Abstract
Introduction
There is a high prevalence of intermittent exotropia and exophoria in myopic populations, and orthokeratology is one of the effective interventions to control myopia progression in children. However, it is still obscure whether intermittent exotropia and exophoria children could wear orthokeratology without experiencing aggravated lens decentration.
Methods
This was a multi-center, prospective cohort study. A total of 123 myopic participants aged 8–14 years were recruited, where conditions of deviation included intermittent exotropia, exophoria, and orthophoria. Uncorrected visual acuity and corneal topography data were obtained at baseline and after 1 month of wearing orthokeratology lens. Lens decentration was analyzed in a MATLAB program. Magnitude of deviation and refractive errors were evaluated prior to orthokeratology treatment. Fisher’s exact test, ANOVA test, and univariate and multivariate linear regression models were established to evaluate the role of magnitude of deviation in lens decentration.
Results
There was no significant difference in magnitude and direction of lens decentration among three groups (magnitude: F = 1.25, P = 0.289; direction: Fisher = 9.91, P = 0.078). According to scale division of decentration, 1 (2.6%) intermittent exotropia subject, 2 (3.8%) exophoria subjects, and 1 (3.0%) orthophoria subject experienced severe decentration (Fisher = 1.10, P = 0.947). Inferotemporal decentration was most common among all subjects (intermittent exotropia 50.0%, exophoria 76.9%, orthophoria 72.7%). Univariate and multivariate linear regression analyses revealed that magnitude of deviation was not an independent risk factor for lens decentration [β = −0.00, 95% confidence interval (CI) −0.01–0.00, P = 0.180], while surface asymmetry index (SAI) (β = 0.21, 95% CI 0.02–0.40, P = 0.028) and surface regularity index (SRI) (β = −0.39, 95% CI −0.66 to −0.13, P = 0.004) had significant correlation with polar decentration.
Conclusion
Patients with intermittent exotropia and exophoria exhibit non-aggravated lens decentration after orthokeratology application. Thus, lens decentration is not the concern for orthokeratology prescription.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There is a high prevalence of intermittent exotropia and exophoria among myopic children. Though orthokeratology has been proved effective in myopia control in recent years, it is still unclear whether children with intermittent exotropia could wear orthokeratology without experiencing increased adverse effects. |
What was learned from the study? |
We compared lens decentration and uncorrected visual acuity after orthokeratology application among intermittent exotropia, exophoria, and orthophoria populations. Subjects with intermittent exotropia and exophoria manifested good response with non-aggravated lens decentration and clear vision. |
We confirmed that lens decentration is not a concern for orthokeratology prescription in subjects with intermittent exotropia. |
Introduction
Exophoria (XPH) is a tendency of oculomotor deviation which can be compensated by fusion to maintain alignment and binocular vision. Intermittent exotropia (IXT) is a transitional strabismus between XPH and constant exotropia, where fusion is only able to control or motor fuse the exodeviation for some time. It is quite common that myopia coexists with XPH or IXT. A population-based study of Australian school children confirmed that 69–75% of children with myopia presented with XPH when near, while the proportion was 9–17% at distance [1]. A retrospective study estimated that myopia occurs in more than 90% of IXT by 20 years of age, which is much higher than that in non-strabismus populations [2]. The increase of accommodation and accommodative convergence to compensate for the insufficiency of fusional convergence in IXT was recognized as one of the most important explanations for the correlation [3, 4]. Therefore, IXT was identified as an influencing factor for myopia. On the other hand, myopia was regarded as an independent indicator for concomitant exotropia. It has been reported that children with myopia had 2.85- to 10.27-fold increase in risk to develop exotropia than those without significant ametropia [5,6,7]. In recent years, studies regarding natural history of IXT reminded ophthalmologists that surgery is not the only therapeutic option for patients with IXT. Regular follow-up and observation could be preferable treatment modalities under some conditions [8]. Due to the common coexistence and possible mutual promotion between myopia and IXT, it is necessary to pay attention to myopia control in patients with IXT and XPH under observation.
