Abstract
Introduction
The purpose of this article was to ascertain the existing literature and find the gaps in economic evaluations of cataracts.
Methods
Systematic methods were used to search and collect the published literature on economic evaluations of cataracts. A mapping review of studies published in the following bibliographical databases was performed: the National Library of Medicine (PubMed), EMBASE, Web of Science (WOS), and the Central of Reviews and Dissemination (CRD) database. A descriptive analysis was conducted and relevant studies were classified into different groups.
Results
Among 984 studies screened, 56 studies were included in the mapping review. Four research questions were answered. There has been a progressive increase of publications during the last decade. The majority of the included studies were published by authors from institutions in the USA and UK. The most commonly investigated area was cataract surgery followed by intraocular lenses (IOLs). The studies were classified into different categories according to the main outcome evaluated, such as comparisons between different surgical techniques, costs of the cataract surgery, second eye cataract surgery costs, quality of life gain after cataract surgery, waiting time of cataract surgery and costs, and cataract evaluation, follow-up, and costs. In the IOL classification, the most frequently studied area was the comparison between monofocal and multifocal IOLs, followed by the comparison between toric and monofocal IOLs.
Conclusions
Cataract surgery is a cost-effective procedure compared with other non-ophthalmic and ophthalmic interventions and surgery waiting time is an important factor to consider because vision loss has a huge and broad-ranging impact on society. Numerous gaps and inconsistencies are found among the studies included. For this reason, there is a need for further studies according to the classification described in the mapping review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Costs of healthcare are increasing, and therefore the importance of quality and efficiency is higher. Economic evaluations are used as a source of information by economists and healthcare providers to make the best decisions. |
In the ophthalmology field, the economic evaluation of healthcare has become an important area to explore. Several studies have analyzed the economic impact of vision impairment due to cataracts; however, there are still different areas to investigate and gaps to find in the published literature. |
A systematic mapping review was conducted to identify gaps in the literature and to analyze and categorize the existing evidence of economic evaluations in the ophthalmic area of cataracts that can be helpful for guiding future research. |
The results provide evidence that cataract surgery is a cost-effective procedure compared with other non-ophthalmic and ophthalmic interventions and surgery waiting time is an important factor to consider because vision loss has a huge and broad-ranging impact on society. |
Introduction
Cataract is the leading cause of blindness and the second most common cause of vision impairment in adults [1]. In 2020, approximately 596 million people had distance vision impairment worldwide, of whom 43 million were blind and 83.48 million had moderate or severe vision impairment (MSVI) [1, 2]. Vision impairment and eye health can impact general health and well-being, thereby reducing quality of life [3]. In spite of the high rate of MSVI, more than 90% have a preventable treatable cause, such as cataracts, with existing highly cost-effective interventions [1].
Currently, the costs of healthcare are increasing, and therefore the importance of quality and efficiency is higher. In the ophthalmology field, the economic evaluation of healthcare has become an important area to explore, which is getting more common as healthcare is becoming more expensive [4]. Nevertheless, in these times, how much is one willing to invest in terms of vision health in society? Several studies have analyzed the economic impact of vision impairment due to cataracts and have summarized what is actually known [1, 4,5,6,7], even though there are still different areas to investigate and gaps to find in the published literature.
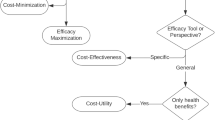
There are different types of economic evaluation in healthcare: cost–consequence analysis (CCA), cost-minimization analysis (CMA), cost-effectiveness analysis (CEA), cost–utility analysis (CUA), and cost–benefit analysis (CBA) [8]. Studies of CEA measure the effects of health outcomes in physical units, such as visual acuity (VA), and patient-reported outcomes (PRO); however, one cannot compare costs and different health interventions which are not in the same units [9]. Comparisons of costs and different health interventions are possible owing to CUA [10]. In contrast to cost-effectiveness studies, which use measurable outcomes, CUA use the dimensionless utility as the outcome parameter. The utility value has been quantified by decision theory methods and psychometric survey methods [7]. One of the most commonly used decision theory methods is the time trade-off (TTO), by which participants have to specify the survival probability they will tolerate to eliminate the medical condition [11]. The higher the number of life years treated (TTO) or the greater the willingness to take risk, the lower the health-related quality of life (HRQoL) associated with the medical condition. HRQoL has been considered a utility variable, with many ways existing to measure it, the most widely used among others being the 5-dimension EuroQol (EQ5D), Health Utilities Index Mark (HUI3), and the 36-item Short Form Survey (SF-36) [12].
The CUA is a type of CEA in which health effects are measured in terms of quality-adjusted life years (QALYs) [13] or disability-adjusted life years (DALYs) in an attempt to capture the two most important features of a health intervention: the effect on survival measured in terms of life years and the effect on quality of life [8]. Several alternatives have been proposed as a unit measure of the CUA; however, the most accepted and used is the QALY [14]. QALYs are calculated by weighting each time interval in a given state by its “utility” on a scale ranging from 0 (death) to 1 (perfect health or normal vision) [13, 15, 16]. The utility value of a patient is a reflection of their preferences, and describes how a patient is able to shape their daily living tasks and allows an objective measurement of quality of life associated with a health state [17]. The higher the utility value, the better quality of life associated with a health state; the lower the value, the poorer the quality of life [18]. Therefore, an improvement in utility value can be used as an objective measurement of efficacy of any medical process to improve a patient’s quality of life [17].
