as compared with that for bacterial keratitis (83.3%) [6] or fungal infections (80.0%) [29]. A recent study by Sing et al. reported overall moderate short-term success of CTA in cases due to infectious keratitis, and often multiple applications are required [30].
OSD is an important contributor to poor healing of corneal wounds and can adversely affect the outcome of any intervention including gluing [2]. Although the differences were not statistically significant, we found that cases with associated predominant DED had lower success rate and long-term CTA survival. Neurotrophic keratopathy affected significant number of our subjects (24.0%; n = 6). Both Acanthamoeba (n = 2) and herpetic keratitis (n = 3) cases developed neurotrophic keratopathy which resulted in corneal thinning in the long-term, and subsequent perforation. Similarly, all three severe chemical injury patients developed limbal stem cell deficiency (LSCD) and their neurotrophic corneas perforated several months post-injury.
Tissue adhesives are usually recommended for small, lesser than 3.0 mm size perforations [2]. In our study, average size of perforation was 2.0 mm which is in line with this recommendation. We had one case with just over 4.0 mm perforation and she failed her first CTA attempt but was successfully sealed on repeat gluing. We did find small but statically insignificant negative correlation between size of perforation and CTA success. Other studies have also highlighted inverse relationship of size of perforation to success rate of tissue adhesives [6, 23]. Location of perforation can also adversely affect the CTA outcome. Although popular recommendation is that CTA works best for central perforations as it can easily dislodge in the peripheral cornea [2], we had a relatively worse success rate for central perforations, and our results seem consistent with Yin et al. [3]. Three out of four cases in our study with perforations in the peripheral cornea achieved successful outcome. This higher success rate could be due to an absence of any case in our study with peripheral ulcerative necrotising keratitis due to autoimmune disease such as rheumatoid arthritis which is considered to have poor outcomes with CTA application alone [31].
We defined success of achieving intact globe as primary and secondary for single and multiple applications, respectively. This definition of success is similar to the previous study by Yin et al. [3] In more than half of our subjects (n = 13; 56.5%) the perforation sealed with a single application of CTA. With repeat application, 86.9% subjects maintained globe integrity. These success rates at 30 days following CTA are significantly higher compared with Yin et al. [3], who reported 39.0% and 61.0% for single and multiple CTA applications, respectively. Similarly, at 90 days our cumulative success was 71.0% compared with 46.0% reported by Yin et al. in their study [3]. Our median CTA retention time (94.0 days) was also substantially higher than Yin et al. [3] series, who reported only 58.0 median days of retention time. These differences may have occurred due to difference in sample sizes of study. Yin et al. [3] had a total of 89 eyes in the perforation group, which is considerably higher than our case series, with only 23 eyes (and 31 CTA applications). Moreover, median size of perforation reported by Yin et al.[3] in their study is 3.19 mm, which is larger compared with ours of 2.0 mm, and hence, could have contributed to their poor overall outcome. Lastly, differences in clinical characteristics of study subjects, such as systemic co-morbidities and causes of perforation, are important factors that cannot be overlooked. Success rates reported by a few other studies are highly variable due to clinical characteristics of perforation, sample size and definition of success itself. Sharma et al. [6] published that single application of CTA was successful in acutely sealing corneal perforation in 68.2% of the eyes. They also reported success rate of 86.4% with multiple CTA applications, which is consistent with our secondary success rate of 86.9% [6]. In contrast, Loya et al. reported much lower success rate of 28.6% following single CTA application [13]. Another two studies found moderate CTA success rates of 44.4% in 80 eyes and 40.9% in 22 eyes [14, 15]. These studies also reported the need for multiple CTA applications, up to 41.3% and 27.3%, respectively [14, 15]. In our study, a total of 8 eyes (34.8%) underwent repeat CTA, of which one eye with rosacea associated sterile melt successfully sealed after third application which was combined with AMT.
