Abstract
Introduction
To profile conjunctival T cell populations in allogeneic hematopoietic stem cell transplant (HSCT) patients after instillation of daily topical cyclosporine-A (CsA) 0.1% cationic emulsion (Ikervis), and to evaluate patients’ tolerance to these eye drops.
Methods
Nineteen participants were prescribed Ikervis prophylaxis once daily to both eyes from 3–5 weeks pre-HSCT to 12 months post-HSCT. The outcome measure was conjunctival T cell proportions from flow cytometry after impression cytology. Covariates included visual acuity, intraocular pressure, slit lamp and fundal examination, dry eye (SPEED) and quality of life questionnaires, non-invasive keratograph tear break-up time (NIKBUT), conjunctival redness, meibography, lipid thickness, Schirmer test, tear cytokines, fluorescein staining, tear osmolarity, and meibomian gland expressibility.
Results
The conjunctival T cell analysis showed either stable or decreased proportions of conjunctival CD4 T cells at the last visit from baseline in compliant patients. CD4 proportions were increased in non-compliant patients and in the single patient who developed ocular graft-versus-host disease (GVHD). All patients were tolerant to Ikervis but 6/19 were not compliant. In the majority of patients, vision did not affect activities of daily living. Pre- and post-HSCT up to the last study visit, there was no statistically significant change in clinical covariates. Only one participant developed ocular GVHD at 9 months post-HSCT.
Conclusion
Superficial conjunctival T cell profile reflects compliance to daily topical Ikervis eye drops and clinical ocular surface parameters in allogenic HSCT patients. Tolerance is comparable to other formulations of topical CsA in the first 12 months.
ClinicalTrials.gov Identifier
NCT04636918. URL: https://clinicaltrials.gov/ct2/show/NCT04636918?cond=ocular+Graft+Versus+Host+Disease&cntry=SG&draw=2&rank=2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? | |
The use of topical cyclosporine-A eye drops prophylactically in hematopoietic stem cell transplant (HSCT) patients to prevent ocular graft-versus-host disease has been shown to be promising. However, the conjunctival T cell profile in these patients has never been analyzed before. | |
This study aims to profile conjunctival T cell populations in HSCT patients after instillation of daily topical cyclosporine-A 0.1% cationic emulsion (Ikervis), and to evaluate patients’ tolerance to these eye drops. | |
What was learned from the study? | |
CD4 T cell counts were either stable or decreased in patients compliant to Ikervis. CD4 counts increased in those who were non-compliant or developed ocular graft-versus-host disease (GVHD). Tolerance of Ikervis was comparable to other formulations of topical cyclosporine-A (CsA). | |
This study is the first to characterize immunological changes in the conjunctiva following topical cyclosporine eye drops in HSCT patients, giving us a better understanding of its mechanism of action. With promising results in terms of efficacy and tolerance, topical cyclosporine has the potential to be a mainstay preventative treatment in HSCT patients for the prevention of ocular GVHD. |
Introduction
Dry eye disease (DED) is a common ocular sequela of graft-versus-host disease (GVHD) after allogeneic hematopoietic stem cell transplantation (allo-HSCT), with one study showing more than 40% of allo-HSCT patients developing chronic ocular GVHD [according to both National Institutes of Health (NIH) consensus criteria and the International Chronic Ocular GVHD Consensus Group] [1]. Acute GVHD is defined as occurring within the first 100 days post-HSCT and chronic GVHD occurs after 100 days. The mean duration between allo-HSCT and the onset of ocular GVHD is approximately 7.5 months [2]. In patients with systemic GVHD after allo-HSCT, the cumulative incidence of patients with DED rose to 73% at 2.5 years follow-up, with a median time to developing dry eyes of 10 months [3].
The pathogenesis of DED in GVHD involves T cell-mediated infiltration and inflammation of lacrimal gland, conjunctiva, ocular surface resulting in scarring of lacrimal gland and conjunctiva, decrease in conjunctival goblet cells, and decreased tear production [4,5,6]. There is also meibomian gland obstruction and anterior and posterior blepharitis [7, 8]. Once fibrosis develops in the lacrimal gland, it is irreversible and the patient is left with significant permanent DED [6]. Conjunctival T cells include both CD4 helper T lymphocytes and CD8 cytotoxic T lymphocytes. Previous literature shows that CD8 cells exceed CD4 in the conjunctival epithelium [9] and the ratio of CD4/CD8 decreased after dry eye treatment [10]. These previous studies looked at T cell changes using conjunctival biopsies, which is invasive and the technique uses immunostaining. We employ a less invasive technique on the bulbar conjunctiva and more accurately quantify longitudinal changes using a flow cytometric assay.
Given the high incidence of DED in allo-HSCT patients, investigating preventive measures of DED in this population is beneficial. Topical cyclosporine-A (CsA) has been reported to be safe and efficacious in the treatment of DED associated with chronic GVHD [11,12,13]. However, there are few reports on topical CsA in the prophylaxis of ocular GVHD [14,15,16]. Three prophylactic regimes have been reported. Malta et al. reported on a retrospective case control study with 81 patients treated with Restasis twice daily (BD) (0.05% CsA, Allergan) [14], Chun et al. performed a prospective randomized controlled trial with a 3-month follow-up of 28 patients treated with Restasis four times a day (QDS) (topical cyclosporine 0.05%, Allergan) [15], and Cantu-Rodriguez et al. performed a longitudinal observational prospective study on 20 patients treated with Modusik-A (0.1% CsA) BD [16]. Whilst these results were promising and showed no significant adverse effects, the effect of topical cyclosporine prophylaxis on conjunctival T cells has not previously been studied. Also, none of these studies use the cationic emulsion form of topical cyclosporine such as Ikervis. Compared with other formulations of topical cyclosporine, cationic emulsions have been shown to be more poorly tolerated in patients with ocular GVHD, with 62% of patients intolerant to cationic emulsion, compared with 33% for castor oil and 39% for liposomal. In DED, however, the cationic emulsion formulation was the most well-tolerated, with only 32% intolerant compared with 47% for castor oil and 63% for liposomal [17]. It is therefore important to investigate the tolerance in our population of patients post-HSCT.
