Abstract
Introduction
The aim of the study was to determine the effect of oral isotretinoin therapy on the functional and morphological condition of the anterior segment of the eye, with particular emphasis on the meibomian glands.
Methods
Twenty-four patients (48 eyes) with a diagnosis of acne vulgaris were involved in the survey. All patients underwent a thorough ophthalmological examination at three time points: before therapy, 3 months after the start of therapy, and 1 month after the completion of isotretinoin therapy. The physical examination included the following elements: blink rate, analysis of the lid margin abnormality score (LAS), tear film break-up time (TFBUT) and Schirmer’s test, meibomian gland loss (MGL), and the evaluation of the meibum quality score (MQS) and meibum expressibility score (MES). Additionally, the total score of an ocular surface disease index (OSDI) questionnaire was analysed.
Results
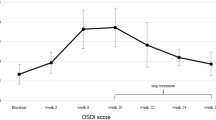
In comparison with pretreatment values, significant increases in OSDI during and after the treatment (p = 0.003 and p = 0.004, respectively) were observed. Substantial deterioration during the treatment was observed for MGL (p < 0.0001), MQS (p < 0.001) and LAS (p < 0.0001), while an improvement in those parameters after isotretinoin cessation was observed (p = 0.006, p = 0.02 and p = 0.0003, respectively). The frequency of using artificial eye drops was positively associated with MGL during (Spearman’s rank correlation coefficient (Rs) = + 0.31; p = 0.03) and after the cessation of the therapy (Rs = + 0.28; p = 0.04). Meibomian gland atrophy correlated significantly with MQS during (Rs = + 0.29; p = 0.04) and after treatment (Rs = + 0.38; p = 0.008). The decrease in TFBUT values correlated with increased LAS (Rs = − 0.31; p = 0.03) during the course of isotretinoin usage. We found no changes in Schirmer's test or blink rates.
Conclusion
Isotretinoin therapy leads to increased ocular complaints related to lipid tear film component dysfunction. This is due to reversible changes in meibomian gland morphology and function observed during drug usage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Isotretinoin is currently the most effective drug for treating refractory acne vulgaris. However, dry eye symptoms might be a cause of drug withdrawal prior to completion of the treatment course. |
There is some evidence that changes in the lipid layer of the tear film occur during isotretinoin usage, but the mechanism or dynamics of those changes, as well as their reversibility after drug cessation, remain unknown. |
The present study aimed to investigate the effect of oral isotretinoin therapy on both functional and morphological changes in the anterior segment of the eye, with particular emphasis on the meibomian glands. |
What was learned from the study? |
This study showed that isotretinoin usage is associated with increased ocular complaints in terms of dry eye related to substantial changes in the quality of a lipid tear film component secondary to meibomian gland dysfunction. |
In patients with acne vulgaris, meibomian gland dysfunction seems to be reversible in the post-cessation period. |
Introduction
Acne is a chronic inflammatory disease associated with overactive sebaceous glands. It affects all age groups but is most common and most severe during adolescence. Common acne occurs all over the world and is the eighth most common skin disease worldwide [1, 2]. This disease is characterized by the presence of comedones accompanied by inflammation and papules, pustules, inflammatory nodules, tumours and cysts. The lesions are located in the seborrheic areas of the face, back and chest. Postinflammatory discolouration is observed in approximately 58% of patients with acne lesions and in 54% of even scars, including a small percentage of hypertrophic and keloid scars [1].
Treatment protocols depend on the severity of skin lesions. Isotretinoin is currently the most effective drug in the treatment of acne lesions that are resistant to other acne medications. Used at the right time, it reduces the extent of changes and complications in the form of acne scars. This drug affects all mechanisms of the formation of acne lesions. It reduces the secretion of sebum and the size of the sebaceous glands by as much as 90% and normalizes the keratinization processes in the ducts of the sebaceous glands. It decreases the number of Propionibacterium acnes bacteria by reducing the nutrients for these bacteria, and it reduces the chemotaxis of neutrophils, thus diminishing the inflammatory symptoms. Moreover, in approximately 50% of patients, it reduces the melanin content in the skin, thus confining the formation of postinflammatory discolourations and limiting the action of skin metalloproteinases, reducing acne scarring [2].