CTA is considered to be a temporary measure in restoring globe integrity in the emergency setting, which often delays or completely eliminates the need for corneal transplantation [2]. Our case series showed that CTA application alone can have a long-lasting effect in maintaining water-tight globe, as 17 (73.9%) of the eyes did not require additional tectonic surgical intervention including keratoplasty until last follow-up. Moreover, almost half (46.0%) of the eyes did not require any further intervention for at least a year. This is in contrast with the findings from other studies which have reported that majority of the eyes required additional intervention within 1 month of CTA application [3, 13, 14, 17]. Once again, this disparity in rate of intervention can be attributed to variability in aetiologies, characteristics of perforation and CTA application technique. Nevertheless, long-term efficacy of CTA found in this case series is reassuring, as subsequent elective corneal transplantation under more optimal conditions once inflammation and infection is adequately treated offers higher chances of graft survival [2].
Adverse events following application of CTA are not uncommon [32]. We had two patients who developed elevated IOP next day. One was successfully treated with anti-glaucoma medication, and the other eventually required cyclodiode photocoagulation. Weiss et al. proposed that inflammatory debris blocking the trabecular meshwork may be a possible mechanism for raised IOP in these patients [14]. Another study reported a case of aqueous blockage from 360° iris adhesions around central perforation leading to an acute rise in IOP [33]. Microbial keratitis has been reported following CTA application [11, 14, 34]. One of our patients developed de novo bacterial keratitis post-CTA, caused by Pseudomonas species, which responded well to topical antibiotic therapy. However, there were two eyes which developed endophthalmitis post-CTA. One case was presumed sterile perforation that underwent two successive CTA applications and subsequently developed endophthalmitis within 5 days of presentation. He was managed successfully with intravitreal antibiotics followed by vitrectomy. The other case was an ocular rosacea related perforation that did achieve primary success, but unfortunately was lost to follow-up afterwards and returned to the eye casualty 4 months later with endophthalmitis. Unfortunately, despite aggressive treatment his eye could not be salvaged and was eventually eviscerated. Weiss et al. [14] suggested that due to intrinsic anti-bacterial properties of CTA [21, 22, 35], the culprit was not the tissue adhesive, but the extended wear BCL in the background of severely diseased eyes. In our case series the single BCL remained in the eye for average 50 days after which it was either re-inserted (if lost) or replaced as long as glue was in situ. We could not compare results with other studies as none calculated median time that BCLs were retained in their subjects. Two of our three patients who developed infection did have significantly prolonged duration of BCL in situ despite topical antibiotic prophylaxis. Therefore, we advocate importance of replacing BCL every 4–6 weeks using sterile technique, and closely observing for any early signs of corneal infiltration [36]. Moreover, it is our protocol to send all removed BCL for microbiological culture with sensitivity to identify any potential organisms that may require alteration in antibiotic therapy.
This study suffers the limitations of being retrospective, non-randomised and with a relatively small sample size for any associations to be of statistical importance. One explanation for lower number of cases that underwent gluing in our tertiary referral centre is the indication, as per our protocol, we perform urgent corneal grafting for relatively larger size perforations. Furthermore, the exact time when CTA came off was difficult to determine later in the survival analysis, as some subjects had spontaneous CTA extrusion only to be found on routinely scheduled follow-up visit.
Conclusions
This study confirms that CTA application is very effective in acutely sealing small-to-medium sized corneal perforations (≤ 3.0 mm). We also demonstrated good long-term success of CTA in maintaining globe anatomic integrity, obviating the need for additional tectonic intervention, which when required, is often in the form of corneal transplantation for visual restoration in an eye that is completely settled. Although risk of serious complications is low, all patients require careful monitoring to reduce the risk of sight-threatening secondary infections. More research is required to establish impact of OSD and its type on CTA success. Until synthetic cornea-like materials [37] are readily available commercially, CTA will remain the treatment of choice for sealing corneal perforations acutely.
References
Portnoy SL, Insler MS, Kaufman HE. Surgical management of corneal ulceration and perforation. Surv Ophthalmol. 1989;34(1):47–58.
Jhanji V, Young AL, Mehta JS, Sharma N, Agarwal T, Vajpayee RB. Management of corneal perforation. Surv Ophthalmol. 2011;56(6):522–38.
Yin J, Singh RB, Al Karmi R, Yung A, Yu M, Dana R. Outcomes of cyanoacrylate tissue adhesive application in corneal thinning and perforation. Cornea. 2019;38(6):668–73.