In this prospective interventional single-arm study, our aims are to profile conjunctival T cell populations in allogeneic hematopoietic stem cell transplant patients after instillation of daily topical cyclosporine-A 0.1% cationic emulsion, and to evaluate patients’ tolerance to these eye drops.
Methods
Design
This is an open-label, single-arm interventional study performed at the Singapore National Eye Centre (SNEC) in collaboration with the Haematology Department at the Singapore General Hospital (SGH).
Study Population
Patients who underwent allo-HSCT at the Haematology Department, SGH, between November 2019 and September 2021 were recruited. All participants provided written informed consent. Our study adhered with the tenets of the Declaration of Helsinki on human research and was prospectively reviewed and approved by the SingHealth Centralised Institutional Review Board (reference number: 2019/2635). The study was registered in the Clinical Trials database (NCT04636918).
Eligibility
The following patients were excluded from participation in this study: age below 13 years, the presence of other concurrent ocular or systemic disease that may interfere with study results, non-resident patients who were unable to complete follow-up, and existing users of topical cyclosporine eye drops.
Study Intervention
Participants were prescribed topical cyclosporine-A 0.1% (Ikervis, Santen) prophylaxis once daily to both eyes and preservative-free sodium hyaluronate 0.3% (Hialid Mini, Santen) lubricating eye drop to be used pro re nata (PRN) from 3–5 weeks prior to allo-HSCT to 12 months after allo-HSCT. Depending on the transplant protocol used, participants received systemic GVHD prophylaxis with systemic CsA or tacrolimus therapy combined with a course of methotrexate or mycophenolate. Antithymocyte globulin (ATG) or post-transplant cyclophosphamide was added to the above regime in cases of unrelated/ sibling donor with antigen mismatch or haploidentical transplant, respectively (refer to Supplementary Table 1 for the individualized GVHD prophylaxis regimen used for each patient).
Conjunctival T Cell Profile
Characterization of Conjunctival T Cells by Flow Cytometry
After instillation of local anesthesia, impression cytology was performed using EyePRIM (Opia Technologies) as described [18]: conjunctival sampling was performed for both the superionasal bulbar conjunctiva and superiotemporal bulbar conjunctiva by asking the participant to look inferiotemporally and inferionasally, respectively, and placing the EyePRIM membrane to the area, ensuring good apposition with the conjunctiva. The two membranes from different conjunctival areas of the same eye were subsequently soaked in an Eppendorf tube containing 1.5 ml of Roswell Park Memorial Institute (RPMI) medium and placed in an ice box. Using a 10 μl micropipette tip, the cells were scraped off the membrane and into the RPMI medium. The Eppendorf tubes containing the scraped membrane and RPMI medium were transported in ice to the laboratory for processing, and the samples were analyzed within 2 h.
Collected cells were centrifuged at 500 rpm for 10 min. Cells from two eyes were combined into one 1.5 ml centrifuge tube and washed with 1 ml of staining buffer [phosphate-buffered saline (PBS) with 0.1% bovine serum albumin (BSA)]. After centrifuging at 500 rpm for 10 min, the cells were resuspended in 50 μl of staining buffer. Other antibodies were then added to the cells and incubated at room temperature for 20 min. Staining buffer (1 ml) was added to the cells, and then the cells were centrifuged at 500 rpm for 10 min. Stained cells were resuspended in 200 μl of staining buffer and analyzed by a BD FACSVerse flow cytometer. Data collection and analysis were performed with BD FACS suite software. All antibodies were purchased from BD Bioscience, Singapore: Anti-CD45-APC-H7 (clone 2D1), anti-CD3-BV510 (clone UCHT1), and anti-CD8-FITC (clone SK1). Cell viability solution 7-aminoactinomycin (7-AAD) was also purchased from BD Bioscience, Singapore.
Assessment of Tolerance/Compliance to Ikervis
The number of patients who were not tolerant to Ikervis instillation were noted. For those who were tolerant, the definition of compliance to the use of Ikervis in this study was more than 70% used, and/or less than five blocks of three consecutive days of not using Ikervis eye drops. Compliance was assessed by looking at the diary chart that all participants were asked to keep, as well as checking the leftover supply of eye drops.
Clinical Covariates
Clinical covariates were recorded at 3–5 weeks prior to allo-HSCT; immediately before allo-HSCT; 3, 6, and 12 months post allo-HSCT; and at ad hoc visits.
Clinical covariates included visual acuity, intraocular pressure, slit lamp examination, fundal examination, dry eye and quality-of-life questionnaire administration, non-invasive keratograph tear break-up time (NIKBUT), conjunctival redness, meibography, lipid thickness, Schirmer test, tear cytokines, fluorescein staining, tear osmolarity, and meibomian gland expressibility.
Table 1 presents the outcome variables and clinical covariates measured at different time points throughout the study. The flow of tests were designed to get the most accurate findings of the tears and ocular surface with minimal disturbance of the tear film from the previous test. Tests were performed in the following sequence: NIKBUT, conjunctival redness, tear osmolarity, lipid layer thickness, Schirmer test, impression cytology, slit lamp examination, corneal staining photo, meibomian gland expressibility, infrared meibography, and lastly fundus examination. Annex A elaborates on the detailed methodology used in this study for the outcome variables.
Dry Eye Questionnaire
The dry eye questionnaire used in this study was the previously validated standard patient evaluation of eye dryness (SPEED) questionnaire, which consists of two questions on the frequency and severity of dry eye, graded on a scale of 0–3 on frequency and 0–4 on severity. Scores from all subquestions were added, and the greater the total score (0–28), the more frequent or severe the dry eye [19]. The average SPEED score was 6.25 for asymptomatic patients and 21.00 for symptomatic patients in the validated study. [19]
NIKBUT and Conjunctival Redness
The Oculus Keratograph 5M (Oculus, Wetzlar, Germany) was used to perform the NIKBUT and to measure conjunctival redness [20, 21]. In a study from Japan, the average NIKBUT was 9.7 ± 6.7 s for normal eyes and 4.6 ± 1.3 s for dry eyes [22]. A study from China showed an average NIKBUT of 4.3 ± 0.3 s for normal eyes and 2.0 ± 0.2 s for dry eyes [23]. The conjunctival hyperemia Jenvis grading scale from 0 to 4 was used, with higher grades indicating increased hyperemia.
