Abstract
Introduction
To investigate the long-term results of laser in situ keratomileusis (LASIK) in patients with one or more topographic indices outside the suggested range preoperatively.
Methods
Patients who had conventional or femtosecond laser-assisted LASIK for myopia correction between 2011 and 2015, and had at least one preoperative corneal topographic index outside the suggested range were contacted for a follow-up examination. Ranges were based on the cutoffs suggested for subclinical keratoconus: thinnest pachymetry (TP) < 497.50 µm, maximum keratometry (Kmax) > 47.20 D, maximum 8 mm best-fit-sphere anterior elevation (MaxAE) > 9.50 µm, maximum 8 mm best-fit-sphere posterior elevation (MaxPE) > 20.50 µm, and Belin/Ambrósio enhanced ectasia display-total deviation (BAD-D) > 1.60.
Results
Two hundred thirty patients (377 eyes) were enrolled; their mean age at baseline and at follow-up was 30.78 ± 8.16 and 9.06 ± 1.91 years, respectively. Mean ± SD was 484.36 ± 11.49 for TP (n = 133), 48.17 ± 0.83 for Kmax (n = 133), 16.33 ± 5.39 for MaxAE (n = 35), 27.87 ± 7.86 for MaxPE (n = 34), and 1.97 ± 0.36 for BAD-D (n = 162). Post-LASIK and suspected ectasia was found in one (0.26%) and two (0.53%) eyes, respectively. In the remaining 374, the efficacy and safety indices were 0.96 ± 0.14 and 1.01 ± 0.08, respectively. Uncorrected distance visual acuity (UDVA) was not reduced in any eyes, and corrected distance visual acuity (CDVA) was reduced one line in 1.9% of the cases; 79.9% of the cases were emmetropic. The long-term changes in UDVA, CDVA, and spherical equivalent were not different between groups with one, two, or three out-of-range topographic indices (all P > 0.05).
Conclusion
A single out-of-range topographic index is not a strong predictor for postoperative complications, and one should consider the combination of topographic and clinical findings, or the pattern they create in tandem. Developing a scoring system that would take a combination of indices and topographic patterns may help improve the predictive accuracy of these indices.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Corneal ectasia is one of the most serious complications after laser vision correction. |
One of the risk factors is abnormal preoperative corneal topography. |
What was learned from the study? |
Out-of-range topographic indices are not strong predictors for postoperative complications in cases with RSB ≥ 300 µm. |
Out-of-range topographic indices are not associated with deteriorating postoperative visual or refractive outcomes in cases with RSB ≥ 300 µm. |
Modifying the reference range of topographic indices is necessary to improve the predictive accuracy in each population. |
Introduction
Laser eye surgery, which is widely used to correct refractive errors, is one of the most effective surgical procedures today, but comes with its own risks. Corneal ectasia is one of the most serious complications after laser vision correction, which although rare, can be quite devastating [1, 2]. Similar to keratoconus, corneal ectasia following laser surgery causes progressive corneal steepening and reduces visual acuity [3, 4]. Previous studies have identified certain risk factors; however, it may also occur without any known predisposing factors [5, 6]. One of the risk factors, which has been widely investigated, is abnormal preoperative corneal topography [3]. Several studies have suggested that abnormal findings at preoperative examinations, such as inferior steepening or thin cornea, are important factors in developing postoperative ectasia; however, there is still no consensus on the efficacy and safety of laser eye surgery in patients with atypical corneal topography [7]. In most cases, clinicians do not rely on only one parameter, and they need to make a discretionary decision based on multiple parameters as well as clinical information such as the amount of correction and corneal thickness. The present study was conducted to evaluate the long-term outcomes of laser in situ keratomileusis (LASIK) in patients with at least one abnormal (outside suggested range) preoperative corneal topography index, and to determine the efficacy and safety of this technique in these patients.
