Abstract
Introduction
To investigate the efficacy of autologous serum gel in patients with lagophthalmos combined with neurotrophic persistent corneal epithelial defects (PEDs).
Methods
This is retrospective, case-series study enrolled 15 patients with lagophthalmos complicated by neurotrophic PEDs refractory to medical treatment including autologous serum eye drops. They were treated with autologous serum gel in conjunction with conservative treatment. The following information was collected from medical records: demographics, underlying diseases, and past ocular history. PEDs healing time was evaluated with visual acuity, visual analog scale (VAS) scores, esthesiometer scores, and the areas of the epithelial defects.
Results
Six men and nine women with a mean age of 63.3 ± 9.9 years were included. The most common cause of the neurotrophic PEDs and lagophthalmos in this group was postherpetic infection (46.7%) and cerebral hemorrhage (26.7%) each. Two months following treatment with autologous serum gel, there was a reduction in the area of the epithelial defects (from 19.2 ± 9.9 to 0.6 ± 1.5 mm2) and a significant improvement in best-corrected visual acuity (BCVA) (from 0.8 ± 0.5 to 0.5 ± 0.4 logMAR) and VAS scores (from 5.1 ± 1.1 to 2.1 ± 0.6) in 13 eyes (87%). Among the 11 completely healed eyes, the mean epithelial healing time was 3.2 ± 1.8 weeks.
Conclusions
Autologous serum gel reduces symptoms and promotes corneal epithelialization of refractory neurotrophic PEDs in patients with lagophthalmos. Therefore, it may be well tolerated and a beneficial addition in the management of neurotrophic PEDs in patients with lagophthalmos.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Refractory lagophthalmic persistent corneal epithelial defects (PEDs) complicated with a neurotrophic component are challenging, so we attempted to treat them by applying gel-type autologous serum rather than liquid type which has never been tried. |
We hypothesized that autologous serum gel could protect the ocular surface of lagophthalmos with a more sufficient surface retention time than liquid type. |
What was learned from the study? |
Autologous serum gel had effects on lagophthalmic PEDs and it had some advantages over autologous serum eye drops. |
We could broaden the application of autologous serum in various ocular diseases by using a gel-type treatment. |
Introduction
Persistent corneal epithelial defects (PEDs) are defined as corneal defects that do not improve after 2 weeks of conventional treatment regardless of the cause. They can have serious consequences on eye health, including infection, scarring, melting, and even perforation when healing is delayed [1]. They are known to usually be resistant to healing with standard therapy such as frequent preservative-free artificial tears, ointments or gels, press patching, punctal plugging, and therapeutic contact lens wear. Several favorable results have been reported in PEDs associated with the use of autologous serum eye drops, insulin eye drops, amniotic membrane extract eye drops, epidermal growth factor (EGF) ointment, and recently developed topical recombinant human nerve growth factor (Cenegermin) [1,2,3,4,5,6,7]. However, PEDs that do not respond to even these drops need more aggressive methods to restore ocular surface health.
PEDs in patients with lagophthalmos tend to be refractory to conventional treatment [8]. Lagophthalmos is usually caused by the dysfunction of facial nerves and can induce an exposure keratopathy that aggravates the course of PEDs [9]. PEDs in lagophthalmos usually undergo a chronic course, with a high recurrence rate for epithelial defects. Hence, conventional medical treatment alone might be insufficient, and surgical interventions are eventually needed to heal those epithelial defects [10]. Furthermore, when the underlying etiology of PEDs is neurotrophic and those severity is more than stage II by Mackie classification, they are more complicated to treat even with the support of surgical treatment. But, patients who have concerns about quality of life or cosmetic problems or who have already given up on the eye lesions might be hesitant to consider surgical options, such as tarsorrhaphy, conjunctival flap, or keratoplasty, or might even outright refuse therapy. Thus, neurotrophic PEDs combined with lagophthalmos are challenging to treat. As for PEDs due to other causes, before offering surgical interventions, medical treatment with the specific aforementioned eye drops might be a valid option [11].
