Abstract
Introduction
Hemodialysis (HD) has various effects on the body, including optimizing body fluid composition and volume, which may have an impact on subfoveal choroidal thickness (SCT) in individuals with end-stage kidney disease (ESKD). However, previous studies have produced conflicting results regarding the effect of HD on SCT in patients with ESKD. Therefore, we conducted a meta-analysis to investigate the influence of HD on SCT.
Methods
A comprehensive search of relevant studies and bibliographies was conducted using Embase, PubMed, and Web of Science databases up to September 2022. Weighted mean difference (WMD) and 95% confidence interval (CI) were used to summarize the SCT change. Heterogeneity and publication bias were assessed, and a random-effects model was employed for the meta-analysis. Subgroup analyses were also performed to evaluate the influence of factors such as diabetes mellitus (DM), the severity of diabetic retinopathy (DR), diurnal variation adjustment, optical coherence tomography (OCT) types, and OCT scan modes.
Results
A total of 15 studies involving 1010 eyes were eligible for this meta-analysis, including 552 diabetic eyes, 230 non-diabetic eyes, and the remaining 228 eyes were uncategorized. The meta-analysis revealed a significant reduction in SCT after HD (WMD = −13.66 μm; 95% CI −24.29 to −3.03 μm; z = −5.115, P < 0.0001). Subgroup analysis indicated a significant difference between the DM and non-DM groups (WMD = −24.10 μm vs. −15.37 μm, 95% CI −27.39 to −20.80 μm vs. −19.07 to −11.66 μm; P = 0.001). Additionally, the group with proliferative diabetic retinopathy (PDR) exhibited a more pronounced reduction in SCT (WMD = −28.66 μm; 95% CI −37.10 to −20.23; z = −6.660, P < 0.0001). Adjusting for diurnal variation, different types or scan modes of OCT did not significantly affect the results.
Conclusion
HD leads to a significant decrease in SCT among patients with ESKD, especially in patients with DM with PDR.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
This study aimed to investigate the impact of hemodialysis (HD) on subfoveal choroidal thickness (SCT) and found a significant reduction in SCT after HD, particularly in patients with diabetes mellitus and proliferative diabetic retinopathy (PDR). |
The sub-analysis revealed that diabetes status, diurnal variation, and the optical coherence tomography (OCT) machine type and scan mode may contribute to the observed decrease in heterogeneity. |
This study suggested that the alteration in SCT after HD could potentially establish SCT as a valuable structural biomarker for non-invasive assessment of systemic vascular conditions. |
Introduction
End-stage kidney disease (ESKD) is the final stage of chronic kidney disease and is characterized by the progression of various clinical manifestations such as hypertension, edema, and endocrine disorders. To address these pathological states and optimize body fluid composition and volume, renal replacement therapy such as hemodialysis (HD) is necessary.
HD leads to fluctuations in systemic hemodynamic parameters and often results in a reduction in blood pressure (BP), which is associated with a decrease in body weight and plasma volume [1]. The effect of HD on ocular parameters such as the choroidal blood flow and systemic blood pressure (SBP) has also been reported. Relevant studies indicate that HD may affect parameters such as intraocular pressure, central corneal thickness, central retinal thickness, retinal nerve fiber layer thickness, and choroidal thickness [2].
The choroid is composed of blood vessels, melanocytes, fibroblasts, resident immunocompetent cells, and collagen and elastic connective tissue. It is typically described as consisting of five sublayers: Bruch’s membrane [3], the capillary layer, Halal's layer, Sattler’s layer [4, 5], and the suprachoroidal space. Due to its rich blood supply, the choroid plays a vital role in maintaining the retinal position, eliminating waste products, and secreting growth factors [6]. There is a close relationship between choroidal blood flow and SBP, and circadian variations in choroidal thickness have been linked to changes in SBP [7, 8]. Some studies suggest that choroidal vessels are poorly autoregulated and that perfusion pressure directly affects blood flow, while more recent investigations have shown that choroidal autoregulation can compensate for fluctuations in SBP [9].
