Abstract
Introduction
Combined phacovitrectomy is gaining popularity due to efficiency and immediate visual improvement. However, concerns regarding erroneous intraocular lens (IOL) calculation in combination surgery are increasing, such as myopic shift owing to a thick macula and consequent underestimation of the axial length. Therefore, this study aimed to compare the refractive outcomes of combined phacovitrectomy in patients with highly myopic and non-highly myopic eyes.
Methods
A retrospective chart review was performed on patients who received combined phacoemulsification, intraocular lens implantation, and small gauge pars plana vitrectomy for cataract and macular pathologies in highly myopic and non-highly myopic eyes. Pre- and postoperative evaluation and ocular parameters were recorded, and analyses were performed using the Student’s t test and regression analysis.
Results
A total of 133 patients with macular pathologies, including myopic tractional maculopathy, macular hole, and epiretinal membrane, were enrolled. SRK II or SRK/T models were used for calculating IOL. The mean absolute error of refraction change was 0.65 D; 83.5% of patients were within 1-D error, 57.9% within 0.5-D error, and 35.3% within 0.25-D error, with SRK/T showing better precision and yielding more myopic shift. Furthermore, the predictive accuracy of SRK II or SRK/T was better in patients with non-highly myopic eyes. Moreover, Barrett’s universal II formula was not superior to SRK II or SRK/T in the prediction of postoperative refractive error (p = 0.48).
Conclusion
Refractive outcomes were satisfactory in the cohort of patients with highly myopic eyes. The combined implementation of SRK II and SRK/T was not inferior to Barrett’s universal II formula in predicting satisfactory refractive outcomes. Combination surgery can be an option for patients with both cataract and macular pathologies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? | |
Given the cataract status and the timing of macular surgery, combined phacovitrectomy is gaining popularity. | |
Concerns regarding erroneous intraocular lens calculation in combination surgery are increasing, with the occurrence of a myopic shift owing to a thicker macula and consequent underestimation of the axial length. | |
This study aimed to compare the refractive outcomes of combined phacovitrectomy in patients with highly myopic and non-highly myopic eyes. | |
What was learned from the study? | |
The mean absolute error of refraction change was 0.65 D; 83.5% of patients were within the 1-D error, 57.9% within the 0.5-D error, and 35.3% within the 0.25-D error. SRK/T showed better precision and yielded more myopic shift. The predictive accuracy of SRK II or SRK/T was better in patients with non-highly myopic eyes. | |
The combined implementation of SRK II and SRK/T was not inferior to Barrett’s universal II formula in predicting satisfactory refractive outcomes. | |
Combination surgery can be an option for patients with both cataract and macular pathologies. |
Introduction
Macular and cataract surgeries are both utilized to improve central vision. Common macular pathologies that require surgery include epiretinal membrane (ERM), macular hole (MH), vitreomacular traction (VMT), and myopic tractional maculopathy (MTM). These conditions, along with cataracts, are highly prevalent in the elderly [1,2,3,4,5,6]. While surgery for macular abnormalities includes vitrectomy and is sometimes associated with intraocular gas fill, the odds of cataract progression are much higher in these patients than in those who have not undergone surgery. In patients with both cataract and macular pathologies, there is a debate on whether to perform both surgeries in the same session or sequentially with an interval between the surgeries for adequate recovery.
In some facilities where the surgeon can operate on either cataracts or macular pathologies, without a co-surgeon to operate in the same session, the surgeries can only be performed separately. However, when the surgeon is competent enough to perform both surgeries simultaneously or has a trusted partner to work with, the decision to operate in one session is considered. The benefits of combined surgery are obvious: better intraoperative visualization, fewer surgical sessions, faster visual recovery, and, thus, higher patient satisfaction [7,8,9]. Moreover, macular functional recovery is not masked by postvitrectomy cataract formation [8]. However, the disadvantages of combined surgery include a longer operation time, increased inflammation, and the demand for a higher level of surgical skill [8, 9]. Erroneous intraocular lens (IOL) calculation in combined surgery is also a concern, with unexpected myopic shift in refractive outcome, owing to a thicker macula and consequent underestimation of the axial length [10].