Considering the exponential increase of systematic reviews and meta-analyses in the last decade, there is a need to evaluate the existing evidence using systematic methods. Evidence mapping is one of these emerging methodologies to analyze, categorize, and identify gaps in the literature [19, 20]. For this reason the aim of this study was to map the existing evidence of economic evaluations in the ophthalmic area of cataracts that can be helpful for guiding future research. The article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Material and Methods
A systematic mapping review was conducted, which is one of the 14 types of reviews in the family of systematic reviews [21]. This type of review has been developed to describe the state of knowledge for a given question within a particular topic and it describes results narratively to answer the question. The term “scoping review” is often used interchangeably with the term “mapping review” owing to their methodological similarities. However, they can be distinguished from scoping reviews, because the subsequent outcome may involve further review of primary research, which is not known previously [21].
Sources of Information and Search Strategy
A comprehensive literature search was performed in June 2021 using the following bibliographical databases: the National Library of Medicine (PubMed), EMBASE, and Web of Science (WOS). Moreover, an additional search of publications was performed in a specialized database, the Centre for Reviews and Dissemination CRD’s NHS Economic Evaluations Database (NHS EED) [22, 23], which contains summaries of economic evaluations. The keywords used in the strategy search were cost-effectiveness analysis, cost–utility analysis, and cataracts. The search strategy included the “cost-effectiveness analysis” because some authors refer to healthcare economic analyses measured as cost/quality-adjusted life years (QALY) cost-effectiveness analyses, whereas those in countries other than the USA refer to them as cost–utility analyses [24]. The final search for each database is shown in Table 1. Additionally, the search with the descriptors used is summarized in the Supplementary Material. The final literature search was concluded on June 17, 2022.
Inclusion Criteria of Studies
The study included full economic evaluations that had to be original articles conducting a CUA or CEA in the field of cataracts. The population of interest for this mapping review was all individuals with cataracts regardless of their age, sex, race, and socioeconomic status. However, studies with a population having disease additional to cataracts were excluded. No restrictions were applied with regard to study design, although systematic reviews, whose main objective is to summarize results of cost-effectiveness or cost–utility analyses, were excluded. Only systematic reviews of randomized control studies (RCT) and observational studies which conduct an economic evaluation of the summarized data were included. Additionally, studies about expert guidelines or opinions, and non-original articles were excluded.
Extraction and Analysis of Data
Two reviewers (JG and NB) independently screened titles and abstracts and then obtained full-text articles that could be considered as potentially relevant. Inclusion assessment was done by one reviewer (JG) and checked by the second reviewer (NB). Disagreements between reviewers were resolved by deliberation and consensus, which included an impartial third reviewer if needed.
A single reviewer was sufficient for the data extraction and the verification of data extraction of a random sample. However, a second reviewer performed all verification of data extraction of a random sample to minimize bias [25].
The definition of research questions (RQs) is a key methodological aspect for a successful systematic mapping review [26, 27]. For this systematic mapping review, four RQs were defined:
- RQ1:
-
How many papers have been published on economic evaluations of cataracts? Is there any temporal trend? What is the geographical distribution of the review authors?
- RQ2:
-
What were the most commonly investigated economic evaluation techniques?
- RQ3:
-
Which areas are the focus of research in the economic evaluation of cataracts?
- RQ4:
-
Which were the variables most commonly included in the economic evaluation?
Results
Literature Search Results
The literature search identified 1632 citations, from which 648 were excluded as duplicates and 984 records were screened. Of these, 242 reports were selected for full-text review and assessed for eligibility. Finally, 56 studies were included in the mapping review (Fig. 1, PRISMA flow diagram) [28] (Supplementary Table 5). The four previously detailed research questions are described in the following section based on the selected literature.
RQ1. How many papers have been published on economic evaluations of cataracts? Is there any temporal trend? What is the geographical distribution of the review authors?
As shown in Fig. 2, the earliest study included was published in 1988. No more economic evaluations of cataracts were included until 1996. However, there was not a progressive increase of published studies until 2002, growing from 4 studies published to 56 in 2022. The last 4 years have seen the greatest increase of studies published.
Economic studies were published by authors from many countries over the world; however, the majority were carried out by researchers from institutions in the USA (n = 7), followed by the UK (n = 5).
RQ2. What were the most commonly investigated economic evaluation techniques?
As shown in Supplementary Table 5, from 56 studies, 45 were described as a CEA, which compares the cost effects of cataract interventions and assesses the impact on specific clinical interventions, such as VA or PRO. An extension of the CEA is the CUA, by which the cost effects of cataract interventions are evaluated in terms of quantity (life years) and quality of life (QALYs).
RQ3. Which areas are the focus of research in the economic evaluation of cataracts?
As a result of classifying publications according to the principal areas of research, the majority of the studies were classified as cataract surgery economic evaluations (n = 43) (Tables 2, 3, 4, 5, 6, and 7) followed by intraocular lenses (IOL) (n = 13) (Table 8). Among the economic evaluations applied to cataract surgery or IOLs, the studies were classified into categories according to the main outcome evaluated, such as surgical techniques (Table 2), cataract surgery costs (Table 3), second eye cataract surgery costs (Table 4), quality of life gain after cataract surgery (Table 5), waiting time of cataract surgery and costs (Table 6), and cataract evaluation, follow-up, and costs (Table 7). In the IOL classification, the most frequently studied area was the comparison between monofocal and multifocal IOLs, followed by the comparison between toric and monofocal IOLs (Table 8).
RQ4. Which were the variables most commonly included in the economic evaluation?
The most commonly included variables were QALY, DALY, and the incremental cost-effectiveness ratio (ICER). DALY has two components also included in some studies: years of life lost (YLL) and years lived with disability (YLD) [29,30,31]. The willingness to pay (WTP) is generally used in CBA; however. it has been included in some studies as a method of valuing health outcomes in monetary units [32]. In terms of HRQoL, as it has been already reported in the literature, the most widely used were EQ-5D and HUI3 [12]. In CUA, health effects are measured by QALYs [13] or DALYs [33]. Additionally, the ICER has been used to summarize the results of the economic evaluations of the health interventions [34].
