Abstract
Introduction
This study assessed retinal nonperfusion area (NPA) changes after anti-VEGF treatment in proliferative diabetic retinopathy (PDR) eyes using swept-source widefield optical coherence tomography angiography (SS-WF OCTA) and investigated the relationships with the microperimetry (MP-1) functional changes observed in the same areas.
Methods
This was a single-center observational case series. Seven PDR eyes naïve to treatment that received three monthly intravitreal injections of aflibercept were included. All eyes were imaged with SS-WF OCTA and MP-1 at baseline (T0) and 1 month after the third injection (T1). The regions of interest (ROIs) with evidence of NPAs at T0 OCTA images were selected. Qualitative and quantitative [perfusion density (PD) and vessel length density (VLD)] OCTA vascular changes in the selected ROIs between T0 and T1 were compared with the corresponding MP-1 functional changes [mean sensitivity (MS)].
Results
Twenty-five ROIs were selected. In 52% of the ROIs, an improvement in MS was observed at T1, which was associated with qualitative and quantitative improvement in 92.3% of NPAs by OCTA. In 32% of the ROIs, MS worsening was observed at T1, which was associated with qualitative and quantitative worsening in 75% of NPAs by OCTA. Positive correlations between MS and both PD and VLD were found. Fisher’s test showed an association between the improvements in MP and VLD.
Conclusions
An association between OCTA and MP-1 parameter changes was found. The concomitant functional and morphological improvement in half of the ROIs suggests that anti-VEGF treatment may promote retinal changes that result in a better functional response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What happens to nonperfusion areas (NPAs) in patients with diabetic retinopathy after anti-VEGF treatment is still under debate |
The aim of this study was to investigate the changes in NPAs as assessed by OCTA and the corresponding microperimetric functional changes observed in the same areas in proliferative diabetic retinopathy eyes treated with anti-VEGF injections. |
In half of the analyzed NPAs (52%), a mean sensitivity improvement was observed after three IVT anti-VEGF injections, and 92.3% of these NPAs were associated with qualitative and quantitative improvement by OCTA. |
These results suggest that anti-VEGF treatment promoting retinal vascular changes would allow a better functional response to be obtained. |
Introduction
Diabetic retinopathy (DR) is the leading cause of blindness in the working-age population (20–74 years) and a primary microvascular complication of type 1 and type 2 diabetes [1, 2]. Vision loss in patients with DR is due to diabetic macular edema or proliferative DR (PDR). PDR is the final stage of DR characterized by preretinal and prepapillary neovascular vessels, which are abnormal vessels that can cause leakage, bleeding, and the development of vitreoretinal membranes with a high risk of tractional retinal detachment.
Panretinal photocoagulation has been the standard of care for PDR for decades [3]; however, recent data have proven that anti-vascular endothelial growth factor (VEGF) intravitreal injections are effective in inducing the regression of new vessels and, acting on retinal vascularity, improving the stage of diabetic retinopathy without photocoagulation of the peripheral retina [4, 5].
The anti-VEGF effects on retinal perfusion in patients with DR have remained unclear in some studies reporting retinal reperfusion [6,7,8] in contrast with others that exclude retinal reperfusion following treatment [9,10,11]. Therefore, what happens to nonperfusion areas (NPAs) after anti-VEGF treatment is still under debate.
Moreover, the relationship between the diffuse damage to the different vascular plexuses and their functional repercussions on retinal sensitivity (RS) is still unknown. Visual acuity is still considered the gold standard in the clinical practice of vision testing, but unfortunately, it does not entirely reflect the real visual functional abnormalities due to the retinal involvement secondary to diabetes mellitus. In contrast, microperimetry provides an accurate topographic correlation between anatomical lesions in the fundus and the corresponding visual function impairment. Previous studies have demonstrated that microperimetry shows a positive correlation with retinography and autofluorescence in DR [12] and with OCT in diabetic maculopathy [13, 14], and NPAs from severe nonproliferative diabetic retinopathy (NPDR) and PDR evaluated by means of fluorescein angiography showed morphologic changes in the retinal vascular structure that were correlated with the areas of RS loss [15]. However, to our knowledge, no studies have investigated the effects of anti-VEGF treatment on the functional status of areas with impaired perfusion in patients with diabetes.
