Abstract
Introduction
To evaluate the characteristics of optic nerve head (ONH) in highly myopic eyes and its role in predicting intraocular pressure (IOP) spikes after cataract surgery.
Methods
Patients who are highly myopic and were scheduled for cataract surgery were enrolled in this prospective case series study. IOP was measured preoperatively and at 1 day and 3 days postoperatively. ONH characteristics including area, tilt ratio, lamina cribrosa (LC) thickness, and depth, and the presence of LC defects were evaluated with enhanced depth imaging optical coherence tomography. Factors influencing LC defects and early IOP spike were investigated using multivariate stepwise logistic regression.
Results
In total, 200 highly myopic eyes of 200 patients were analyzed: 35.00% had small ONH, 53.00% had ONH tilt, and 14.00% had LC defects. Multivariate analysis demonstrated female patients with larger ONH area and deeper LC tended to have LC defects (all P < 0.05). As to postoperative IOP, IOP change, and incidence of IOP spikes, eyes with small ONH, ONH tilt, and LC defects had similar (all P > 0.05), higher (all P < 0.05), and lower (all P < 0.05) outcomes compared with those without the corresponding characteristic, respectively. Multivariate analysis showed that presence of LC defects and thicker LC were protective factors for early IOP spikes, and axial length > 28 mm was a risk factor (all P < 0.05).
Conclusion
Female patients with larger ONH area and deeper LC tend to have LC defects, which, together with thicker LC, was correlated with less IOP spikes in highly myopic eyes.
Trial Registration
This study was conducted as part of a larger project, the Shanghai High Myopia Study, registered at www.clinicaltrials.gov (accession number NCT03062085).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients who are highly myopic have special characteristics of optic nerve head (ONH) and a higher incidence of early transient intraocular pressure (IOP) spikes after cataract surgery. |
We sought to determine if the characteristics of ONH in highly myopic eyes play a role in predicting IOP spikes after cataract surgery. |
What was learned from this study? |
The presence of lamina cribrosa defects and greater lamina cribrosa thickness were correlated with less IOP spikes in highly myopic eyes, while axial length > 28mm had the opposite effect. |
These findings may help surgeons better estimate the onset and degree of postoperative IOP spikes after cataract surgery with an adequate preoperative assessment of ONH features in patients who are highly myopic. |
Introduction
As surgical techniques advanced, the efficacy and safety of phacoemulsification have become well established with minor incisions, faster recovery, and fewer complications. However, patients who were highly myopic reportedly experienced a higher incidence of early transient intraocular pressure (IOP) spikes after cataract surgery than non-myopes [1,2,3,4]. As an acute adverse event, postoperative IOP spikes can cause ocular pain and may increase the risk of sight-threatening complications, such as retinal vascular occlusion, and are potentially more dangerous in eyes with preexisting optic nerve damage [5, 6]. Hence, identifying possible predictive factors for postoperative IOP spikes is meaningful for the clinical management of patients who are highly myopic.
Previously, our research group has explored some potential biometric risk factors for postoperative IOP spikes in highly myopic eyes [3, 4], but the associations with optic nerve head (ONH) characteristics, which are closely related to the course of glaucoma, remain largely unclear. Various ONH changes were found to be linked with high myopia, such as ONH tilt, lamina cribrosa (LC) thinning, and LC defect [7,8,9]. Currently, ONH’s biomechanical responses to IOP elevation have been extensively studied in glaucomatous eyes of monkeys and humans [10, 11]. However, their role in postoperative IOP spikes in highly myopic eyes has seldom been investigated.
Due to the thinning of the peripapillary sclera and the axial stretching in high myopia, the ONH might be morphologically changed, and the biomechanical features of LC might also be different. The LC, a multilayered sieve-like collagen beam, is recognized as the primary and principal site of retinal ganglion cell axonal injury in glaucoma [12]. Structural alternations including LC thinning, posterior displacement, deformation, and defects were previously reported to be associated with the onset of glaucoma or increased IOP [5, 6, 11]. Furthermore, LC defects were considered myopia-related anatomical changes potentially associated with the prevalence of glaucoma-like optic neuropathy [13, 14]. Therefore, we assumed that there might be possible associations between ONH characteristics and IOP spikes after cataract surgery in highly myopic eyes.