Infrared Meibography
Infrared meibography was performed as described by Arita et al., with the exception that the Oculus Keratograph 5M (Oculus, Wetzlar, Germany) was used [24]. Meibomian gland disease (MGD) was graded as follows: 0, no loss of meibomian glands; 1, lost area was less than one-third of the total area of meibomian glands; 2, lost area was between one-third and two-thirds of the total area of meibomian glands; 3, lost area was over two-thirds of the total area of meibomian glands.
Corneal Fluorescein Staining
Corneal fluorescein staining was imaged by the Oculus Keratograph 5M (Oculus, Wetzlar, Germany) and graded using the Cornea and Contact Lens Research Unit (CCLRU) scale, dividing the cornea into five zones and grading each zone from 0 to 4, with 0.5 unit intervening steps, and a greater number indicating more intense or greater area of staining. [25]
Tear Osmolarity
The TearLab system (OcuSense, San Diego, CA) was used to measure tear osmolarity [26]. Tear osmolarity is the single best indicator of the severity of DED. Elevated tear osmolarity has been found to be highly correlated to dry eye disease severity, with test-to-test variability and inter-eye differences characteristic [27,28,29]. In this study, a tear osmolarity value > 305 mOsm/L was considered high.
Lipid Layer Thickness
Lipid layer thickness of the tear film was assessed using an interferometer (LipiView ocular surface interferometer, TearScience Inc, Morrisville, NC). The average lipid layer thickness was 67 nm (range 33–100 nm) in normal eyes. [30]
Schirmer Test and Tear Cytokine Evaluation
The Schirmer test was done with standard 5 mm wide test strips (Clement Clarke), with a notch for folding, without prior anesthesia for 5 min. According to the Asia Dry Eye Society consensus, a Schirmer value less than or equal to 5 mm in 5 min is considered aqueous tear deficient [31]; between 5 and 10 mm is considered moderate aqueous tear deficient [34]; and a Schirmer value of more than 10 mm is considered normal. In this study, participants were considered to have higher baseline Schirmer scores if their Schirmer values were more than 8 mm, which is the median value of moderate aqueous tear-deficient patients. The Schirmer test strips were subsequently stored and tear proteins eluted for tear cytokine evaluation using the multiplex bead-based indirect immunofluorescent assay (Milliplex, Merck-Millipore, Billerica, MA) [32].
Meibomian Gland Expressibility
Meibomian glands were assessed by gently squeezing the lower eyelids using a device that delivers standardized pressure to the eyelids (Meibomian gland expressor, TearScience, France). The texture of the expressed secretion was graded as liquid or viscous, and the number of expressible glands were recorded.
QoL Questionnaire
Participants also completed the Impact of Vision Impairment Profile, a quality-of-life (QoL) questionnaire [33].
Statistical Analysis
Only the right eye from each participant was analyzed to avoid the influence of high correlation between eyes. Associations between continuous variables were assessed using unpaired or paired t-tests as appropriate. Associations between categorical or ordinal variables were performed using the Chi-square or Fisher’s exact probability tests as appropriate. The level of statistical significance was at an alpha of 0.05.
Sample Size Calculation
As there are no previous papers on the effect of daily prophylactic topical cyclosporine on conjunctival T cell profile in HSCT patients, the required effect size is unknown. Hence, we calculated the sample size based on what is needed to show a reduction in ocular complications compared with other untreated (no topical cyclosporine) series in the literature.
Based on a previous study, the 95% confidence interval of the proportion of ocular GVHD within 1 year (NIH criteria) is 0.453–0.584 [1], (https://sample-size.net/confidence-interval-proportion/). Assuming 80% power and alpha of 0.05, the rate of ocular chronic GVHD with prophylaxis would be two cases out of 21 in the first year or less. If 3/21 patients develop ocular GVHD, the rate of treatment success would not be significantly different from cases without prophylaxis reported in Berchicci et al. [1]
Assuming that we accept two patients to develop ocular GVHD, we would need to recruit at least 14 participants (0.0178–0.428) for a significantly lower proportion of cases when given prophylaxis in our study (since the upper limit 0.428 is less than 0.453, the lower limit of the previous study) [1]. This proportion of 14.3% would be significantly lower than 51.9% of the previous study [1] (Fisher’s exact probability test; p = 0.0107). However, to account for potential dropouts or loss to follow-up, we recruited an additional five patients, or 19 patients in total (https://www.graphpad.com/quickcalcs/contingency2/). In this scenario, if the rate of ocular GVHD is 5/19 or 26.3% (no loss to follow-up), it would still be significantly less than the historical 51.9%.
Results
A total of 19 eyes of 19 patients were enrolled into this study and given topical CsA pre-treatment 3–5 weeks prior to allo-HSCT. The indication for allo-HSCT and the systemic GVHD prophylaxis regimen in each of these patients is described in Supplementary Table 1. None of the patients were lost to follow-up. The 19 patients were followed-up for a median of 12 months and a mean of 12 months (Fig. 1). Patients had a mean age of 48.8 years \(\pm\) 13.5, 36.8% of patients were female, 78.9% were Chinese, and 15.8% were Malay. (Supplementary Table 2).
Conjunctival T Cells
We report the results of the first ten patients whose conjunctival immune cells were harvested and T cells successfully quantified before and after allotransplantation. Nine subjects were not included in this analysis, and the reasons are presented in Supplementary Table 3. The first harvest was 2–4 weeks after commencement of topical Ikervis and before the allotransplantation. The timing of the second harvest was at the end of the study (12 months) or at 6 months (if no ocular GVHD occurred). In the event that ocular GVHD occurred, the harvesting was obtained at the time of detection of the ocular GVHD, within the study period.
