Abstract
Introduction
Severe viral keratitis with hypopyon and retrocorneal plaques is easily misdiagnosed as it mimics fungal or bacterial keratitis and is more likely to undergo emergency therapeutic penetrating keratoplasty (TPK) in the presence of active infection, resulting in poor outcomes. This case series offers some important insights for the management strategy of severe viral keratitis.
Methods
This retrospective case series involved five patients with unilateral severe infectious keratitis with hypopyon over 3 mm and retrocorneal endothelial plaques. Testing for corneal sensation, microscopy, culture, and anterior segment optical coherence tomography (ASOCT) were performed.
Results
At presentation, all five cases had visual acuity of counting fingers (CF) or worse, large centrally located ulcer with clean ulcer surface, hypopyon, and retrocorneal plaques with reduced corneal sensation. ASOCT demonstrated the presence of retrocorneal plaques with clear space between corneal endothelium and plaques. All cases received systemic and topical ganciclovir and topical steroids. Two patients received intravenous immunoglobulin (IVIG) weekly for 2 weeks. Complete resolution was achieved in all cases except one patient who underwent TPK because of diffuse anterior synechiae of the iris, with recurrence of infection after 10 days. The patients who received IVIG showed resolution earlier compared to the other patients.
Conclusions
Evaluation of characteristics of retrocorneal plaques by ASOCT and reduced corneal sensation are valuable aids in diagnosis of complicated viral keratitis. Conservative medical management may be a viable option even in severe cases. IVIG may have a role in speedy resolution of severe cases, but more research is needed to confirm this.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Severe viral keratitis with hypopyon and retrocorneal plaques is easily misdiagnosed as fungal or bacterial keratitis and is more likely to undergo emergency therapeutic penetrating keratoplasty (TPK) in the presence of active infection, resulting in poor outcomes. |
What was learned from the study? |
Evaluation of characteristics of retrocorneal plaques by anterior segment optical coherence tomography (ASOCT) and reduced corneal sensation can help in speedy diagnosis of complicated, atypical cases of viral keratitis, even when microbiological tests may be negative. |
Conservative but aggressive medical management may result in resolution of active keratitis, without the need for emergency surgical intervention, which is likely to have better visual outcomes with potential for successful optical keratoplasty at a later stage. |
Introduction
Infectious keratitis (IK) is an important cause of visual impairment and blindness worldwide, with an estimated incidence of 2.5–799 cases per 100,000 population/year [1, 2]. Recent data from the Asia Cornea Society Infectious Keratitis Study (ACSIKS) group demonstrated that the commonest etiology of infectious keratitis in China was viral keratitis, which accounted for 47.7% [3]. Herpes simplex virus (HSV) remains the most common cause of viral keratitis, followed less commonly by varicella zoster virus (VZV) and cytomegalovirus (CMV) [3].
Penetrating keratoplasty (PK) is typically performed in infectious keratitis for therapeutic reasons to remove the refractory corneal infection and provide tectonic support to the globe (therapeutic penetrating keratoplasty, TPK) or for optical reasons and visual rehabilitation as in cases of scarring after the resolution of inflammation (optical penetrating keratoplasty, OPK). Deep anterior lamellar keratoplasty (DALK) is a popular surgical alternative in less severe cases where there is no deep scarring or endothelial dysfunction [1, 4]. It has been widely recognized that the graft survival after TPK was worse than that after OPK. In the Singapore Corneal Transplant Study (SCTS), graft survival rates following tectonic and therapeutic penetrating keratoplasty were lower than optical graft survival rates (41.7%, 58.3%, and 72.0% at 3 years, respectively) [5]. However, emergency TPK is often performed in eyes with impending perforation or uncontrolled infection refractory to medical treatment, possibly as a result of inaccurate diagnosis [6, 7]. It is hence imperative to correctly diagnose and control the inflammation, increasing the possibility of receiving OPK or DALK.
The diagnosis of typical cases of infectious viral keratitis can easily be made according to its typical clinical manifestations. However, even for experienced ophthalmologists, the diagnosis of abnormal or complicated cases is often challenging. Retrocorneal plaques are considered typical of fungal keratitis and appear when the fungus destroys the endothelium and extends into the anterior chamber [7, 8]. In these cases, patients often need surgical intervention like TPK to remove the source of infection. However, retrocorneal endothelial plaques can also occasionally occur in viral keratitis when clusters of keratic precipitates, composed of inflammatory cells from the immune response, gather at the endothelial surface [9]. Viral keratitis with retrocorneal plaques and hypopyon is easily misdiagnosed as fungal or bacterial keratitis because of similar presenting signs, especially in severe cases. Also, the treatments for viral and fungal keratitis are completely different, as corticosteroids are necessary for treating stromal or endothelial immune reactions associated with viral keratitis.