In this study we aimed to evaluate the characteristics of optic nerve head (ONH) in highly myopic eyes, and to explore its role in predicting intraocular pressure (IOP) spikes after cataract surgery.
Methods
Ethics
This prospective case series was carried out at the Eye and Ear, Nose and Throat (ENT) Hospital of Fudan University. This study was conducted as part of a larger project, the Shanghai High Myopia Study, registered at www.clinicaltrials.gov (accession number NCT03062085). The design and conduction of the study were in accordance with the tenets of the Declaration of Helsinki, and were approved by the institutional review board of our hospital. All participants provided their signed informed consent for the use of their clinical data after receiving a full description of the study.
Patient Enrollment
Participants who scheduled for cataract surgery were consecutively recruited from the Eye and ENT Hospital of Fudan University from September 2020 to January 2022. The inclusion criteria were: (1) highly myopic eyes with axial length (AL) ≥ 26.00 mm, (2) eyes with preoperative baseline IOP < 21 mmHg, and (3) eyes with reliable OCT measurements before cataract surgery. The exclusion criteria were: (1) eyes with clinical diagnosis of glaucoma or glaucoma suspect, (2) eyes with other ocular comorbidities or systemic diseases, which may affect the postoperative IOP, such as corneal opacity, zonular weakness, uveitis, and pseudoexfoliation syndrome, with oral tamsulosin etc., (3) eyes with prior surgery or trauma, and (4) eyes with intraoperative or postoperative complications, which may affect the postoperative IOP, such as posterior capsular rupture, corneal edema, IOL dislocation, or with residual viscoelastic material. One eye was randomly selected from each patient if both eyes met the criteria. A total of 213 participants were recruited, and 200 eyes from 200 eligible participants were finally included in the analyses.
Baseline Ophthalmic Examinations
All participants received ophthalmic examinations at the baseline visit, including slit lamp microscopy, Goldmann applanation tonometry (Haag-Streit, Bern, Switzerland), fundoscopy, corneal topography (Pentacam HR; Oculus Optikgeräte, Wetzlar, Germany), B-scan ultrasonography, and AL measurements using IOL Master (Carl Zeiss AG, Oberkochen, Germany).
Enhance Depth Imaging Optical Coherence Tomography of Optic Nerve Head
All participants received enhanced depth imaging optical coherence tomography (EDI-OCT) (Heidelberg Spectralis SD-OCT, Heidelberg Engineering GmbH, Heidelberg, Germany) scans and all scans were performed by one experienced operator (W.W.H.). A 15° × 15° rectangular scan was centered on the ONH. This rectangle was scanned with 97 sections, and each section had 20 OCT frames on average. Infrared fundus images were simultaneously acquired using a confocal scanning laser ophthalmoscope. The serial OCT scan images were carefully reviewed for optic nerve head characteristics by an experienced specialist (X.J.Z.) masked to the clinical information of participants.
The disc margin was measured on infrared fundus images. The longest diameter (LD), shortest diameters (SD), and the area of the ONH were measured. A small ONH was defined as the ONH area < 1.5 mm [2, 15]. The ONH tilt ratio was defined as the ratio between the LD and SD, and a ratio > 1.3 was considered the presence of tilt (Fig. 1A) [4].