Optical coherence tomography (OCT) is a valuable tool for evaluating choroidal lesions [10]. The introduction of swept-source OCT (SS-OCT) and spectral domain OCT (SD-OCT) represents a significant advance in ocular imaging [11,12,13]. These techniques enhance the visualization of ocular structures, leading to more accurate ocular imaging and improved results in the quantitative assessment of choroidal thickness.
The data on choroidal thickness typically rely on data collected through the fovea. The fovea represents the most sensitive position of vision and is supplied by choroidal blood vessels, making it a prime location for detecting changes in choroidal blood flow and vessel structure [14]. To provide a visual representation of this measurement process, a schematic diagram of choroidal thickness measurement is included in Fig. 1.
Representative images of the choroidal layer using swept-source optical coherence tomography. A representative picture of a healthy control (A, C) and a patient with diabetes (B, D). Subfoveal choroidal thickness was measured as the vertical dimension between the hyperreflective band of the retinal pigment epithelium and the choroidal–scleral junction from the subfoveal area of the fovea (C, D). SCT subfoveal choroidal thickness, DM diabetes mellitus
Several previous studies have evaluated the changes in subfoveal choroidal thickness (SCT) induced by HD in patients with ESKD and systemic vascular disease using OCT measurements. Most studies reported a decrease in choroidal thickness after HD; however, Jung et al. reported an increase in choroidal thickness [15]. Given the conflicting results from these studies, the effect of HD on choroidal thickness remains uncertain.
Despite the increasing number of studies on the topic, to our knowledge, no previous meta-analysis has specifically focused on investigating the alterations in choroidal thickness before and after HD. Conducting a meta-analysis can provide comprehensive and robust data to address this research gap, elucidating the range of changes in choroidal thickness following HD. Therefore, in accordance with the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines, we conducted a systematic review and meta-analysis to explore the variations in SCT, as measured by OCT, before and after HD in patients with ESKD.
Methods
Search Strategy and Study Selection
The present meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines in all steps of the study. It was registered in PROSPERO (registration code: CRD42022324799). A systematic literature search was conducted in databases including Embase, PubMed, and Web of Science, and was limited to studies published up to September 2022. The search was conducted using the Medical Subject Headings (MeSH) terms and keywords “Tomography, Optical Coherence,” “Choroid,” “Renal Dialysis,” and “Kidney Failure, Chronic.” The details of the search strategy are listed in the Supplementary Material. In addition, a manual search of the references of eligible studies was performed to reduce the risk of missing relevant papers. After reviewing the titles and abstracts, 22 studies that were written in English, published in peer-reviewed journals, and assessed SCT using OCT measurements were selected for full-text review.
Inclusion and Exclusion Criteria
Studies that met the following criteria were included in this meta-analysis: (1) original human studies with a case–control, cross-sectional, or prospective design; (2) recruitment of patients with ESKD who underwent HD, as well as controls; (3) use of OCT with the measurements reported as the mean and standard deviation (or standard error) for each study group; and (4) diagnosis of patients with ESKD according to established diagnostic systems.
Studies that failed to meet the following exclusion criteria were not included: (1) studies not related to HD or SCT; (2) studies that only performed a single OCT examination; (3) conference abstracts, case reports, comments, or reviews; (3) studies that lacked obtainable data; or (4) non-English records, animal studies, and duplicate articles. In instances where multiple studies were conducted using the same population, the most recent or the most comprehensive study was selected. The screening process was performed independently by two reviewers, and any disagreements were resolved through discussion and consensus.