Hugkulstone C. Use of a bandage contact lens in perforating injuries of the cornea. J R Soc Med. 1992;85(6):322.
Rana M, Savant V. A brief review of techniques used to seal corneal perforation using cyanoacrylate tissue adhesive. Cont Lens Anterior Eye. 2013;36(4):156–8.
Sharma A, Kaur R, Kumar S, Gupta P, Pandav S, Patnaik B, et al. Fibrin glue versus N-butyl-2-cyanoacrylate in corneal perforations. Ophthalmology. 2003;110(2):291–8.
Sun Y-C, Kam JP, Shen TT. Modified conjunctival flap as a primary procedure for nontraumatic acute corneal perforation. Tzu-Chi Med J. 2018;30(1):24.
Rodríguez-Ares MT, Touriño R, López-Valladares MJ, Gude F. Multilayer amniotic membrane transplantation in the treatment of corneal perforations. Cornea. 2004;23(6):577–83.
Korah S, Selvin SS, Pradhan ZS, Jacob P, Kuriakose T. Tenons patch graft in the management of large corneal perforations. Cornea. 2016;35(5):696–9.
Hanada K, Igarashi S, Muramatsu O, Yoshida A. Therapeutic keratoplasty for corneal perforation: clinical results and complications. Cornea. 2008;27(2):156–60.
Leahey AB, Gottsch JD, Stark WJ. Clinical experience with N-butyl cyanoacryiate (Nexacryl) tissue adhesive. Ophthalmology. 1993;100(2):173–80.
Bhat YM, Banerjee S, Barth BA, Chauhan SS, Gottlieb KT, Konda V, et al. Tissue adhesives: cyanoacrylate glue and fibrin sealant. Gastrointest Endosc. 2013;78(2):209–15.
Loya-Garcia D, Serna-Ojeda JC, Pedro-Aguilar L, Jimenez-Corona A, Olivo-Payne A, Graue-Hernandez EO. Non-traumatic corneal perforations: aetiology, treatment and outcomes. Br J Ophthalmol. 2017;101(5):634–9.
Weiss JL, Williams P, Lindstrom RL, Doughman DJ. The use of tissue adhesive in corneal perforations. Ophthalmology. 1983;90(6):610–5.
Setlik DE, Seldomridge DL, Adelman RA, Semchyshyn TM, Afshari NA. The effectiveness of isobutyl cyanoacrylate tissue adhesive for the treatment of corneal perforations. Am J Ophthalmol. 2005;140(5):920–1.
Moschos M, Droutsas D, Boussalis P, Tsioulias G. Clinical experience with cyanoacrylate tissue adhesive. Doc Ophthalmol. 1997;93(3):237–45.
Moorthy S, Jhanji V, Constantinou M, Beltz J, Graue-Hernandez EO, Vajpayee RB. Clinical experience with N-butyl cyanoacrylate tissue adhesive in corneal perforations secondary to herpetic keratitis. Cornea. 2010;29(9):971–5.
Kasetsuwan N, Sukharoch P, Meesoupong P, Reinprayoom U, Puangsricharern V, Pariyakanok L. Efficacy and safety of ethyl-2-cyanoacrylate adhesives for corneal gluing. Asian Biomed. 2013;7(3):437–41.
Refojo MF, Dohlman CH, Ahmad B, Carroll JM, Allen JC. Evaluation of adhesives for corneal surgery. Arch Ophthalmol. 1968;80(5):645–56.
Webster RG, Slansky HH, Refojo MF, Boruchoff SA, Dohlman CH. The use of adhesive for the closure of corneal perforations: report of two cases. Arch Ophthalmol. 1968;80(6):705–9.
Romero IL, Malta JB, Silva CB, Mimica LM, Soong KH, Hida RY. Antibacterial properties of cyanoacrylate tissue adhesive: does the polymerization reaction play a role? Indian J Ophthalmol. 2009;57(5):341.
Eiferman RA, Snyder JW. Antibacterial effect of cyanoacrylate glue. Arch Ophthalmol. 1983;101(6):958–60.
Siatiri H, Moghimi S, Malihi M, Khodabande A. Use of sealant (HFG) in corneal perforations. Cornea. 2008;27(9):988–91.
