Abstract
Diabetic macular oedema (DMO) is the leading cause of vision loss associated with diabetic eye disease. The exponential increase in the diabetic population and thus, of DMO is an impetus for optimizing the management of DMO. One major challenge in DMO management is the discrepancy between treatment outcomes seen in clinical trials and the real world. Contrary to the homogeneity, better patient motivation and shorter study durations seen in randomised control trials, routine clinical practice is fraught with more diverse populations, undertreatment and variable compliance with long-term therapy. Under both circumstances, this review aims to compare efficacy outcomes and adverse events of DMO therapies within the scope of anti-vascular endothelial growth factor (anti-VEGF) medications, specifically the commonly used ones—bevacizumab, ranibizumab and aflibercept. Impediments and methods to achieve better treatment outcomes in the real world will be addressed to achieve better outcomes. Low- to lower-middle-income countries are faced with even more barriers which range from paucity of data on epidemiology and treatment response to scarce human and financial resources to poorer national level attention and then basic issues like transportation. Additionally, to address the lack of a global consensus in DMO treatment, this review generates and recommends, for clinical and research purposes, an up-to-date consensus algorithm for DMO management universally. Underpinned by results from clinical trials and recent guidelines, this therapeutic flowchart can be utilised in various resource settings including low- and lower-middle-income countries where affordability is a major deterrent to treatment access.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Diabetic macular oedema, the leading cause of visual impairment in patients with diabetes, is set to increase as the prevalence of diabetes mellitus increases globally to near epidemic levels. |
Broader insights into the pathophysiology of DMO led to a therapeutic breakthrough—the advent of anti-VEGF medications; however, gaps exist in the optimal utilisation of these medications. |
This article reviews the efficacy results from landmark randomised controlled trials as against those obtained from typical daily clinical practice outcomes. Baseline clinical characteristics of these studies are also reviewed, compared, and noted to differ. |
Many barriers exist to achieve long-term treatment outcomes in the real-world which get close to the outcomes seen in clinical trials. The disparity is more marked in resource-poor countries because of the challenges faced by clinicians, patients, and healthcare payors in these settings. |
Introduction
Diabetes mellitus (DM) is a disease of public health concern. This is due to its global rise to epidemic levels from urbanization, increased sedentary lifestyle and obesity rates. As of 2019, 463 million people had DM globally according to the International Diabetes Federation and this figure is projected to increase to 700 million in 2045 [1]. This alarming rise and increased lifespan of people with diabetes from medical therapy advancements has fuelled the rise in its complications.
Diabetic macular oedema (DMO) is the principal cause of impaired vision in people with diabetes. It is a microvascular condition manifesting as retinal thickening due to exudation and fluid leak in the macula [2]. The sight-threatening effect of DMO can be devastating, taking a significant toll on the individual’s quality of life especially when bilateral, which is common, being borne out of a systemic disease. A Canadian quality of life survey among patients with DMO revealed that 72% of the participants had bilateral DMO [3]. Of therapeutic decision-making importance is the DMO classification based on location of DMO into centre-involving (CI-DMO) and non-centre-involving DMO. From the International Council of Ophthalmology guidelines (ICO), CI-DMO is defined as retinal thickening in the macular involving the central 1 mm, which is the central subfield zone and requires treatment to avoid vision loss [4]. The more commonly used spectral domain optical coherence tomography machines (SD-OCTs) measure macular thickness from the retinal nerve fibre layer to the retinal pigment epithelium (RPE) Bruch’s membrane complex and as regards the central subfield thickness (CST) threshold for treatment, the Diabetic Retinopathy Clinical Research network (DRCR.net) Protocol T study set this at 320 µm or higher for men and 305 µm or higher for women on Heidelberg Spectralis OCT while the National Institute for Health and Care Excellence (NICE) guidelines utilizes 400 µm or higher [5, 6].
DMO affects otherwise economically active individuals (20–79 years). Although data as regards prevalence and incidence rates of DMO are of limited availability compared to those of diabetic retinopathy (DR), global DMO prevalence was reported by Yau et al. to be 7.4% almost a decade ago [7]. Very recently, Teo et al. documented a global prevalence of clinically significant macular oedema, which is a severe form of DMO, to be 4.07% [8]. Interregional disparities were noted in the rates, some of which include the Western Pacific region, which had the highest (5.34%); Europe (3.16%); South-East Asia (2.08%); Africa at the lowest (0.85%). In contrast to these percentages, Asia and Africa have been described as “hotspots” for DM [9], especially the type 2 form; thus, the lower rate reported by Teo et al. in Africa might reflect a lack of data. The Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) reported a 20% and 14–25% incidence of DMO in type 1 and type 2 DM respectively over a 10-year follow-up duration [10].
Vascular endothelial growth factor (VEGF) has logically been a target for DMO treatment due to the central role it plays in the pathogenesis of DMO. Pharmaceutical agents which block the action of VEGF-A are currently the mainstay in the treatment of DMO and over the years, the arsenal of anti-VEGF medications has been improved upon by creation of increasingly higher affinity drugs using innovative biotechnological approaches.
Numerous randomised control trials (RCTs) have proven the efficacy and safety of anti-VEGF drugs, but results obtained in real life have not been commensurate with those seen in RCTs. With more heterogenous populations, including groups excluded from RCTs, real-world studies (RWS) can be better extrapolated to daily practice which equally have a large panel of unselected diversified patients. The strict inclusion and exclusion criteria used to select patients for inclusion in RCTs is not compatible with day-to-day practice where treatment is offered to a much wider range of patients. This review aims to compare results from RCTs and RWS on anti-VEGF use in DMO, elucidate barriers to treatment success in the real world and discuss the implications in low- and lower-middle-income countries.