Discussion
This is the first systematic mapping review carried out on the economic evaluation on cataracts, considering studies of CEA and CUA. The current mapping review includes relevant studies over a period of more than 30 years (1988–2022), providing a global overview of the current state of knowledge in the field of cataracts, health, and costs.
A total of 56 articles were selected from the initial 984 non-duplicated studies from four bibliographical databases (PubMed, WOS, CRD, Embase). As shown in Fig. 2, the number of papers published has increased in the last decade, most notably in the last 4 years. Therefore, a great increase in interest in research on economic evaluations of cataracts has occurred recently.
Comparison between surgical techniques in cataract surgery was one of the most commonly investigated areas. Conventional extracapsular surgery (ECCE), manual small incision cataract surgery (MSICS), and femtosecond laser-assisted cataract surgery (LCS) were compared versus phacoemulsification (PCS). Asimakis et al. [35] in 1996 evaluated the cost-effectiveness of cataract surgery comparing ECCE and PCS, and their results showed that ECCE generates slightly lower costs than PCS. Rizal et al. [36] showed similar results, with ECCE being more cost-effective compared to PCS [37].
With the introduction of new techniques such as MSICS, Jongsareejit et al. [38] reported the similar effectiveness of MSICS and PCS, but PCS had higher costs. Therefore, MSICS had better cost-effectiveness than PCS. Khan et al. [40] also compared the cost-effectiveness of PCS versus MSICS, concluding that MSICS provided comparable visual and QALY improvement, taking less time, and consequently being more cost-effective than PCS. Opposite results were published by Wulandari et al. [42] and Rochman et al. [30], concluding that PCS was more cost-effective than MSICS.
Other authors compared the cost-effectiveness of LCS with conventional PCS. Abell et al. [39] showed that PCS was more cost-effective in spite of potential improvements in VA outcomes and complication rates. Schweitzer et al. [41] reported that despite its advanced technology, LCS was not cost-effective compared with PCS. LCS had higher costs and did not provide an additional benefit over PCS for patients or health systems.
Removal of cataracts may be among the most cost-effective of all ophthalmological interventions, as the surgical procedure can be carried out in less than 5 min, being almost always successful, and providing increase in utility after surgery. Therefore, in low-income countries, cataract surgery programs should be given high priority consideration in the planning health services [44]. Although there are no standardized definitions for what is considered cost-effective, it has been suggested that interventions costing less than $20,000/QALY gain are highly cost-effective, whereas those costing more than $100,000/QALY are not cost-effective [45, 87].
Throughout the course of cataract surgery, different countries have evaluated its cost-effectiveness compared with other surgical interventions. It has been proved that cataract surgery is more cost-effective than other ophthalmic and non-ophthalmic health interventions comparing cost/QALY gain of each intervention [44,45,46], being considerably cheaper in Europe and Canada compared with the USA [48].
Nevertheless, Räsänen et al. [47] obtained low results of the mean utility gain after cataract surgery. The majority of patients included in their study only reported minimal seeing problems in the surgical eye, which might have reduced the benefit of cataract surgery, and consequently would explain the small increase in HRQoL after the intervention. The cost–utility of cataract surgery varies substantially depending how the benefit is assessed and the duration of the assumed benefit. Results of CUA in the USA demonstrated that cataract surgery greatly improved quality of life and was highly cost-effective, decreasing its cost over the time, being 34.4% less expensive in 2012 than in 2000, and 85% less expensive than in 1985 [50].
Cataract surgery resulted in a cost-effectiveness intervention of restoring sight in different parts of the world, e.g., Zambia [46], Vietnam [53], New Zealand [66], or Japan [63]. According to accepted international benchmarks, cataract surgery and presbyopia correction can be considered highly cost-effective in Zambia. However, severe health system and human resource constraints make it difficult to scale up services [51]. Expedited cataract surgery appears very cost-effective in New Zealand, being considered itself very cost-effective, and its value appears largely driven by the falls prevention benefits [66]. According to the literature, cataract surgery has been demonstrated to be good value in terms of benefits net of costs, except for patients whose vision is good at the time of their operation [62].
Concerning cataract surgery waiting times, developed economies like Australia [29] and Canada [67] have evaluated the importance of reducing waiting times for cataract surgery, reporting gains in broad patient outcomes, such as quality of life. These gains can be achieved with good value for money [29, 67].
First eye cataract surgery has been associated with gain in visual function, visual disability, activity, anxiety and depression, confidence and quality of life, resulting cost-effective, especially if a lifelong time frame is considered [49]. On the other hand, second eye cataract surgery has been reported as an extremely cost-effective procedure in ophthalmology when compared with other interventions across medical specialties. Busbee et al. [54] investigated the benefit gained from second eye cataract surgery, and showed in their results slight differences in cost/QALY gained from first eye surgery, suggesting that patients with good vision in one eye and visual loss from cataract in the fellow eye derive substantial benefit from cataract extraction.
Above all, cataract surgery in the first eye, second eye, or both eyes conferred considerable patient value and was very cost-effective by any standard. Both patient value gain and cost-effectiveness have improved since 2012 and before. Cataract surgery in 2018 was 75% more cost-effective than in 2000 in the USA [65]. In bilateral cataract patients, the replacement of the lens in the worst-affected eye was considered as a cost-effective way to improve vision and quality of life. However, it was unclear whether or not lens replacement surgery in the second eye provided enough further benefit to be considered worthwhile by patients and cost-effective for a health system. Health systems, such as the National Health System (NHS) in the UK, have investigated the benefit of the second eye cataract surgery [56, 57]. Results from the NHS showed that second eye cataract surgery is generally cost-effective in the long term, being unlikely cost-effective in the short term for those with mild visual dysfunction pre-operatively [56, 57].