As ERM and MH are more prevalent in aging populations, more patients are opting for combined surgery. Besides, cataracts and MTM are common in high myopes. With the rising trend of myopia, the prevalence of its complication has been steadily increasing [13]. In addition, surgeons with sophisticated skills and competence to perform both surgeries became more accessible [3, 4, 11, 12]. Noticing the gain in popularity of combined phacovitrectomy, we performed this retrospective study to evaluate the pre- and postoperative IOL and compare the refractive outcomes between patients with highly myopic and non-highly myopic eyes who underwent combination surgery. We sought to determine the correlation between the IOL value and the underlying ocular characteristics or pathologies.
Methods
From 2018 to 2020, 170 consecutive cases of combined phacoemulsification with posterior capsular intraocular lens insertion and pars plana vitrectomy were performed by a single surgeon owing to different vitreoretinal pathologies and vision-occluding cataracts. A retrospective chart review was performed on these patients 6 months after surgery. Other inclusion criteria had to be met: 1. Age over 21 years old. 2. Have not received previous vitrectomy. 3. Absence of corneal opacities that may interfere with IOL calculation. This study was approved by the institutional review board of National Taiwan University Hospital (NTUH), and all investigations were performed in accordance with the tenets of the Declaration of Helsinki and its later amendments.
Demographic data, keratometry, refractive error, ocular biometry data, and optical coherence tomography (OCT) results were documented prior to the surgery. Patients with axial length longer than 26 mm were stratified into the highly myopic group, while the others were stratified into the non-highly myopic group. Three months post operation, the refractive data and keratometry readings were recorded again. IOL measurements were carried out using SRK II and SRK/T, as per the clinical context, using the updated version of LS 700 (Lenstar, Haag-Streit). The new generation formula, Barrett’s universal II formula, was used to calculate IOL as a reference. OCT imaging was performed using either Avanti RTVue XR (Optovue) or CIRRUS™ HD-OCT 500 (Carl Zeiss).
Statistical analyses were performed with R (v4.0.3). The Student’s t test was used for comparisons between the two groups. A p value less than 0.05 was considered statistically significant. A multiple regression analysis was performed to evaluate the effect of certain factors on the final refractive outcome.
Results
A total of 133 patients were finally included, of whom 84 presented with ERM, 31 with MTM, 12 with MH, and the remaining 6 with VMT. There were 86 women and 47 men, and the mean age of the patients was 67.11 ± 7.46 years. The mean axial length was 26.44 ± 3.18 mm (Table 1). The mean absolute error of refraction change was 0.65 D, with 83.5% of patients in the range of 1-D error, 57.9% within the 0.5-D error, and 35.3% within the 0.25-D error.
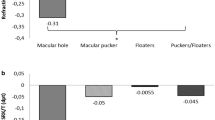
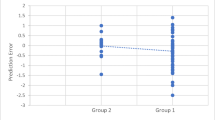
The SRK/T and SRK II models were used for calculating IOL, which accounted for 68.4% and 30.1%, respectively. The refractive outcomes were also calculated in the subgroup of patients with ERM and MTM. The percentage of end refraction within the targeted 1-D, 0.5-D, and 0.25-D errors for patients with ERM were 84.50%, 58.30%, and 36.90%, respectively, whereas the corresponding values of patients with MTM were 83.90%, 54.80%, and 25.80%, respectively (Fig. 1). All data points of final refractive error are shown in the scatter plot in Supplementary Material Fig. 1.
Barrett’s universal II formula was used to calculate IOL to compare the refractive outcome with that obtained with SRK II or SRK/T models; the mean absolute error obtained using Barrett’s universal II formula was 0.56 ± 0.82 D (range 0.2–6.14 D, median 0.35 D), which was similar to that obtained using SRK II or SRK/T models (mean 0.63 ± 0.81 D, range 0–6.21 D, median 0.42 D), showing no statistical significance (p = 0.48).