Therefore, the aim of this study was to investigate the impact of the changes in the NPAs as assessed by OCTA on retinal function in PDR eyes treated with anti-VEGF injections.
Methods
Study Design and Study Population
A single-center observational case series was performed at IRCCS-Fondazione G.B. Bietti in Rome, Italy. The observations included eyes in consecutive patients with a diagnosis of proliferative diabetic retinopathy without macular edema treated with three monthly 2.0 mg intravitreal injections of aflibercept between January 1, 2021 and December 31, 2021. The study received institutional review board approval and followed the tenets of the Declaration of Helsinki. Written informed consent was obtained from all patients. Only patients naïve to treatment were included in the present study. The inclusion criteria were as follows: a minimum of 18 years of age, diagnosis of type 1 or type 2 diabetes, and a Diabetic Retinopathy Severity Scale (DRSS) score at baseline classified as PDR according to the ETDRS-simplified American Academy of Ophthalmology DR grading scale [16].
Patients were excluded if any other retinal diseases were present, if the patients were affected by media opacities (such as vitreous hemorrhage or cataract) or macular edema, and if they were treated with laser therapy or intravitreal injections in the past. Patients were also excluded if contraindications to anti-VEGF injections were present, in the case of a history of recent surgery (less than 4 months; cataract or pars plana vitrectomy) or poor quality of images (a signal strength index less than 6/10 was considered the threshold to define a poor quality of images).
After providing informed consent, all patients underwent a complete ophthalmological examination with best-corrected visual acuity (BCVA) measured with logMAR, anterior segment biomicroscopy, intraocular pressure (IOP) measurement with a Goldmann tonometer, and ocular fundus at baseline (T0) and 1 month after the third aflibercept injection (T1).
Image Acquisition
Ultra-widefield color fundus photographs (UWF-CFPs) and fluorescein angiography (UWF-FA) (Optos California; Optos, PLC, Dunfermline, Scotland) were performed at T0 to verify the Diabetic Retinopathy Severity Scale (DRSS) score as PDR and at T1 to assess any changes in the DRSS score.
At T0 and T1, swept-source (SS) OCT angiography (OCTA) and MP-1 microperimetry were performed by using the following devices:
-
1.
SS-wide field (WF) OCTA (PlexElite OCTA, Carl Zeiss Meditec, Inc., Dublin, CA, USA). Because of the higher lateral resolution, central 15 × 9 mm OCTA images were used. The whole retinal vasculature slab was chosen for the OCTA evaluation, including automatic segmentation from the inner limiting membrane up to 70 mm above the retinal pigment epithelium.
-
2.
MP-1 Microperimetry (Nidek, Gamagori, Japan). Microperimetry was performed under mesopic conditions, as previously described in detail [17]. For the purpose of this study, the following parameters were used: a single cross fixation target 1° in diameter; white, monochromatic background set at 1.27 cd/m2 (= 4 asb); stimulus size Goldmann III with a 200-ms projection time; a 4–2 double staircase strategy; and a grid of 90 stimuli covering the central 40° (centered onto the fovea). Microperimetry was performed twice within 1 week to rule out potential learning effects in each patient after a brief training session, and the second test was used for the analysis.
Image Analysis
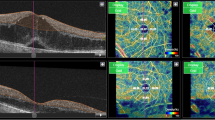
All images were exported in tagged image file format (TIFF). By using i2k Retina software (DualAlign LLC), all fundus images acquired at T1 (the central 15 × 9 SS-WF enface OCTA image and the numerical map MP-1 image) were aligned with respect to those obtained at T0. Then, with ImageJ software (version 1.50; National Institutes of Health, Bethesda, MD; available at http://rsb.info.nih.gov/ij/index.html) and using the vascular landmarks as a reference, the aligned images were overlaid and manually cropped to keep only the same part of the fundus. Finally, all images were divided into a grid with nine identical boxes (S1–S9) for quantitative and qualitative evaluations (Fig. 1).