To date, plenty of diagnostic techniques for viral keratitis have been used to achieve rapid and correct diagnosis [10, 11]. Although microbial culture has been the mainstay of diagnosis of infectious disease, tissue cultures are relatively insensitive in viruses and can be very slow [11]. In addition, cytology including smear and staining for multinucleated giant cells and lymphocytes is a quick and simple method but it has low sensitivity (40–57%) [12, 13]. Currently, molecular diagnosis by polymerase chain reaction (PCR) is the most widely used diagnostic tool for viral keratitis with high sensitivity and shortest time to detection, but it is limited by false-negative results because of small sample load obtained from diseased eyes sometimes [10, 14]. Sensitivity for newer techniques including the multiplex dot hybridization (MDH) assay and immunochromatographic assays (ICGA) is 93.3% and 84%, respectively, but these techniques are as yet less explored [15]. Initial misdiagnosis will misguide the treatment direction, leading to increased severity of the infection, and severe cases still have to receive emergency TPK in the inflammatory phase even without correct diagnosis. However, emergency PK in corneas with active viral infections have poorer prognosis compared to fungal and bacterial keratitis, and the complications and reoperations increase both risks and financial burden for patients [16, 17]. Thus, there is a crucial need to address the tactics of diagnosis and treatment in severe cases of viral keratitis which mimic bacterial and fungal keratitis. Our previous research revealed that mild viral keratitis with retrocorneal plaques can be successfully managed with antiviral drugs and topical steroids, without surgical intervention, but the efficacy of conservative treatment is uncertain in severe cases [18]. Herein, we report our experience of conservative management of patients with severe viral keratitis with hypopyon over 3 mm and retrocorneal endothelial plaques in a cornea and tertiary referral eye care center in northern China.
Methods
We retrospectively reviewed the clinical records of patients with unilateral infectious keratitis who were referred to the Peking University Third Hospital from July 2020 to November 2021. Patients with accompanying hypopyon over 3 mm, retrocorneal endothelial plaques, and negative culture result for bacteria and fungus were enrolled and diagnosed as suspected viral keratitis. Patients with etiological evidence of bacterial or fungal infection were excluded.
Approval was obtained from the ethics committee of Peking University Third Hospital. The research adhered to the Declaration of Helsinki and informed consent was obtained from all patients. All patients underwent complete ophthalmic examination and evaluation by a corneal specialist. Slit lamp photos, testing for corneal sensation, microscopy and culture from corneal scrapings, anterior segment optical coherence tomography (ASOCT), real-time polymerase chain reaction (PCR), and in vivo confocal microscopy (IVCM) were performed in all patients. During the antiviral treatment, to monitor side effects, all patients underwent routine blood tests and blood chemistry tests every 2 weeks.
Patient 1
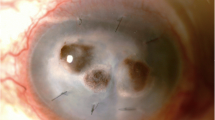
A 66-year-old woman presented with an history of vegetative trauma in her left eye (with a small corn leaf) while working in the field, 1 month back. There was no past medical or ophthalmological history before that. She was diagnosed with fungal keratitis at a local hospital and treated with local antifungal treatment. She did not respond to the treatment and presented to us with progressive loss of vision, corneal ulcer, and swollen eyelids. At presentation, her visual acuity (VA) was hand movements (HM) and her periocular skin had redness, erosion, and nonpitting edema. The corneal sensation in her left eye was markedly reduced. On slit lamp examination, there was a large stromal infiltrate with an overlying 7 × 8-mm epithelial defect, clear ulcer surface, an endothelial plaque underlying the area of active stromal infiltration, and a 4-mm hypopyon (Fig. 1a, b). ASOCT showed retrocorneal endothelial plaque with a clear boundary between the corneal endothelial surface and plaque (Fig. 2a) and IVCM showed the infiltration of inflammatory cells without fungal filaments (Fig. 4a). Corneal scraping was carried out and stains and culture were negative for bacteria and fungi. PCR on corneal scrapings was positive for Epstein–Barr virus (EBV). Treatment with topical ganciclovir (GCV) gel four times a day (7.5 mg: 5 g GCV ophthalmic gel, China Meheco Keyi Pharma Co., Ltd, Hubei, China), GCV 250 mg intravenously twice a day, and intravenous immunoglobulin (IVIG) 5 mg weekly for 2 weeks was commenced. Topical steroid ointment, once at evening (TobreDex, Alcon, Rijksweg, Belgium) was added 3 days after initiation of antiviral therapy. The patient significantly improved in 2 weeks (Figs. 1c, d, 2b) and reached resolution of epithelial defect, hypopyon, inflammatory precipitates of corneal posterior surface, and edema of periocular skin after 4 weeks of therapy (Figs. 1e, f, 2c, 4f, Fig. S1). There has been no recurrence observed for 10 months.