After patients were matched and then grouped on the basis of their axial lengths, the percentages of mean absolute error within 1 D, 0.5 D, and 0.25 D were calculated. The highest precision was observed in patients with axial lengths between 23 and 26 mm, although no statistical significance was observed (Fig. 2).
A regression analysis was performed to evaluate the factors associated with good IOL power prediction. We tested for age, sex, indication for surgery, corneal power, axial length, lens thickness, anterior chamber depth, and the model used for IOL calculation. Among all the aforementioned parameters, the model used for IOL calculation was the most accurate predictor for estimating the IOL power; SRK/T provided the most precise final refractive IOL prediction (p = 0.04). Regression analysis was also performed to detect the factors associated with the myopic shift observed in 53.4% of patients after undergoing combined surgery. The IOL power chosen for the surgery and the preoperative corneal power were the most significant predictors for myopic shift postoperatively. As the IOL power and corneal curvature increase, the final refractive outcome was expected to be on the myopic side (p < 0.01). Furthermore, the use of the SRK/T model was positively associated with the final myopic outcome (p = 0.02).
A subgroup analysis was performed in patients with ERM and MTM to elucidate the factors for the precise determination of the final refractive power. In patients with ERM, only SRK/T served as a positive predictor for a small refractive error (p < 0.01), whereas, in patients with MTM, no factor was found to be significantly associated with the final refractive outcome. However, if the refractive error was considered to be less than 0.5 D, the preoperative central retinal thickness (CRT) and anterior chamber depth (ACD) significantly affect the outcome. Although a thinner CRT predicts the final refractive outcome within the 0.5-D error, a shallow ACD inversely predicts the possibility of achieving an error within 0.5 D (p < 0.05).
Discussion
The benefits and drawbacks of combination surgery for cataract and vitreoretinal (VR) diseases have long been discussed. In situations with less accessibility or higher surgical expenses, simultaneous surgery is a more economical choice than sequential surgery, both in terms of time and money. Needless to say, a faster recovery time is also considered a significant benefit. Most patients recover from surgery within 6 months, with a stable corrected vision and near-normal foveal thickness [7, 14, 15]. However, the primary challenge faced in simultaneous surgery is the decreased accuracy in the final refractory outcome, mostly associated with primary VR pathologies [16]. For example, a few studies reported that, when the final refractive outcomes of patients receiving sequential and combined surgeries were compared, patients who received combined surgery and with risk factors, such as worse vision, greater central macular thickness, and shallow anterior chambers, were prone to inaccurate preoperative biometry [17].
We used SRK II and SRK/T models to calculate IOL in our cohort of patients; we noticed a significant difference in the final refractive outcomes, with SRK/T providing a more precise value. Being viewed as the third-generation formula, SRK/T is not only based on nonlinear terms of the theoretical formulas but also incorporates the empirical regression methodology for perfection. More ocular parameters, such as the corneal curvature and the anterior chamber depth, were included in the analysis [18]. Additionally, one of the most important benefits of using the SRK/T model and other third-generation formulas was their accuracy in eyes with axial lengths longer than 26.0 mm. Our cohort consisted of several patients with highly myopic eyes, and the simplified SRK II might not have been adequate to determine the optimal IOL power. However, despite resulting in a small absolute refractive error, the SRK/T formula was associated with a higher rate of myopic shift. With the newly developed Barrett’s universal II formula, the estimated value was similar to that obtained using SRK/T in this study, which does not affect the choice of the IOL calculation formula in the future.
Considering the myopic shift in the final refractory outcome, it was intuitive that as the IOL power and corneal curvature increase, the chance of the myopic shift increases. Previous studies reported that the erroneous IOL calculation results from an underestimation of the axial length due to a thicker macula and the effect of combined vitrectomy [10, 19, 20]. It was postulated that associated ERM masked the real plane of the final image, thus resulting in inaccurate IOL estimation prior to the operation. Furthermore, the retinal pathology requiring a tamponade agent was found to be more likely to exert a myopic outcome. The authors propose a mechanism of myopic shift depending on the change in the effective lens position [19].