The TTO method is used to determine utility values. At the same time, it is accepted as a formal method for quantifying the relative impact of a given health state or disease on patient lives [7, 16, 61]. VA and visual disability significantly affect utilities controlled for age and ophthalmic comorbidity. It is thus possible to use data on VA and disability in large registries to estimate the cost-effectiveness of cataract surgery and to compare the cost per QALY gained with other healthcare interventions [58]. Several studies reported that cataract surgery is cost-effective, improves patient perceived quality of life, even in a subpopulation of patient with a lower predicted probability of reporting improved visual functioning after surgery [59,60,61, 63].
In general, bilateral cataract extraction can be performed with varying interval between the two surgeries: immediate sequential cataract surgery (ISCS) or delayed sequential cataract surgery (DSCS), with an interval of weeks or months between surgeries. Several studies have reported that ISCS is a cost-effective procedure compared with DSCS. The value for the patient of ISCS compared to DSCS depends on how long the period will be between first and second eye surgery in DSCS and also on the patient’s survival time after surgery [68, 69].
Currently, the high prevalence of cataract is still a public health problem. CEA are evaluated for surgical techniques; however, costs of clinical systems of cataract grading and preoperative new measurements have also been investigated. The high costs of setting up the novel technology are offset by low running costs [71, 72]. In fact, other preoperative screening measurements have been evaluated, such as optical coherence tomography (OCT) during the evaluation of a patient considering cataract surgery, being cost-effective from a third-party payer and societal perspective, as it could increase the detection of macular pathologies and improved the QALYs over time [74].
Numerous studies have estimated the cost-effectiveness of cataract surgery with multifocal IOLs compared to monofocal IOLs [75,76,77,78,79]. Orme et al. [75] showed that multifocal IOLs are cost-effective for patients who desire spectacle independence. However, multifocal IOLs may not be the most cost-effective options for patients who require excellent night vision or do not tolerate any visual disturbances, such as glare or halos. Similar results were described by Hu et al. [79] and Bala et al. [86], considering multifocal diffractive IOL and non-diffractive EDOF IOLs as cost-effective strategies compared to monofocal IOLs for patients seeking spectacle independence.
Lafuma et al. [76] and De Vries et al. [77] compared lifetime costs of spectacle independence after cataract surgery, concluding that multifocal IOLs are a cost-saving alternative to spectacles for patients requiring cataract surgery. Maxwell et al. [32] also proved that the net benefit of the multifocal IOL exceeded its acquisition cost and the net benefit of the monofocal IOL, demonstrating its value to select patients with cataract willing to pay a premium for spectacle independence. Lin et al. [78] showed that multifocal IOLs provide better effectiveness on vision-related indicators like postoperative ICER of postoperative spectacle independence rate and binocular best-corrected VA in near vision.
Other authors have evaluated the cost-effectiveness of toric IOLs in patients with corneal astigmatism compared with monofocal IOLs [81, 83]. Pineda et al. [81] evaluated the economic value of improved uncorrected distance VA after surgery. Their results showed that toric IOLs had higher total costs during the first year, but were lower across patients’ lifetimes. Treating astigmatism with toric IOLs at the time of cataract removal yielded several important benefits, such as VA and patient HRQoL improvement, and consequently long-term healthcare cost-savings. However, opposite results were reported by Simons et al. [83] who concluded that toric IOLs were not cost-effective and increased healthcare costs in the short term. They found that although toric IOLs improved uncorrected distance visual acuity (UDVA) and spectacle independence after cataract surgery, there was not improvement in HRQoL. Discrepancies between studies could be due to the method used to determine QALYs by Pineda et al. [81] leading in an overestimation of toric IOL effectiveness.
Cost-effectiveness of different IOL materials implanted in cataract surgery has also been evaluated. Jain et al. [84] assessed the effects of different types of cataract surgeries and IOL materials as well as QALYs and vision-related quality of life of patients with cataract, using EQ-5D and IND-VFQ 33 instruments, respectively. All three types of surgical procedures (ECCE, PCS, and SICS) showed a QALY gain and vision-related quality of life gain. Rigid poly(methyl methacrylate) (PMMA) and foldable lenses were also analyzed in this study. Quality of life was found to be better in foldable lenses compared to the rigid lenses, and the authors recommended to use a foldable lens with PCS as the incision size is smaller and a rigid lens with ECCE and SICS because of the larger incision size. Results from Lafuma et al. [80] showed that cost-effectiveness ratios of hydrophobic acrylic IOLs were better than those of other types of IOL materials used in most countries. The study showed that at 3 years postoperatively, patients implanted with hydrophobic acrylic IOLs presented less often for Nd:YAG laser therapy than patients implanted with other materials such as PMMA, silicone, and hydrophilic acrylic.
In complicated cataract surgery, the absence of adequate capsular support necessitates alternative approaches to IOL placement, which include scleral fixation in the posterior chamber (SF-IOL), iris fixation, or placement in the anterior chamber angle (AC-IOL) in a single procedure or a subsequent surgery. Ranno et al. [85] compared visual, anatomical, and economic outcomes of patients with secondary AC-IOL implantation and secondary SF-IOL implantation. The global cost of implantation was significantly lower for AC-IOL, but the ICER justified the SF-IOL implantation in patients with low endothelial cell density (ECD). In their results, the authors showed that the ICER favored the secondary AC-IOL implantation in elder patients with good ECD. Although PC-IOL had higher costs, it was recommended to be implanted in patients with low ECD and long life expectancy.
Strengths and Limitations of the Mapping Review
The present systematic mapping review has some limitations. As an intrinsic characteristic of a mapping review, this study does not include extraction of study results or synthesis of results for a deep analysis [21]. Only English language publications were included, which could limit the inclusion of studies.
