Abstract
Introduction
To compare three monthly injections versus one initial injection of intravitreal ranibizumab (IVR) followed by pro re nata (PRN) dosing to treat macular edema secondary to branch retinal vein occlusion (BRVO).
Methods
Seventy-four patients were randomized (1:1) to the 3 + PRN or 1 + PRN groups. Patients underwent monthly evaluations and additional IVR injections were administered if the retreatment criteria were met. The functional and anatomical outcomes were recorded. The factors associated with the improvement in best-corrected visual acuity (BCVA) were analyzed.
Results
Sixty-nine patients (93.2%) completed the study. At 12 months, the mean gain in BCVA was 12.9 letters in the 3 + PRN group and 14.3 letters in the 1 + PRN group, which was not significant (P = 0.59). The mean reduction in central macular thickness was 297.8 μm in the 3 + PRN group and 300.2 μm in the 1 + PRN group (P = 0.96). The macular vascular density changes of the superficial and deep capillary plexuses were not significantly different between the two groups (P = 0.99 and 0.70, respectively). The mean number of IVR injections was 5.0 in the 3 + PRN group and 4.2 in the 1 + PRN group (P = 0.17). The incidence of retinal neovascularization was similar in both groups (P = 0.67). The baseline BCVA, but not the treatment regimen, was significantly associated with the change in BCVA (P < 0.01).
Conclusion
Significant gains in BCVA and maintenance of macular perfusion were achieved in BRVO eyes treated with the 3 + PRN or 1 + PRN regimens. Baseline BCVA was a prognostic factor for the visual improvement.
Trial Registration
A prospective randomized controlled trial to compare the 1 + PRN and 3 + PRN regimen in the treatment of macular edema secondary to branch retinal vein occlusion (ChiCTR2000038086).
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Few prospective randomized studies have compared the efficacy of the 3 + PRN and 1 + PRN regimens and corresponding vascular density changes revealed by SS-OCTA. |
We showed that the 1 + PRN and 3 + PRN treatment regimens resulted in rapid and sustained improvements in anatomy and function at 12 months, with similar intravitreal frequency. |
The macular perfusion of eyes with BRVO shown on SS-OCTA was preserved at month 12 when following the 3 + PRN or 1 + PRN regimen. |
The 1 + PRN and 3 + PRN regimens are effective and affordable for visual acuity improvement without worsening of macular ischemia. |
Baseline BCVA can be helpful in predicting BCVA improvement after anti-VEGF treatment in patients with macular edema due to BRVO. |
Introduction
Branch retinal vein occlusion (BRVO) is a major cause of vision impairment worldwide and frequently causes macular edema (ME). Anti-vascular endothelial growth factor (VEGF) therapy can achieve a rapid reduction in ME and improve visual function, and is thus accepted as first-line therapy for most patients with ME secondary to BRVO [1].
There is a lack of consensus on the best treatment regimen for anti-VEGF dosing for ME secondary to BRVO. The BRAVO study, which was the first prospective, randomized, multicenter study of this type of treatment with ranibizumab, assessed the efficacy and safety of a dosing regimen comprising six monthly intravitreal ranibizumab (IVR) injections followed by six pro re nata (6 + PRN) injections [2]. The study showed favorable visual and anatomical outcomes after 12-month follow-up, and the mean number of IVR injections was 8.4 [3]. The BRIGHTER study, which was also a prospective, randomized, multicenter study, reported favorable functional and anatomical outcomes of a regimen comprising three loading doses followed by PRN (3 + PRN) administration [4]. Over a period of 1 year in clinical practice, Brynskov et al. reported that the mean number of IVR injections was five using the 3 + PRN regimen, and they demonstrated the efficacy of this regimen in the real world [5]. Nevertheless, frequent injections for treatment-naive patients with BRVO are insubstantial in real clinical settings, and multiple continuous injections may increase the risk of ocular and systemic adverse effects [6, 7]. The prospective MARVEL study demonstrated that intravitreal administration of bevacizumab or ranibizumab using a regimen comprising one dose plus PRN (1 + PRN) also led to meaningful improvements in visual acuity in patients with ME secondary to BRVO [8]. Furthermore, Miwa et al. and Bayat et al. compared the 1 + PRN and 3 + PRN regimens for ME caused by BRVO and reported that the visual functional outcomes were comparable for the two regimens [9, 10].