Orthokeratology (Ortho-K), a kind of optical correction method, is one of the most effective interventions to slow down the progression of myopia in children [9]. It is characterized by specially designed reverse geometry and gas-permeable overnight contact lens, temporarily reshaping the cornea by flattening the central zone and steepening the peripheral zone [10]. Peripheral hyperopic defocus and higher-order aberrations were proved to produce marked effect [11, 12]. Lens decentration (LD) refers to the deviation from pupil center to the treatment zone (TZ) center after Ortho-K application. Severe LD could give rise to a variety of vision disturbances (including glare, ghost images, double vision, or reduction in contrast sensitivity), by inducing unexpected astigmatism and higher-order aberrations [13, 14]. In vision shaping treatment (VST) of Ortho-K, alignment curve (AC) is designed to maintain and guarantee the correction of lens fixing and position [15]. However, due to inevitable asymmetry of corneal surface and eyelid pressure, LD remains the most common fitting challenge of Ortho-K.
Fusional vergence, or motor fusion, is an optomotor reflex that aligns images of the two eyes globally. It Is generally accepted that fusion would be less exerted during sleep, thus exodeviation would manifest in patients with XPH and IXT [16, 17]. Due to the possible divergent eye position in IXT during sleep, it is speculated that asymmetry of eyelid pressure may arise and produce adverse effect on the stability of lens location. In the opinion of many ophthalmologists and optometrists, patients with IXT are more likely to experience severe LD after Ortho-K treatment and become less appropriate for wearing Ortho-K. However, excluding the important procedure of Ortho-K, on the basis of empirical speculation for IXT complicated by patients with myopia, lacks evidence, and whether Ortho-k may produce enough followability during sleep for these patients triggers curiosity. This study was designed to determine whether patients with XPH or IXT would experience aggravated LD after Ortho-K application compared with orthophoria in the Nanjing Strabismus Cohort.
Methods
The Nanjing Strabismus Cohort aims to systematically integrate clinical and population resources to achieve strabismus risk assessment and prediction, individualized prevention, precise diagnosis and treatment, and efficacy monitoring in Nanjing, Jiangsu, China. The present study was conducted in the First Affiliated Hospital with Nanjing Medical University and Nanjing Orange Optometry Clinic. The study was approved by the institutional review board in the First Affiliated Hospital with Nanjing Medical University (2019-SR-134) and was conducted in accordance with the tenets of the Declaration of Helsinki. Written consent was obtained from the guardians of all children.
Subjects
Inclusion criteria: (1) age between 8 and 14 years old, (2) myopia between −0.75 and −6.00 D, (3) astigmatism less than or equal to 1.50 D, (4) equal visual acuity (best corrected visual acuity, BCVA) of 0.20 logMAR or better in each eye, and (5) choosing α ORTHO-K.
Exclusion criteria: (1) constant exotropia, (2) prior history of wearing contact lenses, (3) ocular injury or prior surgery, (4) Ortho-K contraindications, and (5) simultaneous application of other measures for myopia control.
Subjects included three groups as follows: (1) IXT group: intermittent or constant exotropia at distance, and XPH or IXT when near, magnitude of deviation ≥ 15 prism diopters (PD) at distance or near measurements by the prism and alternate cover test (PACT), and near/distance deviation difference of ≤ 10PD. (2) Orthophoria group: absolute magnitude of deviation ≤ 2PD both at distance and when near. (3) XPH group: manifest between orthophoria and IXT.
All enrolled participants were fitted with α ORTHO-K (Alpha Corporation, Japan) made of Boston material according to the manufacturer’s guidelines. The optical center thickness was 0.22 mm. The width of base curve (BC) was determined by spherical errors, Jessen factor of 0.75, and flattest corneal curvature. The total diameter was determined by subtraction of 0.1 mm from the horizontal visible iris diameter (HVID), with modifications made to the width of AC. A typical bull’s eye pattern observed by corneal topography on the second day confirmed a satisfactory fit. Subjects enrolled were instructed about the wearing, removing, and caring procedures and wore their Ortho-K lenses on both eyes every night for at least 7 consecutive hours. All follow-up examinations were performed within 2 h after removal of the Ortho-K lens.