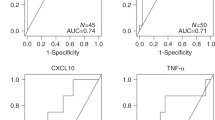
The gating strategy for examining the T cells is shown in Figs. 2 and 3. In this study, we were able to quantify the proportion of CD8+ and CD4+ conjunctival T cells, among the live CD45+CD3+ T lymphocytes. Here, we assumed that CD3+CD8− T cells are primary CD4 cells.
Interestingly, we observed two different change profiles within these ten patients. The exact proportions of CD4 and CD8 T cells in the ten patients at each of the two harvests are presented in Table 2. In profile 1 (six patients), there is a distinct drop of the proportion of conjunctival CD4 T cells, or the proportion remained similar to the baseline proportions. Figure 2 shows the scatter diagrams of the conjunctival cell marker profile for one representative patient from profile 1. All of these patients were compliant to the CsA during the study period. Since none of these patients had ocular GVHD, we deduced that CsA has been effective in keeping the conjunctival T cells from being activated.
In profile 2 (four patients), there is a significant and marked elevation of the proportion of conjunctival CD4 T cells during the re-harvesting, compared with the baseline proportions. Figure 3 shows the scatter diagrams of the conjunctival cell marker profile for one representative patient from profile 2.
Two of these patients in profile 2 were non-compliant to topical CsA. One of these patients developed ocular GVHD that required additional ocular treatment (described below). The last patient, interestingly, had moderately severe corneal staining (grade 2 of CCLRU) prior to allotransplantation, suggesting that he may have asymptomatic compromise of the ocular surface even though he did not reach the diagnostic criteria for dry eye. Even though this patient did not have flare-ups of ocular symptoms or signs in the study period, we would be observing him long term, since ocular GVHD can occur many years after transplantation.
Supplementary Table 1 shows that four of profile 1 patients but none of profile 2 patients had used oral mycophenolic sodium/ mofetil. Profile 1 also had one patient who had cyclophosphamide while profile 2 did not. Both profiles had patients using systemic cyclosporine and methotrexate. Acute systemic GVHD occurred in similar proportions in both profiles.
Tolerance and Compliance
All patients were tolerant to Ikervis and none of the patients withdrew from the study due to intolerance. Within the study period, 13/19 (68.4%) of the participants were compliant to the study CsA eye drops. Six participants used less than 70% of the CsA eye drops and out of these six participants, one participant failed to use CsA over five blocks of three consecutive days. As per the Impact of Vision Impairment (IVI) questionnaire administered, the vision of the majority of the patients does not affect their activities of daily living. For general and near activity, > 90% of patients were unaffected. In terms of emotional impact, > 80% were unaffected (Fig. 4).
Clinical Covariates
Pre-HSCT, the mean NIKBUT, conjunctival redness, tear osmolarity, lipid thickness, Schirmer test, and SPEED scores for the participants were within the normal range (Table 3). Post-HSCT, there was no statistically significant difference in the NIKBUT, conjunctival redness, lipid thickness, corneal fluorescein staining, meibomian gland expressibility, Schirmer test, or SPEED scores (all p > 0.05; paired t-test and Wilcoxon signed rank test) (Table 3). Supplementary Table 4 presents the visit when the laboratory tests (Schirmer test, NIKBUT, impression cytology, etc.) were last performed, but all patients were followed-up for occurrence of ocular symptoms up to 12 months. Only one patient developed ocular GVHD within the 12 month period. Out of all our participants, six (31.6%) had NIKBUT scores < 5 s pre-HSCT, consistent with dry eye. The number of participants with NIKBUT scores < 5 s remained the same post-HSCT. Participants were divided into groups of high (> 305 mOsm/L) versus low (≤ 305 mOsm/L) tear osmolarity and high (> 8 mm/5 min) versus low (≤ 8 mm/5 min) Schirmer tests, and an unpaired t-test analysis was performed to look for a difference in outcomes between the two groups. No difference in any of the outcomes was found (all p > 0.05).
On meibomian gland imaging, 15.8% of participants had healthy meibomian gland status, 57.9% had intermediate status, and 26.3% had unhealthy status. Post-HSCT, the meibomian gland status in all patients remained unchanged (Fig. 5; Table 4).
Out of all the participants, only one developed chronic ocular GVHD at 9 months post-HSCT (according to the NIH consensus criteria) [34], ten participants developed acute systemic GVHD of varying grades, and three participants developed chronic systemic GVHD of varying severity. The participant who developed ocular GVHD also developed grade 3 acute systemic GVHD at 3 months post-HSCT, which progressed to chronic GVHD of moderate severity. At the 3–5 week pre-HSCT visit, this participant did not have any signs or symptoms of dry eye apart from a decreased NIKBUT score in the right eye (Table 5). Specifically, he scored 0 on the CCLRU corneal fluorescein staining (indicating no staining) in all five components of both right and left corneas. Conjunctival redness scores were also low: 0.9 in the right eye and 1.0 in the left eye (Fig. 6). At 6 months post-HSCT, while he was asymptomatic, NIKBUT and Schirmer scores were reduced and the average CCLRU in each component was 1.3 (range 0–3) in the right eye and 2.0 (range 1–4) in the left eye. Conjunctival redness scores were also increased to 1.1 in the right eye and 1.2 in the left (Table 5). At 9 months post-HSCT, he complained of left eye pain, discomfort, and foreign body sensation, and was examined during an ad hoc visit. He was diagnosed with ocular GVHD of both eyes after slit lamp examination, with chemosis and corneal macroerosions seen in both eyes. The average CCLRU corneal fluorescein staining was 3 (range 2–4) in the right eye and 3.8 (range 3–4) in the left eye (Table 5). In addition to topical CsA, one drop of levofloxacin 0.5% (Cravit, Santen Pharmaceuticals Pte Ltd, Japan) four times a day to both eyes and one drop of 0.1% dexamethasone minims (Bausch & Lomb, UK) to both eyes four times a day for 1 week and three times a day for the subsequent week were given and the participant was seen again 2 weeks later. At subsequent follow-up visits, the dexamethasone minims were tapered off and stopped, together with cravit in the right eye, the dexamethasone minims were replaced with fluorometholone (Allergan, USA) twice a day in the left eye due to persistence of staining in the left eye. He was subsequently followed-up for ocular GVHD in SNEC after the 12-month study period.
