Abstract
Introduction
Myopia prevalence among adolescents is increasing annually. While orthokeratology (OK) is effective for controlling myopia progression, it may also be detrimental. We investigated tear film parameters [including tear mucin 5AC (MUC5AC) concentration] in children and adolescents with myopia treated with spectacles or OK compared with those with emmetropia.
Methods
This prospective case–control study enrolled children (aged 8–12 years; 29 and 39 with myopia treated with OK and spectacles, respectively, and 25 with emmetropia) and adolescents (aged 13–18 years; 38 and 30 with myopia treated with OK and spectacles, respectively, and 18 with emmetropia). We recorded the ocular surface disease index (OSDI), visual analog scale (VAS) score, tear meniscus height (TMH), noninvasive tear breakup time (NIBUT), meibomian gland score (meiboscore), ocular redness score, and tear MUC5AC concentration in the emmetropia, spectacle (after 12 months of spectacle wearing), and OK (baseline, and after 1-, 3-, 6-, and 12-month use) groups. We observed changes from baseline to 12 months in the OK group and compared parameters among the spectacle, 12-month OK, and emmetropia groups.
Results
The 12-month OK group differed significantly from the spectacle and emmetropia groups in most indicators among children and adolescents (P < 0.05). Differences were not noticeable between the spectacle and emmetropia groups (only PVAS < 0.05 among the children). In the OK group, the 12-month NIBUT was significantly decreased (P < 0.05) in both age groups; the upper meiboscore was increased at 6 and 12 months (both P < 0.05) among children; ocular redness scores were higher at 12 months than at baseline (P = 0.007), 1 month (P < 0.001), and 3 months (P = 0.007) among children; and the MUC5AC concentration was decreased at 6 and 12 months among adolescents, but only at 12 months among children (all P < 0.05).
Conclusions
Long-term OK can negatively influence the tear film in children and adolescents. Moreover, changes are masked by spectacle wearing.
Trial Registration
This trial is registered with “ChiCTR2100049384.”
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? | |
Myopia incidence rate among adolescents is increasing globally every year and the condition is estimated to reach nearly 5 billion people by 2050, indicating a severe visual health concern. | |
Research on the safety of orthokeratology, believed to be an effective method for controlling myopia progression, has gradually become a hot topic, but there has been no research exploring the changes in tear mucin during the orthokeratology treatment process. | |
This study aimed to evaluate the changes in tear film indicators and tear mucin 5AC (MUC5AC) mucin after 1 year of orthokeratology treatment to deepen the understanding of the safety of this treatment. | |
What was learned from the study? | |
Compared with wearing spectacles, ocular health in children and adolescents undergoing long-term orthokeratology treatment may be more affected. Timely detection of ocular indicators is conducive to improving treatment safety. | |
Changes in various tear film indicators provide us with insights for designing treatment schemes to improve tear film stability in children and adolescents and reduce the incidence of dry eyes. |
Introduction
The annual incidence of myopia in adolescents has increased [1]. Several studies have indicated that Chinese students have a high myopia rate, indicating a severe visual health concern [2, 3]. Orthokeratology (OK) is an effective method for controlling myopia progression [4,5,6]. The treatment process involves the use of rigid contact lenses with an inverse geometric design, thereby altering corneal morphology, which can improve naked-eye vision and retard myopia progression [7, 8]. Many studies from China and abroad have strongly affirmed the efficacy of OK, but some have found that, after OK use, some adolescents experience discomfort, corneal staining [9], or even meibomian gland atrophy [10]. This suggests that OK use may damage the ocular surface in adolescents. A study showed that the incidence of dry eyes among adolescents with myopia is as high as 18.95%, which is lower than that in adults; however, it is difficult to diagnose exactly because of the low expression of eye discomfort symptoms, poor coordination, and higher prevalence of allergic conjunctivitis among adolescents [11,12,13].