Quality Assessment
Two independent assessors (ZXS and YMM) evaluated the methodological quality of the included studies using the Methodological Index for Non-Randomized Studies (MINORS) [16]. The MINORS scale evaluates 12 aspects of the original articles and assigns a score of 0 for absence of reporting, 1 for inadequate reporting, and 2 for adequate reporting. Any discrepancies in the results of the quality assessment were resolved through discussion between the assessors. Inter-rater agreement between the two authors was quantified using Cohen's kappa (κ). Cohen's kappa values were interpreted as follows: ≤ 0 indicating no agreement, 0.01–0.20 indicating no to slight agreement, 0.21–0.40 indicating fair agreement, 0.41–0.60 indicating moderate agreement, 0.61–0.80 indicating substantial agreement, and 0.81–1.00 indicating almost perfect agreement [17]. Additionally, the risk of bias was assessed following the guidelines recommended by PRISMA.
Data Extraction
The data from each of the included studies were extracted and evaluated by two independent authors (ZXS and YMM). The following information was extracted from each study: (1) first author name; (2) publication year; (3) study design; (4) origin of study; (5) type of OCT instrument; (6) sample size; (7) sex ratio(male/female); (8) average age; (9) interval between end of dialysis and OCT; (10) dialysis duration; (11) patient status of diabetes mellitus (DM); (12) whether adjusted for diurnal variation; (13) position of SCT; (14) the severity of diabetic retinopathy (DR); (15) previous treatments; (16) utilization of enhanced-depth imaging (EDI) technology; (17) measurement patterns; (18) scan modes; and (19) change in OCT measurements in SCT [mean ± standard deviation (SD), P values]. Disagreements were resolved by consulting a third reviewer or by consensus. If the necessary data could not be obtained, a conversion formula was applied to calculate the SD from the data in the article. The calculation method was in accordance with the Cochrane Handbook for Systematic Reviews of Interventions [18].
Data Synthesis and Statistical Analysis
All meta-analyses and the funnel plots evaluating publication bias were conducted using Stata 16 software (StataCorp, College Station, TX, USA). We synthesized the quantitative data from the OCT measurements of patient SCT before and after HD to calculate the change (mean ± SD) for each study. The level of difference between the two comparison groups was calculated and reported as a weighted mean difference (WMD), standardized mean difference (SMD), and corresponding 95% confidence interval (CI) using the mean and standard deviation. The heterogeneity of the studies was accurately measured using the Higgins I2 test. The choice of effect models was based on the heterogeneity of the included studies, with the random-effects model used if I2 was greater than 50% and P < 0.05; otherwise the fixed-effects model was used. To interpret the cause of heterogeneity, subgroup analysis was conducted according to the study type, OCT model, participant age group, and complication type. If ten or more studies were included in each meta-analysis, the funnel plot and Egger’s test were used to visually and quantitatively explore possible publication biases using Stata. A significance level of P < 0.05 was used for all statistical tests.
Ethics
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Search Results and Study Characteristics
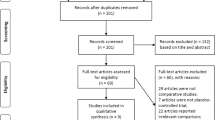
The flowchart of the search procedure is shown in Fig. 2. A total of 903 articles were extracted from three databases, and no further articles were retrieved when reference lists were searched. In all, 816 articles were examined after the removal of duplicates. Based on the titles and abstracts, an additional 794 studies were excluded because they were not related to HD or SCT (n = 729), were reviews (n = 60), or were comments (n = 5). There were 22 full-text articles assessed for eligibility, from which we excluded seven trials based on the following: (1) optical coherence tomography angiography (OCTA) studies (n = 2), (2) only processed OCT once (n = 1), (3) did not provide SCT data (n = 4). Ultimately, a total of 15 articles were included in our study [13, 15, 19,20,21,22,23,24,25,26,27,28,29,30,31], and their characteristics are presented in Table 1. The complementary characteristics of relevant data on DR severity and previous treatments are presented in Supplementary Material Table 1. These studies investigated 655 participants with 1010 eyes and were published between 2012 and 2021. Ten studies used SD-OCT and five studies used SS-OCT to detected the SCT. All participants were from Asian countries. The mean age ranged from 51.2 to 69.4 years. Eleven studies distinguished participants with diabetes, four studies included all kinds of ESKD.