Methods
Patients and Sampling
This historical cohort study was performed at Noor Eye Hospital, Tehran, Iran, in 2020. Patients were identified through a retrospective chart review of those who had conventional or femtosecond LASIK for the correction of myopia between 2011 and 2015. Inclusion criteria was having at least one abnormal topographic index in their preoperative topography. Abnormality was defined based on cutoffs suggested for subclinical keratoconus (KC): thinnest pachymetry (TP) < 497.50 µm [8], Kmax > 47.20 D [9], maximum 8 mm best-fit-sphere anterior elevation (MaxAE) > 9.50 µm [8], maximum 8 mm best-fit-sphere posterior elevation (MaxPE) > 20.50 µm [8], or Belin/Ambrósio enhanced ectasia display (BAD-D) > 1.60 standard deviation of mean [10]. Cases with a history of ocular surgery prior to LASIK or retreatment were not included.
Patients who met the inclusion criteria were contacted by phone and invited to have a follow-up examination. Attempts to call them were repeated once weekly, up to ten times. For those who agreed to participate, an appointment was scheduled to have their examinations at the clinic. The appointments were rescheduled as necessary. On the scheduled day, patients first signed the consent before undergoing follow-up examinations (see Examinations section below).
Compliance with Ethics Guidelines
The study was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1401.013) and adhered to the Helsinki Declaration at all stages. Before enrollment, the objectives and methodology of the study were explained to the patients, and informed consent was obtained for participating in the study.
Baseline Criteria and Surgical Technique
Eligibility criteria for refractive surgery were minimum age of 20.00 years, stable refraction over the past year (maximum 0.50 D change), and a residual stromal bed thickness of ≥ 300.00 µm. Those with any signs suggestive of definite KC or systemic disease were not eligible.
In FS-LASIK, after local anesthesia, a 110.0-μm flap was created using Femto LDV (Ziemer Ophthalmic Systems AG, Port, Switzerland). After lifting the flap, ablation was performed using the ALLEGRETTO Concerto excimer laser (WaveLight Laser Technologie AG) or AMARIS 1050RS (SCHWIND, Munich, Germany). In the conventional LASIK group, flaps were created using the Hansatome mechanical microkeratome (Bausch & Lomb, Miami, FL, USA) with a thickness of 160 μm, and ablation was done using the ALLEGRETTO Concerto excimer laser (WaveLight Laser Technologie AG) or VISX STAR S4 Excimer laser (Abbott Medical Optics Inc, CA, USA). In both groups, the optical zone was 6.5 mm in patients with moderate myopia (3.00–6.00 D) and 6.0 mm in cases with high myopia (> 6.00 D) with a blend zone of 1.25 mm. Postoperative treatment regimen included chloramphenicol 0.5% eye drops (Sina Darou, Tehran, Iran) every 6 h for 3 days and betamethasone 0.1% eye drops (Sina Darou, Tehran, Iran) every 6 h for 7 days.
Examinations
Evaluations included ophthalmologic examination with slit lamp (Haag-Streit, Mason, OH, USA) plus measurement of uncorrected (UDVA) and corrected distance visual acuity (CDVA) using the Snellen SC-2000 (Nidek Inc., Tokyo, Japan) and refraction using a retinoscope (ParaStop HEINE BETA 200; HEINE Optotechnik, Herrsching, Germany). Depending on the imaging device used at baseline, follow-up imaging was done with the Pentacam (Oculus Optikgeräte GmbH, Wetzlar, Germany) for 365 eyes, or with the EyeSys (EyeSys Vision, TX, USA) and ultrasound pachymetry (Echoscan, Camagori, Japan) for 12 eyes. Only photos with quality specification displayed as “OK” in Pentacam or without any measurement error in EyeSys were accepted.
Statistical Analysis
Microsoft Excel and Stata Statistical Software: Release 14. (Stata, Corp. LP, College Station, TX, USA) were used for data analysis. For each index, eyes were classified into normal and abnormal subgroups. They were also subgrouped based on the number of out-of-range indices (1, 2, 3, and 4). Cases with extreme indices (TP < 470.00 µm, Kmax > 48.70 D, MaxAE > 15.75 µm, MaxPE > 25.50 µm, and BAD-D > 2.59) were also assessed as a separate category.
Generalized estimating equations (GEE) were used to compare changes in UDVA, CDVA, and manifest spherical refraction equivalent (MRSE) between these subgroups. The correlation between fellow eyes was accounted for using an exchangeable correlation matrix. In addition, the efficacy (postoperative UDVA/preoperative CDVA) and safety indices (postoperative CDVA/preoperative CDVA) were assessed. A significance level of 0.05 was considered statistically significant. Information on post-LASIK ectasia cases is presented separately.