Optic nerve head (ONH) images using enhanced depth imaging spectral-domain optical coherence tomography. A Measurement of the longest diameter (LD, yellow full line), shortest diameters (SD, yellow dotted line), and area (yellow dotted circle) of the ONH area. B Measurement of lamina cribrosa (LC) depth and LC thickness: the Bruch’s membrane opening (BMO) reference line (blue line) was drawn by connecting the two termination points of Bruch’s membrane on each B-scan. The anterior (yellow full line) and posterior margins (yellow dotted line) of the highly reflective region were used as the borders of the LC. The LC thickness was calculated as the perpendicular distance between those borders (blue line with arrows) and the LC depth was calculated as the vertical distance between the BMO line and the anterior margin of the LC (yellow line with arrows). C Representative image of LC defect (green arrow)
The LC thickness and depth measurements were performed using the horizontal B scans by selecting the frame passing through the vertical center of the ONH with nasal fixation, according to a previously described method [16,17,18]. Briefly, the Bruch’s membrane opening (BMO) reference line was drawn by connecting the two termination points of Bruch’s membrane on each B-scan. The anterior and posterior margins of the highly reflective region were used as the borders of the LC. The LC thickness was calculated as the perpendicular distance between those borders. The LC depth was calculated as the vertical distance between the BMO line and the anterior margin of the LC (Fig. 1B). The measurement was performed by a built-in caliper tool of the intrinsic OCT viewer, and the scaling of B-scan images was corrected to 1:1 μm before evaluation.
LC defects were defined as an anterior laminar surface irregularity violating the normal smooth contour, including features of holes, pits, or scleral disinsertions [19]. To avoid false positives, LC defects were required to be present in two neighboring B-scan images, and have a diameter > 100 μm and a depth > 30 μm. The location of LC defects was classified into the superior or inferior half of the ONH (Fig. 1C) [13].
Surgical Technique
All surgeries were performed by one experienced surgeon (Y.L.). Through a clear corneal incision of 2.6 mm, the DisCoVisc (Alcon Laboratories, Fort Worth, Texas, USA) was injected. After completion of continuous curvilinear capsulorhexis and hydro-dissection, phacoemulsification, removal of the cortex, and IOL implantation in the capsular bag were performed. After removing viscoelastic material, the IOL was adjusted to the center, and the incision was hydrated. No stitches were used in any eyes. Subjects were instructed to take routine postoperative medications, including Cravit eye drops (levofloxacin, Santen Pharmaceutical, Japan) and prednisolone acetate (Allergen Pharmaceutical Ireland, Westport, County Mayo, Ireland) four times a day for 2 weeks, and Pranopulin (pranoprofen, Senju Pharmaceutical, Osaka, Japan) four times a day for 4 weeks. For eyes with postoperative IOP reaching 25–30 mmHg, Mikelan eye drops (carteolol hydrochloride, Otsuka Pharmaceutical, Tokyo, Japan) were used twice daily. For eyes with postoperative IOP reaching 30–35 mmHg, Azarga eye drops (brinzolamide-timolol fixed-combination, Alcon Laboratories) were used twice daily. For eyes with postoperative IOP > 35 mmHg, an intravenous drip injection of d-mannitol was administered. IOP-lowering medication was maintained until the IOP decreased to ≤ 21 mmHg.
Postoperative Examinations
Postoperative examinations were respectively conducted at 1 and 3 days after surgery, including the assessment of best-corrected visual acuity (BCVA), fundoscopy, and measurement of IOP. The IOP change was defined as the maximum postoperative IOP subtracted by the baseline IOP. The IOP spike was defined as postoperative IOP ≥ 25 mmHg or an IOP elevation ≥ 8 mmHg from the baseline [3, 4, 20].
Statistics
Continuous data are presented as mean ± standard deviations and are compared using Student’s t-test between two groups, while categorical data are presented as frequency (percentage) compared using the χ2 test. Multivariable stepwise binary logistic regression was conducted to explore the potential and independent factors for LC defects and IOP spikes. Odds ratios (ORs) and the corresponding 95% confidence intervals (95% CIs) were presented. Using G*Power, the sample size should be more than 191 with α error of 0.05, power of 0.9, and OR of 1.71 for binary logistic regression [21]. A total of 213 participants were recruited, and 200 eyes from 200 eligible participants were finally included in the analyses. Statistical significance was defined as P < 0.05. All statistical analyses were performed using SPSS (version 20, IBM Inc., USA).
Results
Baseline Characteristics
Baseline characteristics of all included eyes are presented in Table 1. The mean AL was 28.67 ± 1.94 mm, ranging from 26.00 to 36.03 mm.