Methods
A literature search was performed using two databases, Ovid MEDLINE (1947–November 2021) and Ovid Embase (1946–November 2021) and the records were retrieved. The keywords include “diabetic macular oedema”, “anti vascular endothelial growth factor”, “bevacizumab”, “ranibizumab”, “aflibercept” and synonyms were searched using free text words and Medical Subject Headings (MeSH) terms, merged with Boolean operators “OR” and “AND”. The initial wide search was narrowed down with extra search terms which include “Randomised clinical trials”, “Systematic review”, “Clinical trial”, “meta-analysis” for feasibility’s sake. “Real-world” was then included into the search strategy to obtain real-life anti-VEGF data. After the references were exported to EndNote X9 software, de-duplication was done. An article-by-article screening was done in a three-staged sequence: (i) title; (ii) abstract and (iii) full article to ensure organization and no omissions. Article relevance was defined as inclusion of key trials in anti-VEGF use in DMO, real-world studies on anti-VEGF use in DMO, DR/DMO therapy in low- to middle-income countries. A further screening led to the exclusion of literature reviews, conference abstracts, commentaries/letters, and book chapters. Relevant studies remaining were further reviewed in stage iii alongside topic-related articles which had been manually added from their reference lists. Essential articles selected from these were the focus of study.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. Thus, ethical approval was not required.
Anti-VEGF Therapy in DMO
The three commonly used anti-VEGF medications used at present in DMO therapy are bevacizumab, ranibizumab and aflibercept. Pegaptanib was the first aptamer to be approved for use in humans and had a short-lived use. This was due to its modest efficacy as it selectively binds VEGF-165 and was therefore replaced by other more effective anti-angiogenic drugs which bind more isoforms. Bevacizumab, a fully humanized monoclonal antibody to VEGF-A, is approved by the US Food and Drug Administration (FDA) for use in colon cancers and thus is utilised as an off-label medication in ophthalmological conditions including DMO. It binds all VEGF-A isoforms.
Originating from the same parent molecule as bevacizumab, ranibizumab is a monoclonal antibody fragment which has the advantage of small size (48 kDa). This allows an expedited clearance from the vitreous into the retina. Although it is able to bind all the VEGF-A isoforms like bevacizumab, the dissociation constant of ranibizumab is a tenth (< 179 pM) that of bevacizumab (1800 pM) translating to tighter binding [11, 12].
Aflibercept was introduced into clinical practice after bevacizumab and ranibizumab. This fusion protein and soluble decoy protein was created by pairing of the second and third binding domains from VEGF receptors 1 and 2 respectively. It binds with more affinity to VEGF-A compared with its predecessors, and additionally binds VEGF-B and placental growth factor (PIGF) [13].
Anti-VEGF Treatment of DMO: Contrast Between RWS and RCTs
Patient Demographics and Baseline Characteristics
The patient selection criteria in RCTs streamline the study populations via exclusion which may be deemed as a bias. For instance, older participants have been reported in some RWS [14,15,16,17] on anti-VEGF use in DMO with average participant age range of 64.5–67.6 years compared to RCTs [5, 18,19,20] which ranged from 60 to 64 years depicting an underrepresentation of older age groups in RCT. With age as a risk factor for comorbidities like hypertension which, in turn, is a risk factor for DMO progression, older participants may contribute to poorer outcomes in RWS compared to RCTs.
Regarding baseline characteristics, the patients with DMO in the real-world LUMINOUS study had a fairly similar or higher basal mean HBA1c (7.9%) compared to RCTs like the RISE and RIDE (7.6–7.7%) and the VIVID and VISTA studies (7.8–7.9%) [17,18,19]. However, the higher standard deviation (3.4) noted in the LUMINOUS study compared to the aforementioned RCTs (1.3–1.6) signifies that a broader cohort was included in the LUMINOUS study which is seen in real-world situations.
Another difference is the increased presence of ocular and systemic comorbidities in participants of RWS [14, 17] compared to RCTs [18, 20]. This is expected, considering the strict eligibility criteria in RCTs. Comorbidities such as hypertension, hyperlipidaemia, previous stroke, diabetic nephropathies, and neuropathies were well represented in RWS and may cause poorer outcomes in these studies due to negative impact on hospital attendance as these patients attend multiple clinics.
Comparing RWS which administered ranibizumab, the BOREAL and LUMINOUS studies had less mean baseline visual acuity (VA) than the RCT counterpart, the RESTORE study (59.2 vs 56.3 vs 64.8 letters respectively) [14, 17, 20]. On the contrary, in studies on aflibercept use in DMO, the VIVID and VISTA study had worse baseline VA than the real-life APOLLON study [15, 19]. Worse baseline VAs may paradoxically produce better outcomes as good VA has been said to cause a “ceiling effect” as described by Ciulla et al. after recording worse outcomes with better VAs [21]. Both RCTs [5] and RWS [22, 23] have identified baseline VA as a determinant of the final best corrected visual acuity (BCVA).
Clinical Monitoring, Utilization of Anti-VEGF
Electronic medical records and charts have revealed that patients with DMO in real-world settings receive fewer injections and undergo less clinical monitoring thereby achieving outcomes inferior to that recorded in landmark RCTs [21, 22, 24]. For instance, in the retrospective analysis by Ciulla et al. of 28,658 patients in clinical practice, 6.3, 6.3 and 6.7 injections of aflibercept, bevacizumab and ranibizumab respectively were given in year 1 compared to 9.2, 9.7 and 9.4 respectively in the Protocol T study after 1 year [5, 21]. This may account for better mean VA improvements in the Protocol T study (about 2–4 times) compared with that recorded in the study by Ciulla et al. despite worse baseline VA in the latter.