An example of the method used to analyze the obtained images. The pre- and posttreatment whole retina 15 × 9 SS-WF enface OCTA image and MP-1 numerical map image were exported in tagged image file format (TIFF) (a). By using i2k Retina software (DualAlign LLC), the images obtained at T0 and T1 were aligned (b), overlaid using the vascular landmarks as a reference (c), and cropped (d) to keep exactly the same part of the fundus. This final image was divided into a grid with nine identical boxes (S1–S9) (e). At this point, we selected the regions of interest (ROIs) from each eye for qualitative and quantitative evaluation that contained evidence of nonperfusion from the OCTA performed at T0 (if present), choosing one for each of the following four boxes which were those that were found to present nonperfusion areas: S5 (foveal and parafoveal region) and S3, S6, and S9 (superotemporal, temporal, and inferotemporal boxes, respectively) (e)
Then, by carefully analyzing each of the nine boxes, for each eye, the senior author selected the regions of interest (ROIs) with evidence of nonperfusion at the OCTA performed at T0 (if present) for qualitative, quantitative, and functional evaluations. The NPAs were defined as areas on the SS-WF OCTA image with the absence of a capillary bed between a terminal arteriole and a proximal venule or larger vessels and the absence of regular retinal arterioles, venules, or capillaries compared with a standard OCTA image. SS-OCTA images were studied meticulously to exclude the presence of pre- or intraretinal material, such as hard exudates, spot bleedings, or intraretinal cysts, before selecting the areas of interest for further analysis.
SS-OCTA Qualitative Evaluation
The selected ROIs were evaluated by two blinded retina specialists (MP and DDG) in separate sessions. The specialists examined all ROIs box by box to detect any changes in vascular perfusion between T0 and T1. In case of discrepancy between the graders, the related images were reviewed by both specialists together to achieve a final common agreement. For each ROI, each grader evaluated the appearance of new vessels at T1 that were absent at T0 (indicated with a green arrow) or the areas in which vessels present at T0 were absent at T1 (indicated with a red arrow) (Fig. 2). If the ROI analysis presented more green arrows than red arrows at T1, the ROI was considered improved. Conversely, if more red arrows than green arrows were counted, the ROI was considered worsened. If perfusion changes detected at T0 appeared unchanged at T1, the perfusion in the ROI was considered stable.
An example of an ROI that showed local mean sensitivity (MS) improvement corresponding to qualitative and quantitative OCTA perfusion improvement. Qualitative evaluation (a): the perfusion changes in the ROIs selected between T0 (left column) and T1 (right column) were evaluated. The green arrow indicates a new vessel in T1 that was absent at T0. The perfusion in the analyzed ROI was considered qualitatively improved. Quantitative evaluation: for the same ROI, perfusion density and vessel length density were calculated after binarizing (b) and skeletonizing (c) the exported images. Only the inserts of the binarized and skeletonized images related to the analyzed ROI are shown. Functional evaluation: for the same ROI, the local MS pre- and posttreatment was considered. The local MS appeared to be improved in T1 compared with T0 (d)
OCTA Quantitative Evaluation
Quantitative analysis was also performed on the ROIs highlighted by the graders. The OCTA computed measures were (1) the whole retina perfusion density (PD) of each sub-ROI with evidence of an NPA and (2) the whole retina vessel length density (VLD) of each sub-ROI with an NPA (Fig. 2). PD was defined as the ratio of the area occupied by the vessels divided by the total area, and VLD is the total vessel length divided by the total number of pixels in the analyzed skeletonized image. A previously reported algorithm was applied to quantify these variables using global thresholding [18,19,20]. The parts of interest from the whole retina slabs were then imported into ImageJ software version 1.50 (National Institutes of Health, Bethesda, MD; available at http://rsb.info.nih.gov/ij/index.html). The PD and VLD were calculated after binarizing and skeletonizing the images with a previously published algorithm [18, 21, 22].
MP-1 Quantitative Evaluation
For each of the selected ROIs, the local mean sensitivity (MS) values at T0 and T1 were considered. The local MS was the mean of all MP values contained inside each of the selected ROIs (Fig. 2).
Finally, a comparison between the OCTA quantitative and qualitative perfusion changes and the functional local MP-1 changes observed after the three aflibercept injections was performed for each ROI.