Characteristics of Optic Nerve Head in Highly Myopic Eyes
Of all eyes included, 35.00% were identified with small ONH, 53.00% were identified with ONH tilt, and 14.00% were identified with LC defects, of which 82.14% had a superior defect, and the rest had an inferior defect. We further compared ONH characteristics among eyes within different AL ranges (Table 2). Compared with eyes with AL 26.00 ~ 28.00 mm, the SD of ONH in eyes with AL > 28.00 mm was significantly shorter, while the tilt ratio and presence of ONH tilt were significantly higher (Student’s t-test or χ2 test, all P < 0.05). Other structural parameters showed no significant difference between two AL subgroups (Student’s t-test or χ2 test, all P > 0.05).
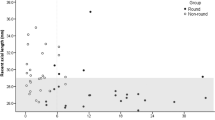
To identify the factors influencing the presence of LC defect, we performed a multivariate stepwise binary logistic regression using predictors including age, sex, AL, ONH LD/SD/area/tilt ratio, LC thickness, and LC depth (Fig. 2). It demonstrated that highly myopic females with larger ONH area and deeper LC had a higher risk of LC defects (all P < 0.05).
Intraocular Pressure Change in Eyes with Different Optic Nerve Head Characteristics
The perioperative IOPs were compared in highly myopic eyes with different ONH characteristics (Table 3). No significant differences were found in perioperative IOPs (Student’s t test, all P > 0.05) or the incidence of IOP spikes between the small ONH present and absent groups (χ2 test, P > 0.05). However, the ONH tilt-present group demonstrated significantly higher postoperative IOP, IOP change, and higher incidence of IOP spikes after cataract surgery compared with the ONH tilt-absent group (Student’s t test or χ2 test, all P < 0.05). Conversely, eyes with LC defects showed significantly lower postoperative IOP, IOP change, and lower incidence of IOP spikes compared with those without (Student’s t test or χ2 test, all P < 0.05).
Predicting Factors for IOP Spikes after Cataract Surgery in Highly Myopic Eyes
We then conducted a multivariable stepwise binary logistic regression analysis for the presence of IOP spike, using predictors including age, sex, AL subgroups, presence of ONH tilt, presence of LC defects, LC depth, and LC thickness (Fig. 3). It demonstrated that the risk factor for IOP spikes was AL ≥ 28.00 mm (P = 0.002), while the protective factors were greater LC thickness and the presence of LC defects (both P = 0.009).
Discussion
Highly myopic eyes were reported to experience a higher incidence of early IOP spikes after cataract surgery [1,2,3,4]. Due to AL elongation and anatomical variation of the posterior segment, highly myopic eyes may have distinct mechanisms for IOP adjustment. The myopia-associated anatomical changes of ONH were previously reported to influence the IOP of patients with glaucoma, but their influence on postoperative IOP spikes remained unclear. In this study, using EDI-OCT, we revealed that the protective factors for IOP spikes in highly myopic eyes were the presence of LC defects and greater LC thickness.
In high myopia, the extreme elongation of the eyeball could lead to various morphologic changes in the ONH. Here, we found that the ONH tilt was prominent in eyes with AL ≥ 28.00 mm compared with eyes with AL 26.00 ~ 28.00 mm. Our finding was consistent with that of Chen et al. [22], who also revealed that longer AL was associated with higher likelihood of disc tilt. This phenomenon might be attributed to excessive axial elongation and posterior scleral remodeling in extremely myopic eyes. However, no significant difference was observed in the presence of LC defects between two AL subgroups, contradicting some previous investigations [23, 24]. This inconsistency may be explained by the fact that those studies were conducted in patients with glaucoma, yet the patients who were highly myopic included in our study were relatively normal. It is also interesting to note that LC defects were more common in highly myopic females with a larger ONH area and deeper LC, suggesting that the formation of LC defects might be associated with additional stress from the expansion of the ONH area and posteriorization of the LC. Therefore, characterization of the LC changes might be necessary for highly myopic eyes.