Side effects include dryness of both the skin and the mucous membranes, sometimes with itching. This can lead to inflammatory changes in the skin and mucous membranes, sometimes with bleeding from the nose, vagina or anus. A very common symptom of dry skin and mucous membranes is inflammation of the cheilitis and eyelids and eczema-like skin lesions. These side effects are known as retinoid dermatitis [1, 3]. During treatment with isotretinoin, mild increases in liver enzymes, creatine phosphokinase, cholesterol and triglyceride levels and sometimes slight anaemia might also be observed. Depression, concentration disorders, bone and joint pain, muscle pain and headaches may also appear. Temporary hair loss may occur in 13% of patients. These symptoms are temporary and disappear after treatment cessation [3]. Hypersensitivity to the sun's rays during treatment was also reported. Isotretinoin is teratogenic; therefore, in women, it is advisable to use double contraception 1 month before treatment and to maintain it up to 2 months after treatment [2]. The most common ocular symptoms include dry eye and decreased function of the meibomian glands (MGs), blepharitis and conjunctivitis. Single cases of corneal ulceration, photosensitivity, and disturbances in vision and colour perception have also been reported [3, 4].
To the best of our knowledge, no study has comprehensively analysed the influence of isotretinoin systemic therapy on dry eye symptoms and MG dysfunction until now. Thus, we designed a prospective interventional study to evaluate ocular surface and MG characteristics in patients with diagnosed acne vulgaris undergoing isotretinoin therapy during and after treatment at precisely selected time points, and to compare them with the baseline values. We also correlated our findings with self-reported ocular symptoms. Furthermore, this is the first study investigating the relationship between MG morphology and function in individuals with acne vulgaris receiving isotretinoin derivatives as long as 1 month after drug cessation.
Methods
Twenty-four patients (i.e. 48 eyes) recruited at the Dermatology Outpatient Clinic were included in the study. The inclusion criteria were as follows: a moderate to advanced stage of acne vulgaris, no significant improvement in acne treatment with local and systemic antibiotic therapy, normal liver transaminase [aspartate transaminase (AST) and alanine transaminase (ALT)] levels, normal cholesterol and triglyceride levels (TG), and no proven liver disease. Subjects were excluded from the study if they exhibited any active infection of the eye or active ocular allergy, had any evidence of lid deformity or abnormal lid movement disorder, had undergone eye surgery within 1 year of the study visit, or were contact lens users. Written informed consent was obtained from all subjects before examination. The study was approved by the Institutional Review Board of Pomeranian Medical University and adhered to the tenets of the Declaration of Helsinki.
Isotretinoin was started at low doses (0.5–1.0 mg/kg per day) and sustained until the threshold dose, 120–150 mg/kg. The treatment duration varied from 24 to 32 weeks with a mean of 28 weeks. To estimate the potential effect of isotretinoin therapy on dry eye disease, we assessed ocular surface parameters before isotretinoin implementation, 3 months after treatment initiation and 1 month after discontinuation of therapy.
To evaluate both self-reported ocular symptoms and lifestyle factors with a potential influence on ocular surface disorders, a detailed medical history was taken. Consequently, a trained physician collected the necessary information including the standardized ocular surface disease index (OSDI) and systemic medical history data (e.g. hypertension, diabetes mellitus, ischaemic heart disease, thyroid disease, current medication usage). Accordingly, several lifestyle factors were established (e.g. cigarette smoking, frequency of using a computer, predominantly indoor or outdoor occupational activity). Additionally, the frequency of artificial eye drop usage was graded as follows: grade 0, never; grade 1, occasionally (once a week); grade 2, frequently (almost every day); and grade 3, constantly (more than once a day).