Data Analysis and Statistical Methods
Statistical evaluation was performed using SPSS (IBM SPSS Statistics 25). All results are expressed as the mean ± standard deviation (SD) and frequency. The intraclass correlation coefficient (ICC; two-way, random-effects model) was calculated to estimate the absolute agreement between the two graders (MP and DDG). Spearman correlation was computed between the variation (T1 − T0) of mean sensitivity and OCTA parameters (perfusion density and vessel length density). Moreover, to investigate the association of the changes in mean sensitivity over time with respect to the OCTA parameters, the changes in MS, PD, and VLD were dichotomized (variation with a “ + ” sign indicates improvement and variation with a “−” sign indicates worsening), and the frequencies of these parameters were studied by using the Fisher test.
Results
Baseline Characteristics
The observational study included seven eyes from six patients with type 2 diabetes and PDR treated with three monthly injections of 2.0 mg of aflibercept between January 1, 2021 and December 31, 2021. Baseline demographic characteristics are shown in Table 1. The mean age was 51.5 ± 19.9 years, and the mean diabetes duration was 13.2 ± 7.4 years. The mean HbA1c value at baseline was 9.2 ± 2.7%, and the BCVA was 80 ± 4.1 ETDRS letters at T0 and 77.7 ± 7.2 ETDRS letters at T1. All seven eyes showed a DRSS score of PDR at baseline.
The graders analyzed all nine boxes for each eye. NPAs were identified exclusively in the following four boxes: S5 (foveal and parafoveal region) and S3, S6, and S9 (superotemporal, temporal, and inferotemporal boxes, respectively). The graders selected one ROI characterized by the presence of an NPA for each of these boxes. Two boxes were excluded from the analysis because of the absence of well-defined NPAs and one was excluded because of the presence of preretinal hemorrhage that masked part of the OCTA image. The remaining 25 boxes allowed the identification of 25 ROIs characterized by the presence of NPAs and were selected for further analysis (Table 2).
Twelve out of the 25 selected ROIs (48%) showed an improvement in the local MS at T1 associated with a concomitant qualitative and quantitative improvement by OCTA. Six out of the 25 selected ROIs (24%) showed a worsening of the local MS at T1 associated with a concomitant qualitative and quantitative worsening by OCTA. Two ROIs (8%) showed both qualitative and quantitative improvement in OCTA perfusion but functional worsening in the MP-1 values. One ROI (4%) showed worsening of both the qualitative and quantitative OCTA perfusion with concomitant increased MP-1 values. One ROI (4%) showed stable microperimetric values with worsening of OCTA qualitative and quantitative perfusion. Three eyes (12%) showed stable microperimetric values and no changes in the OCTA qualitative and quantitative evaluation.
In 52% of the ROIs, an improvement in MS was observed after three IVT anti-VEGF injections. In 92.3% of these ROIs, the MS improvement was associated with qualitative and quantitative improvement in the NPAs. In 7.7% of these ROIs, the MS improvement was not associated with qualitative and quantitative improvement in the NPAs. Conversely, in 32% of the ROIs, MS worsening was observed after three IVT anti-VEGF injections. In 75% of these ROIs, MS worsening was associated with NPA qualitative and quantitative deterioration by OCTA. In 25% of these ROIs, the MS decline was not associated with qualitative and quantitative worsening of the NPAs by OCTA.
Overall, in 80% of the selected ROIs, an association between qualitative and quantitative NPA evaluation and functional changes was found.
In 13 out of the 25 ROIs analyzed (52%), an improvement in local MS could be described. PD improved in 11 out of 25 ROIs (44%) and VLD improved in 13 out of 25 ROIs (52%).
An excellent degree of reliability (ICC = 0.994) was found between the readers grading the NPAs from the OCTA images. Spearman’s rank correlation was computed to assess the relationship between the variations in post–pre mean sensitivity, PD, and VLD. Positive correlations between the MS and PD variables, r(26) = 0.580, p = 0.002, and between the MS and VLD variables, r(26) = 0.490, p = 0.011, were found.
Fisher’s test showed an association between the improvement in MS and VLD (p = 0.015), while there was no significant association between MS and PD (p = 0.246).