Autologous serum eye drops were introduced decades ago and known to contain several substances that aid in the regeneration of the keratoconjunctival epithelium, and many reports show their positive effects on neurotrophic PEDs [1,2,3,4]. Ointments or gels—though accompanied by concomitant visual blurring—are preferred modalities as conservative treatments for exposure keratopathy in lagophthalmos because of the increased contact time with the cornea [12]. Thus, to achieve both epithelial healing enhancement in neurotrophic PEDs and protection from damage by lagophthalmos, a gel-type autologous serum would satisfy those demands. To the best of our knowledge, no study has introduced a gel-type autologous serum rather than liquid type and evaluated the outcomes of its clinical use. Thus, we aimed to develop an autologous serum gel by mixing autologous serum eye drops with a soothing eye gel.
We hypothesized that an autologous serum gel with sufficient surface retention time may benefit patients with neurotrophic PEDs in lagophthalmos who prefer conservative medical therapy. In this study, we investigated the safety and efficacy of this autologous serum gel on neurotrophic PEDs combined with lagophthalmos.
Methods
Patients
This study was approved by the Institutional Review Board (IRB) of Ulsan University Hospital (IRB no. 2022-04-034-001) and was performed in accordance with the tenets of the Declaration of Helsinki and its later amendments. After obtaining IRB approval, we performed a retrospective chart review of all patients who suffered from lagophthalmos and were diagnosed with neurotrophic PEDs from September 2019 to December 2021. A total of 15 eyes of 15 patients were recruited for this study. According to the dynamic function test of orbicularis oculi and frontalis, all patients had lagophthalmos on blink ≥ 5 mm, on gentle closure ≥ 5 mm, and on forced closure ≥ 2 mm [13]. PED diagnoses were confirmed by slit-lamp microscopy with fluorescein staining. We defined PEDs as follows: the size of the epithelial defect either decreased minimally or did not decrease at all despite appropriate conventional treatment such as lubricating eye drops and ointment, punctal plugging, and therapeutic soft contact lenses or pressure patching for over 2 weeks.
All patients with lagophthalmos had neurotrophic PEDs refractory to medical treatment including autologous serum eye drops and were subsequently treated with the autologous serum gel. Before enrollment, informed consent was obtained from each patient after the current hypothesis was explained regarding the application of the autologous serum gel and potential complications such as infections.
Patients who underwent surgical procedures for corneal diseases or discontinued autologous serum gel treatment as a result of side effects such as severe ocular discomfort or allergic keratoconjunctivitis were excluded from the study.
Treatment Agents
A total of 10 ml of blood was obtained by venipuncture in blood collection tubes (BD Vacutainer®, Becton, Dickinson and Company, Franklin Lakes, NJ, USA). Each blood collection tube was centrifuged for 20 min at 3800 rpm, and 2.5 ml of 100% serum was carefully separated and taken up into a 10-ml syringe via a sterile method. Ten grams of lubricating eye gel mainly consisting of carbomer was transferred into a 30-ml syringe. With both syringes connected by a three-way stopcock, the total amount of serum in the 10-ml syringe was pushed into the eye gel in the 30-ml syringe, and the plunger was pulled back to draw 10 ml of the mixture. The push and return cycles were repeated over 10 times to finally obtain a 20% autologous serum gel (Fig. 1). The mixed gel was transferred into a sterile eye drop bottle that was wrapped in aluminum foil to prevent vitamin A degradation. We had chemist consultation on the mixture by this method and confirmed the uniform distribution of the ingredients in the mixture and no other pharmacological changes.
Preparation of autologous serum gel. a The serum was prepared using centrifuged whole blood. b Serum (100%, 2.5 ml) was transferred to a 10-ml syringe and a lubrication eye gel (10 g) was transferred to a 30-ml syringe. c Mixed by push and return more than 10 times through the three-way stopcock. d Autologous serum gel (20%) in a sterile eye drop bottle
After the diagnosis of neurotrophic PEDs in patients with lagophthalmos, all patients stop using autologous serum eye drops and started to use preservative-free sodium hyaluronate 0.18% freely and levofloxacin 0.5% three times a day as conventional therapy. In addition, the autologous serum gel was applied to the ocular surface and the lower conjunctival fornix six times a day in the eyes of the patients undergoing conventional therapy. All topical ointments or gels other than the autologous serum gel were discontinued after the initiation of the autologous serum gel. All topical medications were discontinued with the resolution of the corneal lesions except preservative-free sodium hyaluronate 0.18% and lubrication ointment or gel, which were instilled continuously three or four times daily afterward in patients.
