Abstract
Introduction
The aim of this study was to investigate changes in the Clinical Activity Score, serum thyroid-stimulating hormone receptor antibody and thyroid-stimulating immunoglobulin levels, chorioretinal blood vessels, and extraocular muscle thickness in patients with thyroid eye disease following systemic steroid treatment.
Methods
This prospective observational study enrolled 57 patients with active thyroid eye disease who received systemic intravenous glucocorticoids for 12 weeks. Demographics, clinical activity scores, optical coherence tomography images, and serum thyroid-stimulating immunoglobulin and thyroid-stimulating hormone receptor antibody levels were assessed at baseline, at 6 and 12 weeks after intravenous (IV) GC therapy initiation, and 2 months after IV GC therapy termination. The extraocular muscle thickness, choroidal thickness, and choroidal vascularity index were measured.
Results
The clinical activity scores showed a significant decrease. Serum thyroid-stimulating immunoglobulin levels dropped continuously for 2 months. The thyroid-stimulating hormone receptor antibody level decreased until 12 weeks after treatment but returned to within the normal range in 75% of patients after 77 and 126 days, respectively. The choroidal thickness decreased at all time points. The thickness of the medial and inferior rectus muscles decreased at 2 months after treatment. The clinical activity score decreased to < 3 points in 50% of patients after 78 days.
Conclusion
Intravenous glucocorticoid therapy improved the clinical activity score, chorioretinal blood flow, and extraocular muscle thickness. The serum autoantibody levels were normalized in patients with active thyroid eye disease 2 months after IV GC termination. The serum thyroid-stimulating immunoglobulin and thyroid-stimulating hormone receptor antibody levels correlated with restoration of chorioretinal capillary perfusion and improved clinical symptoms and muscle thickness. Non-invasive optical coherence tomography findings and serologic factors predict the response to intravenous glucocorticoid therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Systemic glucocorticoid therapy has been recommended as the first-line therapy for moderate-to-severe thyroid eye disease, but the relationship between serum thyroid-stimulating hormone receptor autoantibodies, thyroid-stimulating immunoglobulin level, and chorioretinal vascular change is understudied. |
This prospective observational study was performed to investigate the changes in the serum autoantibody levels, clinical symptoms, and eyeball anatomy in patients with thyroid eye disease after intravenous glucocorticoid therapy. |
What was learnt from the study? |
Intravenous glucocorticoid therapy caused overall improvement in clinical activity score, chorioretinal blood flow, and extraocular muscle thickness. |
Decreases in serum thyroid-stimulating immunoglobulin and thyroid-stimulating hormone receptor autoantibody levels are correlated with restoration in chorioretinal capillary perfusion and improvement of clinical symptoms and extraocular muscle thickness. |
The results suggest that serologic factors and non-invasive optical coherence tomography findings can predict the response to intravenous glucocorticoid therapy. |
Introduction
Thyroid eye disease (TED), an autoimmune ocular disease, is generally associated with thyroid disease, including Graves’ disease and, occasionally, hypo- or euthyroidism [1]. In the early phase of acute TED, hydrophilic hyaluronic acid accumulates in the extraocular muscles and orbital adipose tissue, causing edema. In the late or chronic period, fibrosis occurs due to collagen deposition [2, 3]. Consequently, various ocular symptoms occur, ranging from mild foreign body sensation, dry eyes, and eyelid retraction to extraocular muscle hypertrophy, restrictive myopathy, and diplopia [3].
The suspected mechanism of action is the activation of orbital fibroblasts by thyroid-stimulating hormone receptor autoantibodies (TSHR Ab) [4]. Currently, two methods are used to test for TSHR Ab: the thyroid-stimulating hormone receptor binding inhibitory immunoglobulin (TBII) test, which detects thyroid-stimulating immunoglobulin (TSI), neutral, and blocking antibodies [5], and the TSI bioassay, which selectively detects stimulating antibodies by assessing the production of cyclic adenosine monophosphate [6]. Although TBII testing is widely used due to its relative convenience, use of the TSI bioassay is increasing owing to its high sensitivity and specificity [7].