Discussion
In this study, we explored the association between functional retinal changes and changes in OCTA NPAs in PDR eyes treated with anti-VEGF injections. In our population, NPAs were identified exclusively in the foveal and parafoveal regions (S5) and in the temporal boxes (S3, S6, S9). The main involvement in term of vascular impairment of the perifoveal temporal regions in patients with diabetic retinopathy is not surprising considering previous evidence already reported in the literature [23].
Interestingly, in our study, in half of the analyzed ROIs (52%), MS improvement was observed after three IVT anti-VEGF injections, and in 92.3% of these ROIs, the MS improvement was associated with qualitative and quantitative improvement in the NPAs. Overall, in 80% of the selected ROIs, an association between the qualitative and quantitative OCTA evaluations and MP-1 functional changes in the NPAs analyzed was found.
The association between perfusion impairment, imaged by fluorescein angiography or OCTA, and functional impairment, tested with visual field or microperimetry, in diabetic eyes has already been reported and widely discussed in the literature. In 2007, Unoki et al. [15] reported a connection between areas with reduced retinal capillary perfusion on fluorescein angiography and regional visual field sensitivity abnormalities in patients with severe NPDR or PDR. More recently, Scarinci et al. [24] described a correlation between OCTA deep capillary plexus impairment and retinal sensitivity loss on microperimetry in diabetic macular ischemia.
However, this study, in addition to confirming the association between nonperfusion areas and retinal sensitivity loss, shows for the first time the presence of retinal functional improvement after anti-VEGF treatment in half of the NPAs analyzed (52%), corresponding in most of the cases (92.3%) to OCTA qualitative and quantitative improvements. This result allows us to take a further step in understanding the effects of anti-VEGF agents on retinal perfusion as well as the retinal function of patients with diabetes. Furthermore, these data suggest that anti-VEGF treatment that promotes retinal vascular changes (namely, PD and VLD increases) would allow a better functional response to be obtained. This finding could be related to a reduction in intracellular fluid caused by the anti-VEGF agents, resulting in better intercellular signal transmission and retinal functional improvement. If confirmed, this result may allow us to conclude that anti-VEGF treatment could improve retinal function evaluated by means of microperimetry as well as retinal perfusion with a possible impact on the quality of vision of patients with diabetes.
Of note, when we consider the OCTA changes in the NPAs, we have to take into account that the improvement in the visualization of the vasculature in the NPAs after treatment could be related to a change in the velocity of the blood inside the vessels, allowing them to be more visible, and not strictly related to true reperfusion.
The observation of improved retinal perfusion after anti-VEGF treatment agrees with previous results reported by Levin et al. [6] that demonstrated retinal reperfusion following anti-VEGF injection in 12 out of 16 NPDR and PDR eyes (75%), as studied with UWF-FA. Similarly, Campochiaro et al. [7] investigated the effect of an anti-VEGF agents (ranibizumab) on changes in NPAs over time in retinal vein occlusion (RVO) eyes in the BRAVO and CRUISE studies and found that blockade of VEGF prevents the worsening of retinal nonperfusion, thus promoting reperfusion.
We also observed in this study that 32% of the ROIs showed a decline in local MS after anti-VEGF treatment (24% presenting with OCTA perfusion worsening and 8% presenting with OCTA perfusion improvement). Most likely, the perfusion impairment in 24% of the ROIs analyzed may result in MS loss due to photoreceptor suffering caused by hypoperfusion. Conversely, the 8% of ROIs that showed an MS deterioration despite the observed OCTA improvement can be explained by hypothesizing that the functional damage to photoreceptors was too advanced to allow functional improvement, suggesting the progression of photoreceptor damage despite anti-VEGF treatment. Moreover, although analysis of the choroid was outside the aim of this study, focal choriocapillaris ischemia and diabetic choroidopathy cannot be totally excluded in the presence of photoreceptor damage. In another study [25], we reported that outer retina dysfunction in NPDR eyes correlates with choriocapillaris dropout, suggesting that the outer retinal elements are functionally impaired in proportion to the choriocapillaris vascular supply deficit.
A small percentage of ROIs (4%) showed worsening of the qualitative and quantitative features on OCTA with concurrent increases in MP-1 values. These cases could be explained by the hypothesis that despite the reduction in retinal perfusion in some areas, the choroid can still support the function of the photoreceptors.