The flowchart of the search procedure. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. https://doi.org/10.1371/journal.pmed1000097. For more information, visit www.prisma-statement.org. OCT optical coherence tomography, HD hemodialysis, OCTA optical coherence tomography angiography
Quality Appraisal
All studies were critically appraised using the MINORS tool (see Table 2). The before–after study in the same patient design means all included studies were noncomparative studies; the maximum score was 16. Scores of at least 12 were considered high quality with low risk for bias; scores between 8 and 12 were considered medium risk for bias; scores of ≤ 8 were considered high risk for bias. Because the experimental design allowed SCT data to be obtained without follow-up, items assessing duration of follow-up and loss of participants on such studies scored 0 points. All studies had MINORS scores ≥ 8 but < 12, with an average of 9.3, indicating medium quality and risk of bias. For the item assessing prospective calculation of study size, scores of 0 points were obtained for all but one study [25]. The calculated Cohen’s kappa was 0.68, indicating a substantial level of agreement between the two assessors. Detailed scoring data are shown in Supplementary Material Tables 2 and 3.
Changes in Subfoveal Choroidal Thickness
Figure 3 shows the meta-analysis of SCT change before and after HD. Two studies divided patients into a DM group and non-DM group; therefore, we collected and included the data respectively [23, 26]. Two studies only included patients with ESKD without DM [25, 29], and one study only included patients with ESKD with DM [22]. In meta-analysis, a random-effects model was used because the heterogeneity (I2 = 99.7%) was substantial. The results showed that SCT after HD was significantly thinner than before HD (WMD = −18.48 μm; 95% CI −25.57 to −11.40; z = −5.115, P < 0.0001). In contrast, SCT was thicker after HD in one study [15]. The other studies revealed thinner SCT after HD, and all studies were significantly different (P < 0.05).
Sub-analysis by Diabetes
Concurrent diabetes may account for a significant source of heterogeneity between studies. Out of the 11 studies analyzed, two groups were formed based on the diabetes status: ESKD with DM and ESKD without DM. The sub-analysis showed that the SCT for the ESKD group with DM was significantly thinner than that in the ESKD group without DM (WMD = −24.10 μm; 95% CI −27.39 to −23.08; z = −14.335, P < 0.0001). Nonetheless, the SCT change before and after HD in the non-DM group also showed a significant difference (WMD = −15.37 μm; 95% CI −19.07 to −11.66; z = −8.129, P < 0.0001), and the between-subgroup analysis demonstrated a significant difference (P = 0.001). Despite the lower heterogeneity in this sub-analysis, it was still substantial (I2 = 80.3% of DM; I2 = 79.6% of non-DM), so a random-effects model was used (see Fig. 4).
Sub-analysis by Diabetic Retinopathy Severity
To investigate the impact of DM and DR on SCT changes, we performed further subgroup analysis in nine studies. Two studies were excluded due to a lack of explicit exclusion of proliferative diabetic retinopathy (PDR). Among the remaining studies, four were categorized into the PDR group, while the other three were classified into the non-proliferative diabetic retinopathy (NPDR) group. The sub-analysis revealed that the PDR group exhibited more pronounced reduction in SCT (WMD = −28.66 μm; 95% CI −37.10 to −20.23; z = −6.660, P < 0.0001), while the NPDR group showed a similar reduction as the non-DM group (WMD = −19.47 μm; 95% CI −24.99 to −13.96; z = −6.917, P < 0.0001). Although the between-subgroup analysis was not significant (P = 0.074), the non-DM group and the PDR group were significantly different (P = 0.005) (see Supplementary Material Fig. 1). Despite the lower heterogeneity in this sub-analysis, it remained substantial (I2 = 89.0% of PDR; I2 = 57.4% of NPDR), so a random-effects model was used (see Fig. 5).