Intravenous (IV) glucocorticoid (GC) therapy has been recommended by the European Group on Graves’ Orbitopathy (EUGOGO) consensus group as the first-line therapy for moderate-to-severe TED or dysthyroid optic neuropathy [8]. In multiple clinical trials, IV GC therapy was found to be more effective in rapidly reducing inflammation than oral GC therapy, with response rates of 80% and 50%, respectively [9, 10].
Swept-source optical coherence tomography (SS-OCT) is used to evaluate the retinal structure with a high resolution [11]. Furthermore, OCT angiography (OCT-A) can non-invasively and repeatedly assess in detail chorioretinal vessel structures, including the foveal avascular zone (FAZ) and superficial and deep capillary plexus density (sCPD and dCPD, respectively).
We believe that the relationship between serum TSHR Ab, TSI level, and chorioretinal vascular change, especially after systemic GC therapy, is understudied. Furthermore, the time point at which the autoantibody level and clinical activity of the disease normalize has not yet been investigated. Thus, the aim of this study was to evaluate the correlations between the Clinical Activity Score (CAS), serologic levels, and ocular involvement using OCT and the changes in these metrics after IV GC therapy in patients with TED.
Methods
Study Design and Population
This was a prospective observational study conducted in a single hospital. All patients provided written informed consent for study participation and publication. The study was performed in accordance with the 1964 Declaration of Helsinki and its later amendments, and was approved by the Institutional Review Board of the Keimyung University Hospital (approval number: 2021-02-046).
Patients diagnosed with active moderate-to-severe TED from March 2021 to May 2022 were eligible for inclusion in the study. Among these were 25 patients (43.8%) with mild TED who were previously followed up in a single hospital and who later progressed to moderate-to-severe TED. Disease severity was classified according to the EUGOGO guidelines, and active TED was defined as a CAS ≥ 3 of seven criteria [8]. Methylprednisolone (methylprednisolone sodium succinate; SALON®; Hanlim Pharm Co., Seoul, Korea) was administered by IV injection (referred to further as IV GC) for 12 weeks according to a predetermined schedule: 500 mg weekly for the first 6 weeks and 250 mg weekly for the following 6 weeks. All patients were followed up for 2 months after IV GC therapy and were instructed to take 200 µg of selenium daily according to the EUGOGO guidelines [8]. Participants’ ages ranged from 21 to 65 years. The exclusion criteria were age ≥ 80 years, any ocular disease affecting visual acuity, and ocular surgery within the previous 6 months. Patients that were unable to undergo examination or systemic GC therapy due to underlying medical conditions, such as uncontrolled hypertension, diabetic mellitus, gastrointestinal disease, liver, or renal disease, were also excluded. All clinical tests described were performed at baseline, at 6 and 12 weeks after IV GC therapy initiation, and 2 months after IV GC termination.
Clinical Data Collection
Patient demographics and background history were recorded at the initial visit. Baseline ophthalmic assessments were performed. CAS was calculated by assessing the following seven criteria: spontaneous retrobulbar pain, pain on attempted gaze, eyelid redness, conjunctival redness, eyelid swelling, caruncle or plica swelling, and chemosis [12]. The serum TSI and TSHR Ab levels were examined, and the liver function and blood glucose levels were monitored.
We used SS-OCT (DRI OCT Triton®, Topcon, Tokyo, Japan) to obtain OCT and OCT-A images. In OCT-A, the 3.0 × 3.0-mm en face images of the macula were divided automatically into the subfields of a central area of 1.0-mm-diameter and a paracentral area of the remaining annular area, in a 3.0-mm-diameter circle excluding the central area, by IMAGEnet 6 software (version 1.22; Topcon, Tokyo, Japan), and the sCPD and dCPD were calculated. The borderline of the superficial and deep foveal avascular zone (sFAZ and dFAZ, respectively) was measured using IMAGEnet 6 software. Choroidal thickness (CT) was measured from the retinal pigment epithelium to the outer boundary of the choroid at the macular center and at the right and left 300 μm and defined as the average of the three vertical lines. The choroidal vascular index (CVI) was analyzed according to the method by Agrawal et al. [13] to determine the area of the choroidal vessels in the OCT images (Fig. 1).