Although research on the safety of OK has garnered significant attention of late, no studies have explored the changes in tear mucin during the OK treatment process. Thus, in the present study, we used Keratograph 5 M to analyze the ocular surfaces of children and adolescents. MUC5AC is a mucin produced by the conjunctival goblet cells. As one of the main components of the tear film, MUC5AC is involved in maintaining tear film stability [14]. We measured the tear MUC5AC concentration to reflect the degree of damage to the conjunctival goblet cells indirectly. We compared the tear film indicators among children and adolescents who wore spectacles for 12 months, had used OK for 12 months, or had emmetropia. We also recorded indicators at baseline and after 1-, 3-, 6-, and 12 months of OK use in the OK group to explore the influence on the tear film and tear MUC5AC concentration in children and adolescents.
Methods
Participants
This prospective study recruited children aged 8–12 years and adolescents aged 13–18 years from the Second Affiliated Hospital of Anhui Medical University. The study protocol strictly followed the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the Second Affiliated Hospital of Anhui Medical University [YX2021-053(F2)]. Informed consent was obtained from the parents of all participants before enrollment. This study was registered at ChiCTR.org.cn (no. ChiCTR2100049384).
The inclusion criteria for the myopia group (i.e., the OK and spectacle groups) were best corrected visual acuity ≤ 0.0 (LogMAR) and spherical refraction: −0.50 D to −6.00 D, astigmatic power ≤ −2.00 DC. In the spectacle group, children and adolescents had to meet the requirement of 1 year of use. In the emmetropia group, the participants were required to have a spherical refraction range of −0.25 D to +0.50 D and uncorrected visual acuity ≤ 0.0 (LogMAR). Exclusion criteria were as follows: ocular diseases, such as keratopathy, glaucoma, and cataract; a history of eye trauma, eye surgery, or ocular medication (including tear substitute); systemic diseases; and a history of using OK or other types of contact lenses.
We examined and recorded the baseline indicators of the tear film of the patients in the emmetropia, OK, and spectacle groups. In the OK group, the following indicators were evaluated at baseline and after 1, 3, 6, and 12 months of treatment: ocular surface disease index (OSDI), visual analog scale (VAS) scores, and Keratograph 5 M examination [tear meniscus height (TMH), noninvasive tear breakup time (NIBUT), meibomian gland scores (Meiboscore), ocular redness score, and MUC5AC concentration]. For MUC5AC concentration, tears were extracted from the right eye of each patient 2 h after the completion of other examinations to minimize their influence on tear MUC5AC concentration. The concentration was measured using an enzyme-linked immunosorbent assay. Each participant was examined in the same consulting room at a temperature of 22 °C, humidity of 50–60%, and brightness of 300–400 Lx.
Outcome Measures
OSDI Questionnaire
The OSDI was developed at the International Dry Eye Workshop to assess the severity of ocular surface disease. This 12-item questionnaire evaluates 12 symptoms. The total score on the OSDI questionnaire is 100 points, and a score greater than 12 is considered positive [15].
VAS Scale
The VAS is the most commonly used method for pain assessment. This study used VAS to rate seven symptoms: burning sensation, itching, foreign body sensation, blurred vision, dry eyes, photophobia, and pain. Each symptom was rated from 0 to 10, with 0 representing “no discomfort,” 1–3 representing “mild discomfort,” 4–6 representing “moderate discomfort,” 7–9 representing “severe discomfort,” and 10 representing “excruciating discomfort.” The total score was 70. All patients were supervised by the same experienced clinician.
TMH
The patient focused on a red dot in the center of the analyzer and photographed with infrared light directly in front of their eyes.
NIBUT
We measured the first NIBUT [NIBUT(f)], defined as the time from eye opening to the first tear film breakup on the ocular surface, and the average NIBUT [NIBUT (av)], defined as the average time of tear film breakup over the entire measurement period.
Meiboscore
Meiboscores were graded using the following criteria: grade 0, intact meibomian glands; grade 1, < 1/3 meibomian gland loss; grade 2, meibomian gland loss between 1/3 and 2/3; and grade 3, > 2/3 meibomian gland loss.