The eye examination was performed sequentially as follows: slit lamp examination (including fluorescein staining of the ocular surface), tear film break-up time (TFBUT) testing, nonanaesthetized Schirmer's test, quantification of morphologic lid features, examination of meibum expressibility and quality, and meibography. TFBUT was evaluated by placing a single fluorescein strip over the inferior tear meniscus after instilling one drop of normal saline [5]. The time from the last blink to the first appearance of a randomly distributed dry spot on the cornea was measured in seconds. The mean time for three attempts was recorded. Schirmer's test was performed without topical anaesthesia by placing a standard paper strip in the mid-lateral portion of the lower fornix. The amount of wetting was recorded after 5 min. Patients were asked to keep their eyes closed during the test. Lid margin abnormality scores (LASs) were 0 (absent) or 1 (present) for the following parameters: narrowed MG orifices, plugged MG orifices, posterior displacement of the orifices, lid margin telangiectasia, posterior lid margin hyperaemia, rounding of the posterior margin, notching of the lid margin, eyelash loss, and trichiasis. Subsequently, the LAS was calculated according to the number of these abnormalities present in each eye. The meibum quality score (MQS) was graded as proposed by Tomlinson et al. [6]. Briefly, to assess obstruction of the MG orifices, digital pressure was applied to the lower tarsus, and the quality of meibum was scored semiquantitatively in eight central glands as follows: grade 0, clear fluid; grade 1, cloudy fluid; grade 2, cloudy particulate fluid; and grade 3, inspissated, such as toothpaste. Accordingly, the meibum expressibility score (MES) was graded as follows: grade 0, all glands expressible; grade 1, 3–4 glands expressible; grade 2, 1–2 glands expressible; and grade 3, no glands expressible. Meibography was performed using a BG-4 M Non-Contact Meibography System (Topcon Corp, Tokyo, Japan). The MG tissue loss, considered as a percentage of the total upper eyelid area (meibomian gland loss, MGL; %), was calculated using ImageJ software.
Statistical Analysis
Statistical analysis was performed using Statistica version 13.3 (TIBCO Software Inc., California, USA) software. The distribution of variables was tested using the Shapiro–Wilk test. To determine the dynamics of changes between baseline and follow-up points, the Mann–Whitney U test for the comparison of two groups of nonparametric variables was performed. Additionally, Fisher’s exact test for qualitative variables was implemented. To assess the correlation between variables, Spearman’s rank correlation coefficients (Rs) were used. The statistical power of the study at the 0.05 significance level with 24 subjects was sufficient to detect with 95% probability the real effect size corresponding to the minimal difference in OSDI between the consecutive time points equal to ± 2 SD [7, 8]. A p value below 0.05 was considered significant. Since most variables presented strong deviations from a normal distribution, data are presented as the median and interquartile range.
Results
Clinical Characteristics of the Study Group
Overall, 48 eyes of 24 consecutive patients (12 males, 12 females) with acne vulgaris who had been subjected to isotretinoin therapy were recruited for the study. The mean age of the subjects was 27.04 years (ranging from 16 to 47 years). None of the participants had a history of diabetes, 1 participant (4.16%) suffered from heart disease, and 6 (16.6%) had thyroid disease. Seven participants were using contraceptive drugs (29.16%), 2 participants were taking antidepressants (8.33%), and 2 were using systemic antiallergic drugs (8.33%). All patients were questioned regarding their working environment: most of them declared that they worked indoors with air conditioning (41.66%), 8 participants (33.33%) worked mainly indoors without air conditioning, and only 2 participants (8.33%) stayed outdoors for most of the day. In the study group, 12.5% of the participants were nicotine users.
Evaluation of Dry Eye Symptoms and Tear Film Parameters
First, we focused on evaluating self-reported dry eye symptoms and tear film characteristics in study subjects (Table 1). We observed a significant increase in the ocular symptom scores 3 months after treatment initiation and 1 month after discontinuation of the therapy compared to the baseline values (p = 0.003 and p = 0.004, respectively). Interestingly, we found that patients were more likely to use artificial tear drops during isotretinoin therapy than before treatment initiation (median = 0% before treatment and median = 1.5% during the treatment; p = 0.001).