Sub-analysis by Diurnal Variation Adjustment
Diurnal variation is a known factor that may affect the SCT, and its adjustment was also a factor contributing to heterogeneity in our results. Five studies adjusted for diurnal variation. The sub-analysis based on adjustment for diurnal variation showed that the changes in SCT were similar (WMD = −17.25 μm vs. −15.65 μm, 95% CI −21.04 to −13.45 vs. −26.12 to −5.19, z = −8.914, P = 0.013 vs. z = −2.932, P < 0.0001), and the between-subgroup analysis revealed no significant difference (P = 0.779). The heterogeneity was lower but still significant after adjusting for diurnal variation (68.4% vs. 99.8%), and therefore the random-effects model was used (see Supplementary Material Fig. 2).
Sub-analysis by Optical Coherence Tomography Machine Types
Different OCT machine types may also be a significant source of heterogeneity between studies. Nine studies used SD-OCT and five studies used SS-OCT. For the studies that divided patients into DM and non-DM groups, only the non-DM group was included to further reduce the heterogeneity. The sub-analysis was performed in two groups depending on the OCT machine type. The result showed that SCT changes were similar between the SD-OCT and SS-OCT groups (WMD = −16.63 μm vs. −14.59 μm, 95% CI −25.46 to −7.79 vs. −20.19 to −8.99, z = −3.688, P < 0.0001 vs. z = −5.109, P < 0.0001), and the between-subgroup heterogeneity was not significant (P = 0.703). The heterogeneity was lower but still higher than 50% (I2 = 99.8% of SD-OCT; I2 = 62.9% of SS-OCT), and therefore, the random-effects model was used in the sub-analysis (see Supplementary Material Fig. 3).
Sub-analysis by Optical Coherence Tomography Scan Modes
The selection of choroidal thickness scan modes, specifically single B-scan or macular scan, is a methodological consideration based on varying laser penetration intensity and OCT device specifications. Among the included studies, four studies utilized the more advanced SS-OCT technology and employed the macular scan model. Among the remaining 11 studies that employed SD-OCT, four utilized the macular scan mode, five employed the single B-scan mode, and two did not specify the scanning mode used. Sub-analysis based on single B-scan and macular scan indicated similar changes in SCT (WMD = −16.76 μm vs. −19.41 μm, 95% CI −20.02 to −13.05 vs. −27.56 to −11.26, z = −10.071, P < 0.0001 vs. z = −4.668, P < 0.0001), and the between-subgroup analysis showed no significant difference (P = 0.554). The heterogeneity was lower but still significant after adjusting for diurnal variation (78.1% vs. 97.2%), and therefore the random-effects model was used (see Supplementary Material Fig. 4).
Publication Bias
Funnel plots were generated to assess the potential publication bias of the literature (see Supplementary Material Fig. 5). However, the placement of the data points revealed asymmetry. Therefore, we grouped the points by DM and non-DM, and the new funnel plots did not reveal any obvious evidence of asymmetry (see Fig. 6). In addition, quantitative analyses calculated using Egger’s test (P = 0.407) showed no clear evidence of publication bias (see Supplementary Material Fig. 6).
Discussion
This meta-analysis presents a comprehensive assessment and elucidates the range of changes in SCT after HD in patients with ESKD. The study includes a total of 15 self-controlled case series, including 655 participants with 1010 eyes. The results demonstrate a significant decrease in SCT after HD, especially in patients with DM with PDR. Furthermore, the sub-analysis reveals that adjusting for diurnal variation, utilizing different types of OCT, or employing various scan modes did not yield substantial differences in the observed SCT changes. Regarding previous treatments, surgical procedures such as vitrectomy and intravitreal injections were consistently excluded in all studies, and retinal laser photocoagulation was mostly excluded as well. Therefore, we did not analyze previous treatment as a separate subgroup. Previous studies have been restricted by limited sample sizes and high fluctuations in SCT, leading to uncertainty in the results. This meta-analysis addresses these limitations by including a sizable patient cohort, enhancing the reliability and persuasiveness of the assessment. Moreover, the analysis has employed a valid instrument, MINORS, which is designed for non-randomized surgical studies, to evaluate the included studies, making the findings more reliable.