The ocular response to IOP is determined by both the magnitude of IOP and the intrinsic biomechanical properties of the ocular tissues, particularly the connective tissues of the ONH and the sclera [25]. Therefore, an early transient IOP spike could possibly be associated with the biomechanical change of ONH in highly myopic eyes. In the present study, we found that eyes with ONH tilt had a higher incidence of postoperative IOP spikes, but the presence of ONH tilt was not considered a risk factor after adjusting confounding factors in the logistic regression model. This was consistent with our previous research [4], and it might be due to the collinearity of extent of tilt and AL. Additionally, we found that the risk factor for IOP spikes was AL ≥ 28.00 mm in multivariable regression; this may be because axial stretching in high myopia was correlated with dysfunction at the trabecular meshwork and Schlemm’s canal, which was confirmed in our previous study [3]. In this study, the postoperative IOPs in highly myopic eyes with different ONH characteristics were all higher than the preoperative values. This may be because we measured all the IOPs 1 to 3 days after cataract surgery and the microinflammation of trabecular meshwork may lead to the elevated IOP.
Notably, we observed that eyes with LC defects had a lower incidence of postoperative IOP spikes and also confirmed the protective role of LC defects and greater LC thickness. Several previous studies in patients with glaucoma support our findings, showing that normal-tension glaucoma (NTG) eyes with a focal LC defect had lower baseline untreated IOP, lower peak IOP, and lower mean IOP [24, 26,27,28]. Anatomically, the LC located in the posterior sclera helps preserve a pressure gradient between the extraocular and intraocular spaces. Sun et al. [28] reported that LC defects in highly myopic NTG eyes might influence the pressure difference between the vitreous cavity and subarachnoid space through fluid’s slow diffusion, but not through the direct communication. That process might rebalance the higher trans-LC pressure gradient, which was supposed to be one of the recognized risk factors for NTG [29]. These findings led us to speculate that LC defects in highly myopic eyes might be responsible for the fluid diffusion, and thus result in decreased IOP spike after cataract surgery. We therefore hypothesized that although the LC defect, a special structure of highly myopic eyes, was a myopia-related anatomical change, it created a valve-like “back door” for IOP regulation. Furthermore, previous research has also suggested that the LC in patients with NTG and high-tension glaucoma was significantly thinner than in normal subjects [17]. Therefore, an increase in LC thickness among highly myopic eyes may also help stabilize trans-LC pressure fluctuation [25, 30, 31], especially when cerebrospinal fluid pressure changed, leading to a reduced risk of IOP spikes after cataract surgery.
In addition, we found that male sex was one of the risk factors associated with the IOP spike in our previous study [4]. However, in the current study, we did not identify this relationship. This may be because LC defects were more common in females, and the presence of LC defects was an independent protective factor of IOP spikes, rather than sex.
However, there were some limitations of this study. First, the sample size of patients with IOP spikes was not large enough for logistic regression, although the total sample size was enough according to previous research [32]. The effect of the number of events per variable (EPV) analyzed in logistic regression analysis was 7.43 and the recommended EPV is more than 10. Second, we did not study the effect of trabecular meshwork, Schlemm’s canal, and cerebrospinal fluid pressure in this study; however, we will investigate these in further studies.
Conclusion
In this prospective case series, we characterized the ONH in highly myopic eyes and identified the protective role of LC defects and greater LC thickness against early IOP spikes after cataract surgery. Our findings may help surgeons better estimate the onset and degree of postoperative IOP spikes after cataract surgery, with an adequate preoperative assessment of ONH features in patients who were highly myopic.
References
Yao Y, Lu Q, Wei L, Cheng K, Lu Y, Zhu X. Efficacy and complications of cataract surgery in high myopia. J Cataract Refract Surg. 2021;47:1473–80.
Tsai CY, Chang TJ, Kuo LL, Chou P, Woung LC. Visual outcomes and associated risk factors of cataract surgeries in highly myopic Taiwanese. Ophthalmologica. 2008;222:130–5.
Qi J, He W, Lu Q, Zhang K, Lu Y, Zhu X. Schlemm canal and trabecular meshwork features in highly myopic eyes with early intraocular pressure elevation after cataract surgery. Am J Ophthalmol. 2020;216:193–200.