Ung L, Bispo PJ, Shanbhag SS, Gilmore MS, Chodosh J. The persistent dilemma of microbial keratitis: global burden, diagnosis, and antimicrobial resistance. Surv Ophthalmol. 2019;64(3):255–71.
Ting DSJ, Settle C, Morgan SJ, Baylis O, Ghosh S. A 10-year analysis of microbiological profiles of microbial keratitis: the North East England Study. Eye. 2018;32(8):1416–7.
Gnanaraj L, Sandhu S, Hildreth A, Figueiredo F. Postkeratoplasty emergency visits—a review of 100 consecutive visits. Eye. 2007;21(8):1028–32.
Titiyal JS, Negi S, Anand A, Tandon R, Sharma N, Vajpayee RB. Risk factors for perforation in microbial corneal ulcers in north India. Br J Ophthalmol. 2006;90(6):686–9.
McLeod SD, LaBree LD, Tayyanipour R, Flowers CW, Lee PP, McDonnell PJ. The importance of initial management in the treatment of severe infectious corneal ulcers. Ophthalmology. 1995;102(12):1943–8.
Garg P, Gopinathan U, Nutheti R, Rao GN. Clinical experience with N-butyl cyanoacrylate tissue adhesive in fungal keratitis. Cornea. 2003;22(5):405–8.
Singh RB, Zhu S, Yung A, Dohlman TH, Dana R, Yin J. Efficacy of cyanoacrylate tissue adhesive in the management of corneal thinning and perforation due to microbial keratitis. Ocul Surf. 2020;18(4):795–800.
Bernauer W, Ficker LA, Watson PG, Dart JK. The management of corneal perforations associated with rheumatoid arthritis: an analysis of 32 eyes. Ophthalmology. 1995;102(9):1325–37.
Vote BJ, Elder MJ. Cyanoacrylate glue for corneal perforations: a description of a surgical technique and a review of the literature. Clin Experiment Ophthalmol. 2000;28(6):437–42.
Vasquez-Perez A, Matarazzo F, Mandal N, Tuft S. Acute glaucoma following cyanoacrylate glue patch for corneal perforation. J Glaucoma. 2018;27(9):e148–50.
Cavanaugh TB, Gottsch JD. Infectious keratitis and cyanoacrylate adhesive. Am J Ophthalmol. 1991;111(4):466–72.
Lehman RA, West RL, Leonard F. Toxicity of alkyl 2-cyanoacrylates: II. Bacterial growth. Arch Surg. 1966;93(3):447–50.
Baenninger P, Dinah C, Figueiredo F. Survey on bandage contact lens practice in the United Kingdom. J Clin Exp Ophthalmol. 2014;5(325):2.
McTiernan CD, Simpson FC, Haagdorens M, Samarawickrama C, Hunter D, Buznyk O, et al. LiQD Cornea: pro-regeneration collagen mimetics as patches and alternatives to corneal transplantation. Sci Adv. 2020;6(25): eaba2187.
Acknowledgements
Author Contributions
Salman Naveed Sadiq: data collection, analysis and manuscript writing. Cristian Cartes: data collection. Muhammad Numan Sarfraz: manuscript proof reading; referencing. Francisco C Figueiredo: Supervision, study design, data interpretation and manuscript writing.
Funding
No funding or sponsorship was received for this study or publication of this article.
Data Availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
Ethical Approval
This anonymized retrospective study was approved by the Clinical Governance and Audit Department of the Newcastle upon Tyne Hospitals NHS Foundation Trust (Ref: 10323). It was approved by the Caldicott Data Protection Guardian of the Newcastle upon Tyne Hospitals NHS Foundation Trust and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all patients.
Conflict of Interest
Salman Naveed Sadiq, Cristian Cartes and Francisco C Figueiredo have no competing interests. Muhammad Numan Sarfraz’s new affiliation since this study is Kings College Hospital, London, United Kingdom.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sadiq, S.N., Cartes, C., Sarfraz, M.N. et al. Outcomes of N-butyl-2-Cyanoacrylate Tissue Adhesive Application in Corneal Perforation Disorders: Consecutive Case Series. Ophthalmol Ther 12, 3403–3413 (2023). https://doi.org/10.1007/s40123-023-00785-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00785-y