The hypothesis that undertreatment may be associated with poor VA outcomes was also confirmed in the LUMINOUS study where participants with at least 5 injections in 1 year had a 6.4 greater letter increment than those with 4 injections or fewer [17]. Regardless of the fact that less burdensome regimens are aimed at better patient compliance, undertreatment must be avoided to ensure treatment outcome is not compromised.
Efficacy Outcomes
As regards efficacy, differences in the changes in the BCVA versus the CST have been reported [20, 25]. CST may be normal in abnormal retinal function (with poor VA) or the reverse may occur with good VA due to a maintained ellipsoid zone integrity. The latter can be seen with presence of fluid in the subretinal and not the worse intraretinal cystoid form. Thus, BCVA change may be a more reliable prognostic marker in macular oedema [26] and will be emphasized more in this review.
Bevacizumab
Few studies have explored the efficacy of bevacizumab in real-life clinical practice. Choovuthayakorn et al., in a 3-year retrospective study, assessed the visual and anatomical outcomes of patients with CI-DMO treated with bevacizumab in a single centre in Thailand [27]. Visual acuity improvement and CST reduction at 12, 24 and 36 months are shown in Table 2. Although the 12-month VA gain in the BOLT study, which was carried out in the UK, was less than that seen in the Thai study, superior results were obtained at 24 months in the BOLT study [28, 29]. It was highlighted earlier that worse baseline VAs may produce better VA outcomes; indeed, better outcomes may have been reported at 12 months in the Choovuthayakorn et al. study compared to the BOLT study as a result of poorer mean baseline VA reported in the former.
Ranibizumab
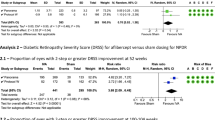
The LUMINOUS study was a prospective, global RWS which assessed the effectiveness and safety of ranibizumab 0.5 mg in 30,138 patients with neovascular age-related macular degeneration (AMD), DMO, myopic choroidal neovascularization and retinal vein occlusions (branch and central). In this review, results reported apply to the DMO cohort only [17] and the mean VA improvement at 1 year was + 3.5 letters, about 40% less than that obtained in the RESTORE study (+ 6.1 letters), which also administered ranibizumab 0.5 mg [20]. Furthermore, in the LUMINOUS study, better visual outcomes (+ 6.9 letters) were noted in patients with higher injection frequency of at least 5 injections compared to those who received less and had a mean VA gain of + 0.5 letters. Better VA gains were also noted in those who received loading injections and who had lower baseline VA [17].
At 36 months, better gains by almost threefold were observed in the RIDE (+ 11.4 letters) and the RISE studies (+ 11 letters) than that in the BOREAL study (+ 4.1 letters) which was a RWS carried out in France [30, 31]. In as much as the baseline VA was lower in the RISE and RIDE studies (Tables 1, 2), the challenge of poorer adherence in real life and therefore lower mean number of injections seen in RWS (undertreatment) may have contributed to this. The difference in mean number of injections at 36 months between the RWS and the RCTs was a stark one—BOREAL totalled 8.0 injections from baseline compared to RESTORE (14.2 injections), RIDE (30.4 injections) and RISE (28.5 injections).
Aflibercept
The APOLLON study was a prospective RWS which evaluated the efficacy of aflibercept in French clinical practice. Here, the mean BCVA gain at month 12 was about half that obtained in the VIVID and VISTA clinical trials (Tables 1, 2) [15, 19]. Results were also lower than reported in another RWS by Lukic et al.—the Moorfield’s RWS—where a gain of + 9.9 letters was obtained at a similar duration [32].
Similarly, the CST reduction was much higher in VIVID and VISTA studies than in the RWS despite lower baseline CSTs in the real-world APOLLON (439 µm) and Lukic et al. (421.8 µm) studies than in the VIVID and VISTA studies (479–518 µm). The better outcomes from the VIVID and VISTA studies are expected considering the better motivated patients and strict appointment schedules seen in RCTs. However, comparing both RWS by Lukic et al. and the APOLLON study, the better results noted in the former despite similar baseline VAs may be explained by the percentage of eyes which were treatment naïve vs eyes which have had previous treatment (which could indicate more treatment-resistant cases, hence, poorer outcomes). The Lukic et al. study was carried out among treatment-naïve patients while the 47.6% of participants in the APOLLON study had received prior therapy [15, 19, 32].
Comparison Studies
As the first to compare the efficacy of all three commercially available anti-VEGF medications in DMO, the DRCR.net Protocol T was a landmark trial in DMO therapy [5]. A total of 660 adults with CI-DMO with no anti-VEGF therapy in the preceding 12 months were randomized in a ratio 1:1:1 to 2.0 mg aflibercept, 1.25 mg bevacizumab or 0.3 mg ranibizumab at similar volumes (0.05 ml). Overall, aflibercept seemed to produce better and statistically significant letter gains than ranibizumab and bevacizumab after 1 year, while aflibercept’s superiority was only statistically significant for bevacizumab and not ranibizumab at 2 years [5, 33]. In as much as there is no RWS comparing all three medications as the Protocol T study, a few studies sort to compare the efficacy of at least two of the drugs in actual clinical practice.