The choroid is a thin and dense network of blood vessels situated between the retina and sclera. It has the highest blood flow per unit weight of any body tissue, which means that SCT is closely related to BP and body weight. Also, changes in the microvasculature of the choroid may indicate systemic diseases affecting blood vessels [32]. In addition, choroidal vessels have specific extrinsic autonomic modulations. Two hypotheses have been proposed to explain the regulatory mechanism of the choroid: the myogenic theory and the neuronal component theory. The myogenic mechanism is the response of arteriolar smooth muscle to stretch through changes in perfusion pressure, while neuronal components include sympathetic vasoconstriction for hypertension or parasympathetic vasodilation for hypotension [33, 34]. HD is a treatment that can correct excessive accumulation and abnormal distribution of body fluids. After a single HD treatment, significant changes in systemic hemodynamic parameters can occur, such as an increase in plasma colloid osmotic pressure and transcapillary colloid osmotic pressure gradient, and a decrease in plasma volume, interstitial fluid volume, and body weight [1]. Consequently, the influence of HD on systemic hemodynamic parameters and the special structure of the choroid may explain the changes in SCT after dialysis.
The more pronounced decline in SCT observed in patients with diabetes after dialysis can be attributed to the disruption of the choroidal vasculature [35]. The disturbance of the blood–retinal inner barrier is an early event in the progression of DR, histologically manifested by an increase in vascular tortuosity, microaneurysm formation, areas of non-perfusion, lumen dilation or narrowing, and choroidal neovascularization [36]. Furthermore, studies have indicated that an increase in subfoveal choroidal vascular resistance in diabetic eyes, as detected by laser Doppler flowmetry, is linked to a decrease in choroidal blood flow [37]. These circumstances may lead to impaired equilibrium of hydrostatic pressure and colloid osmotic pressure inside and outside the choroidal vessels in patients with diabetes, resulting in increased vascular resistance. Therefore, these pathophysiological modifications in the choroidal vasculature may impact the choroidal structure, inducing alterations in the choroidal intravascular and extravascular compartments. This may be the underlying cause for the greater fluctuations in SCT observed in patients with diabeteswith PDR.
Previous studies observed a significant diurnal variation in SCT in normal subjects, with a relative peak thickness early in the morning and progressive decrease during the day to a relative nadir at 17:00 [7]. Nevertheless, certain studies have indicated that measurement differences between SS-OCT and SD-OCT become noticeable when the choroid is thicker, and the accuracy of SD-OCT for SCT measurement decreases significantly [38]. These differences may be the reason for the lower degree of heterogeneity in the adjusted diurnal variation group and the SS-OCT group in the subgroup analysis.
However, the study has several limitations that must be acknowledged. Firstly, the primary analysis exhibited significant heterogeneity, likely attributed to differences in DM status, DR severity, OCT instruments, measurement points, duration of dialysis, and patient characteristics. We conducted sub-analysis, but the heterogeneity still could not be resolved completely. The effect of DR severity and previous treatment situation in these patients, which could not be excluded completely, is also a limitation of the study. Secondly, only published studies were included, and the analysis did not present clear evidence of publication bias, indicating potential bias. Finally, the included studies lacked follow-up data on adverse complications after dialysis, which precluded the analysis of the correlation between SCT and adverse events or the prognosis of patients with ESKD.
Conclusions
In conclusion, the change in SCT after HD possibly relates to the vascular status of patients and systemic hemodynamics, establishing SCT as an essential structural biomarker for noninvasive observable systemic vascular conditions. Advances in OCT technology have enabled effective visualization and quantitative analysis of the choroid, providing technical support for this goal. However, the heterogeneity in the primary analysis and lack of follow-up data require further studies to validate these findings.