Regarding Schirmer's values, we found no differences between the first, second and last follow-up points. Similarly, no differences were found in blink rates between time points. These results may indicate that isotretinoin therapy does not affect the overall tear film amount. In contrast, the tear film break-up time (TFBUT) was significantly shorter 1 month after drug discontinuation compared to the values recorded during the treatment (p = 0.003). However, the during-treatment and posttreatment results did not notably diverge compared to the baseline values.
Assessment of MG Characteristics
According to the available data, isotretinoin may induce meibomian gland disease (MGD). Therefore, analysis of the MG characteristics was performed. The key signs of MGD include MGL, altered MG secretion, and changes in lid morphology. Table 2 presents the MG parameters obtained at three follow-up time points. A significant increase in MGL was observed during the treatment compared to baseline values (p < 0.001). Interestingly, in the follow-up analysis, a statistically significant reduction in this value was demonstrated after the completion of treatment (p < 0.001). However, the MGL exceeded the pretreatment level (p < 0.001). It is worth mentioning that the frequency of using artificial eye drops was positively associated with MGL before (Rs = + 0.29; p = 0.04), during (Rs = + 0.31; p = 0.03) and after (Rs = + 0.28; p = 0.04) the cessation of therapy .
Similar dynamics of changes were observed regarding the parameter describing the quality of MG secretions. A significant deterioration of MQS during treatment compared to baseline values was shown (p < 0.001), and an improvement of this parameter after the end of therapy was noted (p < 0.001). However, this value did not return to the pretreatment level (p < 0.001). With regard to the patency of the MGs, a significant decrease in the values of MES was observed by the end of the therapy compared to the initial values (p = 0.01). Importantly, we also noted a positive relationship between MES and MQS at the second and third follow-up examinations (Rs = + 0.32; p = 0.02 and Rs = + 0.47; p < 0.001, respectively). Moreover, the value of MGL significantly correlated with reduced quality of glandular secretions during (Rs = + 0.29; p = 0.04) and after (Rs = + 0.38; p = 0.008) the treatment. Therefore, these results strongly emphasize the relationship between morphological changes represented by MGL and temporarily impaired function of the MGs during isotretinoin treatment in acne vulgaris.
In the next part of the statistical analysis, we focused on evaluating lid margin alterations. We observed an increase in LAS values at the second follow-up examination compared to the pretreatment state (p < 0.0001). Most importantly, we noticed the transiency of those alterations, since LAS values were remarkably lower after cessation of the therapy compared to those noted in the course of the treatment. Interestingly, we noticed that MGL and MQS positively correlated with lid margin alterations during isotretinoin therapy (Rs = + 0.51; p = 0.004 and Rs = + 0.39; p = 0.005, respectively). It is worth mentioning that lower TFBUT values were associated with higher lid margin alterations during isotretinoin treatment (Rs = – 0.31; p = 0.03). Accordingly, blink rate presented a strong positive correlation with LAS before (Rs = 0.3; p = 0.03) and during (Rs = 0.39; p = 0.006) isotretinoin treatment.
Discussion
It has been widely accepted that adverse effects secondary to isotretinoin include dry eye syndrome and MG changes. However, there are still some significant gaps in our understanding of the extent to which therapy is responsible for ocular surface deterioration. Thus, it is important to determine the dynamics of these changes and answer the question of whether they are persistent or transient.