Discussion
In this paper, we show that the conjunctival helper-T cell (CD4) population changed within a few months, in a way that is associated with compliance to the topical CsA or to the clinical outcome response (ocular GVHD). Previous studies have shown that older people and people with severe dry eye have higher levels of effector T lymphocytes [35]. Our observation that helper-T cells are increased in proportion in patients who developed ocular GVHD or who were non-compliant to CsA deserves confirmation in a larger number of patients, as well as further characterization on the activation status of these lymphocytes. In the single patient with moderate cornea staining before allo-HSCT, there may already be preexisting conjunctival T cell activation (even asymptomatic), or there may be a breakdown in the epithelial barrier function, which may predispose to autoantigen presentation to dendritic cells, as suggested previously. Such patients might require more than topical CsA to prevent the elevation of conjunctival T cells after allo-HSCT.
Table 6 presents some studies on conjunctival T cells. Most studies are different from our current study and involve conjunctival biopsies rather than impression cytology, which was used in our study. Arnous et al. analyzed lymphocytes obtained from the deeper conjunctiva, whereas our study only analyzed superficial epithelial lymphocytes [36]. The advantage of impression cytology is that we can perform it repeatedly, unlike biopsies.
Topical 0.1% cationic emulsion CsA (Ikervis) once a day (OM) has not previously been studied in the prophylaxis of ocular GVHD. The only three previous studies that studied the effectiveness of topical CsA in the prophylaxis of ocular GVHD used topical 0.05% anionic emulsion CsA (Restasis) BD [14], QDS [15], and topical 0.1% non-emulsion CsA (MODUSIK-A) two drops BD [16]. Out of these three papers, only Cantu-Rodriguez et al. reported the tolerance and compliance of topical CsA—one out of 20 patients was intolerant and three out of 20 were non-compliant [16]. In our study, none out of the 19 patients were intolerant and 6 out of the 19 patients were non-compliant. Tolerance to topical cationic CsA (in our study) appears similar or better compared with emulsion CsA (Cantu-Rodriguez et al.) [16], though compliance (in our study) was worse.
Topical CsA treatment was well-tolerated in all of our patients, even in the patient who subsequently developed ocular (o)GVHD. However, in a paper by Gehlsen et al., patients with DED and oGVHD were found to have poor tolerance to topical 0.1% cationic CsA preparation, with 32% and 62% discontinuing the medication in DED and oGVHD patients, respectively [17]. In the SANSIKA study, topical 0.1% cationic CsA was evaluated in patients with severe DED. Compared with the control group who instilled the vehicle only, those who instilled topical cationic CsA had a significantly higher proportion of instillation site pain (29.2% CsA group versus 8.9% vehicle group). Other adverse events in similar proportions in both control and treatment groups were eyelid edema, instillation site erythema, photophobia, eye irritation, and reduced visual acuity [37]. In this paper, we suggest the use of topical 0.1% CsA prophylactically pre-HSCT before the DED or oGVHD symptoms develop, hence topical CsA may be more tolerable in our patients.
Previous studies have analyzed the effectiveness of topical CsA in preventing ocular GVHD based on historical controls (Cantu-Rodriguez et al.) [16]. Although this is not our main aim, with reference to historical data, our findings suggest that topical CsA 0.1% (Ikervis, Santen) once a day prophylaxis starting 3–5 weeks pre-HSCT may be effective in preventing the development of ocular GVHD. Only one out of 19 participants (5.26%) in our study developed chronic ocular GVHD at a mean of 12 months post-HSCT. This percentage is significantly lower (p < 0.001, Fischer’s exact test, two-sided p-value) compared with a study by Berchicci et al., which found that 51.9% of participants who underwent HSCT without any CsA prophylaxis developed dry eye disease at 1 year of follow-up [1]. Other studies by Shikari et al. and Westeneng et al. showed that 64% and 54% of patients developed chronic ocular GVHD, respectively [38, 39]. Furthermore, despite the relatively high incidence of acute systemic GVHD in ten participants and chronic GVHD in three participants, the low incidence of eye involvement is a noteworthy finding.
Only three previous studies have explored the use of topical CsA prophylaxis in GVHD, showing similar results. Malta et al. performed a comparative case series of 105 patients, 81 of whom received topical CsA 0.05% (Restasis) twice a day 1 month pre-HSCT and 24 of whom did not receive CsA (control group) [14]. Dry eye symptoms were found to be significantly more severe in the control group at 3 months, 1 year, and 2 years. Chun et al. performed a comparative study of 58 participants, 28 of whom received topical CsA 0.05% (Restasis) four times a day starting 1 month pre-HSCT and 30 of whom did not receive CsA (control group). At 3 months follow-up, they found that among patients with baseline Schirmer values < 10 mm and tear breakup time (TBUT) < 5 s pre-HSCT, the CsA group had significantly better outcomes than the control group [15]. Cantu-Rodiguez et al. conducted a longitudinal study of 20 participants who were given topical CsA 0.1% (MODUSIK-A OFTENO, Sophia Lab) two drops twice a day for 1 year starting after HSCT was performed [16]. Only one out of the 20 patients developed ocular GVHD over the 20 month follow-up period. In these studies, dry eye outcome measures used were dry eye questionnaires, slit lamp examination, fluorescein staining, tear breakup time, and Schirmer test. Other outcome measures such as meibomian gland analysis, impression cytology, and flow cytometry have not been previously performed in prophylactic studies using topical CsA.