Results
Two hundred thirty myopic patients (377 eyes) with an MRSE −4.24 ± 1.90 D (range −10.75 to −1.00 D) and median age of 29.00 years at the time of surgery were studied; of these, 64.5% were female and 91.0% had undergone FS-LASIK. The mean follow-up time was 9.06 ± 1.91 (range 5.00–10.00) years.
Two eyes of one patient had a suspected corneal pattern at the time of the study, and there were no signs indicative of abnormal progression in the follow-ups until 2019.
One eye of a 35-year-old (at baseline) woman had post FS-LASIK ectasia. By 5 years after surgery (compared with preoperatively), UDVA improved from count fingers to 2 m, CDVA had reduced from 20/20 to 20/32, and MRSE was corrected from −5.75 to 1.00 × 57° to −1.00 to 2.25 × 63°. Among the studied indices, only BAD-D was out of range preoperatively (1.78) and increased to 12.67 at 5 years after surgery. Baseline and postoperative topography maps of these three cases are shown in Fig. 1, and their data were not included in the analysis.
Table 1 presents the mean ± standard deviation (SD), range, 95% confidence interval (CI), and median of each out-of-range and extreme index in the 374 studied eyes. The number of eyes with 1, 2, and 3 out-of-range indices preoperatively were 259, 95, and 19, respectively (Fig. 2). Only one patient had four out-of-range indices. The most common indices were BAD-D (34.10%) and TP (33.60%) among cases with one out-of-range index, BAD-D & TP (37.60%) and BAD-D & Kmax (30.10%) among cases with two out-of-range indices, and Kmax & MaxAE & MaxPE (38.10%) among those with three out-of-range indices.
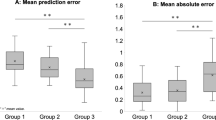
Compared with preoperative results, current UDVA was not reduced and CDVA was 20/20 or better in 96.20% and 20/25 in 2.80% of the cases. Only three eyes (0.90%) had a CDVA of less than 20/32 in which CDVA increased by one line in one eye, was unchanged in one eye, and decreased by one line in the other eye. The efficacy index was 0.96 ± 0.14 and the safety index was 1.01 ± 0.08 (Fig. 3). A decrease of one line of CDVA was observed in seven eyes (1.90%) of seven FS-LASIK patients. There was no sign of ectasia in any of these cases. Long-term vision and refraction outcomes in these seven cases are summarized in Table 2.
In terms of refraction, mean preoperative and long-term follow-up values were, respectively, −3.42 ± 1.95 D and + 0.09 ± 0.58 D for spherical error, −1.65 ± 1.48 D and −0.55 ± 0.41 D for astigmatism, and −4.24 ± 1.90 D and −0.18 ± 0.63 D for MRSE (all P < 0.001). As shown in Fig. 4, 79.9% of the cases were emmetropic, 6.70% were myopic (MRSE < −0.5 D), and 12.00% were hyperopic (MRSE > + 0.5 D) at this long-term follow-up examination.
Table 3 presents the changes in vision and refraction of the patients with one, two, three, and four (n = 1) out-of-range indices. UDVA improvement and MRSE reduction were statistically significant in all groups. CDVA did not show significant changes. None of the differences between the groups was statistically significant (all P > 0.05).
There were 46 eyes with only one extreme range index and 17 eyes with two extreme range indices. As illustrated in Fig. 5, the most common extreme range indices were Kmax (32.60%) and TP (30.40%). In those with two extreme range indices, the most common combination was MaxPE and MaxAE (58.80%). Table 4 summarizes long-term outcomes of cases with extreme range indices. The logMAR of UDVA and MRSE were significantly reduced in these cases, but CDVA showed no significant change. Changes in these three outcome parameters were not significantly different between the two groups with one and two extreme range indices (all P > 0.05).