To the best of our knowledge, there are no published prospective randomized studies comparing the efficacy of 1 + PRN versus 3 + PRN regimens for treating ME secondary to BRVO. In this prospective randomized study, we compared the 12-month visual and anatomical outcomes between these two treatment regimens using multimodal imaging, including swept-source optical coherence tomography angiography (SS-OCTA).
Methods
Study Design
This was an investigator-initiated, prospective, randomized controlled trial (registered at www.chictr.org.cn, accession number ChiCTR2000038086) sponsored by Novartis Pharma AG (Basel, Switzerland). The institutional review board of the Eye and ENT Hospital of Fudan University approved the study (No. 2018037-1) and each participant provided written informed consent. The study adhered to the Declaration of Helsinki. Patients were recruited from January 2019 to December 2020 at the Eye and ENT Hospital of Fudan University, Shanghai, China.
Patients
BRVO was diagnosed based on the results of fundus examination and fluorescein angiography (FA) performed by vitreoretinal specialists (L.W. and C.Q.). Key eligibility criteria included: (1) treatment-naive patients aged ≥ 18 years; (2) baseline best-corrected visual acuity (BCVA) of ≥ 19 letters (approximate Snellen chart equivalent of 20/400) according to the Early Treatment Diabetic Retinopathy Study (ETDRS) scale; (3) spectral-domain optical coherence tomography (SD-OCT) central macular thickness (CMT) ≥ 250 μm caused by ME secondary to BRVO; and (4) time since diagnosis of < 6 months for the study eye. Key exclusion criteria included: (1) ME caused by other ocular pathologies, such as diabetic retinopathy or neovascular age-related macular degeneration; (2) severe media opacities affecting fundus examination; (3) previous intravitreal injection of corticosteroids or anti-VEGF therapies; (4) history of laser photocoagulation or vitreoretinal surgery; and (5) hemi-central or central retinal vein occlusion.
Therapeutic Regimen
Patients were randomly assigned to 3 + PRN or 1 + PRN groups using a random numbers table generated by Microsoft Excel (Microsoft, Redmond, WA, USA). Each injection comprised 0.5 mg/0.05 mL ranibizumab (Novartis Pharma AG, Basel, Switzerland). Patients in the 1 + PRN group were treated with one injection of IVR followed by PRN dosing, and patients in the 3 + PRN group were treated with three consecutive monthly injections of IVR followed by PRN dosing. Further IVR injections were only administered if any of the following retreatment criteria were met: macular thickening, intraretinal or subretinal fluid, or an increase in CMT of > 50 μm versus the previous thinnest measurement. Patients were followed up monthly for 12 months after the first dose. Rescue laser treatment of the affected peripheral retinal sector in eyes with retinal neovascularization (NV) was allowed during the follow-up based on FA or SS-OCTA findings according to the doctor’s judgement.
Examinations
The patients’ baseline demographic characteristics and medical history were collected. All patients underwent complete ophthalmic examinations, including measurement of BCVA using the standardized ETDRS refraction protocol, measurement of intraocular pressure (IOP), slit-lamp biomicroscopy, SD-OCT (Spectralis HRA + OCT, Heidelberg Engineering, Heidelberg, Germany), SS-OCTA (PLEX Elite 9000; Carl Zeiss Meditec, Oberkochen, Germany), fundus photography, and wide-field FA (Optos 200Tx imaging system, Optos Plc., Dunfermline, UK). At each follow-up visit, the patients underwent routine ophthalmic examinations, including measurement of BCVA and IOP, slit-lamp biomicroscopy, SD-OCT, and SS-OCTA. Follow-up wide-field FA was performed at 6 and 12 months. Standardized refraction was performed by certified optometrists and BCVA (EDTRS letters) was determined at a distance of 4 m by examiners blinded to the treatment group. Post-mydriatic SD-OCT images were obtained by certified operators. CMT, defined as the average retinal thickness within the 1-mm ETDRS circle centered on the fovea, was measured using built-in software (Spectralis HRA + OCT). Macular ischemia was evaluated on wide-field FA and SS-OCTA, and it was defined as disruption and enlargement of the foveal avascular zone or a remarkable region of capillary non-perfusion located within one disk diameter of the fovea [11]. The resolution of ME was defined as the absence of both intraretinal and subretinal fluid on SD-OCT at 12 months. The macular vascular densities (VDs) of the superficial capillary plexus (SCP) and deep capillary plexus (DCP) were measured on 3 × 3 mm SS-OCTA images using Fiji ImageJ software (http://fiji.sc/Fiji), as previously reported [12]. The SCP was defined as 70% of the thickness between the inner limiting membrane and the outer plexiform layer, and the DCP was defined as extending from the outer boundary of the SCP to 110 μm above the retinal pigment epithelium. Manual adjustments were conducted before analysis if the automatic segmentation was inaccurate; only good-quality SS-OCTA images were used.