Koc et al. carried out a RWS in Turkey where they compared outcomes of treatment with ranibizumab, bevacizumab and triamcinolone, and by year 2, mean VA improvement of ranibizumab was better than bevacizumab but not statistically significant (p = 0.306) [34]. This was similar to findings from the Protocol T study where pairwise comparison of ranibizumab-bevacizumab was p = 0.11. The drying effect of bevacizumab observed by Koc et al. was lower at 2 years than that recorded for ranibizumab (83.4 and 126.9 µm reduction respectively). This was likewise seen in the cohort with better VA (20/32–20/40) in the Protocol T study (68 µm and 125 µm respectively) and another study which compared the efficacy of Bevacizumab and Ranibizumab in patients with Diabetic Macular Edema (BRDME). The BRDME study was a non-inferiority trial which noted a more significant decrease in the central area thickness in the ranibizumab cohort (138.2 µm) than the bevacizumab cohort (64.2 µm) at 6 months [33, 35].
The RWS by Plaza-Ramos et al. retrospectively compared ranibizumab and aflibercept in a tertiary hospital [36]. They observed no statistically significant difference in the VA improvement in both groups after 4 months (p = 0.888) and after 1 year (p = 0.864). This contrasts with results noted in the Protocol T study where aflibercept produced overall better (and statistically significant) letter gains compared to ranibizumab at year 1. Some contributory factors to the results noted in the Plaza-Ramos et al. study may be that there were more treatment-naïve patients in the ranibizumab cohort compared to the aflibercept cohort and the patients with aflibercept started with better mean VA with the possibility of the ceiling effect in the outcome.
It may seem logical to attribute the superiority of aflibercept to its inhibition of PIGF, which is an “extra” compared to the other duo; however, the Protocol T study researchers felt the differences were not meaningful clinically because of the “small difference” in BCVA gain noted in year 2 [33]. Based on this question of superiority generated by the Protocol T study, more research under practical, real-life circumstances needs to be carried out to further clarify this issue.
Overall, as regards efficacy, another factor which may explain better outcomes in RCTs compared to RWS could be exclusion of some specific macula changes in RCTs such as the Protocol T, BOLT, VIVID and VISTA studies [5, 19, 28]. These changes, which include foveal ischemia, epiretinal membranes, hard exudates, may prevent desired structural and functional outcomes. Kulikov et al. reported a lesser mean change in the CST of eyes with vitreoretinal interface (VRI) abnormalities compared to eyes without these changes (53 µm vs 128 µm; p < 0.05) after 1 month of anti-VEGF therapy [37]. The VRI abnormalities listed in the participants include vitreomacular adhesion, vitreomacular traction and epiretinal membrane involving the macular centre. Similarly, foveal hard exudates have also been proved to account for the reduced visual acuity following 6 months anti-VEGF therapy in the study by Ota et al. In that study, pre-treatment hyperreflective dots were associated with follow-up findings of subfoveal hard exudates (p < 0.0001) [38]. These eyes were, in turn, noted to have poorer functional outcomes.
Safety
RWS have demonstrated similar ocular and systemic adverse events such as seen in RCTs with no new safety concerns.
As seen in RCTs, common ocular adverse effects seen in RWS also demonstrated elevated intraocular pressure (IOP), ocular pain, subconjunctival haemorrhage, cataracts, vitreous haemorrhage, macular and retinal oedema. Endophthalmitis is a complication of concern in anti-VEGF therapy because of the invasive and recurrent nature of treatment. However, some relief is gotten from evidence of its low or no incidence in both RCTs [20, 30] and RWS [36, 39]. Given this low rate, the use of antibiotics, peri- or post-injection is left to the discretion of the ophthalmologist. Additionally, as bevacizumab comes in 4-ml vials, vial sharing via repackaging into single-use syringes is usually required prior to injection and this has been linked to cluster endophthalmitis in different climes [40, 41]. This is of paramount importance in low- and lower-middle-income countries where bevacizumab is used more frequently owing to its lower cost.
As seen in various RCTs, systemic adverse events (SAEs) like cardiovascular accidents, systemic hypertension, myocardial infarction and deaths have been associated with anti-VEGF use in DMO in real life [17, 31].
Barriers to Treatment Success in the Real World
Patient-Associated Factors
Patients with DMO have been noted to have a higher rate of non-adherence [42] or appointment cancellation [43] compared to patients with neovascular AMD. Ehlken et al., who defined non-adherence as unplanned gaps of over 56 days between treatments, noted patient-related causes as topping the list at 83.1% [42]. Also, high values of lost to follow-up (LTFU) cases have been recorded by different RWS—33% at 24 months [44] and 25% at 1 year [45]. These percentages could possibly be due to an increasing younger generation of patients with DMO with work commitments, multiple comorbidities in the older generation, lack of motivation, and attendance of other clinics associated with diabetes care.
Other factors associated with the patients and cited in an interview of patients with diabetes in Nigeria include discouragements from unmet vision expectations, lack of family support in the form of hospital escorts and anxiety [46] (Table 3). In congruence, over half (54%) of a European sample of retinal patients reported 48-h pre-injection anxiety in a study by Sivaprasad et al. [47]. Though the number of missed appointments was not a study outcome, physical effects of anxiety like insomnia and loss of concentration were reported.
Socio-Economic Factors
Cost has been identified as a major barrier to DMO therapy especially in low/lower-middle incomes countries [46, 48] where insurance is lacking and patients tend to pay out of pocket. For example, non-affordability was the reason for being LTFU in 41% of patients in an Indian survey of patients on anti-VEGF therapy. Though less than that of ranibizumab (56.7%), 43.3% of patients could still not afford the lower priced bevacizumab [48]. In another Indian survey by Pramanik et al., participants with DMO had to pay 20.951 times more for ranibizumab + laser therapy compared to bevacizumab + laser therapy [49]. When costs due to diagnostic tests like OCTs are included, things become more complicated. Indirect costs like that of transportation and feasibility of transportation were listed as a challenge in some studies [46, 48, 50]. For older age groups, lack of stamina may deter use of public transport which is particularly rigorous in some developing countries and private transportation will incur more costs.