Parameters Measured
Baseline tests included measurements of uncorrected visual acuity (UCVA), BCVA, magnitude of deviation at distance and when near, refraction, axial length, and corneal topographic parameters. Magnitude of deviation was estimated at 33 cm and 6 m using PACT after performing a 1-h occlusion on the non-dominant eye. Magnitude of deviation at distance was included in the analysis. A previous study has shown that the corneal topography usually stabilizes after 1 month of Ortho-K wearing [18]. Therefore, all the measurements were repeated after 1 month of wearing. All the evaluations were conducted by one professional examiner.
The Medmont E300 corneal topographer (Medmont Studio 4 software version 4.14; Medmont International Pty Ltd, Victoria, Australia) was used to measure corneal topography. Maps with an accuracy of ≥ 95% were brought into analyses. Flat k (k1), Steep k (k2), flat eccentricity (e1), steep eccentricity (e2), surface asymmetry index (SAI), surface regularity index (SRI), and pupil diameter (PD) were recorded, while e ratio (e1/e2) and corneal toricity (k2 − k1) were calculated.
After Ortho-K treatment, a difference map was obtained by subtracting the pre-Ortho-K tangential curvature map from the 1-month post-Ortho-K tangential curvature map. LD was computed in a MATLAB program (Fig. 1). Modified from previous studies [19,20,21,22], we used regiongrowing and imfill function to obtain the outline of TZ. Then, coordinates of the outline were extracted and accessed into circle fit function to calculate the best-fitting circle. The center of the circle was defined as the center of TZ, and its distance from the pupil center by automatic recognition was defined as the magnitude of LD. As LD was moderately correlated between right and left eyes (r = 0.553, P < 0.001), analyses were conducted on right eyes only.
Methods to estimate treatment zone decentration. a Axial map at baseline; b tangential curvature map after 1-month Ortho-K wearing; c tangential curvature difference map between baseline and 1-month visit, with automatically identified pupil; d tangential curvature difference map after step width adjustment, with automatically identified pupil center; e acquired treatment zone using regiongrowing and imfill function; f the best-fitting circle calculated by circle fit function
Statistical Analysis
Data analyses were performed using the IBM Statistical Package for the Social Sciences program statistical package V21.0 (SPSS Inc, Chicago, IL, USA). All statistical tests were two-sided, and P < 0.05 was considered statistically significant. The Kolmogorov–Smirnov test was used to assess the normality of the data distribution. Descriptive statistics were presented as mean ± standard deviation or median (interquartile range, IQR) based on normality test, and as percentage for the categorical measures. Pearson correlation coefficient was used to determine the correlation of LD between two eyes. LD among groups was compared using one-way ANOVA or Kruskal–Wallis H test based on Kolmogorov–Smirnov test for continuous variables, and χ2 test or Fisher's exact test (if the expected count in any cell of the contingency table was < 5) for categorical variables. Univariate and multivariate linear regression models were used to explore the influencing factors of LD.
Results
A total of 123 subjects were included in the analyses, comprised by 38 IXT, 52 XPH, and 33 orthophoria. Table 1 shows the baseline characteristics of IXT, XPH, and orthophoria groups before treatment. Subjects among groups did not show significant difference at baseline (P > 0.05). None of the Ortho-K wearers complained of discomfort, low vision, or obvious adverse events (e.g., severe corneal staining graded on the Oxford scheme [23], corneal abrasion, conjunctivitis, contact lens-induced peripheral ulcer). After 1 month of Ortho-K wearing, the median (IQR) of UCVA was 0.08 (0.00, 0.08) in orthophoria group, 0.04 (0.00, 0.08) in XPH group, and 0.08 (0.00, 0.08) in IXT group. There was no statistically significant difference in UCVA among three groups (H = 0.35, P = 0.841).
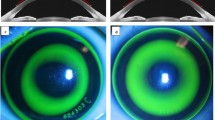
The magnitude and direction of LD after 1 month Ortho-K treatment were presented in Table 2 and Fig. 2. For magnitude of LD, a negative value means temporal and inferior shift, while a positive value stands for nasal and superior shift. No significant difference was found in magnitude of polar, horizontal, or vertical decentration among 3 groups (polar decentration: F = 1.25, P = 0.289; horizontal decentration: F = 1.46, P = 0.236; vertical decentration: F = 0.57, P = 0.567). Besides, 1 (2.6%) in IXT group, 2 (3.8%) in XPH group, and 1 (3.0%) in orthophoria group experienced severe decentration (polar decentration > 1 mm; Fisher = 1.10, P = 0.947). There was no significant difference in the direction of LD (Fisher = 9.91, P = 0.078), with 19 (50.0%) of IXT, 40 (76.9%) of XPH, and 24 (72.7%) of orthophoria experiencing inferotemporal decentration.