Outcomes
The primary outcome measure was the mean change in BCVA from baseline to 12 months in both groups. The secondary outcomes included the mean changes in CMT and VD of the SCP and DCP, the mean number of IVR injections, and the safety profiles in both groups over 12 months.
Statistical Analysis
Continuous variables are presented as the mean ± standard deviation (SD). The sample size was calculated to be 37 in each group at an α error of 5% and power of 80% with an approximate difference of one in the number of IVR injections and an SD of 1.5 in the two groups [9]. Fisher’s exact test was used to compare categorical variables between the 1 + PRN and 3 + PRN groups. The unpaired t-test was used to compare continuous variables, including BCVA and CMT, between the two groups. The paired t-test was used to analyze the longitudinal changes in continuous variables within each group. Univariate and multivariate linear regression analyses with a stepwise variable selection method were performed to determine which baseline factors were significantly associated with the change in BCVA from baseline to 12 months. P < 0.05 was considered to indicate statistical significance. Data analysis was performed using SPSS Statistics (version 21, SPSS, Chicago, IL, USA).
Results
Patients
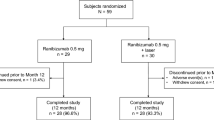
A total of 74 patients were enrolled, of which 37 were randomized to the 3 + PRN regimen and 37 were randomized to the 1 + PRN regimen. The disposition of patients is shown in the Online Supplementary Fig. S1. Overall, 69 patients [93.2%; 35 patients (94.6%) in the 3 + PRN group and 34 patients (91.9%) in the 1 + PRN group, P = 0.64] completed the 12-month visit. At baseline, there were no significant differences between the two groups in terms of patient demographics, systemic diseases, or ocular characteristics (all P > 0.05, Table 1).
Functional Outcomes
There were rapid improvements in BCVA at 1 month in the 3 + PRN and 1 + PRN groups, with further gradual improvements over time (Fig. 1). The change in BCVA from month 1 to month 12 was not significantly different between the two groups (Fig. 1A), irrespective of the macular ischemia status (Fig. 1B,C). The mean change in BCVA from baseline to month 12 was 12.9 ± 10.6 letters in the 3 + PRN group and 14.3 ± 10.6 letters in the 1 + PRN group (P = 0.59, Table 2). At month 12, the final BCVA was 65.3 ± 11.7 letters in the 3 + PRN group and 66.0 ± 12.6 letters in the 1 + PRN group (P = 0.82). The percentage of patients with a BCVA of > 70 letters (Snellen equivalent 20/40) or a BCVA of < 35 letters (Snellen equivalent 20/200) at month 12 were similar in both groups (Table 2). The percentage of patients with a gain in BCVA of ≥ 15 letters at month 12 was 42.9% and 47.1% in 3 + PRN and 1 + PRN groups, respectively (P = 0.78).