Slit lamp photograph with and without flourescein stain of patients 1–4. Patient 1: The large epithelial defect (a) and stromal infiltrate with 4-mm hypopyon (b) at initial visit. Decreased epithelial defect (c) and hypopyon (d) after 2 weeks of treatment. No epithelial defect (e) and hypopyon (f) with scarring left after 4 weeks of treatment. Patient 2: The large epithelial defect (g) and stromal infiltrate with 5-mm hypopyon (h) at initial visit. Decreased epithelial defect (i) and hypopyon (j) after 2 weeks of treatment. Small epithelial defect (k) and scarring left (l) after 3 weeks of treatment. Patient 3: The large epithelial defect (m) and stromal infiltrate with 3-mm hypopyon (n) at initial visit. Decreased epithelial defect (o) and hypopyon (p) after 2 weeks of treatment. No epithelial defect (q) and hypopyon (r) with scarring left after 6 weeks of treatment. Patient 4: The large epithelial defect (s) and stromal infiltrate with hypopyon full of anterior chamber (t) at initial visit. Decreased epithelial defect (u) and hypopyon (v) after 2 weeks of treatment. No epithelial defect (w) and hypopyon (x) with scarring left after 6 weeks of treatment
ASOCT of patients 1–4. Patient 1: Presence of retrocorneal endothelial plaques with a clear boundary at initial visit (a). Decreased inflammatory precipitates after 2 weeks of treatment (b). No inflammatory precipitates after 4 weeks of treatment (c). Patient 2: Presence of retrocorneal endothelial plaques with a clear boundary at initial visit (d). Decreased inflammatory precipitates after 2 weeks of treatment (e). No inflammatory precipitates after 3 weeks of treatment (f). Patient 3: Presence of retrocorneal endothelial plaques with a clear boundary at initial visit (g). Decreased inflammatory precipitates after 2 weeks of treatment (h). No inflammatory precipitates after 8 weeks of treatment (i). Patient 4: Presence of retrocorneal endothelial plaques with a clear boundary at initial visit (j). Decreased inflammatory precipitates after 2 weeks of treatment (k). No inflammatory precipitates after 6 weeks of treatment (l)
Patient 2
A 68-year-old man presented to us with redness and progressive worsening of vision in his left eye. There was no past medical or ophthalmological history before that. He gave a history of treatment with topical antibiotics and steroids for a presumptive diagnosis of bacterial keratitis and lack of response for the same, with worsening of symptoms and rapid deterioration of vision. At presentation, his VA was light perception (LP). Slit lamp examination showed a stromal ring infiltrate, full epithelial defect of the cornea, small endothelial plaque, and 4-mm hypopyon in the patient’s left eye (Fig. 1g, h). Cultures through corneal scraping were performed to rule out bacterial and fungal infection, and IVCM excluded the presence of fungal filaments (Fig. 4b). Since the PCR result on corneal scraping for viruses was negative, on the basis of the characteristics of clean ulcer surface, reduced corneal sensation, and ASOCT findings of a clear boundary between the corneal endothelial surface and plaque, the patient was given a trial of antiviral therapy containing topical GCV eye gel four times a day, GCV 250 mg intravenously twice a day, topical steroid ointment once per evening, IVIG 5 mg weekly for 2 weeks and intravitreal injection of GCV 3 mg once. The patient showed a significant improvement in corneal infiltrate size, epithelial defect, and resolution of hypopyon within 3 weeks of treatment (Figs. 1i–l, 4g). ASOCT showed no inflammatory precipitates on the posterior surface of cornea, supporting the diagnosis of viral keratitis (Fig. 2e, f). No recurrence has been observed for 1 year.