On the other hand, the limitations of this mapping review are coincident with other mapping reviews, such as no formal quality assessment or assessment applicability or usefulness of identified research methods [88]. Thus, the level of evidence was not evaluated for each study in order to provide information about quality of evidence of the studies included in the mapping review.
Future Research
Even though several studies have evaluated the cost-effectiveness between surgical techniques in cataract surgery, there are inconsistencies in their results. ECCE and MSICS seem to be cost-effective compared to PCS, and PCS is cost-effective compared with LCS. Given the differences between studies, there is a need for further investigations about cost-effectiveness and surgical methods in cataract surgery.
There was clear evidence that cataract surgery is more cost-effective than other ophthalmic and non-ophthalmic health interventions, improving visual function and patient perception quality of life. Cataract surgery costs have decreased over the years; however, their cost-effectiveness should be cautiously evaluated according to the country and the population assessed.
Cataract surgery waiting time is an important factor to consider as vision loss has a huge and broad-ranging impact on society. Priority needs to be given to avoid preventable vision loss, to treat treatable eye diseases, and to increase research into vision loss from eye diseases that can be treated. ISCS has been demonstrated to be a more cost-effective method compared with DSCS. This finding could be highly useful for policy-makers, decision-makers, clinicians, hospital administrators, and payers in making cost-efficient decisions, although more robust studies are needed to confirm these findings.
First eye and especially second eye cataract surgery are the most cost-effective procedures in ophthalmology and other medical specialties. They are associated with gain visual function, visual disability, and quality of life among others. In spite of the large number of publications, there is a need for more research because of inconsistent results reported for short- and long-term outcomes of second eye cataract surgery.
Regarding to the peer-reviewed literature, new grading preoperative cataract systems and preoperative additional measurements such as OCT should be introduced in clinical practice to save time, costs, and resources by eliminating unnecessary patient visits. However, few studies have focused on the economic analysis of the preoperative protocols.
The desire for spectacle independence allowed by multifocal IOLs is greatly valued by patients with cataracts who are willing to pay for the advanced technology. Multifocal IOLs can be highly cost-effective for patients who prefer to be spectacle independent, and therefore it is important to ensure that patients have realistic expectations when making choices between monofocal and multifocal IOLs.
References
Burton MJ, Ramke J, Marques AP, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Global Health. 2021;9:e489–551. https://doi.org/10.1016/S2214-109X(20)30488-5.
Marques AP, Ramke J, Cairns J, et al. Global economic productivity losses from vision impairment and blindness. EClinicalMedicine. 2021;35:100852. https://doi.org/10.1016/J.ECLINM.2021.100852.
Assi L, Rosman L, Chamseddine F, et al. Eye health and quality of life: an umbrella review protocol. BMJ Open. 2020;10:e037648. https://doi.org/10.1136/BMJOPEN-2020-037648.
Atik A, Barton K, Azuara-Blanco A, Kerr NM. Health economic evaluation in ophthalmology. Br J Ophthalmol. 2021;105:602–7. https://doi.org/10.1136/bjophthalmol-2020-316880.
Grimes CE, Henry JA, Maraka J, Mkandawire NC, Cotton M. Cost-effectiveness of surgery in low- and middle-income countries: a systematic review. World J Surg. 2014;38:252–63.
Javed Q. Cost-effectivness of surgical interventions in low and middle income countries (LMICs). Int J Surg. 2017;47:S58.
Hahn U, Krummenauer F. Results and methodology of cost–utility evaluation of cataract surgery in developed countries: quality-adjusted life years and cataract. J Cataract Refract Surg. 2017;43:839–47.
Gray AM, Clarke PM, Wolstenholme JL, Wordsworth S. Applied methods of cost-effectiveness analysis in health care. 2010. Oxford: OUP; 1386. ISBN 9780199227280.
Gov.UK. Cost effectiveness analysis: health economic studies. https://www.gov.uk/guidance/cost-effectiveness-analysis-health-economic-studies. Accessed 11 Nov 2022.
Gov.UK. Cost utility analysis: health economic studies. https://www.gov.uk/guidance/cost–utility-analysis-health-economic-studies. Accessed 11 Nov 2022.
Gafni A. The standard gamble method: what is being measured and how it is interpreted. Health Serv Res. 1994;29(2):207–24.
Dixon P, Hollingworth W, Sparrow J. Mapping to quality of life and capability measures in cataract surgery patients: from Cat-PROM5 to EQ-5D-3L, EQ-5D-5L, and ICECAP-O using mixture modelling. MDM Policy Pract. 2020;5:2381468320915447.
Brauer CA, Rosen AB, Greenberg D, Neumann PJ. Trends in the measurement of health utilities in published cost–utility analyses. Value Heal. 2006;9:213–8. https://doi.org/10.1111/J.1524-4733.2006.00116.X.
Pinto Prades JL, Sánchez Martínez FI. Métodos Para La Evaluación Económica de Nuevas Prestaciones. Madrid: Ministerio de Sanidad y Consumo; 2003.
Brown GC, Brown MM, Chaudhry I, Stein JD. Opportunities to reduce potential bias in ophthalmic cost–utility analysis. JAMA Ophthalmol. 2021;139:389–97. https://doi.org/10.1001/jamaophthalmol.2020.6591.
Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis. 1987;40:593–600. https://doi.org/10.1016/0021-9681(87)90019-1.
Brown MM, Brown GC, Sharma S, Kistler J, Brown H. Utility values associated with blindness in an adult population. Br J Ophthalmol. 2001;85:327–31. https://doi.org/10.1136/BJO.85.3.327.