Discussion
The present study examined the long-term results of LASIK in patients with topographic indices outside the suggested ranges. Minimum follow-up time was 5 years, and the average follow-up was 9 years, which, to the best of our knowledge, is the longest follow-up time among similar studies. The results showed that the incidence of post-LASIK ectasia in patients with topographic indices outside suggested ranges was about 0.26% at 9 years after surgery. This value ranges between 0.11 and 0.93 in similar studies on patients with normal ranges of indices [11,12,13,14,15,16,17,18,19]. Some of the variation in the reported incidence of post-LASIK ectasia can be attributed to differences in the sample size and follow-up time, as well as corneal characteristics of the study populations. Of note, post-LASIK ectasia has been reported in cases with normal preoperative topography, and not all ectatic cases necessarily have abnormal thickness, keratometry, or corneal topographic patterns.
In our study, the efficacy and safety indices of LASIK were 0.96 and 1.01, respectively. Gomel et al. [2] reported 13-year safety and efficacy indices of 1.03 and 0.97, respectively, for patients without any sign of KC, similar to the present study. Chua et al. [12] found that 97.8% of the patients without any sign of KC and ectasia achieved a UCVA of ≥ 20/40 and less than 5.00% experienced a CDVA reduction of one or more lines after 18 years, while all patients had a UCVA of ≥ 20/40 and only 1.90% experienced a CDVA reduction in the present study. None of these cases had signs of corneal ectasia or irregular astigmatism in their topography. The one-line CDVA decline could be due to an increase in spherical error in one eye, and perhaps on account of measurement repeatability over such a long follow-up time in others. Therefore, it seems that there is no significant difference in the safety of LASIK between patients with out-of-range topographic indices and the normal population.
In our study, achieving a target refraction after LASIK in patients with out-of-range corneal indices preoperatively is similar to the reported normal population. Based on the results of the present study, 79.90% of eyes achieved ± 0.50 D and 92.40% of eyes achieved ± 1.00 D of the target refraction. These results are similar to previous studies in normal populations where the authors reported that 67.80–74.80% of the eyes achieved ± 0.50 D of target refraction and 76.20–97.60% of the eyes achieved ± 1.00 D of target refraction [12, 20, 21]. It can be concluded that patients with topographic indices slightly over the suggested range experienced good refractive changes after LASIK.
Lack of difference between cases with one, two, or three out-of-range indices indicates that the none of these indices alone could predict the complications or ineffectiveness of LASIK. Even patients with two or more out-of-range topographic indices experienced acceptable outcomes without any complications.
The main strength of this study was the long-term follow-up of patients. Since ectasia, as one of the most important complications of the LASIK procedure, may occur 1 week to several years after surgery [12], long-term follow-up can lead to more accurate conclusions. Furthermore, a larger sample size allows examination of the effect of corneal abnormality on the outcomes in each of the low, moderate, and high myopia subgroups separately. Another limitation was lack of data on corneal biomechanics; having such data would allow us to perform more detailed analyses of these cases using novel predictive indices of corneal ectasia.
Conclusions
In conclusion, having slight to moderately out-of-range topographic indices alone does not predict ectasia and unfavorable outcomes after surgery in patients with RSB ≥ 300 µm. Perhaps the suggested ranges are not suitable for identifying risk factors in our population, and they need to be revised to improve the predictive accuracy. Developing a scoring system that would take a combination of indices, especially novel ones, as well as topographic patterns may help achieve this goal.
References
Moshirfar M, Tukan AN, Bundogji N, et al. Ectasia After Corneal Refractive Surgery: A Systematic Review. Ophthalm Ther. 2021;10:753–76.
Gomel N, Negari S, Frucht-Pery J, Wajnsztajn D, Strassman E, Solomon A. Predictive factors for efficacy and safety in refractive surgery for myopia. PLoS ONE. 2018;13: e0208608.
Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110:267–75.
Seiler T, Quurke AW. Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. J Cataract Refract Surg. 1998;24:1007–9.
Giri P, Azar DT. Risk profiles of ectasia after keratorefractive surgery. Curr Opin Ophthalmol. 2017;28:337–42.
Santhiago MR, Giacomin NT, Smadja D, Bechara SJ. Ectasia risk factors in refractive surgery. Clin Ophthalmol. 2016;10:713–20.