Patient 3
A 60-year-old man, without past medical or ophthalmological history, presented to us with a 2-month history of progressive vision loss and pain in his left eye. A slit lamp examination revealed temporal circular stromal infiltrate along with epithelial defect of the same size, underlying endothelial plaques temporally, and a 3-mm hypopyon in his left eye (Fig. 1m, n). The patient was initially diagnosed with severe bacterial keratitis and antibacterial treatment was started. The patient was unresponsive to the treatment and ASOCT performed subsequently showed a clear boundary between the corneal endothelial surface and endothelial plaques (Fig. 2g). IVCM ruled out fungal infection (Fig. 4c). Corneal sensation in the left eye was markedly reduced. Although PCR tests through corneal scraping were negative for viruses, a diagnosis of viral keratitis was suspected and therapeutic trial with the antiviral drugs was started, containing topical and intravenous GCV and topical steroids. In addition, the patient received intravitreal injection of GCV 3 mg in his left eye on the 8th and 13th day of hospitalization. Although PCR was negative for virus, a marked improvement was observed in 2 weeks (Figs. 1o, p, 2h), and resolution of lesions was observed in 6 weeks, thereafter, proving our diagnosis correct (Figs. 1q, r, 2i, 4h). There has been no recurrence observed for 18 months.
Patient 4
A 50-year-old healthy woman presented to the local hospital with a 2-month history of blurred vision of her right eye, with no response to antifungal treatment given by a local doctor. She denied any past medical or ophthalmological history. At presentation, her VA of the right eye was HM. Slit lamp examination demonstrated ring-shaped epithelial defect and full-thickness corneal infiltration with hypopyon filling half of the anterior chamber (Fig. 1s, t). Corneal scraping was negative for bacteria and fungi. Meanwhile, the result of ICVM indicated that there were no fungal filaments (Fig. 4d). PCR on corneal scrapings was positive for VZV. Corneal sensation was markedly reduced. ASOCT showed the presence of retrocorneal plaques and a clear boundary between the plaques and the cornea (Fig. 2j). Therefore, with a clinical suspicion of viral keratitis, we added antiviral drugs, topical steroids, and intravitreal injection of GCV 3 mg at 2nd and 9th day of hospitalization. After 2 weeks of treatment, marked progress was observed in epithelial defect, hypopyon, and inflammatory precipitates (Figs. 1u, v, 2k). After 6 weeks of treatment, the lesions started to resolve with scarring of the lesion subsequently (Figs. 1w, x, 2l, 4i). There has been no recurrence observed for 10 months.
Patient 5
A 42-year-old man, with poorly controlled type 2 diabetes mellitus and no past ophthalmological history, presented with progressive vision loss and foreign body sensation in his left eye that started 2 months ago. He was treated unsuccessfully with antifungal and antibacterial treatment outside. At presentation, his VA of left eye was finger counting (CF) and IOP was within normal range. Slit lamp examination revealed diffuse stromal infiltration with overlying epithelial defects and hypopyon affecting more than half of the anterior chamber (Fig. 3a). Corneal sensation was reduced in the left eye. ASOCT showed endothelial plaques and a clear boundary between the corneal endothelial surface and plaque (Fig. 3e). Microscopy and culture were negative for bacteria and fungi, and corresponding IVCM helped rule out the presence of fungal filaments (Fig. 4e). PCR on corneal scraping was positive for HSV-I. The patient was started on topical and systemic GCV, topical steroids, and intravitreal injection of GCV on 8th and 16th day of hospitalization. After 3 weeks of treatment, he partially improved (Figs. 3b, 4j) but ASOCT revealed diffuse anterior synechiae of the iris in his left eye (Fig. 3f), and he underwent TPK during the acute stage. However, there was recurrence on the inferotemporal side 10 days after TPK (Fig. 3c, g) and the graft presented with irreversible loss of clarity and edema 1 month after TPK (Fig. 3d, h).
Slit lamp photograph and ASOCT of patient 5. Large epithelial defect, deep stromal infiltrate with hypopyon over 8 mm at initial visit (a). Partially improved after 3 weeks of medical therapy (b). Recurrence observed on the inferotemporal side 10 days after TPK (c). Irreversible loss of clarity and edema of the graft 1 month after TPK (d). ASOCT at initial visit showing presence of retrocorneal endothelial plaques and corneal infiltrate (e). ASOCT after 3 weeks of medical therapy showing decreased inflammatory precipitates and diffuse anterior synechiae of the iris (f). ASOCT showing edema of the graft 10 days after TPK (g) and 1 month after TPK (h)
IVCM in the endothelial layer of patients 1–5. IVCM showing the presence of many hyper-reflective inflammatory cells in the endothelial layer without fungal filaments at initial visit of patient 1 (a), patient 2 (b), patient 3 (c), patient 4 (d), and patient 5 (e). Decreased inflammatory cells after 3 weeks of treatment in patient 1 (f), 4 weeks of treatment in patient 2 (g), 6 weeks of treatment in patient 3 (h), 6 weeks of treatment in patient 4 (i), and 4 weeks of treatment in patient 5 (j)
Results
The age of the patients ranged from 40 to 68 years. All five cases had visual acuity of CF or worse at presentation and with large ulcer size, clean ulcer surface, hypopyon over 3 mm, and retrocorneal plaques. All cases showed reduced corneal sensation. All cases had been treated unsuccessfully with antifungal or antibacterial drugs previously and presented to us with a delay of 1–2 months from the start of symptoms. ASOCT demonstrated the presence of retrocorneal plaques with clear boundaries between the corneal endothelium and the plaques in all cases. IVCM in all cases showed plenty of inflammatory cells without fungal elements in all layers of the cornea and absence or reduction of the sub-basal nerve.