Ocular Redness
Each patient was instructed to expose their bulbar conjunctiva fully after blinking. Ocular redness was analyzed using software for the temporal bulbar conjunctiva, temporal corneoscleral margin, nasal corneoscleral margin, and nasal bulbar. The average value of conjunctival hyperemia (ocular redness) was automatically calculated.
Tear Extraction and Determination of MUC5AC Concentration
Without administering surface anesthesia, 60 μL of phosphate-buffered saline was slowly dripped into the inferior fornix, and the eyes were gently moved to mix this with the tear fluid content. Approximately 30 μL of the mixture was collected from each conjunctival sac near the lateral canthus, using a micropipette [16]. The mixture was placed in a 1.5-mL Eppendorf tube and immediately stored at −80 °C until use. The MUC5AC concentration was measured using a specific MUC5AC ELISA kit (Jiangsu Enzyme Immunity Company, Yancheng, China), as per the manufacturer’s instructions. The lower limit of detection was 1 ng/mL.
Statistical Analysis
All statistical analyses were performed using SPSS v24.0 (IBM SPSS Inc., Armonk, NY, USA). Pearson’s χ2 test was used for categorical variables. The results are presented as the mean ± standard deviation (SD) for continuous variables. The Kolmogorov–Smirnov (K–S) test was used to evaluate the normality of distribution of continuous variables. Mann–Whitney U and Kruskal–Wallis H tests were used to compare non-normally distributed data. The Friedman test of multiple related samples was used to compare data at different timepoints in the OK group. The test level was α = 0.05, and P < 0.05 was considered statistically significant. When there were differences among multiple groups, the significance level of pairwise comparisons was adjusted using the Bonferroni correction.
Results
Figure 1 shows the management flowchart of the cases. A total of 179 participants (89 males and 99 females) were screened in the study from February 2021 to August 2021 at the Ophthalmology Clinic of the Second Affiliated Hospital of Anhui Medical University. In the child group, there were 29 participants enrolled in the OK group, 39 participants enrolled in the spectacle group, and 25 participants enrolled in the emmetropia group. In the adolescent group, there were 38 participants enrolled in the OK group, 30 participants enrolled in the spectacle group, and 18 participants enrolled in the emmetropia group. No significant differences in sex or age were observed among the three groups (all P > 0.05). No significant difference was observed in the mean spherical equivalent between the OK and spectacle groups (P > 0.05). The basic information of the children and adolescent groups are presented in Tables 1 and 2.
OSDI Score
Significant differences were not noted in the OSDI scores among the three groups of children (χ2 = 1.899, P = 0.387) and adolescents (χ2 = 5.079, P = 0.079). No significant difference was observed in the OSDI scores at any timepoint in the OK group among either age group (child group χ2 = 0.937, P = 0.919; adolescent group: χ2 = 1.568, P = 0.814) (Tables 3, 4, 5, 6).
VAS Score
A significant difference was detected in the VAS scores among the three groups of children (χ2 = 8.562, P = 0.014), but none was observed in the adolescents (χ2 = 1.577, P = 0.455). In the child group, the VAS scores of the spectacle group were higher than that of the emmetropia group (P = 0.012). No significant difference was observed between the other pairwise comparisons (P > 0.05). Further analysis of the VAS questionnaire of children showed that the scores of blurred visions in the OK (P = 0.015) and spectacle (P < 0.001) groups were higher than that in the emmetropia group (Table 7). No significant difference was observed in VAS scores at any timepoint in the OK group of both age groups (child group χ2 = 3.026, P = 0.553; adolescent group: χ2 = 6.708, P = 0.152) (Tables 3, 4, 5, 6).
TMH
No significant difference was observed in TMH among the three groups (child group: χ2 = 1.067, P = 0.587; adolescent group: χ2 = 1.738, P = 0.419). No significant difference was observed in TMH at any timepoint in the OK group (child group: χ2 = 5.207, P = 0.267; adolescent group: χ2 = 6.130, P = 0.19) (Tables 3, 4, 5, 6).