In a high-income country, Weiss et al. via telephone survey reported that 8% of patients with DMO missed appointments as a result of insurance problems and the proportion of patients who missed one therapy because of delay in reimbursement from the German health insurance reduced from 52% to 31% after payment was made [50].
Health System Factors
Ehlken et al. also identified centre-associated issues as a challenge: poor or untimely arrangement of patient treatment appointments was responsible for treatment break-offs in over a quarter (26.9%) of patients with DMO [42]. Patients in the Nigerian survey stated previously experienced long clinic waiting time as a discouragement to want to attend subsequent appointments [46]. The authors suggested appointment staggering, i.e. scheduling and seeing patients in batches each day, as a modality to be employed to solve this.
Therapy-Related Factors
Bilateral injection was significantly (p < 0.001) related to adherence, i.e. two visits not missed or delayed, when compared to unilateral injections in a study carried out in Egypt [51]. Perhaps, it could be that patients are more dedicated knowing that both eyes are at risk of vision loss if non-adherent.
Condition-Related Factors
Among participants LTFU, i.e. absent for at least a year, in the study by Kelkar et al., 28.4% stopped because of “no improvement in vision” [48]. A direct proportionality was also established between adherence and VA improvement in a Jordanian study [52]. Gains in vision seem to spur patients on especially in regions where out-of-pocket payments are made as patients get value for their money.
Consensus Treatment Algorithm
A major gap in the real-life treatment of DMO is the variation in its management globally. There is an unmet need for a global consensus algorithm, which captures the updated best practice. Based on results of clinical trials and recent guidelines, a practical universal algorithm is recommended to foster uniformity (Fig. 1). This proposed consensus therapeutic pathway currently addresses an existing gap in DMO care and serves as a foundational template for later evidence-based improvements. Alongside upper-middle- and high-income countries, this algorithm may be applicable in low- and lower-middle-income countries where access to therapy is hindered by affordability.
Suggested consensus algorithm for treatment of centre-involving DMO in the real-world. Ensure optimal control of HBA1c (≤ 7.0%) and hypertension. *If cost constraints or low-resource setting, use bevacizumab or consider laser alone/in combination with anti-VEGF therapy. In high-resource setting, use aflibercept in 1st year or ranibizumab. ** Responder: > 10% CST reduction or > 5 letters gained. ***Persistent DMO: if CST is ≥ 250 µm at each visit for 24 weeks duration. ****Stop injections if VA or OCT stability (< 10% change) is maintained over two consecutive visits after maximum interval is reached. Then commence 8–12 weekly observation visits
To determine the line of therapy in CI-DMO which has been defined earlier, a cut-off VA of 6/9 was used in the consensus algorithm. The was due to some reasons. First, as established earlier, VA is more standardised than CST. Secondly, the DRCR.net Protocol V study showed that for eyes with CI-DMO and good VA (6/7.5 or better), observation resulted in insignificant differences in outcomes when compared with aflibercept or laser [57]. Thus, in good VA, patients can be observed and treatment considered when visual impairment is noticed.
In the same (Protocol V) study, criteria for intervention in this observed group was loss of 10 letters at any visit or loss of 5–9 letters at two consecutive visits. Monitoring was carried out every 8 weeks for two visits and subsequently every 16 weeks. This was compatible with a RWS which reported a median time to first treatment of 9.5 weeks in patients with CI-DMO and good VA [58]. Also, this follow-up regimen is not tedious in real life. It is important to note, however, that the Protocol V participants had a mean HbA1c of 7.6% [57]. Thus, good blood sugar control should be ensured in these patients as highlighted in the algorithm.
In CI-DMO, aflibercept may be used as first choice in year 1 if VA ≤ 6/12 based on results from the Protocol T study [2, 5]. This should be done after ruling out vitreomacular traction (by OCT) for which vitrectomy may be indicated with or without adjunctive anti-VEGF injections, corticosteroid or laser therapy [59]. Loading doses of anti-VEGF injections have been proven to produce better outcomes [17] but the question of how many initial monthly doses arises as inter-study variations exist. The Protocol T study used 6 loading doses whereas, the Protocol I study administered 4–6 initial doses [5, 60]. Ziemssen et al., in an evaluation of the VIVID and VISTA studies, noted continuous positive outcomes, both functional and anatomic, after injections four and five [61]. Thus, they suggested that a prolonged upload may be beneficial.
In as much as there is a wide variability in individual patient response to anti-VEGF therapy, a standard and unified definition of response is necessary. The Protocol I study defined response as CST reduction of less than 20% or a 5-letter improvement, whereas the Protocol T study chose a stricter CST reduction value of less than 10% [5, 60]. The latter criteria may not clearly distinguish responders from non-responders in real life and miss out a lot of potential responders. For instance, the BOLT study established the possibility of late response by classifying responders into early, intermediate and late responders [29]. Another complicating factor is the different retinal thickness measurements from the various commercially available OCT machines. Although the Protocol I definition was adopted in the algorithm in Fig. 1, further research using commonly available OCT machines can be carried out to achieve a univocal agreement. Evidence regarding when to evaluate for a response can be derived from the Protocol I study which assessed at 3 months. A post hoc analysis of Protocol I documented that the response at 12 weeks is a good indicator to prognosticate long-term outcome [62].
Laser treatment can be beneficial when faced with financial constraints as seen in low- or low- to middle-income countries. In these situations, rather than exposing patients who cannot afford anti-VEGF to the devastating outcomes of untreated DMO, laser can be used primarily. It can also be combined with anti-VEGF for patients who cannot continue to afford injections. With non-inferior structural and functional outcomes, some studies have proved combination therapy safe in DMO therapy with resultant fewer injections [63, 64].