Functional outcomes. Changes in the mean BCVA in terms of ETDRS letter scores from baseline through to month 12 in the 3 + PRN (black line) and 1 + PRN (dotted line) groups (a). The mean change in BCVA between baseline and month 12 was 12.9 letters in the 3 + PRN group and 14.3 letters in the 1 + PRN group, and was not significantly different between the two groups. In subgroups of patients with (b) or without (c) macular ischemia, the mean changes in BCVA at months 1–12 from baseline were not significantly different between the 3 + PRN and 1 + PRN groups. Values are mean ± standard error of the mean. BCVA best-corrected visual acuity, ETDRS Early Treatment Diabetic Retinopathy Study, PRN pro re nata
Anatomical Outcomes
The mean CMT decreased dramatically between baseline and month 1, and then decreased gradually thereafter, with similar trends in the 3 + PRN and 1 + PRN groups (Fig. 2A). The mean reduction in CMT between baseline and month 12 was −297.8 ± 187.1 μm in the 3 + PRN group versus −300.2 ± 216.5 μm in the 1 + PRN group (P = 0.96, Table 2). At month 12, the CMT was 260.8 ± 52.2 μm in the 3 + PRN group and 263.0 ± 51.0 μm in the 1 + PRN group (P = 0.86). During the 12-month observation period, the changes in CMT over time were similar in patients with and without macular ischemia, regardless of the treatment regimen (Fig. 2B, C). The percentage of patients with resolution of ME at month 12 was 85.7% and 79.4% in the 3 + PRN and 1 + PRN groups, respectively (P = 0.49). The mean VDs of the SCP and DCP at month 12 were not significantly different between the 3 + PRN and 1 + PRN groups (SCP: P = 0.28; DCP: P = 0.89). Furthermore, the changes in VD between baseline and month 12 were not significantly different between the two groups (SCP: P = 0.99; DCP: P = 0.70).
Anatomical outcomes. Changes in the mean CMT from baseline through to month 12 in the 3 + PRN (black line) and 1 + PRN (dotted line) groups (a). The mean change in CMT from baseline to month 12 was −297.8 μm in the 3 + PRN group and −300.2 μm in the 1 + PRN group, and was not significantly different between the two groups. In subgroups of patients with (b) or without (c) macular ischemia, the mean changes in CMT at months 1–12 from baseline were not significantly different between the 3 + PRN and 1 + PRN groups. Values are mean ± standard error of the mean. CMT central macular thickness, PRN pro re nata
Injection Frequency
Over 12 months, the mean number of ranibizumab injections was 5.0 ± 2.2 in the 3 + PRN group and 4.2 ± 2.4 in the 1 + PRN group (P = 0.17). During the PRN period, additional injections were required in 24 of 35 eyes (68.5%) in the 3 + PRN group and 32 of 34 eyes (94.1%) in the 1 + PRN group. The mean number of additional injections was 2.9 ± 2.0 in the 3 + PRN group and 3.4 ± 2.3 in the 1 + PRN group, and was not significantly different between the two groups (P = 0.38). Overall, 73.5% of patients in the 1 + PRN group received three consecutive monthly injections of IVR, including the first initial dose.
Factors Associated with Change in BCVA from Baseline to Month 12
Table 3 provides the results of univariate and multivariate analyses of factors, including the treatment regimen (3 + PRN or 1 + PRN), that were potentially associated with the primary endpoint; i.e., the change in BCVA from baseline to month 12. Univariate linear regression analysis showed that the duration of symptoms (P = 0.03), baseline BCVA (P < 0.01), and VD of the DCP (P = 0.01) were significantly correlated with the change in BCVA from baseline to month 12. However, in the multivariate regression, only the baseline BCVA was independently and significantly associated with the change in BCVA from baseline to month 12 (P < 0.01).
Safety
Retinal NV was reported in two eyes (5.7%) in the 3 + PRN group and in three eyes (8.8%) in the 1 + PRN group, of which one (2.9%) developed mild vitreous hemorrhage, which resolved gradually after scatter retinal photocoagulation and IVR. The incidence of retinal NV was similar in both groups (P = 0.67). The mean duration until the development of NV was 6.6 ± 4.2 months from the initial visit and 3.6 ± 2.7 months from the last ranibizumab injection. These patients received 4.0 ± 1.0 IVR injections through to month 12, which was not significantly different compared with the number of injections (4.7 ± 2.3) in patients without retinal NV (P = 0.53). During the study period, the incidence of ocular adverse events was similar in both groups (Online Supplementary Table S1), and there were no serious non-ocular adverse events.