NIBUT
No significant difference was observed in the NIBUT (f) among the three groups in both age groups (child group: χ2 = 3.714; P = 0.156; adolescent group: χ2 = 1.865, P = 0.393); however, there was a significant difference in NIBUT (av) among the three groups in both children and adolescents (child group: χ2 = 6.916; P = 0.031; adolescent group: χ2 = 8.618, P = 0.013). In the child group, the NIBUT (av) of the OK group after 12 months of use was lower than that of the spectacle group (P = 0.046). In the adolescent group, the NIBUT (av) of the OK group after 12 months of use was lower than that of the emmetropia group (P = 0.013). No significant difference was observed in the NIBUT (av) between the other pairwise comparisons (P > 0.05). In the OK group of children, the NIBUT(f) at 12 months was significantly lower than that at 3 months (P = 0.048), and the NIBUT (av) at 12 months was significantly lower than that at baseline (P = 0.005). In the OK group of adolescents, the NIBUT(f) at 12 months was significantly lower than that at 1 month (P = 0.001) and at 3 months (P = 0.023). The NIBUT (av) at 12 months was significantly lower than that at baseline (P = 0.035) and 1 month (P < 0.001). The NIBUT(f) and the NIBUT (av) at other timepoints showed no significant change (P > 0.05) (Tables 3, 4, 5, 6 and Figs. 2, 3).
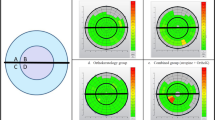
Meibomian Gland Analysis
There was a significant difference in the upper meibomian gland scores among the three groups in both age groups (child group: χ2 = 32.492; P < 0.001; adolescent group: χ2 = 28.128, P < 0.001). The scores of the OK group among children and adolescents after 12 months of use were both higher than those of the spectacle group (both P < 0.001) and the emmetropia group (both P < 0.001), and no significant difference was observed between the other two groups (P > 0.05). In the OK group of children, the scores at 12 months were significantly higher than those at baseline (P < 0.001), 1 month (P < 0.001), and 3 months (P < 0.001), but not at 6 months (P > 0.05). Moreover, the scores at 6 months were significantly higher than those at baseline (P = 0.001) and 1 month (P = 0.003). There was no significant change at the other timepoints as compared with the time before use (P > 0.05). In the OK group of adolescents, there was an upward trend in the upper meibomian gland scores over time (χ2 = 62.018; P < 0.001), however, no significant difference was observed at different timepoints (P > 0.05) (Tables 3, 4, 5, 6 and Fig. 4a).
A significant difference was detected in the lower meibomian gland scores among the three groups of adolescents χ2 = 7.761, P = 0.021), but was not observed in children (χ2 = 4.420, P = 0.11). In adolescents, the scores of the OK group with 12-month use were higher than those of the emmetropia group (P = 0.02), and no significant differences were observed between the other two groups (P > 0.05). In the OK group of children and adolescents, there was an upward trend in the lower meibomian gland scores over time (child group:χ2 = 32.057; P < 0.001; adolescent group: χ2 = 45.333, P < 0.001), but significant difference was not observed at different timepoints (all P > 0.05) (Tables 3, 4, 5, 6 and Fig. 4b).
Ocular Redness Score
There was a significant difference in the ocular redness scores among the three groups of children (χ2 = 9.395, P = 0.009), but no significant difference was observed in the adolescents (χ2 = 1.466, P = 0.48). The scores of the OK group after 12–month use were higher than that of the spectacle (P = 0.043) and emmetropia groups (P = 0.014) among children. No significant difference was observed in the other pairwise comparisons (P > 0.05). In the OK group of children, the scores at 12 months were significantly higher than those at baseline (P = 0.007), 1 month (P < 0.001), and 3 months (P = 0.007). There was no significant change at the other timepoints as compared with the time before use (P > 0.05) (Tables 3, 4, 5, 6 and Fig. 5).