An image from swept-source optical coherence tomography angiography (OCT-A) in thyroid eye disease. i Choroidal thickness was measured from the retinal pigment epithelium to the outer boundary of choroid at the macular center and at the right and left 300 μm and defined as the average of the 3 vertical lines. ii The choroidal vascular index (CVI) is defined as the ratio of the vascular area in the choroid tissue, and was examined using Image J software, which generates the binarization of the choroid tissue and estimates CVI by calculating the ratio of the luminal area to the total choroid area. iii, iv Superficial and deep foveal avascular zones were examined using IMAGE Net 6 software. v, vi Superficial and deep capillary plexus density were automatically measured using IMAGE Net 6 software. vii Anterior segment OCT showing the thickness of the medial rectus muscle of the right eye. The thickness of muscle is defined as the vertical line (green), which creates a 90° angle on the plane of muscle insertion site (yellow)
The anterior segment OCT images of the superior, inferior, medial, and lateral rectus (SR, IR, MR, and LR, respectively) were examined using the “anterior segment module” of SS-OCT. Extraocular muscle thickness was defined as the perpendicular length between the muscle insertion site and the thinnest point of the muscle tendon and was analyzed by one skilled examiner to compensate for physiological differences [14] (Fig. 1).
Statistical Analysis
Data are presented as the mean ± standard deviation and 95% confidence interval (CI). SPSS version 20.0 for Windows software (SPSS IBM Co., Armonk, NY, USA) was used for all statistical analysis. Generalized estimating equations were used to examine the overall changes in serologic levels, OCT parameters, and CAS during the follow-up period. Pearson’s correlation test was used to examine the correlation between the serologic indicators, clinical activity, and OCT parameters. Kaplan–Meier survival analysis was used to evaluate the time point from the initiation of IV GC therapy at which the serum TSHR Ab and TSI levels and CAS decreased to normal. A p-value < 0.05 was considered to be statistically significant.
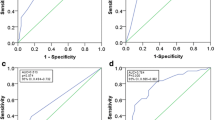
Results
Overall, 57 patients with TED were enrolled in the study. The baseline characteristics are presented in Table 1. The baseline average CAS was 3.263 ± 0.518, serum TSI level was 459.263 ± 143.021 SSR% (specimen-to-reference ratio percentage), and TSHR Ab level was 17.424 ± 24.520 IU/L (Table 1). The overall changes in autoantibody levels, CAS, and OCT factors are shown in Fig. 2 and Table 2. CAS significantly decreased at all follow-up points; the average score was 3.26 at baseline, 2.58 and 1.80 at 6 and 12 weeks after IV GC therapy initiation, respectively, and 1.02 at 2 months after termination of IV GC therapy (p < 0.001, for all time points). Serum TSI levels continuously and significantly decreased from 459.26 SSR% at baseline to 394.66 SSR% at 6 weeks, 343.54 SSR% at 12 weeks, and 331.95 SSR% at 2 months after IV GC therapy (p = 0.007, < 0.001, and < 0.001, respectively). The serum TSHR Ab levels showed a continuous decrease until 12 weeks after IV GC therapy and exhibited a minimal increase at 2 months of follow-up: 17.50, 11.94, 7.73, and 8.01 IU/L at baseline, 6 weeks, 12 weeks, and 2 months after IV GC therapy, respectively (p = 0.442, 0.015, < 0.001, respectively). Among the extraocular muscles, the SR, IR, and LR thicknesses showed minimal change from the baseline thickness, while the MR thickness markedly decreased at 2 months from the baseline thickness; the IR thickness was reduced, and SR and LR thicknesses were slightly increased at 2 months (p > 0.05). CT showed a continuous reduction from 357.94 μm at baseline to 345.90 μm at 6 weeks, 335.38 μm at 12 weeks, and 300.58 μm at 2 months after IV GC therapy (p > 0.05). CVI showed minimal change; it was 0.63% at baseline, 0.64% at 6 weeks, 0.66% at 12 weeks, and 0.67% at 2 months after IV GC therapy (p > 0.05). sFAZ increased, whereas dFAZ decreased at 2 months compared with the baseline (p > 0.05). The sCPD and dCPD increased after the initiation of IV GC therapy and then showed a decrease (p > 0.05).