Topical CsA has been reported to be safe and efficacious in the treatment of DED associated with chronic GVHD [11,12,13]. Though the pathogenesis of ocular GVHD is still not fully understood, periductal fibroblasts in ocular GVHD patients have been shown to express certain surface antigens to CD4+ and CD8+ T cells, resulting in a fibrogenic immune process [4, 5]. CsA is an immunosuppressant that blocks T cell proliferation [40, 41]. Systemic CsA has long been used in the prevention of acute and chronic systemic GVHD. It is hence postulated that topical ophthalmic CsA would exert a similar effect in ocular tissues to reduce inflammation. Starting topical CsA treatment 1 month before HSCT would allow greater ocular tissue levels of CsA in the early phase (< 120 days after HSCT) of GVHD, preventing damage to lacrimal acini [12].
In clinical practice, we can consider the prophylactic use of Ikervis for patients undergoing bone marrow allotransplantation. This will likely most benefit the patient population in whom GVHD risk is predicted to be high, or for patients who have significant ophthalmological findings of preexisting increased corneal staining, even if asymptomatic for dry eye. This was found to be acceptable to a high proportion of participants. It is likely that the burning sensation of the formulation may be a cause of non-compliance. In the real world scenario, drugs would have to be paid for by patients and the cost of the prophylaxis drug may also be a deterrent.
The main strength of our study is that we are the first to report T cell population changes after initiation of topical CsA in HSCT patients. We also reported numerous clinical outcomes in a standardized fashion, whereas though the three previous studies in literature have explored the use of topical CsA prophylaxis in GVHD, none included meibomian gland analysis, impression cytology, or flow cytometry. Our study is also the first study using topical CsA 0.1% (Ikervis, Santen) once a day, which could theoretically increase compliance compared with a regime of BD or QDS. Our main limitation is that we did not include additional arms of HSCT patients not on CsA prophylaxis or non-HSCT patients using Ikervis (recruitment rates affected by COVID pandemic restrictions would have resulted in an unacceptably long study), as well as the lack of follow-up beyond 1 year post-HSCT. It remains to be seen if prophylactic CsA can prevent ocular complications in the longer term (which could occur 10 years or later). Also, our sample size was relatively small and a larger sample size would be beneficial. There are limitations to the impression cytology as it may fail to harvest deeper conjunctival immune cells, and we did not have enough channels in the flow to further evaluate the conjunctival CD4 subsets for their activation state. Additionally, in our paper, we assumed that CD8− CD3+ cells were CD4+ cells. However a recent paper has shown that apart from CD4+ and CD8+ cells, the conjunctival epithelium also contains interleukin (IL)17-producing γδ T cells and natural killer (NK) T cells, which may also be involved in modulating DED [42]. We did not account for this group of T cells in our paper. We did not evaluate dendritic cells and other immune cell populations. We did not evaluate T cells outside the bulbar conjunctiva. Apart from bulbar conjunctiva, CD4 T cells may also be activated along the eyelid margin or within the lacrimal glands themselves. Future studies may require multicenter randomized controlled trials (RCTs) to evaluate the efficacy of topical CsA, as larger numbers and a control group would be ideal. However, it may not be ethical to withhold prophylactic treatment from the control group and comparison with other treatment modalities such as lifitigrast may have to be considered instead. As for systemic GVHD prophylaxis, the effect on its prevention of oGVHD cannot be studied by RCTs since there are many potential drug combinations.
Conclusion
The superficial conjunctival T cell profile reflects compliance to daily topical 0.1% cationic CsA eye drops and clinical ocular surface parameters in allo-HSCT patients. Tolerance is comparable to other formulations of topical CsA in the first 12 months.
References
Berchicci L, Rabiolo A, Marchese A, et al. Ocular chronic graft-versus-host disease after allogeneic hematopoietic stem cell transplantation in an Italian referral center. Ocul Surf. 2018;16(3):314–21. https://doi.org/10.1016/j.jtos.2018.04.001.
Na KS, Yoo YS, Mok JW, Lee JW, Joo CK. Incidence and risk factors for ocular GVHD after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2015;50(11):1459–64. https://doi.org/10.1038/bmt.2015.187.
Mian SI, De la Parra-Colín P, De Melo-Franco R, Johnson C, Barrientos-Gutierrez T. Dry eye disease incidence associated with chronic graft-host disease: nonconcurrent cohort study (an american ophthalmological society thesis). Trans Am Ophthalmol Soc. 2015;113:T11.
Ogawa Y, Yamazaki K, Kuwana M, et al. A significant role of stromal fibroblasts in rapidly progressive dry eye in patients with chronic GVHD. Invest Ophthalmol Vis Sci. 2001;42(1):111–9.
Ogawa Y, Kuwana M, Yamazaki K, et al. Periductal area as the primary site for T-cell activation in lacrimal gland chronic graft-versus-host disease. Invest Opthalmol Vis Sci. 2003;44(5):1888. https://doi.org/10.1167/iovs.02-0699.
Shikari H, Antin JH, Dana R. Ocular graft-versus-host disease: a review. Surv Ophthalmol. 2013;58(3):233–51. https://doi.org/10.1016/j.survophthal.2012.08.004.
Townley JR, Dana R, Jacobs DS. Keratoconjunctivitis sicca manifestations in ocular graft versus host disease: pathogenesis, presentation, prevention, and treatment. Semin Ophthalmol. 2011;26(4–5):251–60. https://doi.org/10.3109/08820538.2011.588663.
Munir SZ, Aylward J. A review of ocular graft-versus-host disease. Optom Vis Sci. 2017;94(5):545–55. https://doi.org/10.1097/OPX.0000000000001071.
Hingorani M, Metz D, Lightman SL. Characterisation of the normal conjunctival leukocyte population. Exp Eye Res. 1997;64(6):905–12. https://doi.org/10.1006/exer.1996.0280.
Reinoso R, Martín-Sanz R, Martino M, et al. Topographical distribution and characterization of epithelial cells and intraepithelial lymphocytes in the human ocular mucosa. Mucosal Immunol. 2012;5(4):455–67. https://doi.org/10.1038/mi.2012.27.