All cases received systemic and topical antiviral treatment combined with topical steroids and two cases received IVIG weekly for 2 weeks. All cases, except case 1 received intravitreal GCV, too. All patients tolerated high-dose systemic GCV therapy, and no side effects were observed. Steroids were gradually tapered and stopped within 4–8 weeks, once the stromal opacity was stable. No recurrence was observed for cases 1–4, during the follow-up period, ranging from 3 to 7 months. All cases, except case 5, who had a history of uncontrolled diabetes and presented late, showed complete resolution of the lesions with nonsurgical treatment within 8 weeks. Case 5 underwent TPK as a result of diffuse anterior synechiae of the iris which eventually failed because of recurrence of viral infection. Table 1 summarizes the five cases.
Discussion
Successful management of infectious keratitis is dependent on timely and accurate diagnosis followed by appropriate interventions. It is primarily diagnosed clinically, supplemented by microbiological examination with staining and culture and sensitivity testing. However, in a real-world setting, diagnosis of infectious keratitis often poses significant diagnostic and therapeutic dilemmas, often due to indistinguishable clinical features shared among different causative organisms and polymicrobial infection [19]. Feathery infiltration and retrocorneal endothelial plaques are commonly associated with fungal keratitis [20, 21]; however, in some cases, viral keratitis will mimic fugal keratitis and present with similar characteristics, which will be misdiagnosed easily and delay the treatment [18, 22]. The inherent limitations of conventional microbiological testing such as variably low culture positivity rate and a long turnaround time are a recurrent theme in literature [19]. While molecular diagnostic techniques like PCR have enhanced the diagnostic yield and accuracy in viral keratitis through corneal scraping or aqueous humor samples, the detection rate is reported to be unsatisfactory and sometimes with numerous false negatives [23, 24]. Recently, a small case series reported that PCR plays an effective role in diagnosing HSV diffuse endotheliitis with feathery infiltration, hypopyon, and retrocorneal plaques [22]. In our study, PCR was positive in three cases and negative in two cases, which might be related to limited sample volume. Thus, the use of imaging techniques like ASOCT plays a crucial role in the accurate and speedy diagnosis of complicated cases of viral keratitis with retrocorneal endothelial plaques. In our study, all five cases had homogeneous and regularly shaped retrocorneal plaques with clear boundaries between the corneal endothelium and the plaque, which were similar to the ASOCT findings of the plaques found in other studies with viral keratitis [18, 25]. However, in fungal keratitis, retrocorneal endothelial plaques showed irregular shape and unclear boundary between the plaque and cornea, which implied that the fungal damage to the endothelium expands from the stroma into the anterior chamber [25]. Besides, ASOCT helped monitor pathology and the response to the treatment, especially the sizes of retrocorneal plaques, which reduced or disappeared within 2 weeks of initiation of treatment. In addition, slit lamp examination revealed the presence of clean ulcerative surface with clear edges (Fig. 1), unlike the dry rough texture seen in fungal keratitis and the dirty and irregular edge seen in bacterial keratitis [26, 26]. Reduced corneal sensation, classically associated with viral infection, played a pivotal role in the diagnosis of severe viral keratitis [28, 29]. When the dormant virus in the trigeminal ganglion is reactivated by triggers like immunosuppression or stress, they start to replicate and travel down the ophthalmic branch of trigeminal nerve, resulting in corneal denervation and reduced corneal sensation [30]. Our findings suggest that the evaluation of characteristics of retrocorneal plaques by noninvasive techniques like ASOCT, clinical findings of clean ulcerative surface on slit lamp examination, and reduced corneal sensation are valuable aids in the differential diagnosis of viral and fungal keratitis.