One of the first reports of retinoic acid derivative treatment for acne was published in 1983 by Kanigsberg and DesGroseilliers [9]. The authors observed that in a group of 28 patients who completed a 16-week treatment course, 33% presented dry eye syndrome changes. Two years later, Fraunfelder et al. [10] analysed a group of 261 patients who received isotretinoin and documented that adverse ocular effects occurred in 237 participants, including blepharoconjunctivitis, subjective complaints of dry eyes, blurred vision, contact lens intolerance, and photodermatitis. All presented reactions were reversible. Similarly, both Caglar et al. [11] and Düzgün et al. [12] documented a significant increase in the average OSDI score during the follow-up (ranging from 1.5 to 6 months). The authors did not conduct the examination after drug cessation; thus, we cannot be certain if the reported alterations were persistent. On the other hand, Eser et al. [13] declared no changes in OSDI both 1 and 3 months after the beginning of the treatment. Again the authors did not manage to provide any follow-up after drug cessation. Interestingly, preclinical studies in a mouse model revealed a decreased number of goblet cells in the conjunctiva exposed to this treatment [14]. Consequently, the complex mechanism of tear film instability and exaggerated evaporation can cause symptoms of dry eye disease. Consistent with cited reports, we observed an increased prevalence of dry eye symptoms 3 months after the beginning of isotretinoin therapy. Interestingly, patients treated with this drug were more likely to use moisturizing eye drops during their treatment. Nonetheless, in our study, OSDI scores remained higher after treatment discontinuation than at baseline.
A reliable assessment of the eye surface condition cannot be taken without blink rate, Schirmer's test or TFBUT measurements. In our study, none of these parameters changed during or after therapy compared to pretreatment values. Several reports support our observations in terms of Schirmer’s test [11,12,13, 15,16,17,18]. On the other hand, Polat et al. [18] demonstrated a statistically significant difference in Schirmer's values between measurements before and at the end of the treatment. However, the treatment duration was not standardized in the study sample and varied from 4 to 7 months. As a result, drawing any conclusions might be misleading. Nonetheless, considering previous reports and our findings, we suppose that isotretinoin does not affect the overall tear film amount.
It is widely known that in terms of a complex tear film analysis with particular emphasis on lipids, the TFBUT is recommended. We observed that the TFBUT was significantly shorter 1 month after drug discontinuation than during treatment. In accordance, Yildirim et al. [19] conducted an extensive follow-up schedule, including three time points during the treatment: 1, 3 and 6 months from receiving the first dose of the drug, as well as 6 months after the completion of the therapy. Consequently, the authors found that TFBUT values decreased notably during the treatment. Similarly, other reports documented decreasing values of TFBUT as early as 1 month after treatment initiation, which lasted for 6 months during therapy [17, 20]. Interestingly, Tanriverdi et al. [7] emphasized that TFBUT reached its lowest values 3 months after the beginning of drug usage.
Due to available data that suggest that isotretinoin may induce MGD [21,22,23], a quantitative and qualitative characterization of MG changes throughout the duration of the study was performed. We found that systemic isotretinoin was accompanied by a significant increase in MGL 3 months from the beginning of the treatment. Remarkably, in the follow-up analysis, a statistically significant increase in this value was demonstrated after the completion of the treatment. Accordingly, Mathers et al. [16] conducted a study on 11 patients treated with isotretinoin and observed a significant loss of MG density and tissue atrophy. Unfortunately, the investigation was not performed after the end of the therapy. In contrast, another group of researchers, Moy et al. [8], did not perceive any morphological changes in MGs in imaging studies. Unfortunately, the lack of follow-up in the posttreatment time in both study designs makes it impossible to draw any conclusions in terms of process reversibility. It is important to mention that the correlation between structural and functional changes defined as MQS assessment was not provided by the authors [17]. In contrast, in our study, a detailed analysis of MG function was performed, and a similar pattern of changes was observed with regard to MQS.