Evaluation
The following information was collected from medical records: demographics, past ocular history, and underlying diseases for neurotrophic PEDs and lagophthalmos. BCVA, VAS score, and corneal sensation were assessed, and slit-lamp examination on cornea with fluorescein staining and photography were performed before autologous serum gel treatment and at 2-week intervals afterward for 2 months.
Corneal sensation measured with an esthesiometer (Cochet-Bonne esthesiometer®, Luneau Ophthalmology, Chartres Cedex, France) was obtained in the central, superior, inferior, nasal, and temporal areas of the cornea, and the mean of the measurements was recorded as the corneal sensitivity reading for that eye. Corneal sensitivity measurements of less than 45 mm were regarded as low in this study.
The size of the corneal epithelial defects was calculated using image analysis software (i-Solution®, IMT i-Solution Inc., Vancouver, BC, Canada) after photography of the fluorescein dye-stained cornea was taken. Treatment was considered to result in complete healing if complete epithelial healing was achieved and partial healing if the epithelial healing was inadequate but decreased defect sizes compared to the baseline without signs of worsening within the study period.
Statistical Analysis
SPSS Statistics for Windows, version 18.0 (IBM Corp., Armonk, NY, USA) was used for analysis. The Wilcoxon signed-rank test was used for the comparison in changes of variables before and after treatment. A p value less than 0.05 was considered statistically significant.
Results
Six men and nine women with a mean age of 63.3 ± 9.9 years (range 47–78 years) at the time of the autologous serum gel use were included. Neurotrophic corneal lesions were all above grade II in the Mackie classification. Four (26.7%) patients had hypertension, three (20.0%) patients had diabetes mellitus, and one (6.7%) patient had hyperthyroidism. All 15 patients exhibited monocular involvement. The BCVA (logMAR) was 0.9 ± 0.6, the VAS score was 5.3 ± 1.2, the corneal sensation was 11.0 ± 5.4 mm, and the area of the epithelial defects was 18.5 ± 9.3 mm2 at the time of diagnosis of the neurotrophic PEDs (Table 1). The causative conditions of the neurotrophic PEDs varied from postherpetic infection in seven eyes (46.7%); postneurosurgical procedures for trigeminal neuralgia and trauma in two eyes (13.3%) each; tumors—namely, Schwannoma of the trigeminal nerve and acoustic neuroma—in two eyes (13.3%) each; diabetic neurotrophic keratitis in one eye (13.3%); long-term use of anti-glaucoma eye drops (timolol®) in one eye (6.7%); and contact lens wear in one eye (6.7%). The cause of lagophthalmos varied from cerebral hemorrhage in four patients (27.0%); Bell’s palsy in three patients (20.0%); tumors—namely, Schwannoma involving the facial nerve, adenoid cystic carcinoma in the parotid gland, and acoustic neuroma—in three patients (20.0%) each; neurosurgery for meningioma and skull base infection in two patients (13.3%) each; posttraumatic cicatrization of the upper eyelid in two patients (13.3%), and thyroid eye disease in one patient (6.7%) (Table 2).
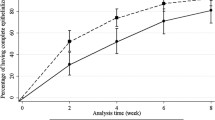
At 1 and 2 months post treatment with the autologous serum gel, 13 eyes showed improvement or were completely healed. In those 13 eyes, at 1 and 2 months after treatment, the BCVA was improved from 0.8 ± 0.5 logMAR to 0.7 ± 0.5 logMAR (p = 0.027) and 0.5 ± 0.4 logMAR (p = 0.001), VAS score was decreased from 5.1 ± 1.1 to 4.9 ± 1.0 (p = 0.046) and 2.1 ± 0.6 (p = 0.001), corneal sensation was improved from 11.5 ± 5.6 to 11.9 ± 6.3 (p = 0.317) and 13.5 ± 7.1 (p = 0.059), and the area of epithelial defects was decreased from 19.2 ± 9.9 mm2 to 3.5 ± 7.0 mm2 (p = 0.002) and 0.6 ± 1.5 mm2 (p = 0.001), respectively (Fig. 2). All clinical features except corneal sensation were significantly improved. Corneal epithelial defects were completely healed in 11 eyes (73.3%). Among these individuals, the edema of the corneal epithelium and stroma improved within 2 months after treatment, and the mean duration of complete epithelial healing was 3.2 ± 1.8 weeks. Two eyes (13.0%) showed partial improvement with a decrease in corneal epithelial defect size and partial decrease in corneal edema. Two eyes (13%) showed no response to the autologous serum gel, including no improvement in BCVA, VAS score, and no decrease in the area of the corneal epithelial defect, until 2 months after treatment (Table 3).