Further application of laser in DMO can be seen in the Protocol T study where laser was given if DMO persisted after 24 weeks or if there was no improvement noted in the BCVA or CST from the last two consecutive injections given. Persistence was defined as CST of at least 250 µm at each visit over the first 24 weeks of injection [5, 65].
Implications for Low- and Lower-Middle-Income Countries: Research and Clinical Practice
Sparse evidence exists from low- and lower-middle-income countries on the reality of DMO clinical practice. As with epidemiological studies on DMO, data on the efficacy of the different treatment modalities in these environments is not available. To inform treatment choices, studies on what treatment patterns will work based on the peculiarities of these regions are also needed. RW outcomes have indicated that more pragmatic efforts are needed especially in these settings, where many barriers to therapeutic success exist.
Furthermore, national diabetic retinopathy or maculopathy database registries are essential in low- to lower-middle-income countries to identify unmet therapeutic targets in different geographical locations within each country and, as such, efforts can be made to improve quality of care in deficient regions. They also provide epidemiological data and aid in healthcare policy making. The lack of electronic medical records in some countries is a major barrier to development of such registries.
Long-term robust, observational research is also required to determine safety of the chronic use of anti-VEGF medications in DMO. Also, as treatment costs are borne by individuals in low- and lower-middle-income countries, research is needed to ascertain the affordability of the different medications, the alternatives and other cost-effective options such as biosimilars.
Suboptimal results from RWS have also called for the use of better treatment regimens, newer long-lasting classes of drugs, sustained less invasive drug-delivery systems, and use of artificial intelligence algorithms to classify treatment burdens to strengthen real-life outcomes. The concern, however, is the universal availability of these interventions, which already are in use or in the horizon, such that low- and lower-middle-income countries are not left behind.
Conclusion
Real-life clinical settings are faced with a lot of hindrances such that achieving efficacy outcomes as documented from the use of anti-VEGF in DMO in landmark RCTs has been a daunting task. The challenges faced are greater in resource-poor settings and thus, there is a need for more evidence which will facilitate prioritization of DMO/DR care from national levels in these regions. Aside cost, another major impediment, amongst others, is the lack of an evidence-based consensus treatment algorithm and this has been developed in this review.
The desired end is that while complementing each other, in an RCT and RWS manner (rather than an RCT vs RWS approach), barriers in DMO management are surmounted and better outcomes are obtained thereby reducing blindness from this sight-threatening disease.
References
Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157: 107843.
Schmidt-Erfurth U, Garcia-Arumi J, Bandello F, et al. Guidelines for the management of diabetic macular edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica. 2017;237:185–222.
Gonder JR, Walker VM, Barbeau M, et al. Costs and quality of life in diabetic macular edema: Canadian Burden of Diabetic Macular Edema Observational Study (C-REALITY). J Ophthalmol. 2014;939315:1–9.
Wong TY, Sun J, Kawasaki R, et al. Guidelines on diabetic eye care: the International Council of Ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125:1608–22.
Diabetic Retinopathy Clinical Research Network, Wells JA, Glassman AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372(3):1193–203.
National Institute for Health and Care Excellence. Ranibizumab for treating diabetic macular oedema. Technology appraisal guidance. 2013. https://www.nice.org.uk/guidance/ta274. Accessed 28 Oct 2022.
Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–64.
Teo ZL, Tham YC, Yan Yu MC, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021;128(11):1580–91.
Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat Rev Endocrinol. 2011;8(4):228–36.
Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin epidemiologic study of diabetic 548 retinopathy. XV. The long-term incidence of macular edema. Ophthalmology. 1995;102(1):7–16.
Presta LG, Chen H, O’Connor SJ, et al. Humanization of an anti-vascular endothelial growth factor monoclonal antibody for the therapy of solid tumors and other disorders. Cancer Res. 1997;57:4593–9.
Lowe J, Araujo J, Yang J, et al. Ranibizumab inhibits multiple forms of biologically active vascular endothelial growth factor in vitro and in vivo. Exp Eye Res. 2007;85(4):425–30.
Papadopoulos N, Martin J, Ruan Q, et al. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF Trap, ranibizumab and bevacizumab. Angiogenesis. 2012;15(2):171–85.
Massin P, Creuzot-Garcher C, Kodjikian L, et al. Real-world outcomes with ranibizumab 0.5 mg in patients with visual impairment due to diabetic macular edema: 12-month results from the 36-month boreal-dme study. Ophthalmic Res. 2019;62(2):101–10.
Korobelnik JF, Daien V, Faure C, et al. Real-world outcomes following 12 months of intravitreal aflibercept monotherapy in patients with diabetic macular edema in France: results from the APOLLON study. Graefes Arch Clin Exp Ophthalmol. 2020;258(3):521–8.
Ziemssen F, Wachtlin J, Kuehlewein L, et al. Intravitreal ranibizumab therapy for diabetic macular edema in routine practice: two-year real-life data from a non-interventional, multicenter study in Germany. Diabetes Ther. 2018;9(6):2271–89.
Mitchell P, Sheidow TG, Farah ME, et al. Effectiveness and safety of ranibizumab 0.5 mg in treatment-naive patients with diabetic macular edema: results from the real-world global LUMINOUS study. PLoS ONE. 2020;15(6):e0233595.
Nguyen QD, Brown DM, Marcus DM, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789–801.
Korobelnik JF, Do DV, Schmidt-Erfurth U, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121(11):2247–54.
Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118(4):615–25.