Discussion
In this prospective randomized study of patients with BRVO, we found that the 1 + PRN regimen and 3 + PRN regimen using IVR improved visual acuity effectively and safely during the 12-month study period. Furthermore, the macular perfusion was preserved at 12 months in eyes with BRVO treated with either regimen.
The mean change in BCVA was comparable between the 3 + PRN and 1 + PRN groups (12.9 versus 14.3 letters, respectively). Overall, 42.9% and 47.1% of patients in the 3 + PRN and 1 + PRN groups, respectively, showed a gain in BCVA of ≥ 15 letters at 12 months. These results may appear inferior to those of the BRAVO and BLOSSOM studies using ranibizumab [3, 13]. In the BRAVO study, patients treated with a 6 + PRN regimen showed an average gain of 18.3 letters and 60.3% had a gain of ≥ 15 letters [3]. In patients treated with a 3 + PRN regimen in the BLOSSOM study, the mean BCVA gain was 16.4 letters, and the proportion of eyes gaining ≥ 15 letters was 55.6% [13]. The differences in BCVA gain among these studies may be explained at least partly by the greater number of injections (7–9) administered to patients enrolled in those RCTs [3, 13]. Furthermore, the variations in inclusion criteria and retreatment criteria among the studies may also contribute to the differing results [3, 13]. We found that the 3 + PRN and 1 + PRN regimens significantly improved morphological parameters determined by OCT in patients with BRVO, without significant differences in the final CMT or the improvement in CMT between the two groups. Miwa et al. reported that the CMT at 12 months in the 3 + PRN group (286.1 μm) was significantly thinner than that in the 1 + PRN group (337.0 μm), but the changes in CMT from baseline to month 12 were not significantly different between the 3 + PRN (−206.9 μm) and 1 + PRN (−170.5 μm) regimens [9]. The reduction in CMT in our study (approximately −300 μm) was greater than that reported by Miwa et al. [9], which might be explained by our higher baseline CMT.
Ito et al. reported that the 1 + PRN regimen could be safer and less invasive owing to a lower number of bevacizumab injections (2.1 ± 0.8) compared with the 3 + PRN regimen (4.3 ± 1.4), while matching the improvements in vision achieved by bevacizumab [14]. In contrast, Miwa et al. found that the mean number of IVR injections was not significantly different between the 1 + PRN (3.8 ± 1.8) and 3 + PRN (4.6 ± 1.4) groups [9]. Similarly, in the present study, the number of IVR injections in the 1 + PRN group (4.2 ± 2.4) was not significantly less than that in the 3 + PRN group (5.0 ± 2.2). Surprisingly, most of the patients (73.5%) in the 1 + PRN group received three consecutive monthly injections of IVR in the first 3 months under the same retreatment criteria as the 3 + PRN group. Because the functional and anatomical outcomes and the treatment burden at 12 months were similar for both regimens, three loading doses may be preferable as an intensive treatment regimen in terms of improving and stabilizing BCVA.
To date, few studies have compared the microvascular changes assessed using SS-OCTA between single injections versus monthly injections of ranibizumab for the treatment of ME secondary to BRVO. Sellam et al. reported slight, although not statistically significant, decreases in the VDs of the SCP and DCP in patients with retinal vein occlusion treated with intravitreal injections of anti-VEGF drugs during a mean follow-up period of 19 weeks [15]. More recently, using projection-resolved OCTA, Tsuboi et al. reported that the VDs of the SCP and DCP in eyes with BRVO treated with a 1 + PRN regimen remained unchanged over a 12-month follow-up period [16]. One highlight of our study is that we used SS-OCTA to compare the microvascular changes in eyes treated with different dosing regimens. We detected no significant differences in the VD changes in the SCP and DCP from baseline to month 12 between the 1 + PRN and 3 + PRN regimens, confirming that anti-VEGF therapy in 1 + PRN or 3 + PRN regimens helps maintain macular capillary perfusion in eyes with BRVO.