Brown MM, Brown GC, Sharma S, Hollands H, Landy J. Quality of life and systemic comorbidities in patients with ophthalmic disease. Br J Ophthalmol. 2002;86:8–11. https://doi.org/10.1136/BJO.86.1.8.
Miake-Lye IM, Hempel S, Shanman R, Shekelle PG. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. 2016. https://doi.org/10.1186/s13643-016-0204-x.
Hetrick SE, Parker AG, Callahan P, Purcell R. Evidence mapping: illustrating an emerging methodology to improve evidence-based practice in youth mental health. J Eval Clin Pract. 2010;16:1025–30.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108.
NIHR Centre for Reviews and Dissemination. CRD Database. http://www.crd.york.ac.uk/CRDWeb/ResultsPage.asp. Accessed 11 Sept 2021.
National Institute for Health and Care Excellence. NICE. The Guidelines Manual; 2012; ISBN 978-1-4731-1906-2.
Brown GC, Brown MM, Sharma S, et al. Value-based medicine and ophthalmology: an appraisal of cost–utility analyses. Trans Am Ophthalmol Soc. 2004;102:177.
Plüddemann A, Aronson JK, Onakpoya I, Heneghan C, Mahtani KR. Redefining rapid reviews: a flexible framework for restricted systematic reviews. BMJ Evid-Based Med. 2018;23:201–3. https://doi.org/10.1136/bmjebm-2018-110990.
Dominski FH, Lorenzetti Branco JH, Buonanno G, Stabile L, da Gameiro Silva M, Andrade A. Effects of air pollution on health: a mapping review of systematic reviews and meta-analyses. Environ Res. 2021;201: 111487. https://doi.org/10.1016/J.ENVRES.2021.111487.
Fernández-Sotos P, Torio I, Fernández-Caballero A, et al. Social cognition remediation interventions: a systematic mapping review. PLoS ONE. 2018;14:1–20. https://doi.org/10.1371/journal.pone.0218720.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. https://doi.org/10.1371/journal.pmed.1000100.
Taylor H, Pezzullo L, Keeffe J. The economic impact and cost of visual impairment in Australia. Br J Ophthalmol. 2006;90(3):272–5.
Rochmah TN, Wulandari A, Dahlui M, Ernawaty, Wulandari RD. Cost effectiveness analysis using disability-adjusted life years for cataract surgery. Int J Environ Res Public Health. 2020;17:6010. https://doi.org/10.3390/ijerph17166010
Kapse R, Agarwal S, Rishikeshi N, et al. Cost analysis of pediatric cataract surgery in a tertiary eye care hospital in Western India. Indian J Ophthalmol. 2022;70:420. https://doi.org/10.4103/ijo.IJO_1229_21.
Maxwell WA, Waycaster CR, D’Souza AO, Meissner BL, Hileman K. A United States cost-benefit comparison of an apodized, diffractive, presbyopia-correcting, multifocal intraocular lens and a conventional monofocal lens. J Cataract Refract Surg. 2008;34:1855–61. https://doi.org/10.1016/j.jcrs.2008.07.024.
Weinstein MC, Torrance G, McGuire A. QALYs: the basics. Value Heal. 2009;12:S5–9. https://doi.org/10.1111/j.1524-4733.2009.00515.x.
Paulden M. Calculating and interpreting ICERs and net benefit. Pharmacoeconomics. 2020;38:785–807. https://doi.org/10.1007/s40273-020-00914-6.
Asimakis P, Coster DJ, Lewis DJ. Cost effectiveness of cataract surgery: a comparison of conventional extracapsular surgery and phacoemulsification at flinders medical centre. Aust N Z J Ophthalmol. 1996;24:319–25. https://doi.org/10.1111/J.1442-9071.1996.TB01602.X.
Rizal AM, Aljunid SM, Normalina M, et al. Cost analysis of cataract surgery with intraocular lens implantation: a single blind randomised clinical trial comparing extracapsular cataract extraction and phacoemulsification. Med J Malaysia. 2003;58:380–6.
Manaf MRA, Aljunid SM, Annuar FH, Leong CK, Mansor N. Cost-effectiveness analysis of cataract surgery with intraocular lens implantation: extracapsular cataract extraction versus phacoemulsification. Med J Indones. 2007;16:25–31.
Jongsareejit A, Wiriyaluppa C, Kongsap P, Phumipan S. Cost-effectiveness analysis of manual small incision cataract surgery (MSICS) and phacoemulsification (PE). J Med Assoc Thail. 2012;95:212–20.
Abell RG, Vote BJ. Cost-effectiveness of femtosecond laser-assisted cataract surgery versus phacoemulsification cataract surgery. Ophthalmology. 2014;121:10–6.
Khan A, Amitava A, Rizvi SA, Siddiqui Z, Kumari N, Grover S. Cost-effectiveness analysis should continually assess competing health care options especially in high volume environments like cataract surgery. Indian J Ophthalmol. 2015;63:496. https://doi.org/10.4103/0301-4738.162600.
Schweitzer C, Brezin A, Cochener B, et al. Femtosecond laser-assisted versus phacoemulsification cataract surgery (FEMCAT): a multicentre participant-masked randomised superiority and cost-effectiveness trial. Lancet. 2020;395:212–24.
Wulandari A, Dahlui M, Wulandari RD, Rochmah TN. Cost effectiveness analysis between small incision cataract surgery and phacoemulsification. J Heal Transl Med. 2020;23:231–7.
Tuominen R, Immonen I, Raivio I. Economic evaluation of cataract surgery: a comparison between IOL and Non-IOL techniques. Acta Ophthalmol. 1988;66:577–81. https://doi.org/10.1111/j.1755-3768.1988.tb04383.x.
Marseille E. Cost-effectiveness of cataract surgery in a public health eye care programme in Nepal. Bull World Health Organ. 1996;74:319–24.