Jin SX, Dackowski E, Chuck RS. Risk factors for postlaser refractive surgery corneal ectasia. Curr Opin Ophthalmol. 2020;31:288–92.
Uçakhan Ö, Cetinkor V, Özkan M, Kanpolat A. Evaluation of Scheimpflug imaging parameters in subclinical keratoconus, keratoconus, and normal eyes. J Cataract Refract Surg. 2011;37:1116–24.
Rabinowitz YS, Rasheed K. KISA% index: a quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J Cataract Refract Surg. 1999;25:1327–35.
Villavicencio GF, Henriquez MA, Izquierdo L Jr, Ambrosio RR Jr, Belin MW. Independent population validation of the Belin/Ambrosio enhanced ectasia display: implications for keratoconus studies and screening. Int J Kerat Ect Cor Dis. 2014;3:1–8.
Bohac M, Koncarevic M, Pasalic A, et al. Incidence and clinical characteristics of post LASIK ectasia: a review of over 30,000 LASIK cases. Semin Ophthalmol. 2018;33:869–77.
Chua D, Htoon HM, Lim L, et al. Eighteen-year prospective audit of LASIK outcomes for myopia in 53 731 eyes. Br J Ophthalmol. 2019;103:1228–34.
Condon PI, O’Keefe M, Binder PS. Long-term results of laser in situ keratomileusis for high myopia: risk for ectasia. J Cataract Refract Surg. 2007;33:583–90.
Moshirfar M, Smedley JG, Muthappan V, Jarsted A, Ostler EM. Rate of ectasia and incidence of irregular topography in patients with unidentified preoperative risk factors undergoing femtosecond laser-assisted LASIK. Clin Ophthalmol. 2014;8:35.
Pallikaris IG, Kymionis GD, Astyrakakis NI. Corneal ectasia induced by laser in situ keratomileusis. J Cataract Refract Surg. 2001;27:1796–802.
Rad AS, Jabbarvand M, Saifi N. Progressive keratectasia after laser in situ keratomileusis. J Refract Surg. 2004;20:S718–22.
Reinstein DZ, Srivannaboon S, Archer TJ, Silverman RH, Sutton H, Coleman DJ. Probability model of the inaccuracy of residual stromal thickness prediction to reduce the risk of ectasia after LASIK part II: quantifying population risk. J Refract Surg. 2006;22:861–70.
Schallhorn JM, Schallhorn SC, Teenan D, Hannan SJ, Pelouskova M, Venter JA. Incidence of intraoperative and early postoperative adverse events in a large cohort of consecutive laser vision correction treatments. Am J Ophthalmol. 2020;210:97–106.
Spadea L, Cantera E, Cortes M, Conocchia NE, Stewart CW. Corneal ectasia after myopic laser in situ keratomileusis: a long-term study. Clin Ophthalmol. 2012;6:1801.
Ide T, Toda I, Fukumoto T, Watanabe J, Tsubota K. Outcome of a 10-year follow-up of laser in situ laser keratomileusis for myopia and myopic astigmatism. Taiwan J Ophthalmol. 2014;4:156–62.
Kim J-Y, Lee H, Joo C-K, et al. Three-year follow-up of laser in situ keratomileusis treatments for myopia: multi-center cohort study in Korean population. J Pers Med. 2021;11:419.
Acknowledgements
We thank the patients for participating in this study.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Concept and design (HH, SA), acquisition of data (SA and TA), statistical analysis (SM and SA), interpretation of result (HH, SA and SM), drafting the manuscript (SM, PP and SA), critical revision and final approve (all authors).
Disclosures
Hassan Hashemi, Shiva Mehravaran, Parsa Panahi, Tahereh Abdollahinia, and Soheila Asgari have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1401.013) and adhered to the Helsinki Declaration at all stages. Before enrollment, the objectives and methodology of the study were explained to the patients, and informed consent was obtained for participating in the study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hashemi, H., Mehravaran, S., Panahi, P. et al. Long-Term Results of Laser In Situ Keratomileusis in Myopic Patients with Topographic Indices outside Suggested Ranges. Ophthalmol Ther 11, 2285–2295 (2022). https://doi.org/10.1007/s40123-022-00589-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00589-6