References
Leypoldt JK, et al. Relationship between volume status and blood pressure during chronic hemodialysis. Kidney Int. 2002;61(1):266–75.
Azem N, et al. Effect of hemodialysis on retinal thickness in patients with diabetic retinopathy, with and without macular edema using optical coherence tomography. J Ophthalmol. 2014;2014: 709862.
Bhutto I, Lutty G. Understanding age-related macular degeneration (AMD): relationships between the photoreceptor/retinal pigment epithelium/Bruch’s membrane/choriocapillaris complex. Mol Aspects Med. 2012;33(4):295–317.
Li XQ, et al. Enhanced-depth imaging optical coherence tomography of the human choroid in vivo compared with histology after enucleation. Invest Ophthalmol Vis Sci. 2016;57(9):371–6.
Mrejen S, Spaide RF. Optical coherence tomography: imaging of the choroid and beyond. Surv Ophthalmol. 2013;58(5):387–429.
Parver LM. Temperature modulating action of choroidal blood flow. Eye. 1991;5(2):181–5.
Tan CS, et al. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53(1):261–6.
Usui S, et al. Circadian changes in subfoveal choroidal thickness and the relationship with circulatory factors in healthy subjects. Invest Ophthalmol Vis Sci. 2012;53(4):2300–7.
Reiner A, et al. Choroidal blood flow compensation in rats for arterial blood pressure decreases is neuronal nitric oxide-dependent but compensation for arterial blood pressure increases is not. Exp Eye Res. 2010;90(6):734–41.
Benavente-Pérez A, et al. Reproducibility-repeatability of choroidal thickness calculation using optical coherence tomography. Optom Vis Sci. 2010;87(11):867–72.
Agawa T, et al. Choroidal thickness measurement in healthy Japanese subjects by three-dimensional high-penetration optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2011;249(10):1485–92.
Yamashita T, et al. Repeatability and reproducibility of subfoveal choroidal thickness in normal eyes of Japanese using different SD-OCT devices. Invest Ophthalmol Vis Sci. 2012;53(3):1102–7.
Shin YU, et al. Optical coherence tomography angiography analysis of changes in the retina and the choroid after haemodialysis. Sci Rep. 2018;8(1):17184.
Manjunath V, et al. Choroidal thickness in normal eyes measured using Cirrus HD optical coherence tomography. Am J Ophthalmol. 2010;150(3):329.e1.
Jung JW, et al. Changes in subfoveal choroidal thickness and choroidal extravascular density by spectral domain optical coherence tomography after haemodialysis: a pilot study. Br J Ophthalmol. 2014;98(2):207–12.
Slim K, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6.
McHugh ML. Interrater reliability: the kappa statistic. Biochemia Medica. 2012;22(3):276–82.
Cumpston M, et al. Updated guidance for trusted systematic reviews a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10:ED000142.
Chang IB, Lee JH, Kim JS. Changes in choroidal thickness in and outside the macula after hemodialysis in patients with end-stage renal disease. Retina. 2017;37(5):896–905.
Chen H, Zhang X, Shen X. Ocular changes during hemodialysis in patients with end-stage renal disease. BMC Ophthalmol. 2018;18(1):208.
Elbay A, et al. Are the effects of hemodialysis on ocular parameters similar during and after a hemodialysis session? Arq Bras Oftalmol. 2017;80(5):290–5.
Hwang H, et al. Changes in optical coherence tomography findings in patients with chronic renal failure undergoing dialysis for the first time. Retina. 2019;39(12):2360–8.
Ishibazawa A, et al. Choroidal thickness evaluation before and after hemodialysis in patients with and without diabetes. Invest Ophthalmol Vis Sci. 2015;56(11):6534–41.
Lee WJ, et al. Effect of hemodialysis on peripapillary choroidal thickness measured by swept-source optical coherence tomography. J Glaucoma. 2021;30(6):459–64.