Scatterplot showing the distribution of the treatment center of Ortho-K relative to the pupil center. Marginal plot (box plot) displays the distribution of horizonal and vertical decentration in three groups. The algorithm of ellipse fitting shows the 90% confidence interval of lens decentration distribution
Univariate linear regression analysis revealed that SRI was significantly negatively associated with polar LD. Though SAI was not significantly associated with LD in the univariate analysis, we put it into multivariate analysis, as positive association was found in a previous study. Whether deviation affects LD was our concern. Thus, apart from SRI and SAI, we included magnitude of deviation into multivariate linear regression model. However, magnitude of deviation was not significantly associated with LD (β = −0.00, 95% CI −0.01 to 0.00, P = 0.180). SAI (β = 0.21, 95% CI 0.02–0.40, P = 0.028) and SRI (β = −0.39, 95% CI −0.66 to −0.13, P = 0.004) were still significantly associated with LD (Table 3).
Discussion
In this study, we compared LD and UCVA after Ortho-K application among IXT, XPH, and orthophoria populations and found no significant difference.
With the deepening of insight into the natural course of IXT [8, 24], regular follow-up visits and observation have been the first choice for many patients with IXT. As we have known, there is a high prevalence of IXT and XPH among myopic children [1, 6]. For these children, the need of myopia control should not be ignored, and should even be addressed due to the possibility of mutual promotion between IXT and myopia. However, controversy still remains whether IXT children could choose myopia control procedures without experiencing increased adverse effects.
Ortho-K is a kind of eye contact lenses that is worn overnight, to correct myopia and to slow myopia progression. Due to asymmetry of eyelid pressure and corneal topographical parameters [20] (paracentral corneal asymmetry, corneal elevation, the diameter of the cornea [25], and Q value [26]), LD is common and ineluctable in Ortho-K application. Consistent with a previous study [21], the most common direction of LD was found to be inferonasal. This might result from the steeper corneal shape in temporal and inferior areas, and the tendency of lenses drifting to the steeper side [25]. Similarly, according to linear regression models, we found SAI as an independent risk factor for LD and SRI as a protective factor. SAI stands for the asymmetry of the corneal surface, which is a centrally weighted summation of differences in corneal power between corresponding points in opposite directions on 128 equally separated meridians. On the contrary, SRI represents the regularity of corneal surface, obtained by a summation of local corneal power along 256 equally separated meridians [27].
In the opinion of many doctors and optometrists, Ortho-K has been recommended less for patients with IXT due to the concern for the possibility of aggravated LD. In our study, among IXT, XPH, and orthophoria groups, we did not find any statistical difference either in magnitude or direction of LD. The reasons might include the following. Firstly, favorable fitting of Ortho-K lenses depends on proper matching of the lens sag height with the corneal sag height along the flatter corneal meridian, to create a water-tight space filled with tear [20]. According to hydrodynamics ductility principle, when wearing an eye contact lens, once “seesaw” (two sides of the lens become tilted) occurs in any corneal meridian, lens will decenter to get access to another water-tight location. Even during rapid eye movement (REM), where bursts of eye movements are present and characterized as ocular rotation at a speed greater than 30° per second, well-matched Ortho-K lens could fit well on the central part of cornea [28]. Secondly, sleep–wake cycles include four periods: awake, non-rapid eye movement (NREM) sleep, period of transition to REM sleep, and REM sleep [29], with NREM occupying most of the sleep time [30]. During non-REM sleep, the two eyes slowly rotate upwards and in the abducting direction, producing a tonic divergent position [31]. Thus, it is rational to speculate that the three groups shared similar divergent eye position during NREM sleep [32], which makes for comparable magnitude and direction of LD after overnight wearing of Ortho-K lenses.