Ciulla TA, Pollack JS, Williams DF. Visual acuity outcomes and anti-VEGF therapy intensity in diabetic macular oedema: a real-world analysis of 28 658 patient eyes. Br J Ophthalmol. 2021;105(2):216–21.
Holekamp NM, Campbell J, Almony A, et al. Vision outcomes following anti-vascular endothelial growth factor treatment of diabetic macular edema in clinical practice. Am J Ophthalmol. 2018;191:83–91.
Busch C, Fraser-Bell S, Zur D, et al. Real-world outcomes of observation and treatment in diabetic macular edema with very good visual acuity: the OBTAIN study. Acta Diabetol. 2019;56:777–84.
Dugel PU, Layton A, Varma R. Diabetic macular edema diagnosis and treatment in the real world: an analysis of medicare claims data (2008 to 2010). Ophthalmic Surg Lasers Imaging Retina. 2016;47(3):258–67.
Soheilian M, Garfami KH, Ramezani A, Yaseri M, Peyman GA. Two-year results of a randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus laser in diabetic macular edema. Retina. 2012;32(2):314–21.
Diabetic Retinopathy Clinical Research Network, Browning DJ, Glassman AR, et al. Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007;114(3):525–36.
Choovuthayakorn J, Phinyo P, Tantraworasin A, et al. Intravitreal anti-vascular endothelial growth factor therapy for diabetic macular edema in clinical practice of single center: three-year outcomes. Ophthalmic Res. 2021;64(3):483–93.
Michaelides M, Kaines A, Hamilton RD, et al. A prospective randomized trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular edema (BOLT study) 12-month data: report 2. Ophthalmology. 2010;117(6):1078–86.
Rajendram R, Fraser-Bell S, Kaines A, et al. A 2-year prospective randomized controlled trial of intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema: 24-month data: report 3. Arch Ophthalmol. 2012;130(8):972–9.
Brown DM, Nguyen QD, Marcus DM, et al. Long-term outcomes of ranibizumab therapy for diabetic macular edema: the 36-month results from two phase III trials: RISE and RIDE. Ophthalmology. 2013;120(10):2013–22.
Massin P, Creuzot-Garcher C, Kodjikian L, et al. Real-world outcomes after 36 months treatment with ranibizumab 0.5 mg in patients with visual impairment due to diabetic macular edema (BOREAL-DME). Ophthalmic Res. 2021;64(4):577–86.
Lukic M, Williams G, Shalchi Z, et al. Intravitreal aflibercept for diabetic macular oedema in real-world: 36-month visual acuity and anatomical outcomes. Eur J Ophthalmol. 2021;31(3):1201–7.
Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123(6):1351–9.
Koc I, Kadaylfcllar S, Eldem B. Real-world results of intravitreal ranibizumab, bevacizumab, or triamcinolone for diabetic macular edema. Ophthalmologica. 2018;239:85–93.
Vader MJC, Schauwvlieghe ASME, Verbraak FD, et al. Comparing the efficacy of bevacizumab and ranibizumab in patients with diabetic macular edema (BRDME): the BRDME study, a randomized trial. Ophthalmol Retina. 2020;4:777–88.
Plaza-Ramos P, Borque E, Garcia-Layana A. Evaluation of ranibizumab and aflibercept for the treatment of diabetic macular edema in daily clinical practice. PLoS ONE. 2019;14(10): e0223793.
Kulikov AN, Sosnovskii SV, Berezin RD, Maltsev DS, Oskanov DH, Gribanov NA. Vitreoretinal interface abnormalities in diabetic macular edema and effectiveness of anti-VEGF therapy: an optical coherence tomography study. Clin Ophthalmol. 2017;11:1995–2002.
Ota M, Nishijima K, Sakamoto A, et al. Optical coherence tomographic evaluation of foveal hard exudates in patients with diabetic maculopathy accompanying macular detachment. Ophthalmology. 2010;117(10):1996–2002.
Jain P, Sheth J, Anantharaman G, Gopalakrishnan M. Real-world evidence of safety profile of intravitreal bevacizumab (Avastin) in an Indian scenario. Indian J Ophthalmol. 2017;65:596–602.
Khan P, Khan L, Mondal P. Cluster endophthalmitis following multiple intravitreal bevacizumab injections from a single use vial. Indian J Ophthalmol. 2016;64:694–6.
Edison LS, Dishman HO, Tobin-D’Angelo MJ, Allen CR, Guh AY, Drenzek CL. Endophthalmitis outbreak associated with repackaged bevacizumab. Emerg Infect Dis. 2015;21(1):171–3.
Ehlken C, Helms M, Bohringer D, Agostini HT, Stahl A. Association of treatment adherence with real-life VA outcomes in AMD, DME, and BRVO patients. Clin Ophthalmol. 2018;12:13–20.
Jansen ME, Krambeer CJ, Kermany DS, et al. Appointment compliance in patients with diabetic macular edema and exudative macular degeneration. Ophthalmic Surg Lasers Imaging Retina. 2018;49(3):186–90.
Kodjikian L, Lecleire-Collet A, Dot C, et al. ETOILE: real-world evidence of 24 months of ranibizumab 0.5 mg in patients with visual impairment due to diabetic macular edema. Clin Ophthalmol. 2021;15:2307–15.
Best AL, Fajnkuchen F, Nghiem-Buffet S, et al. Treatment efficacy and compliance in patients with diabetic macular edema treated with ranibizumab in a real-life setting. J Ophthalmol. 2018;2018:4610129.
Ibrahim OA, Foster A, Oluleye TS. Barriers to an effective diabetic retinopathy service in Ibadan, Nigeria (sub-Saharan Africa)—a pilot qualitative study. Ann Ib Postgrad Med. 2015;13:36–43.