Visual acuity, visual analog scale (VAS) score, corneal sensation, and the area of the epithelial defects before and after 1 and 2 months of treatment for neurotrophic persistent epithelial corneal defects with autologous serum gel in patients with lagophthalmos. a Visual acuity (logMAR). b VAS score. c. Esthesiometer score (mm). d Area of the epithelial defect (mm2). *Significant difference between groups (p < 0.05, Wilcoxon-signed ranks test), logMAR = logarithm of minimum angle of resolution
Case (Patient No. 9)
This case involved a woman in her sixties who suffered paralytic lagophthalmos and neurotrophic keratitis in her left eye for 3 months due to an intracranial trigeminal Schwannoma involving the facial nerve. She exhibited paralytic lagophthalmos with lower eyelid retraction and PEDs with stromal edema and conjunctival injection in the left eye. On her first visit, her visual acuity was 1.5 logMAR and corneal sensation was less than 10 mm. She did not complain except for mild eye injection and discomfort even with large PEDs. She had previously used topical levofloxacin 0.5%, topical sodium hyaluronate 0.18%, lubricant ointment, and autologous serum eye drops. Therapeutic contact lens was tried, but was spontaneously lost within 2 days. The area of the epithelial defects was 42 mm2, and corneal edema persisted near the center for at least 2 weeks without any improvement. The patient was recommended to have surgery such as amniotic membrane transplantation or tarsorrhaphy. However, the patient refused surgery and wanted only medical treatment. Therefore, the patient was instructed to hold autologous serum eye drops and apply the autologous serum gel six times a day in conjunction with conventional treatment except for lubricant ointment. There was no adverse drug reaction. The lesion had improved after 2 weeks of treatment, and the corneal epithelial defects were completely healed with stromal haziness after 4 weeks of treatment (Fig. 3).
External photographs of left lagophthalmos and slit-lamp examination of persistent corneal epithelial defects. a The patient has a left lagophthalmos and a lower lid retraction. b Before autologous serum gel treatment, the epithelial defect stained with fluorescein was seen in the central cornea with stromal edema. c Two weeks after autologous serum treatment, the epithelial defect had decreased. d Four weeks after autologous serum treatment, the epithelial defect was healed with stromal haziness
Discussion
In this study, we investigated the efficacy of autologous serum gel on neurotrophic PEDs in patients with lagophthalmos. We selected a concentration of 20% of the autologous serum gel because higher concentrations of some cytokines in autologous serums may provoke inflammation or suppress wound healing [14]. Although there was no control in this study, the healing of epithelial defects was achieved within 2–8 weeks after use of autologous serum gel, with an average of 110 days’ delay in healing with autologous serum eye drops in neurotrophic PEDs with lagophthalmos.
There were many reports on treatment of neurotrophic PEDs with autologous serum eye drops [15]. Matsumoto et al. reported that neurotrophic PEDs without lagophthalmos healed completely in 14 eyes within 6–32 days after treatment with autologous serum eye drops [16]. In our study with neurotrophic PEDs with lagophthalmos which were refractory to autologous serum eye drops in most cases, epithelial healing time was 3.2 weeks on average. Report on treating neurotrophic PEDs with lagophthalmos is relatively rare and usually about surgical interventions because such PEDs are commonly refractory to medical treatment and result in progression of corneal ulcer or corneal perforation. We accessed four clinical features to evaluate the outcomes of treatment with autologous serum gel in this study. All clinical features except corneal sensation, i.e., epithelial defects, VAS, and BCVA, were significantly improved. To achieve epithelial healing in lagophthalmos with autologous serum eye drops, the ocular surface must be frequently wet with trophic components of autologous serum eye drops by blinking. In lagophthalmos which lacks frequent blinking, there must be a limitation of autologous serum as liquid-type eye drops. Combination of serum eye drops with hydrogel bandage contact lenses was tried to keep humidity over the ocular surface and prevent mechanical stress [17]. But, it is difficult to keep bandage contact lenses on because of the high spontaneous loss rate in lagophthalmos. In a preliminary study, we compared the precorneal retention times of four different eye drops in healthy subjects using ultrahigh-resolution anterior segment spectral-domain optical coherence tomography (OCT). These eye drops comprised preservative-free sodium hyaluronate 0.18%, autologous serum eye drops, autologous serum gel, and lubricating eye gel [18]. Central tear film thickness was measured before instillation and then after 10, 20, 40, and 60 min. The autologous serum gel was retained on the ocular surface until 40 min after instillation in healthy subjects with normal washout by lacrimal secretion. The ocular retention time might be prolonged in patients with decreased lacrimal secretion such as neurotrophic keratopathy. So we recommended the patients to use autologous serum gel 6–8 times a day in our study. We could keep the ocular surface moist along with continuously supplying trophic components of the autologous serum gel. We found that combined use of autologous serum eye drops and lubricating eye gel is quite different from use of autologous serum gel.