Average magnitude of decentration in orthophoria group in this study was 0.51 mm and in accordance with previous reports [19, 20]. It is generally regarded that, decentration less than 0.5 mm (mild decentration) is optimal while 0.5–1.0 mm (moderate decentration) is acceptable, and greater than 1.0 mm (severe decentration) should be avoided [33]. Only 1 in 38 of the IXT group experienced severe decentration, with a vertical decentration of −1.17 mm, which was comparable to other groups, produced by distinct eyelid pressure and inappropriate fit tightness. Also, none of the IXT or XPH subjects experienced low vision or under-correction. Therefore, LD should not be a main concern when prescribing overnight Ortho-K for patients with XPH or IXT.
To our knowledge, this is the first study to evaluate the application of Ortho-K in patients with IXT. However, one limitation is that patients with IXT included in this study manifested a deviation that ranged from 0 to 37 PD, and the application of Ortho-K in IXT with larger angles of deviation needs further study. Secondly, we only confirmed the non-aggravated LD of Ortho-K in IXT and XPH subjects. It is promising to evaluate the effect of Ortho-K in myopia control, binocular function, and exodeviation control for patients with IXT in the future.
Conclusion
In conclusion, we did not find aggravated LD after Ortho-K treatment in patients with IXT or XPH. LD is not a concern for Ortho-K prescription.
References
Leone JF, Cornell E, Morgan IG, et al. Prevalence of heterophoria and associations with refractive error, heterotropia and ethnicity in Australian school children. Br J Ophthalmol. 2010;94(5):542–6.
Ekdawi NS, Nusz KJ, Diehl NN, et al. The development of myopia among children with intermittent exotropia. Am J Ophthalmol. 2010;149(3):503–7.
Ahn SJ, Yang HK, Hwang JM. Binocular visual acuity in intermittent exotropia: role of accommodative convergence. Am J Ophthalmol. 2012;154(6):981-986 e3.
Ha S-G, Jang S-M, Cho YA, et al. Clinical exhibition of increased accommodative loads for binocular fusion in patients with basic intermittent exotropia. BMC Ophthalmol. 2016;16(1):77.
Robaei D, Kifley A, Mitchell P. Factors associated with a previous diagnosis of strabismus in a population-based sample of 12-year-old Australian children. Am J Ophthalmol. 2006;142(6):1085–8.
Zhu H, Yu JJ, Yu RB, et al. Association between childhood strabismus and refractive error in Chinese preschool children. PLoS ONE. 2015;10(3): e0120720.
Cotter SA, Varma R, Tarczy-Hornoch K, et al. Risk factors associated with childhood strabismus: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 2011;118(11):2251–61.
Pediatric Eye Disease Investigator G, Writing C, Mohney BG, et al. Three-year observation of children 3 to 10 years of age with untreated intermittent exotropia. Ophthalmology. 2019;126(9):1249–60.
Huang J, Wen D, Wang Q, et al. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology. 2016;123(4):697–708.
Jonas JB, Ang M, Cho P, et al. IMI prevention of myopia and its progression. Invest Ophthalmol Vis Sci. 2021;62(5):6.
Hiraoka T, Kakita T, Okamoto F, et al. Influence of ocular wavefront aberrations on axial length elongation in myopic children treated with overnight orthokeratology. Ophthalmology. 2015;122(1):93–100.
VanderVeen DK, Kraker RT, Pineles SL, et al. Use of orthokeratology for the prevention of myopic progression in children: a report by the American Academy of Ophthalmology. Ophthalmology. 2019;126(4):623–36.
Hiraoka T, Furuya A, Matsumoto Y, et al. Quantitative evaluation of regular and irregular corneal astigmatism in patients having overnight orthokeratology. J Cataract Refract Surg. 2004;30(7):1425–9.
Hiraoka T, Okamoto C, Ishii Y, et al. Contrast sensitivity function and ocular higher-order aberrations following overnight orthokeratology. Invest Ophthalmol Vis Sci. 2007;48(2):550–6.
Nti AN, Berntsen DA. Optical changes and visual performance with orthokeratology. Clin Exp Optom. 2020;103(1):44–54.
He G. A contribution to the pathogeny of concomitant squinting. Trans Ophthalmol Soc UK. 1890;10:1.
Morris AP, Kubischik M, Hoffmann KP, et al. Dynamics of eye-position signals in the dorsal visual system. Curr Biol. 2012;22(3):173–9.