A significantly large proportion of patients with microbial keratitis progress, usually as a result of missed diagnosis, inappropriate or lack of response to treatment, and often require an emergency tectonic or therapeutic penetrating keratoplasty [31]. It is universally acknowledged that PK has better outcomes if performed at a later, quiescent stage [32]. However, in cases of uncontrolled infection, or impending perforation, TPK may be required without waiting for inflammation to regress and a number of complications like secondary glaucoma, reinfection etc. are expected [31, 33]. Studies have shown that patients with poor presenting visual acuity, large corneal ulcer size over 16 mm2, central location, and presence of hypopyon tend to have higher rates of TKP and poorer outcomes [34, 35]. All cases in our study had significantly poor presenting visual acuity (CF or worse), large centrally located ulcer with size over 16 mm2 and hypopyon over 3-mm, non-responsive to the antibacterial and antifungal treatment given initially, and were potential candidates for emergency TPK. Nevertheless, with only conservative but aggressive treatment, we achieved complete resolution of the lesions with scarring, with potential for successful optical keratoplasty at a later stage.
In our study, four cases benefited from conservative treatment. Only patient 5 underwent TPK in the inflammatory stage because of diffuse anterior synechiae of the iris. However, the graft failed with recurrence seen on day 10 and irreversible loss of clarity in 1 month after TPK. While TPK was performed to prevent secondary glaucoma, the graft failed probably because of the uncontrolled inflammation caused by active virus. PK for herpetic infections is usually associated with poor visual outcomes mainly due to recurrences of herpetic infection, graft rejection, and graft failure [36]. Grafts in eyes with active inflammation have an even more dismal outlook with less than a quarter of eyes with active inflammation surviving compared to 85% of those with quiescent scars as a result of the increasing risks of rejection caused by deep corneal vascularization, corneal hypoesthesia, and reduced endothelial cell density (ECD) [37,38,39]. Waiting until the eye is quiet for a few months may improve the outcomes.
An interesting aspect in our study was the use of IVIG in severe viral keratitis. IVIGs are therapeutic preparations of human immunoglobulins derived from pooled plasma of healthy individuals [40]. IVIG therapy aims to replenish sufficient amounts of IgG antibodies that passively neutralize a broad spectrum of infectious pathogens and elicit an active immune response, thus conferring protection against diverse diseases [41]. Studies have shown that in severe infections, they act synergistically with antibiotics with immunomodulatory and additional anti-inflammatory activity, too [40, 41]. While the role of IVIG in severe suppurative keratitis in humans is unclear, a study on a mouse ocular infection model demonstrated that treating epithelial herpes simplex keratitis with topical immunoglobulins attenuates the spread and incidence rate of HSV-1 [42]. In a recent study, IVIG was used as rescue treatment in a ganciclovir-resistant cytomegalovirus retinitis [43]. In our study, the two cases (patients 1 and 2) who received weekly IVIG (5 mg) for 2 weeks, in addition to antivirals and steroids, showed significant improvement within 3–4 weeks. In contrast, the other two cases (patients 3 and 4) took longer to achieve resolution of inflammation with only antiviral medication and steroids. Although the number of cases is too small, IVIG seems to show promise as a potential treatment for treating severe refractory viral keratitis and future investigations of this therapy will be valuable.
There are some limitations in our study. Firstly, the sample size was small as it was basically a retrospective study in a single center, over a year. However, our study offers some important insights into diagnosis and treatment strategy of severe viral keratitis. Conservative medical management may be a viable option even in severe cases instead of the conventional therapeutic keratoplasty which carries the risk of poor outcomes in eyes with active viral infection. Though our study preliminarily suggests IVIG may have a role in cases of severe viral keratitis, further research is needed to investigate its dosage, ocular penetrability, drug-giving modalities (intravenously or topically), and validate its effectiveness.
Conclusions
Evaluation of characteristics of retrocorneal plaques by ASOCT and reduced corneal sensation can help in speedy diagnosis of complicated, atypical cases of viral keratitis, even when microbiological tests may be negative. Conservative but aggressive medical management may result in resolution of active keratitis, without the need for emergency surgical intervention.
References
Tan DT, Dart JK, Holland EJ, Kinoshita S. Corneal transplantation. Lancet. 2012;379(9827):1749–61.
Ting DSJ, Ho CS, Deshmukh R, Said DG, Dua HS. Infectious keratitis: an update on epidemiology, causative microorganisms, risk factors, and antimicrobial resistance. Eye (Lond). 2021;35(4):1084–101.
Khor WB, Prajna VN, Garg P, et al. The Asia Cornea Society infectious keratitis study: a prospective multicenter study of infectious keratitis in Asia. Am J Ophthalmol. 2018;195:161–70.
Luengo-Gimeno F, Tan DT, Mehta JS. Evolution of deep anterior lamellar keratoplasty (DALK). Ocul Surf. 2011;9(2):98–110.