Similarly, in the subgroup analysis, we found a significant relationship between a thick CRT and less precise refractive outcomes in patients with MTM. This finding corresponds to that observed in a previous study, confirming that the myopic shift results from the underestimation of the axial length due to a thicker macula [10]. However, this effect was not observed in patients with ERM in our study. This could be due to a thicker CRT and larger standard deviation in patients with MTM than in those with ERM (440.97 ± 132.31 µm and 418.85 ± 106.40 µm, respectively). In addition, most patients who were operated on for MTM received a gas tamponade and were placed in a prone position after the combination surgery. The result corresponds to the previously described changes in the effective lens position, which yielded a more myopic result in patients with highly myopic versus non-highly myopic eyes.
There are some limitations in this study. As this was a retrospective study and the follow-up schedule was not as strict as a prospective trial, some valuable secondary endpoints are missing and could not be discussed. In addition, we did not enroll the group of patients who received consecutive surgeries, according to the routine management in the clinic; instead, we only focused on the refractive outcome of patients with highly myopic and non-highly myopic eyes who underwent combination surgery. Future studies comparing both sequential and combined surgeries in this group of patients are warranted.
Conclusion
Combined phacovitrectomy is gaining popularity. Refractive outcomes were satisfactory in the cohort of patients with both highly myopic and non-highly myopic eyes. Although the predictive accuracy of SRK II or SRK/T was better in patients with non-highly myopic eyes as compared with highly myopic eyes, the combined implementation of SRK II and SRK/T was not inferior to Barrett’s universal II formula in predicting satisfactory refractive outcomes. In conclusion, combination surgery can be an option for patients with both cataract and macular pathologies.
References
Mitchell P, Smith W, Chey T, Wang JJ, Chang A. Prevalence and associations of epiretinal membranes. The Blue Mountains Eye Study, Australia. Ophthalmology. 1997;104:1033–40.
Ng CH, Cheung N, Wang JJ, et al. Prevalence and risk factors for epiretinal membranes in a multi-ethnic United States population. Ophthalmology. 2011;118:694–9.
Xiao W, Chen X, Yan W, Zhu Z, He M. Prevalence and risk factors of epiretinal membranes: a systematic review and meta-analysis of population-based studies. BMJ Open. 2017;7: e014644.
McCannel CA, Ensminger JL, Diehl NN, Hodge DN. Population-based incidence of macular holes. Ophthalmology. 2009;116:1366–9.
Mehdizadeh M, Jamshidian M, Nowroozzadeh MH. Macular hole epidemiology. Ophthalmology. 2010;117:2442–3.
Kook D, Haritoglou C, Kampik A, Kohnen T. Combined cataract and vitreoretinal surgery. Klin Monbl Augenheilkd. 2010;227:630–7. (German)
Dugas B, Ouled-Moussa R, Lafontaine PO, et al. Idiopathic epiretinal macular membrane and cataract extraction: combined versus consecutive surgery. Am J Ophthalmol. 2010;149:302–6.
Senn P, Schipper I, Perren B. Combined pars plana vitrectomy, phacoemulsification, and intraocular lens implantation in the capsular bag: a comparison to vitrectomy and subsequent cataract surgery as a two-step procedure. Ophthalmic Surg Lasers. 1995;26:420–8.
Jalil A, Steeples L, Subramani S, Bindra MS, Dhawahir-Scala F, Patton N. Microincision cataract surgery combined with vitrectomy: a case series. Eye (Lond). 2014;28:386–9.
Kovács I, Ferencz M, Nemes J, Somfai G, Salacz G, Récsán Z. Intraocular lens power calculation for combined cataract surgery, vitrectomy and peeling of epiretinal membranes for macular oedema. Acta Ophthalmol Scand. 2007;85:88–91.