Zhu X, Qi J, He W, Zhang S, Zhang K, Lu Q, Lu Y. Early transient intraocular pressure spike after cataract surgery in highly myopic cataract eyes and associated risk factors. Br J Ophthalmol. 2020;104:1137–41.
Grzybowski A, Kanclerz P. Early postoperative intraocular pressure elevation following cataract surgery. Curr Opin Ophthalmol. 2019;30:56–62.
Hildebrand GD, Wickremasinghe SS, Tranos PG, Harris ML, Little BC. Efficacy of anterior chamber decompression in controlling early intraocular pressure spikes after uneventful phacoemulsification. J Cataract Refract Surg. 2003;29:1087–92.
Liu HH, Xu L, Wang YX, Wang S, You QS, Jonas JB. Prevalence and progression of myopic retinopathy in Chinese adults: the Beijing Eye Study. Ophthalmology. 2010;117:1763–8.
Sung MS, Kang YS, Heo H, Park SW. Characteristics of optic disc rotation in myopic eyes. Ophthalmology. 2016;123:400–7.
Adams DL, Economides JR, Horton JC. Cortical representation of a myopic peripapillary crescent. Ophthalmology. 2016;123:1494–9.
Stein JD, Khawaja AP, Weizer JS. Glaucoma in adults-screening, diagnosis, and management: a review. JAMA. 2021;325:164–74.
Bellezza AJ, Rintalan CJ, Thompson HW, Downs JC, Hart RT, Burgoyne CF. Deformation of the lamina cribrosa and anterior scleral canal wall in early experimental glaucoma. Invest Ophthalmol Vis Sci. 2003;44:623–37.
Krzyzanowska-Berkowska P, Czajor K, Syga P, Iskander DR. Lamina Cribrosa Depth and Shape in Glaucoma Suspects. Comparison to Glaucoma Patients and Healthy Controls. Curr Eye Res 2019;44:1026–1033.
Miki A, Ikuno Y, Asai T, Usui S, Nishida K. Defects of the lamina cribrosa in high myopia and glaucoma. PLoS One. 2015;10: e0137909.
Jonas JB, Panda-Jonas S, Wang YX. Glaucoma neurodegeneration and myopia. Prog Brain Res. 2020;257:1–17.
Bayer A, Harasymowycz P, Henderer JD, Steinmann WG, Spaeth GL. Validity of a new disk grading scale for estimating glaucomatous damage: correlation with visual field damage. Am J Ophthalmol. 2002;133:758–63.
Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009;147:811–5.
Park HY, Jeon SH, Park CK. Enhanced depth imaging detects lamina cribrosa thickness differences in normal tension glaucoma and primary open-angle glaucoma. Ophthalmology. 2012;119:10–20.
Sirakaya E, Kucuk B, Agadayi A, Yilmaz N. Evaluation of the lamina cribrosa thickness and depth in patients with migraine. Int Ophthalmol. 2020;40:89–98.
Park SC, Hsu AT, Su D, Simonson JL, Al-Jumayli M, Liu Y, Liebmann JM, Ritch R. Factors associated with focal lamina cribrosa defects in glaucoma. Invest Ophthalmol Vis Sci. 2013;54:8401–7.
Jiang Y, Chang DS, Foster PJ, He M, Huang S, Aung T, Friedman DS. Immediate changes in intraocular pressure after laser peripheral iridotomy in primary angle-closure suspects. Ophthalmology. 2012;119:283–8.
Harrell FE Jr. Regression modeling strategies; with applications to linear models, logistic regression, and survival analysis. New York: Springer-Verlag; 2001.
Chen Q, He J, Yin Y, Zhou H, Jiang H, Zhu J, Ohno-Matsui K, Zou H, Fan Y, Xu X. Impact of the morphologic characteristics of optic disc on choroidal thickness in young myopic patients. Invest Ophthalmol Vis Sci. 2019;60:2958–67.
Han JC, Cho SH, Sohn DY, Kee C. The characteristics of lamina cribrosa defects in myopic eyes with and without open-angle glaucoma. Invest Ophthalmol Vis Sci. 2016;57:486–94.