Tan DT, Janardhanan P, Zhou H, et al. Penetrating keratoplasty in Asian eyes: the Singapore Corneal Transplant Study. Ophthalmology. 2008;115(6):975e1–82e1.
Bajracharya L, Gurung R. Outcome of therapeutic penetrating keratoplasty in a tertiary eye care center in Nepal. Clin Ophthalmol. 2015;9:2299–304.
Xie L, Hu J, Shi W. Treatment failure after lamellar keratoplasty for fungal keratitis. Ophthalmology. 2008;115(1):33–6.
Palioura S, Tsiampali C, Dubovy SR, Yoo SH. Endothelial biopsy for the diagnosis and management of culture-negative retrocorneal fungal keratitis with the assistance of optical coherence tomography imaging. Cornea. 2021;40(9):1193–6.
Mocan MC, Irkec M, Mikropoulos DG, Bozkurt B, Orhan M, Konstas AG. In vivo confocal microscopic evaluation of the inflammatory response in non-epithelial herpes simplex keratitis. Curr Eye Res. 2012;37(12):1099–106.
Taravati P, Lam D, Van Gelder RN. Role of molecular diagnostics in ocular microbiology. Curr Ophthalmol Rep. 2013;1(4):181–9.
Leal SM Jr, Rodino KG, Fowler WC, Gilligan PH. Practical guidance for clinical microbiology laboratories: diagnosis of ocular infections. Clin Microbiol Rev. 2021;34(3): e0007019.
Subhan S, Jose RJ, Duggirala A, et al. Diagnosis of herpes simplex virus-1 keratitis: comparison of Giemsa stain, immunofluorescence assay and polymerase chain reaction. Curr Eye Res. 2004;29(2–3):209–13.
Erdem E, Harbiyeli İİ, Öztürk G, et al. Atypical herpes simplex keratitis: frequency, clinical presentations and treatment results. Int Ophthalmol. 2020;40(3):659–65.
Koizumi N, Nishida K, Adachi W, et al. Detection of herpes simplex virus DNA in atypical epithelial keratitis using polymerase chain reaction. Br J Ophthalmol. 1999;83(8):957–60.
Poon SHL, Wong WHL, Lo ACY, et al. A systematic review on advances in diagnostics for herpes simplex keratitis. Surv Ophthalmol. 2021;66(3):514–30.
Kosker M, Duman F, Suri K, Hammersmith KM, Nagra PK, Rapuano CJ. Long-term results of keratoplasty in patients with herpes zoster ophthalmicus. Cornea. 2013;32(7):982–6.
Soong HK, Schwartz AE, Meyer RF, Sugar A. Penetrating keratoplasty for corneal scarring due to herpes zoster ophthalmicus. Br J Ophthalmol. 1989;73(1):19–21.
Yu S, You D, Agrawal R, Feng Y. Noninvasive Diagnosis of Viral Keratouveitis with Retro-corneal Endothelial Plaques: a Case Series. Ocul Immunol Inflamm. 2021;1–7.
Ting DSJ, Gopal BP, Deshmukh R, Seitzman GD, Said DG, Dua HS. Diagnostic armamentarium of infectious keratitis: a comprehensive review. Ocul Surf. 2022;23:27–39.
Thomas PA, Leck AK, Myatt M. Characteristic clinical features as an aid to the diagnosis of suppurative keratitis caused by filamentous fungi. Br J Ophthalmol. 2005;89(12):1554–8.
Ting DSJ, Galal M, Kulkarni B, et al. Clinical characteristics and outcomes of fungal keratitis in the United Kingdom 2011–2020: a 10-year study. J Fungi (Basel). 2021;7(11):966.
Todokoro D, Hosogai M, Nakano S, Akiyama H. Effective diagnosis by real-time PCR of herpes simplex diffuse endotheliitis that is similar in appearance to fungal keratitis: case series. J Ophthal Inflamm Infect. 2021;11(1):20.
McGilligan V, Moore J, Tallouzi M, et al. A comparison of the clinical and molecular diagnosis of herpes simplex keratitis. Open J Ophthalmol. 2014;4:65–74.
Schacher S, Garweg JG, Russ C, Böhnke M. Diagnosis of herpetic uveitis and keratouveitis. Klin Monbl Augenheilkd. 1998;212(5):359–62.
Takezawa Y, Suzuki T, Shiraishi A. Observation of retrocorneal plaques in patients with infectious keratitis using anterior segment optical coherence tomography. Cornea. 2017;36(10):1237–42.
Castano G, Elnahry AG, Mada PK. Fungal keratitis. In: StatPearls. StatPearls Publishing, Treasure Island, FL; 2022.