Changes in the autoantibody levels, clinical activity scores, and OCT parameters after glucocorticoid therapy. Asterisks indicate a significant difference at *p < 0.05 and **p < 0.01, with p values were calculated using generalized estimating equations. CAS Clinical Activity Score, TSI thyroid stimulating immunoglobulin, TSHR Ab thyroid stimulating hormone receptor autoantibody, SR superior rectus, IR inferior rectus, MR medial rectus, LR lateral rectus, sFAZ superficial foveal avascular zone, dFAZ deep foveal avascular zone, 1 mm fovea sCPD superficial capillary plexus density (sCPD) in a 1-mm-diameter circle from fovea, 3 mm parafovea sCPD mean of sCPD in a 3-mm-diameter circle from the fovea except for the 1-mm fovea sCPD, 1 mm fovea dCPD deep capillary plexus density (dCPD) in a 1-mm-diameter circle from the fovea, 3 mm parafovea dCPD mean of dCPD in a 3-mm-diameter circle from the fovea except for the 1-mm fovea dCPD, CT choroidal thickness, CVI choroidal vascularity index
The correlation of autoantibody levels, CAS, and OCT factors were evaluated using Pearson’s correlation test (Table 3). CAS showed a significant positive correlation with TSI and 3-mm parafoveal sCPD at 6 weeks (p < 0.05 and p < 0.01, respectively). TSHR Ab had a significant positive correlation with TSI at 12 weeks and 2 months after IV GC therapy (p < 0.05 and p < 0.01, respectively), and with CT and CVI at 6 weeks after IV GC therapy (p < 0.05 and p < 0.05, respectively). TSHR Ab also showed a negative correlation with sFAZ and dFAZ at 2 months after IV GC therapy (p < 0.01 and p < 0.05, respectively) and with the thickness of SR at 12 weeks and 2 months after IV GC therapy (p < 0.05 and p < 0.05, respectively).
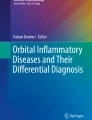
The time points at which the patients’ CAS, TSHR Ab, and TSI stabilized to the normal range after IV GC therapy are indicated using a Kaplan–Meier survival curve in Fig. 3. At 78 days after treatment initiation, the CAS of 50% of our patients had normalized to < 3. Further, TSHR Ab and TSI levels of 75% of our patients decreased to normal at 77 and 126 days after IV GC therapy initiation, respectively. The normal ranges of serum autoantibody levels are as follows: TSHR Ab < 1.5 IU/L, TSI level < 140 SRR%.
Discussion
Medical treatment for moderate-to-severe TED aims to reduce disease activity, reduce muscle involvement, alleviate optic nerve compression, and ultimately decrease the need for rehabilitative surgery [15]. IV GC therapy rapidly and effectively reduces soft-tissue edema and improves clinical parameters, including visual acuity and ocular motility [8, 15, 16]. Inactivation of TED (final CAS ≤ 2) occurred in 59% of cases in nine randomized trials and in 89% of cases in 13 non-randomized trials, and CAS decreased by 2.5 in randomized trials and 3.5 in non-randomized trials [17]. Our results also revealed consecutive improvement in CAS, which was statistically significant. At 12 weeks after IV GC therapy initiation, CAS was < 2, verifying TED inactivation, and an average decrease of 1.5 in CAS was noted. Most of our patients saw a significant improvement in clinical symptoms, with decreased eyelid retraction and proptosis 2 months after IV GC therapy initiation and complete recovery of conjunctival hyperemia and symptoms, including eyelid retraction and proptosis by Hertel exophthalmometry, after 8 months (Electronic Supplementary Material Fig. S1).
As IV GC exerts genomic effects by increasing anti-inflammatory protein expression and nongenomic effects by changing and stabilizing the cellular membrane, the restoration of blood flow and improvement of venous congestion can reasonably be expected at follow-up examinations [18]. Yu et al. reported that the choroidal thickness increased in patients with TED and explained that inflammatory cells infiltrated the choroidal vessels, leading to leakage of exudate and increased intraocular blood flow, which led to an increase in the choroidal thickness [19]. Cagiltay et al. suggested that the choroidal thickness may increase due to orbital vein occlusion and congestion in patients with TED [20]. We expected a decrease in CT and CVI after IV GC therapy. Our result confirmed a continuous reduction in CT with improvement. However, CVI exhibited only minor variance. We believe that CT was reduced because of a systemic pharmacological effect restoring choroidal blood circulation and improving orbital vein congestion. However, a 2-month follow-up appears to be insufficient to trigger structural remodeling of choroidal vessels.