Mayali H, et al. Multimodal ocular evaluation in hemodialysis patients. Int Ophthalmol. 2021;41(5):1799–805.
Nakano H, et al. Choroid structure analysis following initiation of hemodialysis by using swept-source optical coherence tomography in patients with and without diabetes. PLoS ONE. 2020;15(9): e0239072.
Shin YU, et al. Evaluation of changes in choroidal thickness and the choroidal vascularity index after hemodialysis in patients with end-stage renal disease by using swept-source optical coherence tomography. Medicine (Baltimore). 2019;98(18): e15421.
Sun G, et al. The effect of hemodialysis on ocular changes in patients with the end-stage renal disease. Ren Fail. 2019;41(1):629–35.
Ulaş F, et al. Evaluation of choroidal and retinal thickness measurements using optical coherence tomography in non-diabetic haemodialysis patients. Int Ophthalmol. 2013;33(5):533–9.
Yang SJ, et al. Changes of choroidal thickness, intraocular pressure and other optical coherence tomographic parameters after haemodialysis. Clin Exp Optom. 2013;96(5):494–9.
Zhang Y, et al. Changes in retina and choroid after haemodialysis assessed using optical coherence tomography angiography. Clin Exp Optom. 2018;101(5):674–9.
Yeung SC, et al. Choroidal thickness in patients with cardiovascular disease: a review. Surv Ophthalmol. 2020;65(4):473–86.
Kiel JW. Choroidal myogenic autoregulation and intraocular pressure. Exp Eye Res. 1994;58(5):529–43.
Kolb B, Rotella DL, Stauss HM. Frequency response characteristics of cerebral blood flow autoregulation in rats. Am J Physiol Heart Circ Physiol. 2007;292(1):H432–8.
Takamura Y, et al. Functional and anatomical changes in diabetic macular edema after hemodialysis initiation: one-year follow-up multicenter study. Sci Rep. 2020;10(1):7788.
Xu J, et al. Subfoveal choroidal thickness in diabetes and diabetic retinopathy. Ophthalmology. 2013;120(10):2023–8.
Nagaoka T, et al. Alteration of choroidal circulation in the foveal region in patients with type 2 diabetes. Br J Ophthalmol. 2004;88(8):1060–3.
Lee M-W, et al. Comparison of choroidal thickness measurements using swept source and spectral domain optical coherence tomography in pachychoroid diseases. PLoS ONE. 2020;15(2): e0229134.
Acknowledgements
The authors thank all members of the Department of Ophthalmology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology for their critical comments on this manuscript.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Concept and design: Zixuan Su, Xinghua Wang and Fagang Jiang. Acquisition, analysis, or interpretation of data: Zixuan Su, Yamin Mao, Zhiyi Qi, Meng Xie, Banghuan Hu, Xinghua Wang and Fagang Jiang. Drafting of the manuscript: Zixuan Su, Yamin Mao, Zhiyi Qi. Critical revision of the manuscript for important intellectual content: Zixuan Su, Yamin Mao, Zhiyi Qi, Meng Xie, Banghuan Hu, Xinghua Wang and Fagang Jiang. Statistical analysis: Zixuan Su and Xueqing Liang. Administrative, technical, or material support: Xinghua Wang and Fagang Jiang. Supervision: Xinghua Wang and Fagang Jiang. All authors participated in final approval of the article and agreed to be accountable for all aspects of the work.
Disclosures
Zixuan Su, Yamin Mao, Zhiyi Qi, Meng Xie, Xueqing Liang, Banghuan Hu, Xinghua Wang, and Fagang Jiang declare no conflicts of interest.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Su, Z., Mao, Y., Qi, Z. et al. Impact of Hemodialysis on Subfoveal Choroidal Thickness Measured by Optical Coherence Tomography: A Systematic Review and a Pooled Analysis of Self-Controlled Case Series. Ophthalmol Ther 12, 2265–2280 (2023). https://doi.org/10.1007/s40123-023-00761-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00761-6