Lelli GJ, Musch DC, Gupta A, Farjo QA, Nairus TM, Mian SI. Ophthalmic cyclosporine use in ocular GVHD. Cornea. 2006;25(6):635–8. https://doi.org/10.1097/01.ico.0000208818.47861.1d.
Kiang E, Tesavibul N, Yee R, Kellaway J, Przepiorka D. The use of topical cyclosporin A in ocular graft-versus-host-disease. Bone Marrow Transplant. 1998;22(2):147–51. https://doi.org/10.1038/sj.bmt.1701304.
Wang Y, Ogawa Y, Dogru M, et al. Ocular surface and tear functions after topical cyclosporine treatment in dry eye patients with chronic graft-versus-host disease. Bone Marrow Transplant. 2008;41(3):293–302. https://doi.org/10.1038/sj.bmt.1705900.
Malta JB, Soong HK, Shtein RM, et al. Treatment of ocular graft-versus-host disease with topical cyclosporine 0.05%. Cornea. 2010;29(12):1392–1396. https://doi.org/10.1097/ICO.0b013e3181e456f0
Chun YH, Beak JU, Kim HS, Na KS. Topical cyclosporine pretreatment of ocular surface in allogeneic hematopoietic stem cell transplant recipients. J Ocul Pharmacol Ther Off J Assoc Ocul Pharmacol Ther. 2018;34(9):628–32. https://doi.org/10.1089/jop.2018.0006.
Cantú-Rodríguez OG, Vázquez-Mellado A, González-Treviño JL, et al. Cyclosporine A for the prevention of ocular graft versus host disease in allogeneic hematopoietic stem cell transplant recipients is safe and feasible. Acta Haematol. 2020;143(5):425–31. https://doi.org/10.1159/000502405.
Gehlsen U, Siebelmann S, Steven P. Tolerance and Adherence to Cationic 0.1% Cyclosporine in Ocular Graft-versus-Host Disease. Ophthalmic Res. 2021;64(1):77–84. https://doi.org/10.1159/000509034
Bose T, Lee R, Hou A, Tong L, Chandy KG. Tissue resident memory T cells in the human conjunctiva and immune signatures in human dry eye disease. Sci Rep. 2017;7:45312. https://doi.org/10.1038/srep45312.
Ngo W, Situ P, Keir N, Korb D, Blackie C, Simpson T. Psychometric properties and validation of the standard patient evaluation of eye dryness questionnaire. Cornea. 2013;32(9):1204–10. https://doi.org/10.1097/ICO.0b013e318294b0c0.
Best N, Drury L, Wolffsohn JS. Clinical evaluation of the Oculus Keratograph. Cont Lens Anterior Eye J Br Contact Lens Assoc. 2012;35(4):171–4. https://doi.org/10.1016/j.clae.2012.04.002.
Wu S, Hong J, Tian L, Cui X, Sun X, Xu J. Assessment of bulbar redness with a newly developed keratograph. Optom Vis Sci Off Publ Am Acad Optom. 2015;92(8):892–9. https://doi.org/10.1097/OPX.0000000000000643.
Koh S, Ikeda C, Fujimoto H, et al. Regional differences in tear film stability and meibomian glands in patients with aqueous-deficient dry eye. Eye Contact Lens. 2016;42(4):250–5. https://doi.org/10.1097/ICL.0000000000000191.
Hong J, Sun X, Wei A, et al. Assessment of tear film stability in dry eye with a newly developed keratograph. Cornea. 2013;32(5):716–21. https://doi.org/10.1097/ICO.0b013e3182714425.
Arita R, Itoh K, Inoue K, Amano S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology. 2008;115(5):911–5. https://doi.org/10.1016/j.ophtha.2007.06.031.
Terry RL, Schnider CM, Holden BA, et al. CCLRU standards for success of daily and extended wear contact lenses. Optom Vis Sci Off Publ Am Acad Optom. 1993;70(3):234–43. https://doi.org/10.1097/00006324-199303000-00011.
Versura P, Campos EC. TearLab® osmolarity system for diagnosing dry eye. Expert Rev Mol Diagn. 2013;13(2):119–29. https://doi.org/10.1586/erm.12.142.
Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol. 2011;151(5):792-798.e1. https://doi.org/10.1016/j.ajo.2010.10.032.
Sullivan BD, Whitmer D, Nichols KK, et al. An objective approach to dry eye disease severity. Invest Opthalmol Vis Sci. 2010;51(12):6125. https://doi.org/10.1167/iovs.10-5390.
Massof RW, McDonnell PJ. Latent dry eye disease state variable. Invest Opthalmol Vis Sci. 2012;53(4):1905. https://doi.org/10.1167/iovs.11-7768.
Jung JW, Park SY, Kim JS, Kim EK, Seo KY, Kim T im. Analysis of factors associated with the tear film lipid layer thickness in normal eyes and patients with dry eye syndrome. Investig Opthalmology Vis Sci. 2016;57(10):4076. https://doi.org/10.1167/iovs.16-19251
Tsubota K, Yokoi N, Watanabe H, et al. A new perspective on dry eye classification: proposal by the asia dry eye society. Eye Contact Lens. 2020;46(Suppl 1):S2–13. https://doi.org/10.1097/ICL.0000000000000643.
Tong L, Beuerman R, Simonyi S, Hollander DA, Stern ME. Effects of punctal occlusion on clinical signs and symptoms and on tear cytokine levels in patients with dry eye. Ocul Surf. 2016;14(2):233–41. https://doi.org/10.1016/j.jtos.2015.12.004.
Lamoureux EL, Pallant JF, Pesudovs K, Rees G, Hassell JB, Keeffe JE. The impact of vision impairment questionnaire: an assessment of its domain structure using confirmatory factor analysis and rasch analysis. Invest Ophthalmol Vis Sci. 2007;48(3):1001–6. https://doi.org/10.1167/iovs.06-0361.