Klein R, Klein BE, Wang Q, Moss SE. The epidemiology of epiretinal membranes. Trans Am Ophthalmol Soc. 1994;92:403–30.
Cho SC, Park SJ, Byun SJ, Woo SJ, Park KH. Five-year nationwide incidence of macular hole requiring surgery in Korea. Br J Ophthalmol. 2019;103:1619–23.
Wong YL, Sabanayagam C, Ding Y, et al. Prevalence, risk factors, and impact of myopic macular degeneration on visual impairment and functioning among adults in Singapore. Invest Ophthalmol Vis Sci. 2018;59:4603–13.
Kauffmann Y, Ramel JC, Isaico R, De Lazzer A, Bron AM, Creuzot-Garcher C. Long-term anatomical and functional outcomes after combined cataract and idiopathic epiretinal membrane surgery. Ophthal Res. 2017;57:125–34.
Alexandrakis G, Chaudhry NA, Flynn HW Jr, Murray TG. Combined cataract surgery, intraocular lens insertion, and vitrectomy in eyes with idiopathic epiretinal membrane. Ophthalmic Surg Lasers. 1999;30:327–8.
Al-Habboubi HF, Al-Zamil W, Al-Habboubi AA, Khandekar R. Visual outcomes and refractive status after combined silicone oil removal/cataract surgery with intraocular lens implantation. J Ophthalmic Vis Res. 2018;13:17–22.
Tranos PG, Allan B, Balidis M, et al. Comparison of postoperative refractive outcome in eyes undergoing combined phacovitrectomy vs cataract surgery following vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2020;258:987–93.
Retzlaff JA, Sanders DR, Kraff MC. Development of the SRK/T intraocular lens implant power calculation formula. J Cataract Refract Surg. 1990;16:333–40.
Falkner-Radler CI, Benesch T, Binder S. Accuracy of preoperative biometry in vitrectomy combined with cataract surgery for patients with epiretinal membranes and macular holes: results of a prospective controlled clinical trial. J Cataract Refract Surg. 2008;34:1754–60.
Kim YK, Woo SJ, Hyon JY, et al. Refractive outcomes of combined phacovitrectomy and delayed cataract surgery in retinal detachment. Can J Ophthalmol. 2015;50:360–6.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Medical Writing
We would like to thank Editage (www.editage.com) for English language editing.
Author Contributions
Conceptualization: I-Hsin Ma, Tzyy-Chang Ho; Methodology: I-Hsin Ma; Shih-Wen Wang, Wei-Lun Huang, Yun Hsia, Kuo-Chi Hung, Chien-Jung Huang, Muh-Shy Chen, Tzyy-Chang Ho; Formal analysis and investigation: I-Hsin Ma, Tzyy-Chang Ho, Writing—original draft preparation: I-Hsin Ma; Writing—review and editing: I-Hsin Ma, Tzyy-Chang Ho; Supervision: Muh-Shy Chen, Tzyy-Chang Ho.
Prior Presentation
This study was presented at the Asia–Pacific Vitreoretinal Society (APVRS) annual meeting in Taipei, Taiwan, 18–20 November 2022.
Disclosures
I-Hsin Ma, Shih-Wen Wang, Wei-Lun Huang, Yun Hsia, Kuo-Chi Hung, Chien-Jung Huang, Muh-Shy Chen and Tzyy-Chang Ho declare that there are no conflicts of interest related to this article. None of the authors received any funding for this study.
Compliance with Ethics Guidelines
This study was approved by the institutional review board of National Taiwan University Hospital and all investigations were in accordance with the tenets of the Declaration of Helsinki and its later amendments. Waiver of informed consent was granted by the ethics committee.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ma, IH., Wang, SW., Huang, WL. et al. Comparison of Refractive Outcomes in Patients with Highly Myopic Versus Non-highly Myopic Eyes Undergoing Phacovitrectomy. Ophthalmol Ther 12, 1025–1032 (2023). https://doi.org/10.1007/s40123-023-00655-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00655-7