Eventually, we found a positive correlation between MQS and MGL. These data are consistent with our previous observations based on a rosacea population [24]. Similarly, in acne vulgaris samples, Düzgün et al. [12] observed a deterioration in functional MG parameters presenting as cloudiness of the meibum and a decreased amount of excretion 4 months from the beginning of the therapy. Interestingly, they found a positive correlation between MQS and both LAS and MG damage in meibography. This highlighted that morphological and functional assessments were complementary in complex examinations in this group of patients. Additionally, our findings robustly indicate that presented MG morphological and functional deviations are a part of a strictly defined process rather than random fluctuations. Therefore, it is reasonable to assume that MGs might have the ability to induce the self-regeneration process. However, neither the whole mechanism nor the initiating factors are clearly understood. It is also important to determine whether our observations of MG changes are due to actual atrophy or a transient loss of function. It was proven that the course of MGD occurs gradually, and eventual acinar atrophy represents an advanced stage of the disease [25]. Referring to the current guidelines, acne treatment should last from 6 to 8 months. At that time, glands are exposed to the negative influence of the drug. Apparently, the exposure time is too short to leave any persistent changes in MG function and morphology. Furthermore, it can be concluded that both MGD and MGL may be reversible up to a point. Further evidence is needed to establish the dose amount or the period of time that would constitute a certain safe limit.
The LAS reflects the degree of advancement of abnormalities in the eyelid margin, with particular emphasis placed on changes secondary to MG insufficiency. In our study, a significant increase in lid pathologies during isotretinoin treatment in comparison with baseline conditions was observed. Importantly, a notable reduction in this parameter after the discontinuation of the drug was determined, suggesting reversibility and resolution of those features. Similarly, Düzgün et al. [12] reported a significant increase in LAS in the 4th month of isotretinoin treatment. However, no further follow-up was performed, thus preventing an evaluation of the impact of treatment cessation on lid margins. In contrast, Tanriverdi et al. [7] reported a continuous increase in LAS both during the isotretinoin course and 12 months after the completion of the treatment. Although the authors performed a detailed analysis of the dynamics of changes over the treatment period and after its withdrawal, only lid margin telangiectasia, posterior lid margin hyperaemia and irregularity of the lid margin were evaluated. The inconsistency of LAS components and their grading system reported in the literature makes a proper comparative analysis of consecutive studies less feasible. It is worth highlighting that in this study, a standardized evaluation of nine lid margin features was implemented, providing robust practical information on lid margin conditions. Nonetheless, all authors agreed that LAS increases significantly during the course of therapy in isotretinoin users. Accordingly, LAS seems to be a clinically powerful tool not only for differentiating between MG dysfunction and healthy subjects but also in disease progression and treatment monitoring [26].
Since the clinical perspective sometimes seems ambiguous, laboratory investigations at the cellular level should be taken into consideration. Accordingly, Ding et al. [23] treated immortalized human MG epithelial cells with varying doses of 13-cis retinoid acid and found that it significantly decreased MG cellular activity even a few hours after exposure by altering epithelial cell gene expression, reducing cell survival mediators, inhibiting cell proliferation, and eventually increasing cell death. The additional mechanism for isotretinoin’s impact on MGs is downregulation of a gene of peroxisome proliferator-activated receptor γ (PPARγ), which is engaged in the process of sebaceous gland differentiation and lipid metabolism [14]. This receptor was detected in both skin and lids, as well as in lacrimal glands.
Although the authors put effort into providing data with high internal and external validity, a few aspects of this report might rise some concerns. Firstly, the follow-up measurements were taken exclusively at one time point during the treatment (at the third month after isotretinoin commencement), and once after drug cessation. It is worth highlighting that several authors observed both structural and functional changes in the MGs as a result of the isotretinoin therapy precisely at the 3-month follow-up visit [8, 13, 17]. Importantly, Tanriverdi et al. [7] noted that the deterioration of the lipid tear film component reaches its lowest level 3 months after isotretinoin initiation and subsequently improves. On the other hand, only a limited number of papers evaluated variations in the ocular surface condition after isotretinoin cessation. Accordingly, Tanriverdi et al. [7] performed long-term observations with examinations during the 6th and 12th month after the completion of the isotretinoin therapy. Therefore, there is a substantial gap in the detection of an early phase of this process. Consequently, the selection of a follow-up visit during the first month after drug termination might be complementary to previous reports [7]. In light of the discussion above, the selection of the follow-up points in this study seems to provide optimized sensitivity for the detection of ocular surface changes in patients treated with isotretinoin, along with high adherence of the subjects to the study protocol. Secondly, no comparison with a control group was performed in this study. Although the acne vulgaris might cause ocular surface abnormalities, both disease stage and implemented treatment might have modifying effects on the eye condition [1,2,3]. In light of the above, the inclusion of these healthy subjects as well as patients undergoing different treatment modalities or treatment-naive patients in this study might have created misleading outcomes. In order to perform the analysis of the dynamics of changes in the ocular surface parameters during and after drug cessation, a longitudinal study design was selected.