Results regarding the corneal sensation recovery after treating with autologous serum eye drops in neurotrophic keratitis are known to vary among studies. In our study, corneal sensation was not improved significantly, but tends to improve with treatment.
We also noted that autologous serum gel treatment was associated with improved BCVA. If PEDs are treated more rapidly, increased corneal surface regularity with decreased intensity of corneal scarring would have likely contributed to the increase in visual acuity.
As we used soothing eye gel containing benzalkonium chloride (BAK), we had to check the toxicity of the autologous serum gel. BAK concentration in the final autologous serum gel is estimated to be 0.00048%, which is effective against Escherichia coli and Staphylococcus aureus but not Pseudomonas aeruginosa [19]. So patients were instructed to keep using antibiotic eye drops and to store the serum gel bottle in a cool place [20]. On the first day of autologous serum application and every week of use before discarding the serum gel bottle, we examined the remaining serum gel for microbial growth with routine bacterial cultures and smears. We confirmed the absence of microbial growth in all patients’ bottles cultures. BAK with a concentration of 0.0005% showed no toxicity toward human corneal epithelial cells (HCEs) and conjunctival cells in vitro [21]. In vitro experiments on HCEs and conjunctival epithelium with BAK showed minimal reduction in migratory ability at 0.0005% BAK. In a migration assay, the same results were observed with a mixture of 20% autologous serum and 0.002% BAK as without BAK [21]. In our study, BAK-related toxic keratitis was not observed in any patient during the study period. But long-term follow-up is needed.
Thus, autologous serum gel might have the advantages of a lower risk of infection, convenient transport or storage in a cool place, and requires less frequent use than serum eye drops for efficacy.
This study has several limitations. The sample size is too small, and there could be many confounding factors. The first is that the study design is a case series and lacks a comparison group; therefore, the study has low interval validity. The second limitation is the small sample size, which means that this patient population may not be truly representative of patients with lagophthalmos combined with neurotrophic PEDs. Additionally, the observation might be a statistical artifact generated from the small sample size. Future studies should be conducted by comparing the intervention group with a control group and employing a large sample size and various other causative conditions for PEDs to properly determine the treatment effect.
Conclusions
Autologous serum gel prompted corneal epithelial healing, improved visual acuity, and mitigated ocular symptoms in patients with lagophthalmos complicated by refractory neurotrophic PEDs. These findings indicate that autologous serum gel is potentially beneficial in the management of neurotrophic PEDs in patients with lagophthalmos.
References
Jeng BH, Dupps WJ Jr. Autologous serum 50% eyedrops in the treatment of persistent corneal epithelial defects. Cornea. 2009;28:1104–8.
Tsubota K, Goto E, Shimmura S, Shimazaki J. Treatment of persistent corneal epithelial defect by autologous serum application. Ophthalmology. 1999;106:1984–9.
Poon AC, Geerling G, Dart JK, Fraenkel GE, Daniels JT. Autologous serum eyedrops for dry eyes and epithelial defects: clinical and in vitro toxicity studies. Br J Ophalmol. 2001;85:1188–97.
Diaz-Valle D, Burgos-Blasco B, Rego-Lorca D, et al. Comparison of the efficacy of topical insulin with autologous serum eye drops in persistent epithelial defects of the cornea. Acta Opthalmol. 2021. https://doi.org/10.1111/aos.14997.
Perez ML, Barreales S, Sabater-Cruz N, Martinez-Conesa EM, Vilarrodona A, Casaroli-Marano RP. Amniotic membrane extract eye drops: a new approach to severe ocular surface pathologies. Cell Tissue Bank. 2021. https://doi.org/10.1007/s10561-021-09962-4.