Cabrera-Aguas M, Khoo P, Watson SL. Infectious keratitis: a review. Clin Exp Ophthalmol. 2022;50(5):543–62.
Safi M, Rose-Nussbaumer J. Overview of neurotrophic keratopathy and a stage-based approach to its management. Eye Contact Lens. 2021;47(3):140–3.
Hsu HY, Modi D. Etiologies, quantitative hypoesthesia, and clinical outcomes of neurotrophic keratopathy. Eye Contact Lens. 2015;41(5):314–7.
Herpetic Eye Disease Study Group. Psychological stress and other potential triggers for recurrences of herpes simplex virus eye infections. Arch Ophthalmol. 2000;118(12):1617–25.
Raj A, Bahadur H, Dhasmana R. Outcome of therapeutic penetrating keratoplasty in advanced infectious keratitis. J Curr Ophthalmol. 2018;30(4):315–20.
Lomholt JA, Ehlers N. Graft survival and risk factors of penetrating keratoplasty for microbial keratitis. Acta Ophthalmol Scand. 1997;75(4):418–22.
Sharma N, Jain M, Sehra SV, et al. Outcomes of therapeutic penetrating keratoplasty from a tertiary eye care centre in northern India. Cornea. 2014;33(2):114–8.
Miedziak AI, Miller MR, Rapuano CJ, Laibson PR, Cohen EJ. Risk factors in microbial keratitis leading to penetrating keratoplasty. Ophthalmology. 1999;106(6):1166–70.
Gümüş G, Kırgız A, Yıldırım Y, et al. Prognostic factors affecting graft survival in patients undergoing penetrating keratoplasty for infectious keratitis. Turk J Ophthalmol. 2020;50(6):324–31.
Altay Y, Tamer S, Kaya AS, Balta O, Burcu A, Ornek F. The outcome of penetrating keratoplasty for corneal scarring due to herpes simplex keratitis. Arq Bras Oftalmol. 2017;80(1):41–5.
Killingsworth DW, Stern GA, Driebe WT, Knapp A, Dragon DM. Results of therapeutic penetrating keratoplasty. Ophthalmology. 1993;100(4):534–41.
Said DG, Rallis KI, Al-Aqaba MA, Ting DSJ, Dua HS. Surgical management of infectious keratitis. Ocul Surf. 2021. https://doi.org/10.1016/j.jtos.2021.09.005.
Kusano Y, Yamaguchi T, Nishisako S, et al. Elevated cytokine levels in aqueous humor are associated with peripheral anterior synechiae after penetrating keratoplasty. Int J Mol Sci. 2021;22(22):12268.
Perez EE, Orange JS, Bonilla F, et al. Update on the use of immunoglobulin in human disease: a review of evidence. J Allergy Clin Immunol. 2017;139(3S):S1–46.
Daneshpazhooh M, Soori T, Isazade A, Noormohammadpour P. Mucous membrane pemphigoid and COVID-19 treated with high-dose intravenous immunoglobulins: a case report. J Dermatol Treat. 2020;31(5):446–7.
Kläger AJ, Büchi ER, Osusky R, Burek-Kozlowska A, Morell A. Topical immunoglobulins for epithelial herpes simplex keratitis. Ophthalmologica. 1993;207(2):78–81.
Fu L, Santhanakrishnan K, Al-Aloul M, Jones NP, Steeples LR. Management of ganciclovir resistant cytomegalovirus retinitis in a solid organ transplant recipient: a review of current evidence and treatment approaches. Ocul Immunol Inflamm. 2020;28(7):1152–8.
Acknowledgements
Funding
The study, and the journal’s Rapid Service fees, were supported in part by National Natural Science Foundation of China (No. 81700799; 82070926). The funders had no role in the study design, data collection and analysis, decision on publishing, or preparation of the manuscript.
Author Contributions
All authors contributed to the conception and design, acquisition of data, analysis and interpretation of data. Zhen Yang and Yun Feng wrote the manuscript. All authors read and approved the submission of this manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest and no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Compliance with Ethics Guidelines
The study was performed in accordance with the Declaration of Helsinki of 1964 and its later amendments and approval was obtained from the ethics committee of Peking University Third Hospital. Informed consent was obtained from all participants included in the study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yang, Z., Yu, S., Zhang, C. et al. Nonsurgical Management of Severe Viral Keratitis with Hypopyon and Retrocorneal Plaques: A Case Series. Ophthalmol Ther 12, 599–611 (2023). https://doi.org/10.1007/s40123-022-00592-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00592-x