Conclusion
In conclusion, we have presented evidence that systemic therapy with a retinoid derivative is an independent risk factor for dysfunction and atrophy of the MG in patients with acne vulgaris. Interestingly, the statistical analysis carried out in the follow-up study unambiguously showed that the side effects induced by isotretinoin started to subside. Nonetheless, the precise mechanism of the MG regeneration process has not yet been discovered. Our findings clarify the clinical knowledge about the course of changes during and after isotretinoin treatment. Furthermore, we hope that this report will open the discussion regarding possible regeneration processes, which could be vital for patients suffering from MGD.
References
Oon HH, Wong SN, Wee DCAW, Cheong WK, Goh CL, Tan HH. Acne management guidelines by the Dermatological Society of Singapore. J Clin Aesthet Dermatol. 2019;12(7):34–50.
Lynn D, Umari T, Dellavalle R, Dunnick C. The epidemiology of acne vulgaris in late adolescence. Adolesc Health Med Ther. 2016;7:13–25.
Fraunfelder FW. Ocular side effects associated with isotretinoin. Drugs Today. 2004;40(1):23–7.
Rosen E, Raz J, Segev F. Giant cobblestone-like papillae during isotretinoin therapy. Ocul Immunol Inflamm. 2009;17(5):312–3.
DEWS. The definition and classification of dry eye disease: report of the definition and classification of the Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):75–92.
Tomlinson A, Bron AJ, Korb DR, Amano S, Paugh JR, Ian Pearce E, et al. The International Workshop on Meibomian Gland Dysfunction: report of the diagnosis subcommittee. Investig Ophthalmol Vis Sci. 2011;52(4):2006–49.
Tanriverdi C, Nurozler Tabakci B, Donmez S. Longitudinal assessment of meibomian glands and tear film layer in systemic isotretinoin treatment. Eur J Ophthalmol. 2022;32(2):885–93.
Moy A, McNamara NA, Lin MC. Effects of isotretinoin on meibomian glands. Optom Vis Sci. 2015;92(9):925–30.
Kanigsberg N, DesGroseilliers JP. Use of 13-cis-retinoic acid in cystic acne. Can Med Assoc J. 1983;129(3):224 (228).
Fraunfelder FT, LaBraico JM, Meyer SM. Adverse ocular reactions possibly associated with isotretinoin. Am J Ophthalmol. 1985;100(4):534–7.
Caglar C, Senel E, Sabancilar E, Durmus M. Reduced ocular surface disease index (OSDI) scores in patients with isotretinoin treatment. Int Ophthalmol. 2017;37(1):197–202.
Düzgün E, Özkur E. The effect of oral isotretinoin therapy on meibomian gland morphology and dry eye tests. J Dermatolog Treat. 2022;33(2):762–8.
Acar Eser N, Kocabeyoğlu S, Atakan N, Irkec M. The effects of the systemic isotretinoin treatment on ocular surface and meibomian glands: a prospective longitudinal study. Cutan Ocul Toxicol. 2022;41(2):155–61.
Zhang P, Tian L, Bao J, Li S, Li A, Wen Y, et al. Isotretinoin impairs the secretory function of meibomian gland via the PPARγ signaling pathway. Investig Ophthalmol Vis Sci. 2022;63(3):29.
Bozkurt B, Irkeç MT, Atakan N, Orhan M, Geyik PÖ. Lacrimal function and ocular complications in patients treated with systemic isotretinoin. Eur J Ophthalmol. 2002;12(3):173–6.