In our study population, sCPD and dCPD initially slightly increased and then decreased following the initiation of IV GC therapy. sFAZ exhibited a continuous increasing tendency, whereas dFAZ showed decreasing tendency. Previous results regarding the changes in retinal microvascular circulation are conflicting. Some studies have insisted that these markers are reduced by the influence of endothelin-1 and, compared with healthy people, the retinal capillaries are destroyed due to inflammation caused by the deposition of autoantibodies in the retinal blood vessels [21]. Conversely, Ye et al. [22] and Perri et al. [23] reported that the retinal blood flow increased during active TED and concluded that the increased retinal capillary density resulted from blood flow delay due to venous congestion. In the present study, the increasing tendency of sFAZ and the reduction in sCPD and dCPD soon after the rise with the initiation of IV GC suggest that the effect of GC is decreased retinal capillary density and improved capillary blood flow. These findings support the latter assertion and demonstrate that, although few retinal capillaries may have been damaged by inflammatory proteins, the recovery of retinal microvascular circulation with the restoration of venous congestion is more noticeable in patients with TED after IV GC therapy.
Extraocular muscle enlargement is a significant alteration in patients with TED, occurring due to the inflammatory reaction in the acute phase or the extraocular muscle fibrosis after inflammation in the chronic phase, leading to restricted eye movements or diplopia [24]. Generally, when an extraocular muscle is involved in active TED, it occurs in the order of IR, MR, SR, and LR, with IR being the most often involved [25]. Cirić et al. found that the enlargement of extraocular muscles was reduced in ten of 14 patients with TED after pulse GC therapy [26]. Xu et al. measured orbital fat and extraocular muscle thickness using magnetic resonance imaging (MRI) and found that the steroid-responsive group had significantly thicker IR muscle than the non-responsive group at baseline [27].
In the present study, we investigated the changes in extraocular muscle thickness using anterior segment OCT and found an improvement of MR and IR muscle thickness at 2 months after IV GC. Our result indicates that the muscles that are the most likely and earliest to swell are the first to improve with IV GC therapy. Furthermore, compared with orbit MRI, anterior segment OCT has the benefit of being able to be performed easily and promptly in ophthalmology clinics. Therefore, the change in MR and IR muscle thickness measured by anterior segment OCT can be safely and non-invasively used as a predictor of response to IV GC therapy.
The autoantibody that plays the most important role in the pathogenesis of TED is TSHR Ab, which is called TBII or TSI, depending on the measurement method. The TSHR Ab level indicates the level of autoantibodies in the microvascular system, which is known to play a role in triggering as well as sustaining autoimmune processes in the eye [28, 29]. TSI measures the functional properties of autoantibodies that stimulate thyroid function in patients with TED and is closely related to the activity and severity of TED [6].
The correlation between the autoantibody levels and TED severity is controversial. Two studies have discovered a positive correlation between TED activity and serum antibody levels after anti-inflammatory therapy. Khoo et al. reported that TSI levels and the absence of antithyroperoxidase antibodies were independent predictors of TED [30]. Eckstein et al. found that the presence of TBII and TSI was associated with a significantly higher severity of TED [28]. Although participants were not differentiated according to therapy, Noh et al. [31] reported that the TSI levels, but not the TBII levels, are related to TED activity, while Gerding et al. [32] confirmed the correlation between the CAS and TSI and TBII levels. Conversely, Kung et al. found no significant correlation between TED exacerbation after radioiodine therapy and TSI levels [33].