Sivaprasad S, Oyetunde S. Impact of injection therapy on retinal patients with diabetic macular edema or retinal vein occlusion. Clin Ophthalmol. 2016;10:939–46.
Kelkar A, Webers C, Shetty R, et al. Factors affecting compliance to intravitreal anti-vascular endothelial growth factor therapy in Indian patients with retinal vein occlusion, age-related macular degeneration, and diabetic macular edema. Indian J Ophthalmol. 2020;68:2143–7.
Pramanik S, Mondal LK, Paine SK, et al. Efficacy and cost-effectiveness of anti-VEGF for treating diabetic retinopathy in the Indian population. Clin Ophthalmol. 2021;15:3341–50.
Weiss M, Sim DA, Herold T, et al. Compliance and adherence of patients with diabetic macular edema to intravitreal anti-vascular endothelial growth factor therapy in daily practice. Retina. 2018;38:2293–300.
Habib AE, Abdel-Kader AA, Eissa IM, Awadein A. Adherence to intravitreal anti-vascular endothelial growth factor (anti-VEGF) drugs in diabetic macular edema in an Egyptian population: a health belief model. Curr Eye Res. 2019;44(3):303–10.
Abu-Yaghi NE, Abed AM, Khlaifat DF, et al. Factors affecting compliance to anti-vascular endothelial growth factor treatment of diabetic macular edema in a cohort of Jordanian patients. Clin Ophthalmol. 2020;14:921–9.
Burgess PI, Msukwa G, Beare NA. Diabetic retinopathy in sub-Saharan Africa: meeting the challenges of an emerging epidemic. BMC Med. 2013;11(1):157.
Resnikoff S, Lansingh VC, Washburn L, et al. Estimated number of ophthalmologists worldwide (International Council of Ophthalmology update): will we meet the needs? Br J Ophthalmol. 2020;104(4):588–92.
Silpa-Archa S, Limwattanayingyong J, Tadarati M, Amphornphruet A, Ruamviboonsuk P. Capacity building in screening and treatment of diabetic retinopathy in Asia-Pacific region. Indian J Ophthalmol. 2021;69:2959–67.
Sivaprasad S, Conroy D, Das T. Bridging the valley of death between research and implementing a systematic diabetic retinopathy screening program in low- and medium-income countries. Indian J Ophthalmol. 2021;69:3068–71.
Baker CW, Glassman AR, Beaulieu WT, et al. Effect of initial management with aflibercept vs laser photocoagulation vs observation on vision loss among patients with diabetic macular edema involving the center of the macula and good visual acuity: a randomized clinical trial. JAMA. 2019;321(19):1880–94.
Luu KY, Akhter MM, Durbin-Johnson BP, et al. Real-world management and long-term outcomes of diabetic macular oedema with good visual acuity. Eye. 2020;34:1108–15.
Diabetic Retinopathy Clinical Research Network, Haller JA, Qin H, Apte RS. Vitrectomy outcomes in eyes with diabetic macular edema and vitreomacular traction. Ophthalmology. 2010;117:1087–93.
Diabetic Retinopathy Clinical Research Network, Elman MJ, Aiello LP, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(6):1064–77.
Ziemssen F, Schlottman PG, Lim JI, Agostini H, Lang GE, Bandello F. Initiation of intravitreal aflibercept injection treatment in patients with diabetic macular edema: a review of VIVID-DME and VISTA-DME data. Int J Retina Vitreous. 2016;2(1):16.
Dugel PU, Campbell JH, Kiss S, et al. Association between early anatomic response to anti-vascular endothelial growth factor therapy and long-term outcome in diabetic macular edema: an independent analysis of Protocol I study data. Retina. 2019;39(1):88–97.
Altınel MG, Acikalin B, Alis MG, et al. Comparison of the efficacy and safety of anti-VEGF monotherapy versus anti-VEGF therapy combined with subthreshold micropulse laser therapy for diabetic macular edema. Lasers Med Sci. 2021;36(7):1545–53.
Kanar HS, Arsan A, Altun A, et al. Can subthreshold micropulse yellow laser treatment change the antivascular endothelial growth factor algorithm in diabetic macular edema? A randomized clinical trial. Indian J Ophthalmol. 2020;68:145–51.
Bressler NM, Beaulieu WT, Glassman AR, et al. Persistent macular thickening following intravitreous aflibercept, bevacizumab, or ranibizumab for central-involved diabetic macular edema with vision impairment: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2018;136(3):257–69.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization and idea: Olapeju A. Sam-Oyerinde and Praveen J. Patel; Literature search: Olapeju A. Sam-Oyerinde; Writing-original draft preparation: Olapeju A. Sam-Oyerinde; Writing—review and editing: Olapeju A. Sam-Oyerinde and Praveen J. Patel; Supervision: Praveen J. Patel.
Disclosures
Praveen J. Patel works in the advisory board for Bayer UK, Novartis UK and Roche UK. Olapeju A. Sam-Oyerinde has no conflict of interest.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors. Ethical approval was not required for this study.
Prior Presentation
This manuscript is part of a dissertation submitted to the Institute of Ophthalmology, University College London in part fulfilment of the award of MSc Ophthalmology, October 2021.
Data Availability
Data sharing is not applicable to this article as no data sets were generated or analysed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sam-Oyerinde, O.A., Patel, P.J. Real-World Outcomes of Anti-VEGF Therapy in Diabetic Macular Oedema: Barriers to Treatment Success and Implications for Low/Lower-Middle-Income Countries. Ophthalmol Ther 12, 809–826 (2023). https://doi.org/10.1007/s40123-023-00672-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00672-6