Busbee BG, Brown MM, Brown GC, Sharma S. Incremental cost-effectiveness of initial cataract surgery. Ophthalmology. 2002;109:606–12. https://doi.org/10.1016/S0161-6420(01)00971-X.
Baltussen R, Sylla M, Mariotti SP. Cost-effectiveness analysis of cataract surgery: a global and regional analysis. Bull World Health Organ. 2004;82:338–45.
Räsänen P, Krootila K, Sintonen H, et al. Cost-utility of routine cataract surgery. Health Qual Life Outcomes. 2006;4:74. https://doi.org/10.1186/1477-7525-4-74.
Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114:1670–8.
Sach TH, Foss AJE, Gregson RM, et al. Falls and health status in elderly women following first eye cataract surgery: an economic evaluation conducted alongside a randomised controlled trial. Br J Ophthalmol. 2007;91:1675–9.
Brown GC, Brown MM, Menezes A, Busbee BG, Lieske HB, Lieske PA. Cataract surgery cost utility revisited in 2012. Ophthalmology. 2013;120:2367–76. https://doi.org/10.1016/j.ophtha.2013.04.030.
Griffiths UK, Bozzani FM, Gheorghe A, Mwenge L, Gilbert C. Cost-effectiveness of eye care services in Zambia. Cost Eff Resour Alloc. 2014;12:6. https://doi.org/10.1186/1478-7547-12-6.
Boyd M, Kho A, Wilson G, Wilson N. Expediting cataract surgery in New Zealand is cost-effective for falls prevention and improving vision-so what might be the next steps? N Z Med J. 2019;132:73–8.
Essue BM, Jan S, Phuc HT, Dodson S, Armstrong K, Laba T-L. Who benefits most from extending financial protection for cataract surgery in Vietnam? An extended cost-effectiveness analysis of small incision surgery. Health Policy Plan. 2018;550000:399–407. https://doi.org/10.1093/heapol/czz181.
Busbee BG, Brown MM, Brown GC, Sharma S. Cost-utility analysis of cataract surgery in the second eye. Ophthalmology. 2003;110:2310–7. https://doi.org/10.1016/S0161-6420(03)00796-6.
Sach TH, Foss AJE, Gregson RM, et al. Second-eye cataract surgery in elderly women: a cost–utility analysis conducted alongside a randomized controlled trial. Eye. 2010;24:276–83. https://doi.org/10.1038/eye.2009.112.
Frampton G, Harris P, Cooper K, et al. The clinical effectiveness and cost-effectiveness of second-eye cataract surgery: a systematic review and economic evaluation. Health Technol Assess. 2014;18:1–206. https://doi.org/10.3310/hta18680.
Cooper K, Shepherd J, Frampton G, Harris P, Lotery A. The cost-effectiveness of second-eye cataract surgery in the UK. Age Ageing. 2015;44:1026–31. https://doi.org/10.1093/ageing/afv126.
Kobelt G, Lundström M, Stenevi U. Cost-effectiveness of cataract surgery: method to assess cost-effectiveness using registry data. J Cataract Refract Surg. 2002;28:1742–9. https://doi.org/10.1016/S0886-3350(02)01220-8.
Naeim A, Keeler EB, Gutierrez PR, Wilson MR, Reuben D, Mangione CM. Is cataract surgery cost-effective among older patients with a low predicted probability for improvement in reported visual functioning? Med Care. 2006;44:982–9. https://doi.org/10.1097/01.mlr.0000228216.18270.3e.
Lansingh VC. Use of global visual acuity data in a time trade-off approach to calculate the cost utility of cataract surgery. Arch Ophthalmol. 2009;127:1183. https://doi.org/10.1001/archophthalmol.2009.113.
Hiratsuka Y. Cost-effectiveness of cataract surgery in Japan. Jpn J Ophthalmol. 2011;55:333–42. https://doi.org/10.1007/S10384-011-0041-3/TABLES/9.
Weale M. A cost-benefit analysis of cataract surgery based on the English longitudinal survey of ageing. J Health Econ. 2011;30:730–9. https://doi.org/10.1016/j.jhealeco.2011.05.008.
Hiratsuka Y. Cost-utility analysis of cataract surgery in Japan: a probabilistic Markov modeling study. Jpn J Ophthalmol. 2013;57:391–401. https://doi.org/10.1007/s10384-013-0238-8.
Moore DB, Slabaugh MA. Surgical outcomes and cost basis for resident-performed cataract surgery in an uninsured patient population. JAMA Ophthalmol. 2013;131:891. https://doi.org/10.1001/jamaophthalmol.2013.202.
Brown GC, Brown MM, Busbee BG. Cost-utility analysis of cataract surgery in the United States for the year 2018. J Cataract Refract Surg. 2019;45:927–38. https://doi.org/10.1016/j.jcrs.2019.02.006.
Boyd M, Kvizhinadze G, Kho A, Wilson G, Wilson N. Cataract surgery for falls prevention and improving vision: modelling the health gain, health system costs and cost-effectiveness in a high-income country. Inj Prev. 2020;26:302–9. https://doi.org/10.1136/injuryprev-2019-043184.
Hopkins RB, Tarride J-E, Bowen J, et al. Cost-effectiveness of reducing wait times for cataract surgery in Ontario. Can J Ophthalmol. 2008;43:213–7. https://doi.org/10.3129/i08-002.
Lundström M, Albrecht S, Roos P. Immediate versus delayed sequential bilateral cataract surgery: an analysis of costs and patient value. Acta Ophthalmol. 2009;87:33–8. https://doi.org/10.1111/j.1755-3768.2008.01343.x.