Mathers WD, Shields WJ, Sachdev MS, Petroll WM, Jester JV. Meibomian gland morphology and tear osmolarity: changes with Accutane therapy. Cornea. 1991;10(4):286–90.
Gurlevik U, Kemeriz F, Yasar E. The effect of isotretinoin on meibomian glands in eyes: a pilot study. Int Ophthalmol. 2022;42(7):2071–8.
Polat M, Kükner Ş. The effect of oral isotretinoin on visual contrast sensitivity and amount of lacrimation in patients with acne vulgaris. Cutan Ocul Toxicol. 2017;36(1):35–8.
Yildirim Y, Olcucu O, Agca A, Alagoz C, Demircan A, Basci A, et al. Evaluation of corneal topography and biomechanical parameters after use of systemic isotretinoin in acne vulgaris. J Ophthalmol. 2014;701361.
Karalezli A, Borazan M, Altinors DD, Dursun R, Kiyici H, Akova YA. Conjunctival impression cytology, ocular surface, and tear-film changes in patients treated with systemic isotretinoin. Cornea. 2009;28(1):46–50.
Knop E, Knop N, Millar T, Obata H, Sullivan DA. The International Workshop on Meibomian Gland Dysfunction: Report of the Subcommittee on Anatomy, Physiology, and Pathophysiology of the Meibomian Gland. Investig Ophthalmol Vis Sci. 2011;52(4):1938–78.
Schaumberg DA, Nichols JJ, Papas EB, Tong L, Uchino M, Nichols KK. The International Workshop on Meibomian Gland Dysfunction: Report of the Subcommittee on the Epidemiology of, and Associated Risk Factors for, MGD. Investig Ophthalmol Vis Sci. 2011;52(4):1994–2005.
Ding J, Kam WR, Dieckow J, Sullivan DA. The influence of 13-cis retinoic acid on human meibomian gland epithelial cells. Investig Ophthalmol Vis Sci. 2013;54(6):4341–50.
Machalińska A, Zakrzewska A, Markowska A, Safranow K, Wiszniewska B, Parafiniuk M, Machaliński B. Morphological and functional evaluation of meibomian gland dysfunction in rosacea patients. Curr Eye Res. 2016;41(8):1029–34.
Machalińska A, Zakrzewska A, Safranow K, Wiszniewska B, MacHaliński B. Risk factors and symptoms of meibomian gland loss in a healthy population. J Ophthalmol. 2016;7526120.
Arita R, Itoh K, Maeda S, Maeda K, Furuta A, Fukuoka S, et al. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology. 2009;116(11):2058–64.
Acknowledgements
Funding
No funding or sponsorship was received for this study or the publication of this article. The journal’s Rapid Service fee was funded by the authors.
Author Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Aleksandra Zakrzewska, Sylwia Słuczanowska-Głąbowska and Anna Machalińska. The analysis was performed by Aleksandra Zakrzewska, Krzysztof Safranow, Marta P. Wiącek and Anna Machalińska. The manuscript was written by Aleksandra Zakrzewska, Marta P. Wiącek and Anna Machalińska.
Disclosures
Aleksandra Zakrzewska, Marta P. Wiącek, Sylwia Słuczanowska-Głąbowska, Krzysztof Safranow and Anna Machalińska declare that they have no competing interests.
Compliance with Ethics Guidelines
Ethical review and approval was obtained from the institutional review board, no. KB-0012/61/13. The authors confirm that the study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All subjects provided informed consent to participate in the study and for the publication of any identifying information included in the manuscript.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zakrzewska, A., Wiącek, M.P., Słuczanowska-Głąbowska, S. et al. The Effect of Oral Isotretinoin Therapy on Meibomian Gland Characteristics in Patients with Acne Vulgaris. Ophthalmol Ther 12, 2187–2197 (2023). https://doi.org/10.1007/s40123-023-00737-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00737-6