In the present study, the serum TSI and TSHR Ab levels showed a continuous decrease in accordance with the reduction in CAS until 2 months of follow-up, except for a slight increase in TSHR Ab levels at 2 months. Furthermore, a significant positive correlation between the activity of TED and serum TSI levels was revealed 6 weeks after initiation of IV GC therapy, which is concordant with the findings of previous studies. We also investigated the correlation between autoantibody levels and chorioretinal capillary perfusion indicators detected by OCT factors and confirmed the improvement of intraocular capillary congestion after IV GC. As the decreases in sCPD and CT indicate the improvement of congestion in the choroid and retinal vessels, and CAS and TSHR Ab levels decreased post-IV GC therapy, the positive correlation between CAS and 3 mm sCPD and those between the TSHR Ab levels and CT and CVI confirm the alleviation of vascular congestion through systemic therapy. The increase in sFAZ and dFAZ indicates decreased congestion of vessels, and the negative correlations between the TSHR Ab levels and sFAZ and dFAZ confirm the improvement of retinal capillary congestion. Therefore, it can be concluded that the decrease in TSI and TSHR Ab levels can be an indicator of restoration of chorioretinal capillary perfusion and improvement of clinical symptoms after IV GC therapy in patients with TED.
To our knowledge, only a limited number of studies have investigated the time point at which the indicators stabilize to the normal range. Eckstein et al. reported a significant decrease in CAS to 1 or 0 at 4.5 months and a reduction in proptosis of > 2 mm 12 months after initiating steroid treatment for TED, with an especially higher decrease in non-smokers [34]. Cirić et al. also found that CAS showed a significant decrease in the first week of pulse GC therapy [26]. A study on children with Graves’ disease reported that the thyrotropin receptor antibody levels of the pulse group were lower than those of the control group on day 30 but rose on day 60 after IV methylprednisolone and oral prednisolone therapy, suggesting that the effect of systemic therapy on thyroid function was temporary [35]. In our study, CAS in 50% of patients and serum TSHR Ab levels in 75% of patients decreased to the normal value at approximately 2.5 months, and the TSI levels decreased to the normal value in 75% of patients at 4 months after IV GC therapy initiation. These results suggest that due to the systemic effect of GC therapy, the CAS and serum TSHR Ab levels decrease first, followed by the TSI levels, and that 2–4 months are required for the clinical and serologic indicators to normalize.
Our study is limited by the relatively small number of patients and the short follow-up time, which might have influenced the evaluation of efficacy outcomes. Moreover, the interpretation of the choroidal vascular index and serum autoantibody levels might have been complicated by the wide range of participants’ age. As serum autoantibodies and chorioretinal vessels change sensitively in a time-dependent manner, we intend to conduct further research on these patients. Furthermore, as the poor OCT and OCT-A image quality may have resulted in the presence of artifacts, we have excluded such cases to minimize bias.
Conclusion
Despite the limitations mentioned above, this study is significant in that we prospectively investigated the changes in serum autoantibody levels, clinical symptoms, and eyeball anatomy in patients with TED and their correlation after IV GC therapy, a field that is currently understudied. Systemic IV GC therapy resulted in overall improvement of CAS and chorioretinal blood flow and normalization of serum TSHR Ab and TSI level at 2 months after therapy initiation in patients with TED. Furthermore, it can be concluded that the decrease in the serum TSI and TSHR Ab levels is correlated with restoration in chorioretinal capillary perfusion and improvement of clinical symptoms and extraocular muscle thickness, suggesting that the serologic factors and non-invasive OCT findings can be a predictor to indicate response to IV GC therapy.
Change history
08 May 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40123-023-00722-z
References
Mizen TR. Thyroid eye disease. Semin Ophthalmol. 2003;18:243–7.
Garrity JA, Bahn RS. Pathogenesis of graves ophthalmopathy: implications for prediction, prevention, and treatment. Am J Ophthalmol. 2006;142:147–53.
Bahn RS. Graves’ ophthalmopathy. N Engl J Med. 2010;362:726–38.
Zöphel K, Roggenbuck D, Schott M. Clinical review about TRAb assay’s history. Autoimmun Rev. 2010;9:695–700.
Tahara K, Ishikawa N, Yamamoto K, et al. Epitopes for thyroid stimulating and blocking autoantibodies on the extracellular domain of the human thyrotropin receptor. Thyroid. 1997;7:867–77.
Lytton SD, Kahaly GJ. Bioassays for TSH-receptor autoantibodies: an update. Autoimmun Rev. 2010;10:116–22.