Limitations of the present study are the relatively small number of patients and a short follow-up period. Furthermore, OCTA technology allows the visualization of vessels with a flow rate above a certain threshold; thus, some vessels that were deemed revascularized after anti-VEGF treatment could have been vessels in which the flow rate increased and were more visible. Moreover, we did not analyze the superficial and deep capillary plexuses separately. Instead, we used whole retinal vasculature segmentation because discrimination between different perfusion changes in different retinal layers was outside the aim of this study. Finally, we did not analyze the effects of anti-VEGF treatment on DR severity because of the small number of eyes studied and the short follow-up period. On the other hand, the strength of this work is represented by the homogeneous population included, as it was characterized by PDR eyes without macular edema treated with three intravitreal injections of aflibercept.
Conclusions
We observed in PDR eyes treated with the anti-VEGF agent an association between changes in retinal function that was evaluated by means of microperimetry and qualitative and quantitative OCTA NPAs. We observed that in most of the ROIs analyzed (52%), the MS improvement corresponded to a qualitative and quantitative OCTA improvement. This result may help to further understand the effects of anti-VEGF therapy on retinal perfusion as well as retinal function in patients with diabetes.
References
Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64.
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond). 2015;2:17.
Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Ophthalmology. 1991;98(5 Suppl):766–85.
Writing Committee for the Diabetic Retinopathy Clinical Research Network, Gross JG, Glassman AR, et al. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA. 2015;314:2137–2146.
Sivaprasad S, Prevost AT, Vasconcelos JC, et al. Clinical efficacy of intravitreal aflibercept versus panretinal photocoagulation for best corrected visual acuity in patients with proliferative diabetic retinopathy at 52 weeks (CLARITY): a multicentre, single-blinded, randomised, controlled, phase 2b, non-inferiority trial. Lancet. 2017;389:2193–203.
Levin AM, Rusu I, Orlin A, et al. Retinal reperfusion in diabetic retinopathy following treatment with anti-VEGF intravitreal injections. Clin Ophthalmol. 2017;21(11):193–200.
Campochiaro PA, Bhisitkul RB, Shapiro H, Rubio RG. Vascular endothelial growth factor promotes progressive retinal nonperfusion in patients with retinal vein occlusion. Ophthalmology. 2013;120(4):795–802.
Mir TA, Kherani S, Hafiz G, et al. Changes in retinal nonperfusion associated with suppression of vascular endothelial growth factor in retinal vein occlusion. Ophthalmology. 2016;123(3):625–34.
Ghasemi Falavarjani K, Iafe NA, Hubschman JP, Tsui I, Sadda SR, Sarraf D. Optical coherence tomography angiography analysis of the foveal avascular zone and macular vessel density after anti-VEGF therapy in eyes with diabetic macular edema and retinal vein occlusion. Invest Ophthalmol Vis Sci. 2017;58(1):30–4.
Bonnin S, Dupas B, Lavia C, et al. Anti-vascular endothelial growth factor therapy can improve diabetic retinopathy score without change in retinalperfusion. Retina. 2019;39(3):426–34.
Couturier A, Rey PA, Erginay A, et al. Widefield OCT-angiography and fluorescein angiography assessments of nonperfusion in diabetic retinopathy and edema treated with anti vascular endothelial growth factor. Ophthalmology. 2019;126(12):1685–94.
Midena E, Vujosevic S. Microperimetry in diabetic retinopathy. Saudi J Ophthalmol. 2011;25(2):131–5.
Vujosevic S, Midena E, Pilotto E, Radin PP, Chiesa L, Cavarzeran F. Diabetic macular edema: correlation between microperimetry and optical coherence tomography findings. Invest Ophthalmol Vis Sci. 2006;47(7):3044–51.
Vujosevic S, Torresin T, Berton M, Bini S, Convento E, Midena E. Diabetic macular edema with and without subfoveal neuroretinal detachment: two different morphologic and functional entities. Am J Ophthalmol. 2017;181:149–55. https://doi.org/10.1016/j.ajo.2017.06.026.