MUC5AC Concentration
There was a significant difference in the MUC5AC concentration among the three groups of children (χ2 = 9.850, P = 0.007) and adolescents (χ2 = 8.748, P = 0.013). In the children, the MUC5AC concentration in the OK group with 12-month use was lower than that in the spectacle group (P = 0.03) and the emmetropia group (P = 0.013), and in the adolescents, the MUC5AC concentration in the OK group with 12-month use was lower than that in the emmetropia group (P = 0.024). No significant differences were observed between the other pairwise comparisons (P > 0.05). In the OK group of children, the MUC5AC concentration at 12 months was significantly lower than that at baseline (P = 0.004) and 1 month (P = 0.021). In the OK group of adolescents, the MUC5AC concentration at 12 months was significantly lower than that at baseline (P < 0.001), 1 month (P = 0.001), and 3 months (P = 0.002), and the concentration at 6 months was significantly lower than that at baseline (P = 0.014), but not at the other timepoints (all P > 0.05) (Tables 3, 4, 5, 6 and Fig. 6).
Adverse Events
All participants in the OK group had good compliance in completing the insertion and removal of OK lenses. There was no keratitis or corneal ulceration during the whole follow-up. However, some children and adolescents had mild corneal staining that could be fully recovered approximately 1–2 days after ceasing OK lens wearing. For such cases, the measurements were taken 2 days later.
Discussion
The prevalence of myopia is increasing annually among adolescents worldwide, which may be caused by a decrease in outdoor activities and an increase in near work [17]. Spectacles and OK are common correction methods for myopia in adolescents. Spectacles are convenient but cannot control myopia, whereas OK can both correct and control myopia progression [6]. As the use of OK has become increasingly widespread, its safety has received increasing attention. Rojas-Carabali et al. [18] reported that, among 60 adolescents using OK, 44.7% had thinner lipid layers, 70.8% had positive conjunctival lissamine green staining, 47.4% had positive corneal fluorescein staining, and 36.64% had partial meibomian gland loss, suggesting that ocular surface problems in adolescents using OK should not be ignored. There is a difference in the time spent on near work between primary school and middle school students: local middle school students aged 13–18 years would have more time for self-study at night than primary school students aged 8–12 years, accounting for about 3 h. Our study divided participants aged 8–18 years into a child group and an adolescent group to observe the change in trend in tear film indicators in these age groups.
The OSDI questionnaire can be used to evaluate the severity of dry eye in adolescents [19]. The VAS scale can also be used to evaluate subjective feelings such as ocular surface discomfort. In the children and adolescent groups, pairwise comparisons indicated that the OSDI scores of the OK group were not significantly different from those of the other two groups. However, in the child group, our study showed that the VAS scores in the spectacle group were slightly higher than those in the emmetropia group. Through further analysis of each symptom score in the VAS questionnaire, we found that “blurred vision” scored higher in the OK and spectacle groups than in the emmetropia group, and was more significant in the spectacle group. In other words, participants with myopia might be more likely to have eyesight fluctuations and blurred vision than participants with emmetropia, which may be related to the fact that participants with myopia use more accommodation. However, in the adolescent group, no significant difference was observed in VAS scores in the pairwise comparisons. Therefore, we speculated about the likelihood of such a difference. Firstly, the ocular axial length of children changed quickly [20], and vision would be blurred by glasses with inappropriate degree or high wear. Secondly, children’s tolerance is lower than that of adolescents, which might result in amplification of discomfort scores. Furthermore, children are younger and less cognitively able, which could increase the possibility of recall bias. Additionally, the OK groups of both age groups exhibited no significant changes in OSDI and VAS scores at any timepoint. Wang et al. [21] reported that OSDI scores for ocular discomfort increased with the OK use at 6 months and declined at 12 months. However, Na et al. [10] observed that OSDI scores increased significantly when the OK lens was worn for 24 months and 36 months, but not at 12 months, which is consistent with our results. The study conducted by Yang et al. [22] reported similar results that no significant changes were found in OSDI scores during a 1-year follow-up.
The Keratograph 5 M can be used for objective and noninvasive evaluation of the tear film of patients, increasing their comfort and improving their degree of cooperation. In the two age groups, no significant difference was observed in the TMH among the three groups, and the change in TMH at any timepoint in the OK group was not significant. Xie et al. [23] and Yang et al. [22] also reported that overnight OK had no significant effect on the TMH.