Michelangeli VP, Munro DS, Poon CW, Frauman AG, Colman PG. Measurement of thyroid stimulating immunoglobulins in a new cell line transfected with a functional human TSH receptor (JPO9 cells), compared with an assay using FRTL-5 cells. Clin Endocrinol (Oxf). 1994;40:645–52.
Bartalena L, Baldeschi L, Boboridis K, et al. The 2016 European Thyroid Association/European Group on Graves’ orbitopathy guidelines for the management of Graves’ orbitopathy. Eur Thyroid J. 2016;5:9–26.
Marcocci C, Bartalena L, Tanda ML, et al. Comparison of the effectiveness and tolerability of intravenous or oral glucocorticoids associated with orbital radiotherapy in the management of severe Graves’ ophthalmopathy: results of a prospective, single-blind, randomized study. J Clin Endocrinol Metab. 2001;86:3562–7.
Kahaly GJ, Pitz S, Hommel G, Dittmar M. Randomized, single blind trial of intravenous versus oral steroid monotherapy in Graves’ orbitopathy. J Clin Endocrinol Metab. 2005;90:5234–40.
Hamzah F, Shinojima A, Mori R, Yuzawa M. Choroidal thickness measurement by enhanced depth imaging and swept-source optical coherence tomography in central serous chorioretinopathy. BMC Ophthalmol. 2014;14:145.
Mourits MP, Prummel MF, Wiersinga WM, Koornneef L. Clinical activity score as a guide in the management of patients with Graves’ ophthalmopathy. Clin Endocrinol (Oxf). 1997;47:9–14.
Agrawal R, Gupta P, Tan KA, Cheung CM, Wong TY, Cheng CY. Choroidal vascularity index as a measure of vascular status of the choroid: Measurements in healthy eyes from a population-based study. Sci Rep. 2016;6:21090.
Häner NU, Dysli M, Abegg M, Zinkernagel MS. Enhanced-depth optical coherence tomography for imaging horizontal rectus muscles in Graves’ orbitopathy. Graefes Arch Clin Exp Ophthalmol. 2015;253:1569–73.
Marcocci C, Marinò M. Treatment of mild, moderate-to-severe and very severe Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab. 2012;26:325–37.
Bartalena L, Krassas GE, Wiersinga W, et al. Efficacy and safety of three different cumulative doses of intravenous methylprednisolone for moderate to severe and active Graves’ orbitopathy. J Clin Endocrinol Metab. 2012;97:4454–63.
Zang S, Ponto KA, Kahaly GJ. Clinical review: intravenous glucocorticoids for Graves’ orbitopathy: efficacy and morbidity. J Clin Endocrinol Metab. 2011;96:320–32.
Schwartz N, Verma A, Bivens CB, Schwartz Z, Boyan BD. Rapid steroid hormone actions via membrane receptors. Biochim Biophys Acta. 2016;1863:2289–98.
Yu N, Zhang Y, Kang L, Gao Y, Zhang J, Wu Y. Analysis in choroidal thickness in patients with Graves’ ophthalmopathy using spectral-domain optical coherence tomography. J Ophthalmol. 2018;2018:3529395.
Cagiltay E, Akay F, Demir O, Aydın E, Akmaz B, Pamuk B. The increment of choroidal thickness in euthyroid graves’ ophthalmopathy: is it an early sign of venous congestion. J Ophthalmol. 2018;2018:5891531.
Wu Y, Tu Y, Bao L, et al. Reduced retinal microvascular density related to activity status and serum antibodies in patients with Graves’ ophthalmopathy. Curr Eye Res. 2020;45:576–84.
Ye L, Zhou SS, Yang WL, et al. Retinal microvasculature alteration in active thyroid-associated ophthalmopathy. Endocr Pract. 2018;24:658–67.
Perri P, Campa C, Costagliola C, Incorvaia C, D’Angelo S, Sebastiani A. Increased retinal blood flow in patients with active Graves’ ophthalmopathy. Curr Eye Res. 2007;32:985–90.