Filipovich AH, Weisdorf D, Pavletic S, et al. national institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11(12):945–956. https://doi.org/10.1016/j.bbmt.2005.09.004
Williams GP, Denniston AKO, Oswal KS, et al. The dominant human conjunctival epithelial CD8αβ+ T cell population is maintained with age but the number of CD4+ T cells increases. Age Dordr Neth. 2012;34(6):1517–28. https://doi.org/10.1007/s11357-011-9316-3.
Arnous R, Arshad S, Sandgren K, Cunningham AL, Carnt N, White A. Tissue resident memory T cells inhabit the deep human conjunctiva. Sci Rep. 2022;12(1):6077. https://doi.org/10.1038/s41598-022-09886-3.
Leonardi A, Van Setten G, Amrane M, et al. Efficacy and safety of 0.1% cyclosporine a cationic emulsion in the treatment of severe dry eye disease: a multicenter randomized trial. Eur J Ophthalmol. 2016;26(4):287–296. https://doi.org/10.5301/ejo.5000779
Shikari H, Amparo F, Saboo U, Dana R. Onset of ocular graft-versus-host disease symptoms after allogeneic hematopoietic stem cell transplantation. Cornea. 2015;34(3):243–7. https://doi.org/10.1097/ICO.0000000000000340.
Westeneng AC, Hettinga Y, Lokhorst H, Verdonck L, van Dorp S, Rothova A. Ocular graft-versus-host disease after allogeneic stem cell transplantation. Cornea. 2010;29(7):758–63. https://doi.org/10.1097/ICO.0b013e3181ca321c.
Paavonen T, Hayry P. Effect of cyclosporin A on T-dependent and T-independent immunoglobulin synthesis in vitro. Nature. 1980;287(5782):542–4.
Eckstein LA, Van Quill KR, Bui SK, Uusitalo MS, O’Brien JM. Cyclosporin a inhibits calcineurin/nuclear factor of activated T-cells signaling and induces apoptosis in retinoblastoma cells. Invest Ophthalmol Vis Sci. 2005;46(3):782–90. https://doi.org/10.1167/iovs.04-1022.
Li L, Li Y, Zhu X, et al. Conjunctiva resident γδ T cells expressed high level of IL-17A and promoted the severity of dry eye. Invest Opthalmol Vis Sci. 2022;63(12):13. https://doi.org/10.1167/iovs.63.12.13.
Knop N, Knop E. Conjunctiva-associated lymphoid tissue in the human eye. Invest Ophthalmol Vis Sci. 2000;41(6):1270–9.
Chan JH, Amankwah R, Robins RA, Gray T, Dua HS. Kinetics of immune cell migration at the human ocular surface. Br J Ophthalmol. 2008;92(7):970–5. https://doi.org/10.1136/bjo.2007.131003.
Power WJ, Mullaney P, Farrell M, Collum LM. Effect of Topical Cyclosporin A on Conjunctival T Cells in Patients with Secondary Sj??gren???s Syndrome: Cornea. 1993;12(6):507–511. https://doi.org/10.1097/00003226-199311000-00008
Kunert KS. Analysis of topical cyclosporine treatment of patients with dry eye syndromeeffect on conjunctival lymphocytes. Arch Ophthalmol. 2000;118(11):1489. https://doi.org/10.1001/archopht.118.11.1489.
Hingorani M, Calder VL, Buckley RJ, Lightman S. The immunomodulatory effect of topical cyclosporin A in atopic keratoconjunctivitis. Invest Ophthalmol Vis Sci. 1999;40(2):392–9.
Acknowledgements
The authors thank all the participants of this study.
Funding
This trial was sponsored by Santen Pharmaceutical Asia Pte. Ltd. The sponsors did not have a role in the design or conduct of the study. The journal’s Rapid Service fee was funded by Santen Pharmaceutical Asia Pte. Ltd.
Author Contributions
Louis Tong and Li Lim contributed in the concept and design of this article, acquisition, analysis and interpretation of data, wrote the manuscript and revised it for important intellectual content. Elizabeth Wen Ling Lim, Sharon Wan Jie Yeo and Aihua Hou contributed in the acquisition, analysis and interpretation of data, wrote the manuscript and revised it for important intellectual content. Yeh Ching Linn contributed in the concept and design of this article, the acquisition of data and revision of the manuscript for important intellectual content. Aloysius Ho, Hein Than, Jeffrey Kim Siang Quek, William Ying Khee Hwang and Francesca Lorraine Wei Inng Lim contributed in the acquisition of data and revision of the manuscript for important intellectual content.
Disclosures
Li Lim received funding from Santen Pharmaceutical Asia Pte. Ltd. for this study. She has no other conflicts of interest pertaining to this study. Louis Tong, Elizabeth Wen Ling Lim, Sharon Wan Jie Yeo, Aihua Hou, Yeh Ching Linn, Aloysius Ho, Hein Than, Jeffrey Kim Siang Quek, William Ying Khee Hwang, Francesca Lorraine Wei Inng Lim do not have any conflicts of interest pertaining to this study.
Compliance with Ethics Guidelines
Our study adhered with the tenets of the Declaration of Helsinki on human research and was prospectively reviewed and approved by the SingHealth Centralised Institutional Review Board (reference number: 2019/2635). The study was registered in the Clinical Trials database (NCT04636918).
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available as the informed consent signed by the study subjects did not include public sharing of their data.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
40123_2023_686_MOESM1_ESM.tif
Supplementary Figure 1: Graph of Schirmers values of individual patients pre- and post-HSCT. Three outliers are seen in this graph, 2 of whom had a pre-HSCT Schirmer value of 14mm and post-HSCT Schirmer value of 0mm. These outliers were excluded from paired t test analysis (TIF 1705 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tong, L., Lim, E.W.L., Yeo, S.W.J. et al. Conjunctival T Cell Profile in Allogeneic Hematopoietic Stem Cell Transplant Patients after Instilling Topical Cyclosporine-A 0.1% Cationic Emulsion. Ophthalmol Ther 12, 1547–1567 (2023). https://doi.org/10.1007/s40123-023-00686-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00686-0