Furthermore, we investigated the impact of several baseline characteristics, including the SS-OCTA parameters, on the visual outcomes after anti-VEGF therapy. Most of the variables, including CMT measured using SD-OCT, VDs measured using SS-OCTA, macular ischemia classification, number of IVR injections, and the treatment regimen (3 + PRN or 1 + PRN), were not associated with the gain in BCVA at 12 months. However, worse visual function at baseline was strongly associated with a greater gain in vision after treatment for BRVO. This finding is consistent with the results of previous retrospective studies by Sakanishi et al. [17] and Khayat et al. [18], indicating that baseline BCVA is a good prognostic factor for visual improvement after anti-VEGF treatment in patients with BRVO.
Previous studies have reported that 20% of patients with BRVO developed retinal NV in the natural course of the disorder, of which 60–90% developed vitreous bleeding [19, 20]. The landmark Branch Vein Occlusion Study (BVOS) study revealed that, although sectoral retinal photocoagulation for patients with ischemic BRVO failed to prevent NV development, it significantly reduced the risk of vitreous hemorrhage [21]. In our study, anti-VEGF treatment did not prevent the development of retinal NV in either group. Retinal NV was detected in 7.2% of eyes with BRVO during the 12-month follow-up, which appears to be lower than that reported in BVOS (15%) [21]. Scatter photocoagulation reduced the risk of vitreous hemorrhage and did not affect treatment burden in patients with BRVO who received ongoing anti-VEGF therapy. A recent study revealed that the BRVO eyes with resolved ME, which meant the last anti-VEGF injections were within 6 months from the baseline, had more NV at the 1-year visit [22]. Consistently, three eyes (60.0%) of the five eyes with NV were classified as resolved ME in our study according to their classification criteria [22]. Therefore, retinal NV and NV-associated complications should be carefully monitored, even in eyes with resolved ME, after anti-VEGF therapy using the 3 + PRN and 1 + PRN regimen.
This study had several limitations. This was a single-center study and was not double masked. Furthermore, it is unknown whether BCVA, CMT, or macular capillary perfusion remain stable over a follow-up period longer than that of the current study (12 months). Larger longitudinal studies are needed in the future to confirm our results.
Conclusion
Our prospective randomized study has shown that the 3 + PRN and 1 + PRN regimens effectively reduced macular thickness, improved BCVA, and preserved macular perfusion as determined by SS-OCTA. The 3 + PRN regimen may be preferable as an intensive treatment regimen in terms of improving and stabilizing BCVA.
References
Mitry D, Bunce C, Charteris D. Anti-vascular endothelial growth factor for macular edema secondary to branch retinal vein occlusion. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD009510.pub2.
Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010;117(1102–12): e1.
Brown DM, Campochiaro PA, Bhisitkul RB, et al. Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology. 2011;118:1594–602.
Tadayoni R, Waldstein SM, Boscia F, et al. Individualized stabilization criteria-driven ranibizumab versus laser in branch retinal vein occlusion: six-month results of brighter. Ophthalmology. 2016;123:1332–44.
Brynskov T, Kemp H, Sorensen TL. Intravitreal ranibizumab for retinal vein occlusion through 1 year in clinical practice. Retina. 2014;34:1637–43.
Mansour AM, Shahin M, Kofoed PK, et al. Insight into 144 patients with ocular vascular events during VEGF antagonist injections. Clin Ophthalmol. 2012;6:343–63.
Falavarjani KG, Nguyen QD. Adverse events and complications associated with intravitreal injection of anti-VEGF agents: a review of literature. Eye (Lond). 2013;27:787–94.
Narayanan R, Panchal B, Das T, et al. A randomized, double-masked, controlled study of the efficacy and safety of intravitreal bevacizumab versus ranibizumab in the treatment of macular edema due to branch retinal vein occlusion: MARVEL Report No. 1. Br J Ophthalmol. 2015;99:954–9.
Miwa Y, Muraoka Y, Osaka R, et al. Ranibizumab for macular edema after branch retinal vein occlusion: one initial injection versus three monthly injections. Retina. 2017;37:702–9.
Bayat AH, Cakir A, Ozturan SG, et al. Comparison of one and three initial monthly intravitreal ranibizumab injection in patients with macular edema secondary to branch retinal vein occlusion. Int J Ophthalmol. 2018;11:1534–8.