Malvankar-Mehta MS, Filek R, Iqbal M, et al. Immediately sequential bilateral cataract surgery: a cost-effective procedure. Can J Ophthalmol. 2013;48:482–8. https://doi.org/10.1016/j.jcjo.2013.05.004.
Cernat A, Jamieson M, Kavelaars R, et al. Immediate versus delayed sequential bilateral cataract surgery in children: a cost-effectiveness analysis. Br J Ophthalmol. 2022;106:211–7. https://doi.org/10.1136/bjophthalmol-2020-316507.
Dimock J, Robman LD, McCarty CA, Taylor HR. Cost-effectiveness of digital cataract assessment. Aust N Z J Ophthalmol. 1999;27:208–10. https://doi.org/10.1046/j.1440-1606.1999.00207.x.
Jastrzebski A, Villafranca A, Sethi S, Bellan L. Safety and comparative costs of preoperative assessments for cataract surgery: traditional mandatory assessment versus a novel graded assessment system. Can J Anesth. 2016;63:842–50.
Meltzer ME, Congdon N, Kymes SM, et al. Cost and expected visual effect of interventions to improve follow-up after cataract surgery. JAMA Ophthalmol. 2017;135:85. https://doi.org/10.1001/jamaophthalmol.2016.4735.
Leung EH, Gibbons A, Koch DD. Cost-effectiveness of preoperative oct in cataract evaluation for multifocal intraocular lens. Ophthalmology. 2020;127:859–65. https://doi.org/10.1016/j.ophtha.2020.01.049.
Orme ME, Paine AC, Teale CW, Kennedy LM. Cost-effectiveness of the AMOArray multifocal intraocular lens in cataract surgery. J Refract Surg. 2002;18:162–8.
Lafuma A, Berdeaux G. Modelling lifetime cost consequences of ReSTOR in cataract surgery in four European countries. BMC Ophthalmol. 2008;8:12. https://doi.org/10.1186/1471-2415-8-12.
De Vries NE, Laurendeau C, Lafuma A, Berdeaux G, Nuijts RMMA. Lifetime costs and effectiveness of ReSTOR compared with a monofocal IOL and Array-SA40 in the Netherlands. Eye. 2010;24:663–72. https://doi.org/10.1038/eye.2009.151.
Lin J-C, Yang M-C. Cost-effectiveness comparison between monofocal and multifocal intraocular lens implantation for cataract patients in Taiwan. Clin Ther. 2014;36:1422–30. https://doi.org/10.1016/j.clinthera.2014.07.009.
Hu JQ, Sarkar R, Murphy J, Afshari NA. Cost-effectiveness of multifocal intraocular lenses compared to monofocal intraocular lenses in cataract surgery. Investig Ophthalmol Vis Sci. 2018;59:208–305.
Smith AF, Lafuma A, Berdeaux G, et al. Cost-effectiveness analysis of PMMA, silicone, or acrylic intra-ocular lenses in cataract surgery in four European countries. Ophthalmic Epidemiol. 2005;12:343–51.
Pineda R, Denevich S, Lee WC, Waycaster C, Pashos CL. Economic evaluation of toric intraocular lens: a short- and long-term decision analytic model. Arch Ophthalmol. 2010;128:834–40. https://doi.org/10.1001/archophthalmol.2010.127.
Kristianslund O, Dalby M, Moe MC, Drolsum L. Cost-effectiveness analysis in a randomized trial of late in-the-bag intraocular lens dislocation surgery: repositioning versus exchange. Acta Ophthalmol. 2019;97:771–7. https://doi.org/10.1111/aos.14108.
Simons RWP, Visser N, van den Biggelaar FJHM, et al. Trial-based cost-effectiveness analysis of toric versus monofocal intraocular lenses in cataract patients with bilateral corneal astigmatism in the Netherlands. J Cataract Refract Surg. 2019;45:146–52.
Jain S, Chauhan A, Rajshekar K, et al. Generic and vision related quality of life associated with different types of cataract surgeries and different types of intraocular lens implantation. PLoS ONE. 2020;15:e0240036. https://doi.org/10.1371/journal.pone.0240036.
Ranno S, Rabbiolo GM, Lucentini S, et al. Angle-supported intraocular lens versus scleral-sutured posterior chamber intraocular lens in post-cataract surgery aphakic patients: two-year follow-up cost-effectiveness analysis. Int Ophthalmol. 2022;42:871–9. https://doi.org/10.1007/s10792-021-02068-6.
Athanasiov P, Bala C, Holland J, Dhariwal M, Gupta A, Rathi H. A cost-effectiveness analysis of AcrySof IQ vivity intraocular lens from private health fund perspective in Australia. Clin Exp Ophthalmol. 2022;49:878–9.
Laupacis A, Feeny D, Detsky AS, Tugweli PX. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992;146(4):473–81.
Diane C. What is a “mapping study?” J Med Libr Assoc. 2016;104:76–8. https://doi.org/10.3163/1536-5050.104.1.013.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
Conceptualization, Jose Ginel, Noemi Burguera and Joaquín Fernández; resources, Joaquín Fernández; writing–original draft preparation, Jose Ginel and Noemi Burguera; writing–review and editing, David Piñero and Alejandro Sáez; supervision, David Piñero and Alejandro Sáez; project administration, Joaquín Fernández. All authors have read and agreed to the published version of the manuscript.
Disclosures
Jose Ginel, Noemi Burguera, Carlos Rocha-de-Lossada, David Piñero, Alejandro Sáez and Joaquín Fernández declare that they have no competing interests.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ginel, J., Burguera, N., Rocha-de-Lossada, C. et al. Economic Evaluation of Cataract: A Systematic Mapping Review. Ophthalmol Ther 12, 789–807 (2023). https://doi.org/10.1007/s40123-023-00678-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00678-0