Unoki N, Nishijima K, Sakamoto A, et al. Retinal sensitivity loss and structural disturbance in areas of capillary nonperfusion of eyes with diabetic retinopathy. Am J Ophthalmol. 2007;144(5):755–60.
Early Treatment Diabetic Retinopathy Study Research Group. Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Ophthalmology. 1991;98(5 Suppl):823–33.
Midena E, Vujosevic S, Convento E, et al. Microperimetry and fundus autofluorescence in patients with early age-related macular degeneration. Br J Ophthalmol. 2007;91:1499–503.
Uji A, Balasubramanian S, Lei J, Baghdasaryan E, Al-Sheikh M, Sadda SR. Impact of multiple en face image averaging on quantitative assessment from optical coherence tomography angiography images. Ophthalmology. 2017;124(7):944–52.
Durbin MK, An L, Shemonski ND, et al. Quantification of retinal microvascular density in optical coherence tomographic angiography images in diabetic retinopathy. JAMA Ophthalmol. 2017;135(4):370.
Kim AY, Chu Z, Shahidzadeh A, Wang RK, Puliafito CA, Kashani AH. Quantifying microvascular density and morphology in diabetic retinopathy using spectral-domain optical coherence tomography angiography. Investig Ophthalmol Vis Sci. 2016;57(9):362–70.
Di Antonio L, Viggiano P, Ferro G, et al. Retinal vascular metrics difference by comparison of two image acquisition modes using a novel OCT angiography prototype. PLoS ONE. 2020;15(12): e0243074.
Borrelli E, Toto L, Viggiano P, Evangelista F, Palmieri M, Mastropasqua R. Widefield topographical analysis of the retinal perfusion and neuroretinal thickness in healthy eyes: a pilot study. Eye. 2020;34(12):2264–70.
Alam M, Zhang Y, Lim JI, Chan RVP, Yang M, Yao X. Quantitative optical coherence tomography angiography features for objective classification and staging of diabetic retinopathy. Retina. 2020;40(2):322–32.
Scarinci F, Varano M, Parravano M. Retinal sensitivity loss correlates with deep capillary plexus impairment in diabetic macular ischemia. J Ophthalmol. 2019;13(2019):7589841.
Parravano M, Ziccardi L, Borrelli E, et al. Outer retina dysfunction and choriocapillaris impairment in type 1 diabetes. Sci Rep. 2021;11(1):15183.
Acknowledgements
Funding
The research for this paper was financially supported by the Italian Ministry of Health and Fondazione Roma. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author Contributions
All authors contributed to the conception and design, acquisition of data, analysis and interpretation of data, and drafting and critical review of the manuscript. All authors read and approved the submission of this manuscript.
Disclosures
Mariacristina Parravano reports personal fees from Allergan, Bayer, Novartis, and Roche. Giuseppe Querques reports personal fees outside of the submitted work from Alimera Sciences, Inc., Allegro, Allergan, Apellis, Baush & Lomb, Bayer Healthcare Pharmaceuticals, Boehringer Ingelheim, Heidelberg Engineering, Lumithera, Nevacar, Novartis Pharmaceuticals Corporation, Roche, SIFI, Sooft/Fidia, Topcon, Thea, and Zeiss. Daniele De Geronimo, Riccardo Sacconi, Daniela Giannini, Eliana Costanzo, Serena Fragiotta, Pasquale Viggiano and Monica Varano have nothing to disclose.
Compliance with Ethics Guidelines
All patients provided informed consent before starting treatment. The retrospective data collection protocol was approved by the central ethics committee IRCCS Lazio, Sezione IFO—Fondazione Bietti (N.114/21/FB) and performed in agreement with the Declaration of Helsinki for research involving human subjects and in accordance with the Italian laws on privacy and data protection.
Data Availability
All data generated or analyzed during this study are included in this published article and in the Supplementary Material.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Parravano, M., De Geronimo, D., Sacconi, R. et al. Impact of Intravitreal Anti-VEGF Therapy on Microperimetry of the Retinal Nonperfusion Areas of Patients with Proliferative Diabetic Retinopathy. Ophthalmol Ther 11, 2117–2128 (2022). https://doi.org/10.1007/s40123-022-00568-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00568-x