Park DG, Jeong WJ, Park JM, et al. Prospective trial of treat-and-extend regimen with aflibercept for branch retinal vein occlusion: 1-year results of the PLATON trial. Graefes Arch Clin Exp Ophthalmol. 2021;259:2879–86.
Su L, Ji YS, Tong N, et al. Quantitative assessment of the retinal microvasculature and choriocapillaris in myopic patients using swept-source optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol. 2020;258:1173–80.
Wei W, Weisberger A, Zhu L, et al. Efficacy and safety of ranibizumab in Asian patients with branch retinal vein occlusion: results from the randomized BLOSSOM study. Ophthalmol Retina. 2020;4:57–66.
Ito Y, Saishin Y, Sawada O, et al. Comparison of single injection and three monthly injections of intravitreal bevacizumab for macular edema associated with branch retinal vein occlusion. Clin Ophthalmol. 2015;9:175–80.
Sellam A, Glacet-Bernard A, Coscas F, et al. Qualitative and quantitative follow-up using optical coherence tomography angiography of retinal vein occlusion treated with anti-VEGF: optical coherence tomography angiography follow-up of retinal vein occlusion. Retina. 2017;37:1176–84.
Tsuboi K, Kamei M. Longitudinal vasculature changes in branch retinal vein occlusion with projection-resolved optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol. 2019;257:1831–40.
Sakanishi Y, Lee A, Usui-Ouchi A, et al. Twelve-month outcomes in patients with retinal vein occlusion treated with low-frequency intravitreal ranibizumab. Clin Ophthalmol. 2016;10:1161–5.
Khayat M, Wright DM, Yeong J, et al. Impact of retinal ischemia on functional and anatomical outcomes after anti-vascular endothelial growth factor therapy in patients with retinal vein occlusion. Retina. 2020;40:1098–109.
Zegarra H, Gutman FA, Conforto J. The natural course of central retinal vein occlusion. Ophthalmology. 1979;86:1931–42.
Hayreh SS, Rubenstein L, Podhajsky P. Argon laser scatter photocoagulation in treatment of branch retinal vein occlusion A prospective clinical trial. Ophthalmologica. 1993;206:1–14.
Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. A randomized clinical trial. Branch Vein Occlusion Study Group. Arch Ophthalmol. 1986;104:34–41.
Takatsu H, Tsuboi K, Wakabayashi T, et al. Vascular abnormalities may progress in branch vein occlusion despite resolution of macular edema. Ophthalmol Retina. 2022;6:252–4.
Acknowledgements
The authors would like to thank all of the patients who participated in this study.
Funding
This work was supported by Novartis Pharma AG, the National Natural Science Foundation of China (82101150, 82171078, 81870670), Shanghai clinical three-year action plan-major clinical research (SHDC2020CR2041B, SHDC2020CR5014-003), the Shanghai Sailing Program (21YF1405300), and the Shanghai Committee of Science and Technology (20Y11911100, 18411965100). The journal’s Rapid Service Fee was also covered by the funding.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Wenyi Tang: acquisition, analysis and interpretation of data; Jingli Guo: acquisition, analysis and interpretation of data; Gezhi Xu: conception and design of the work; Wei Liu: conception and design of the work, manuscript preparation; Qing Chang: conception and design of the work, manuscript revision. All authors read and approved the final manuscript.
Disclosures
Wenyi Tang, Jingli Guo, Gezhi Xu, Wei Liu and Qing Chang have nothing to disclose.
Compliance with Ethics Guidelines
This study was approved by the Ethics Committee of the Eye and ENT Hospital of Fudan University (No. 2018037-1) and conducted in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from every participant.
Data Availability
All data will be made available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tang, W., Guo, J., Xu, G. et al. Three Monthly Injections Versus One Initial Injection of Ranibizumab for the Treatment of Macular Edema Secondary to Branch Retinal Vein Occlusion: 12-Month Results of a Prospective Randomized Study. Ophthalmol Ther 11, 2309–2320 (2022). https://doi.org/10.1007/s40123-022-00588-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00588-7