No significant difference was observed in the NIBUT (f) among the three groups of children and adolescents. In the children, the NIBUT (av) of the OK group after 12–month use was significantly lower than that of the spectacle group. Interestingly, in the adolescents, the NIBUT (av) of the OK group after 12–month use was significantly lower than that of the emmetropia group. In the OK group in both age groups, the NIBUT (f) and NIBUT (av) after 12 months were significantly lower than before, suggesting that OK indeed reduced tear film stability, which was similar to the research findings of Yang et al. [22] and Li et al. [24]
Several studies speculated that the cause of tear film instability could be related to changes to meibomian gland function and tear mucins [16, 22]. In this study, the upper meibomian gland scores in the OK group after 12 months among children and adolescents were both significantly higher than those of the spectacle and emmetropia groups. The lower meibomian gland scores in the OK group after 12 months, only among adolescents, were higher than those of the emmetropia groups. Further analysis of the change in trend within the OK group showed that the upper meibomian gland scores of children at 6 months and 12 months were higher than at baseline; and there was an upward trend in the scores of the upper and lower meibomian glands in adolescents, although no statistically significant difference was found at any timepoint. The increase in meibomian gland scores was mainly caused by meibomian gland loss. The long-term use of OK carries the risk of meibomian gland injury. Lee et al. [25] reported that OK mainly affected the lower meibomian glands, whereas Yang et al. [22] stated that the upper meibomian glands were more significantly affected. In our study, long-term use of OK damaged both the upper and lower meibomian glands, with the upper meibomian glands being damaged more significantly in the child group. This may be because the upper eyelid has a larger lens contact area, or due to the high presence of subclinical allergic conjunctivitis in children, or poor meibomian gland function before OK use. Lens wearing would then aggravate the original disease, leading to further meibomian gland structural abnormalities [25, 26].
Tear mucins can lubricate the ocular surface, nourish the cornea, and participate in specific and nonspecific immune responses simultaneously [27]. Changes in mucins often indicate ocular surface disorders, such as dry eyes [28]. MUC5AC is the main component of tear mucins, and changes in its content affect tear film stability [14]. It is mainly produced by conjunctival goblet cells; therefore, it can be used as a marker for conjunctival goblet cell–related diseases [29].
Considering that our cohort included children and adolescents, whose ocular surface may be damaged due to histopathology and conjunctival impression cytology, we opted to assess the degree of damage to conjunctival goblet cells indirectly and noninvasively by quantifying tear MUC5AC concentration. In the child group, the MUC5AC concentration in the OK group with 12-month use was lower than that in the other two groups. In the adolescent group, the MUC5AC concentration in the OK group with 12-month use was lower than that in the emmetropia group. In the OK group, there was a slight downward trend in tear MUC5AC concentration over time, which was significant at 6 months and 12 months in adolescents, but only at 12 months in children, and which changed similar to the tear breakup time. These results strongly indicated that long-term OK use negatively affected conjunctival goblet cells and the tear film.
The ocular redness scores, which reflect the degree of conjunctival inflammation, were comparable among the three groups of children but not in adolescents. Moreover, in the OK group of children, the ocular redness scores at 12 months were higher than those at baseline, 1 month, and 3 months, implying higher conjunctival inflammation at 12 months in these participants. Huang et al. [30] reported that conjunctival inflammation could affect tear film stability, but in the present study, the correlation of ocular redness scores with NIBUT (f) and NIBUT (av) was not significant.
This study had some limitations. We only recorded the data of wearing spectacles at 1 year, and thus our study lacked a 1-year follow-up of the spectacle group. Therefore, we could not compare the baseline parameters of the OK and spectacle groups. Second, the aging of the OK lens was not ruled out. The service life of an OK lens is 12–18 months, while most tear film indicators obviously changed when OK was used for 12 months in this study. This possibility can be ruled out by extending the follow-up time and observing tear film changes after OK replacement. Simultaneously, the possibility of meibomian gland recovery in adolescents with myopia and meibomian gland loss after discontinuing OK use should be explored. In the future, we should pay attention to the ocular surface health of OK wearers, and further the study of the tear film proteome.