Moon HS, Li L, Yoon HJ, Ji YS, Yoon KC. Effect of epidermal growth factor ointment on persistent epithelial defects of the cornea. BMC Ophthalmol. 2020;20:147.
Pflugfelder SC, Massaro-Giordano M, Perez VL, et al. Topical recombinant human nerve growth factor (Cenegermin) for neurotrophic keratopathy: a multicenter randomized vehicle-controlled pivotal trial. Ophthalmology. 2020;127:14–26.
Portelinha J, Passarinho MP, Costa JM. Neuro-ophthalmological approach to facial nerve palsy. Saudi J Ophthalmol. 2015;29:39–47.
Sohrab M, Abugo U, Grant M, Merbs S. Management of the eye in facial paralysis. Facial Plast Surg. 2015;31:140–4.
Wolkow N, Chodosh J, Freitag SK. Innovations in treatment of lagophthalmos and exposure keratopathy. Int Ophthalmol Clin. 2017;57:85–103.
Pocobelli A, Komaiha C, Carlo LD, Pocobelli G, Boni N, Gisoli RAMC. Role of topical cenegermin in management of a cornea transplant in a functionally monocular patient with neurotrophic keratitis and facial nerve palsy: a case report. Int Med Case Rep J. 2020;13:617–21.
Jeng BH. Treating the nonhealing epithelial defect: an overview of standard and investigational therapies for persistent corneal epithelial defects. CRSTEurope. 2011;9:25–8.
Malhotra R, Ziahosseini K, Litwin A, Nduka C. CADS grading scale: towards better grading of ophthalmic involvement in facial nerve paralysis. Br J Ophthalmol. 2016;100:866–70.
Cho YK, Huang W, Kim GY, Lim BU. Comparison of autologous serum eye drops with different diluents. Curr Eye Res. 2013;38:9–17.
Shtein RM, Shen JF, Kuo AN, Hammersmith KM, Li JY, Weikert MP. Autologous serum-based eye drops for treatment of ocular surface disease. Ophthalmology. 2020;127:128–33.
Matsumoto Y, Dogru M, Goto E, et al. Autologous serum application in the treatment of neurotrophic keratopathy. Ophthalmology. 2004;111:1115–20.
Schrader S, Wedel T, Moll R, Geerling G. Combination of serum eye drops with hydrogel bandage contact lenses in the treatment of persistent epithelial defects. Graefes Arch Clin Exp Ophthalmol. 2006;244:1345–9.
Gagliano C, Papa V, Amato R, Malaguarnera G, Avitabile T. Measurement of the retention time of different opthalmic formulations with ultrahigh-resolution optical coherence tomography. Curr Eye Res. 2018;434:499–502.
Iwasawa A, Ayaki M, Niwano Y. Cell viability score (CVS) as a good indicator of critical concentration of benzalkonium chloride for toxicity in cultured ocular surface cell lines. Regul Toxicol Pharmacol. 2013;66:177–83.
Cassano R, Di Gioia ML, Trombino S. Gel-based materials for ophthalmic drug delivery. Gels. 2021;7:130.
Moon J, Ko JH, Yoon CH, Kim MK, Oh JY. Effects of 20% human serum on corneal epithelial toxicity induced by benzalkonium chloride: in vitro and clinical studies. Cornea. 2018;5:617–23.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study or publication of this article. The journal’s Rapid Service Fee was funded by the authors.
Author Contributions
Hyeong Ju Kim performed data acquisition and analysis as well as drafting of the manuscript. Hyun Chul Youn and Jeong Jae Hyun were involved in data analysis. Sang Woo Kim contributed to the conception of the work and revised the manuscript. All authors reviewed and approved the final manuscript.
Disclosures
All named authors declare that they have no competing interests.
Compliance with Ethics Guidelines
This study adhered the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Ulsan University Hospital (IRB approval number 2022-04-034-001). Written informed consent was obtained from each patient prior to enrollment. Written consent to publish this study has been obtained.
Data Availability
The datasets supporting the conclusions of this article are included within the article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kim, H.J., Youn, H.C., Hyun, J.J. et al. Efficacy of Autologous Serum Gel in Neurotrophic Persistent Corneal Epithelial Defects Combined with Lagophthalmos. Ophthalmol Ther 11, 2129–2139 (2022). https://doi.org/10.1007/s40123-022-00575-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00575-y