Park HY, Hwang YS, Park CK. Ocular characteristics associated with the location of focal lamina cribrosa defects in open-angle glaucoma patients. Eye (Lond). 2017;31:578–87.
Jonas JB, Berenshtein E, Holbach L. Anatomic relationship between lamina cribrosa, intraocular space, and cerebrospinal fluid space. Invest Ophthalmol Vis Sci. 2003;44:5189–95.
Takayama K, Hangai M, Kimura Y, Morooka S, Nukada M, Akagi T, Ikeda HO, Matsumoto A, Yoshimura N. Three-dimensional imaging of lamina cribrosa defects in glaucoma using swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54:4798–807.
Kim YK, Jeoung JW, Park KH. Effect of focal lamina cribrosa defect on disc hemorrhage area in glaucoma. Invest Ophthalmol Vis Sci. 2016;57:899–907.
Sun Y, Guo Y, Xie Y, Cao K, Liu X, Yang Y, Shi Y, Fan S, Wang H, Wang N. Intereye comparison of focal lamina cribrosa defect in normal-tension glaucoma patients with asymmetric visual field loss. Ophthalmic Res. 2021;64:447–57.
Jonas JB, Wang N, Yang D, Ritch R, Panda-Jonas S. Facts and myths of cerebrospinal fluid pressure for the physiology of the eye. Prog Retin Eye Res. 2015;46:67–83.
Jonas JB, Berenshtein E, Holbach L. Lamina cribrosa thickness and spatial relationships between intraocular space and cerebrospinal fluid space in highly myopic eyes. Invest Ophthalmol Vis Sci. 2004;45:2660–5.
Xu L, Li Y, Wang S, Wang Y, Wang Y, Jonas JB. Characteristics of highly myopic eyes: the Beijing eye study. Ophthalmology. 2007;114:121–6.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9.
Acknowledgements
We thank all the participants of the study.
Funding
This study and its publication, including the journal’s rapid service fee, were supported by research grants from the National Natural Science Foundation of China (82122017, 82271069, 81900838, 81870642, 81970780, 81470613, and 81670835), Science and Technology Innovation Action Plan of Shanghai Science and Technology Commission (19441900700 and 21S31904900), Clinical Research Plan of Shanghai Shenkang Hospital Development Center (SHDC2020CR4078, SHDC12019X08, and SHDC12020111), Double-E Plan of Eye and ENT Hospital (SYA202006), Shanghai Municipal Key Clinical Specialty Program (shslczdzk01901), and the Fudan University Outstanding 2025 Program.
Author Contributions
Contributuons were as follows: study design (Xiangjia Zhu), study performance (Wenwen He, Ling Wei, Shuyu Liu, Zhiqian Huang, Jiao Qi, Keke Zhang, Jiaqi Meng, Yu Du), data collection and management (Wenwen He, Ling Wei, Shuyu Liu), data analysis and interpretation (Xiangjia Zhu, Wenwen He, and Ling Wei), drafting the manuscript (Wenwen He, Ling Wei, Shuyu Liu, Zhiqian Huang, Jiao Qi, Keke Zhang, Jiaqi Meng, and Yu Du), and revising the manuscript (Xiangjia Zhu, and Yi Lu). All of the authors approved the manuscript.
Disclosures
Wenwen He, Ling Wei, Shuyu Liu, Zhiqian Huang, Jiao Qi, Keke Zhang, Jiaqi Meng, Yu Du, Yi Lu, and Xiangjia Zhu have nothing to declare.
Compliance with Ethics Guidelines
The design and conduction of the study were in accordance with the tenets of the Declaration of Helsinki and were approved by the institutional review board of Eye and Ear, Nose, and Throat (ENT) Hospital of Fudan University (No. 2014055). All the participants were informed to follow-up and use their data for medical research, and the data used for publication does not contain their personal information.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
He, W., Wei, L., Liu, S. et al. Role of Optic Nerve Head Characteristics in Predicting Intraocular Pressure Spikes after Cataract Surgery in Highly Myopic Eyes. Ophthalmol Ther 12, 2023–2033 (2023). https://doi.org/10.1007/s40123-023-00714-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00714-z