Lennerstrand G, Tian S, Isberg B, et al. Magnetic resonance imaging and ultrasound measurements of extraocular muscles in thyroid-associated ophthalmopathy at different stages of the disease. Acta Ophthalmol Scand. 2007;85:192–201.
Imbrasienė D, Jankauskienė J, Stanislovaitienė D. Ultrasonic measurement of ocular rectus muscle thickness in patients with Graves’ ophthalmopathy. Medicina (Kaunas). 2010;46:472–6.
Cirić J, Zarković M, Stojanović M, et al. Treatment of Grave’s ophthalmopathy with high doses of corticosteroids. Srp Arh Celok Lek. 2000;128:179–83 (Article in Serbian).
Xu L, Li L, Xie C, Guan M, Xue Y. Thickness of extraocular muscle and orbital fat in MRI predicts response to glucocorticoid therapy in Graves’ ophthalmopathy. Int J Endocrinol. 2017;2017:3196059.
Eckstein AK, Plicht M, Lax H, et al. Thyrotropin receptor autoantibodies are independent risk factors for Graves’ ophthalmopathy and help to predict severity and outcome of the disease. J Clin Endocrinol Metab. 2006;91:3464–70.
Bahn RS, Dutton CM, Natt N, Joba W, Spitzweg C, Heufelder AE. Thyrotropin receptor expression in Graves’ orbital adipose/connective tissues: potential autoantigen in Graves’ ophthalmopathy. J Clin Endocrinol Metab. 1998;83:998–1002.
Khoo DH, Ho SC, Seah LL, et al. The combination of absent thyroid peroxidase antibodies and high thyroid-stimulating immunoglobulin levels in Graves’ disease identifies a group at markedly increased risk of ophthalmopathy. Thyroid. 1999;9:1175–80.
Noh JY, Hamada N, Inoue Y, Abe Y, Ito K, Ito K. Thyroid-stimulating antibody is related to Graves’ ophthalmopathy, but thyrotropin-binding inhibitor immunoglobulin is related to hyperthyroidism in patients with Graves’ disease. Thyroid. 2000;10:809–13.
Gerding MN, van der Meer JW, Broenink M, Bakker O, Wiersinga WM, Prummel MF. Association of thyrotrophin receptor antibodies with the clinical features of Graves’ ophthalmopathy. Clin Endocrinol (Oxf). 2000;52:267–71.
Kung AW, Yau CC, Cheng A. The incidence of ophthalmopathy after radioiodine therapy for Graves’ disease: prognostic factors and the role of methimazole. J Clin Endocrinol Metab. 1994;79:542–6.
Eckstein A, Quadbeck B, Mueller G, et al. Impact of smoking on the response to treatment of thyroid associated ophthalmopathy. Br J Ophthalmol. 2003;87:773–6.
Hu Y, Man Y, Sun X, Xue Y. Effects of glucocorticoid pulse therapy on thyroid function and thyroid antibodies in children with graves’ disease. Ital J Pediatr. 2021;47:46.
Acknowledgements
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2021R1G1A1003971). The funder had no role in the design of the study or collection, analysis, or interpretation of data or in writing the manuscript. The Rapid Service Fee was funded by the “The National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2021R1G1A1003971)”.
Medical Writing, Editorial, and Other Assistance
Editage (https://www.editage.com/) is acknowledged for English language editing.
Author Contributions
Dong Cheol Lee analyzed the data and designed the study. Jaekyoung Lee contributed to the writing of the manuscript. All authors read and approved the manuscript.
Disclosures
Jaekyoung Lee and Dong Cheol Lee declare that they have no competing interests.
Compliance with Ethics Guidelines
All patients provided written informed consent for study participation and publication of their data. The study was performed in accordance with the 1964 Declaration of Helsinki and its later amendments, and was approved by the Institutional Review Board of the Keimyung University Hospital (approval number: 2021-02-046). The consent for Supplementary Material Fig. 1 was obtained from the patient.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised to correct the funding note.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lee, J., Lee, D.C. Changes in Clinical Activity, Serum Autoantibody Levels, and Chorioretinal Vessels After Systemic Glucocorticoid Therapy in Thyroid Eye Disease. Ophthalmol Ther 12, 1851–1863 (2023). https://doi.org/10.1007/s40123-023-00696-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00696-y