Alharbi A, Swarbrick HA. The effects of overnight orthokeratology lens wear on corneal thickness. Invest Ophthalmol Vis Sci. 2003;44(6):2518–23.
Chen Z, Xue F, Zhou J, et al. Prediction of orthokeratology lens decentration with corneal elevation. Optom Vis Sci. 2017;94(9):903–7.
Maseedupally VK, Gifford P, Lum E, et al. Treatment zone decentration during orthokeratology on eyes with corneal toricity. Optom Vis Sci. 2016;93(9):1101–11.
Gu T, Gong B, Lu D, et al. Influence of corneal topographic parameters in the decentration of orthokeratology. Eye Contact Lens. 2019;45(6):372–6.
Chen R, Chen Y, Lipson M, et al. The effect of treatment zone decentration on myopic progression during Or-thokeratology. Curr Eye Res. 2020;45(5):645–51.
Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22(7):640–50.
Cotter SA, Mohney BG, Chandler DL, et al. Three-year observation of children 12 to 35 months old with untreated intermittent exotropia. Ophthalmic Physiol Opt. 2020;40(2):202–15.
Li Z, Cui D, Long W, et al. Predictive role of paracentral corneal toricity using elevation data for treatment zone decentration during orthokeratology. Curr Eye Res. 2018;43(9):1083–9.
Li J, Yang C, Xie W, et al. Predictive role of corneal Q-value differences between nasal-temporal and superior-inferior quadrants in orthokeratology lens decentration. Medicine (Baltimore). 2017;96(2): e5837.
Wilson SE, Klyce SD. Advances in the analysis of corneal topography. Surv Ophthalmol. 1991;35(4):269–77.
Takahashi K, Atsumi Y. Precise measurement of individual rapid eye movements in REM sleep of humans. Sleep. 1997;20(9):743–52.
Blumberg MS, Lesku JA, Libourel PA, et al. What is REM sleep? Curr Biol. 2020;30(1):R38–49.
Le Bon O. Relationships between REM and NREM in the NREM-REM sleep cycle: a review on competing concepts. Sleep Med. 2020;70:6–16.
Marquez-Ruiz J, Escudero M. Tonic and phasic phenomena underlying eye movements during sleep in the cat. J Physiol. 2008;586(14):3461–77.
Ku HC, Lee SY, Lee YC. Change of eye position in patients with orthophoria and horizontal strabismus under general anesthesia. Korean J Ophthalmol. 2005;19(1):55–61.
Tsai Y-Y, Lin J-M. Ablation centration after active eye-tracker-assisted photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2000;26(1):28–34.
Acknowledgements
We thank the children, their parents or legal guardians, all the members of Department of Ophthalmology, The First Affiliated Hospital with Nanjing Medical University, Nanjing, China, and Nanjing Orange Optometry Clinic, Nanjing, China for their helpful advice and support.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No.82273159); Jiangsu Province's Science and Technology Project (Grant No. BE2020722). The study sponsors are also funding the journal’s Rapid Service Fee, but had no role in the design or conduct of this research.
Author Contributions
Zijin Wang and Hu Liu designed the study and revised this article. Tianxi Li contributed to writing and revision of this article. Tianxi Li and Xiaoxia Zuo performed data interpretation and analysis. Tong Zhang, Lei Liu, Zhongzheng Wang and Lin Han performed the ocular examinations.
Disclosures
Tianxi Li, Xiaoxia Zuo, Tong Zhang, Lei Liu, Zhongzheng Wang, Lin Han, Hu Liu and Zijin Wang have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the institutional review board in the First Affiliated Hospital with Nanjing Medical University (2019-SR-134) and was conducted in accordance with the tenets of the Declaration of Helsinki. Written consent was obtained from the guardians of all children.
Data Availability
The data used in this study are not publicly available because they contain information that could compromise research participants’ privacy, but may be available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Li, T., Zuo, X., Zhang, T. et al. Patients with Intermittent Exotropia and Exophoria Exhibit Non-aggravated Lens Decentration After Orthokeratology Application: The Nanjing Strabismus Cohort. Ophthalmol Ther 12, 1535–1545 (2023). https://doi.org/10.1007/s40123-023-00685-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00685-1