Conclusions
There was no significant difference in the parameters of tear film between children and adolescents with myopia who used spectacles and those with emmetropia. However, the results of a VAS questionnaire suggested that children with myopia have a higher degree of ocular discomfort, particularly blurred vision symptoms. Additionally, when OK was used for 12 months, the participants had increased ocular surface discomfort, ocular redness, meibomian gland dysfunction, and decreased tear film stability. These changes were not obvious when OK was used for a short duration, suggesting that long-term OK use may damage the tear film stability of children and adolescents. Regular monitoring of tear film indicators is crucial to increasing the safety of OK use.
References
Morgan IG, French AN, Ashby RS, et al. The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res. 2018;62:134–49.
Wang SK, Guo Y, Liao C, et al. Incidence of and factors associated with myopia and high myopia in Chinese children, based on refraction without cycloplegia. JAMA Ophthalmol. 2018;136(9):1017–24.
Shi X, Gao Z, Leng L, Guo Z. Temporal and spatial characterization of myopia in China. Front Public Health. 2022;16(10): 896926.
Hiraoka T, Kakita T, Okamoto F, et al. Influence of ocular wavefront aberrations on axial length elongation in myopic children treated with overnight orthokeratology. Ophthalmology. 2015;122(1):93–100.
Chen Z, Zhou J, Qu X, et al; Shanghai Orthokeratology Study (SOS) Group. Effects of orthokeratology on axial length growth in myopic anisometropes. Cont Lens Anterior Eye. 2018;41(3):263–266.
Jakobsen TM, Møller F. Control of myopia using or thokeratology lenses in Scandinavian children aged 6–12 years. Eighteen-month data from the Danish Randomized Study: Clinical study Of Near-sightedness; TReatment with Orthokeratology Lenses (CONTROL study). Acta Ophthalmol. 2022;100(2):175–182.
Lui WO, Edwards MH, Cho P. Contact lenses in myopia reduction—from orthofocus to accelerated orthokeratology. Cont Lens Anterior Eye. 2000;23(3):68–76.
Cheng HC, Liang JB, Lin WP, et al. Effectiveness and safety of overnight orthokeratology with Boston XO2 high-permeability lens material: a 24-week follow-up study. Cont Lens Anterior Eye. 2016;39(1):67–71.
Miao CX, Xu XY, Zhang H. Analysis of corneal complications in children wearing orthokeratology lenses at night. Chin J Ophthalmol. 2017;53:198–202.
Na KS, Yoo YS, Hwang HS, et al. The influence of overnight orthokeratology on ocular surface and meibomian glands in children and adolescents and adolescents. Eye Contact Lens. 2016;42(1):68–73.
Sahai A, Malik P. Dry eye: prevalence and attributable risk factors in a hospital-based population. Indian J Ophthalmol. 2005;53(2):87–91.
Hom MM, Nguyen AL, Bielory L. Allergic conjunctivitis and dry eye syndrome. Ann Allergy Asthma Immunol. 2012;108(3):163–6.
Wang X, Lu X, Yang J, et al. Evaluation of dry eye and meibomian gland dysfunction in teenagers with myopia through noninvasive keratograph. J Ophthalmol. 2016; 2016:6761206.
Itoh R, Yokoi MD, et al. Tear film instability induced by rigid contact lenses. Cornea. 1999;18(4):440–443
Ozcura F, Aydin S, Helvaci MR. Ocular surface disease index for the diagnosis of dry eye syndrome. Ocul Immunol Inflamm. 2007;15(5):389–93.
Argüeso P, Balaram M, Spurr-Michaud S, et al. Decreased levels of the goblet cell mucin MUC5AC in tears of patients with Sjögren syndrome. Invest Ophthalmol Vis Sci. 2002;43(4):1004–11.
Cho P, Tan Q. Myopia and orthokeratology for myopia control. Clin Exp Optom. 2019;102(4):364–77.
Rojas-Carabali W, Uribe-Reina P, Muñoz-Ortiz J, et al. High prevalence of abnormal ocular surface tests in a healthy pediatric population. Clin Ophthalmol. 2020;22(14):3427–38.
Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118(5):615–21.
Hou W, Norton TT, Hyman L, et al. COMET Group. Axial elongation in myopic children and its association with myopia progression in the correction of myopia evaluation trial. Eye Contact Lens. 2018;44(4):248–259.
Wang X, Li J, Zhang R, Li N, Pang Y, Zhang Y, Wei R. The influence of overnight orthokeratology on ocular surface and meibomian gland dysfunction in teenagers with myopia. J Ophthalmol. 2019;21(2019):5142628.
Yang L, Zhang L, Jian Hu R, et al. The influence of overnight orthokeratology on ocular surface and dry eye-related cytokines IL-17A, IL-6, and PGE2 in children [published online ahead of print, 2020 Apr 29. Cont Lens Anterior Eye. 2020; S1367–0484(20)30062-X.
Xie W, Zhang X, Xu Y, et al. Assessment of tear film and bulbar redness by keratograph 5M in pediatric patients after orthokeratology. Eye Contact Lens. 2018;44(Suppl 2):S382–6.
Li J, Dong P, Liu H. Effect of overnight wear orthokeratology lenses on corneal shape and tears. Eye Contact Lens. 2018;44(5):304–7.
Lee J, Hwang G, Ha M, et al. Evaluation of the meibomian glands using the tear interferometer wearing orthokeratology lenses. BMC Ophthalmol. 2022;22(1):133.
Arita R, Itoh K, Inoue K, et al. Contact lens wear is associated with decrease of meibomian glands. Ophthalmology. 2009;116:379–84.
Ohashi Y, Dogru M, Tsubota K. Laboratory findings in tear fluid analysis. Clin Chim Acta. 2006;369(1):17–28.
Argüeso P, Balaram M, Spurr-Michaud S, et al. Decreased levels of the goblet cell mucin MUC5AC in tears of patients with Sjögren syndrome. Investig Ophthalmol Vis Sci. 2002;43:1004–11.
Khimani KS, Go JA, De Souza RG, et al. Regional comparison of goblet cell number and area in exposed and covered dry eyes and their correlation with tear MUC5AC. Sci Rep. 2020;10(1):2933. (Published 2020 Feb 19)
Huang T, Wang Y, Liu Z, Wang T, Chen J. Investigation of tear film change after recovery from acute conjunctivitis. Cornea. 2007;26(7):778–81.
Acknowledgements
We sincerely thank all the participants of the study.
Funding
This work was supported by Scientific Research Project of Anhui Provincial Health Commission (No. AHWJ2021b115); Provincial Quality Project of Higher Education Department of Anhui Province (No.2021jyxm0711); Anhui Province Scientific Research Planning Project (No.2022AH050792); Clinical Cultivation Program of the Second Affiliated Hospital of Anhui Medical University (No.2020LCZD09); Research Fund Project of Anhui Medical University (No.2022xkj189). Anhui Medical University Early Contact Research (No.2021-ZQKY-151). The funders had no role in study design or conduct of this research. The journal’s Rapid Service fee was funded by the authors.
Author Contributions
Jing Wang and Jingjing Hou designed the study and revised this article. Jingjing Hou contributed to writing of this article. Ningna Zhang, Xueyan Li, Zijun Wang collected and analyzed data. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Jingjing Hou, Ningna Zhang, Xueyan Li, Zijun Wang, and Jing Wang confirm that they have no conflicts of interests to disclose.
Compliance with Ethics Guidelines
The study was approved by the Ethics Committee of the Second Affiliated Hospital of Anhui Medical University (YX2021-053(F2)). Informed consent was obtained from the participants’ parents before they were enrolled in the study.
Data Availability
The data used in this study are available at ChiCTR.org.cn or from the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hou, J., Zhang, N., Li, X. et al. The Effects of Spectacles or Orthokeratology on the Tear Film in Children and Adolescents. Ophthalmol Ther 12, 1913–1927 (2023). https://doi.org/10.1007/s40123-023-00719-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00719-8