Abstract
Introduction
This study aimed to test and evaluate modified corneal cross-linking (CXL) protocols regarding improved treatment effects on the peripheral cornea in terms of tissue stability and cellular response.
Methods
Peripheral CXL (pCXL) was performed within a ring of 9–11 mm of 36 human donor corneas with variations in applied energy (5.4, 7.2, and 10 J/cm2) at 9 mW/cm2 irradiance. Each energy level was additionally modulated regarding the oxygen level surrounding the cornea during treatment (21%; 100%). Stress–strain tests with endpoints at 12% strain and collagenase A-assisted digestions to complete digestion were performed to evaluate the rigidity and resistance of treated and control tissue. Further, corneas were processed histologically via TUNEL assay and H&E staining to demonstrate the effects on stromal cells during treatment under varying CXL conditions.
Results
Increases in energy dosage achieved significant increases in resistance to stress in all variations except when comparing protocols A and B under normoxic conditions. Supplemental oxygen significantly increased rigidity in protocols B (p < 0.01) and C (p = 0.018). Hyperoxic conditions significantly increased resistance to digestion in all protocols. The number of DNA strand breaks in TUNEL assay staining showed significant increases in all increases in energy as well as with oxygen supplementation.
Conclusions
Increases in energy and supplemental oxygen improved the effect of CXL, though endothelial safety could not be verified with confidence in high-fluence CXL with supplemental oxygen. Results suggest that CXL protocols using 7.2 J/cm2 with 100% O2 or 10 J/cm2 without supplemental oxygen prove most effective without anticipated risk of endothelial damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Currently, corneal cross-linking (CXL) protocols are focused solely on the central cornea. |
Finding CXL protocols that are effective in the peripheral cornea could improve topographic transplant stability, directly affecting refractive outcomes. |
This study looked at what levels of total energy dosage with and without supplemental oxygen improve CXL effectiveness in terms of tissue stability and cellular effect in the peripheral cornea. |
What was learned from the study? |
CXL with 7.2 J/cm2 with 100% O2 or 10 J/cm2 without supplemental oxygen prove most effective in achieving increases in tissue stability and cellular response. |
Introduction
Corneal cross-linking (CXL) is routinely used as a first surgical measure when the progression of an ectasia such as keratoconus or post-LASIK ectasia is observed and has shown beneficial short- and long-term results regarding keratometric stabilization and a lower rate of corneal transplantation to treat the underlying ectasia [1,2,3,4,5]. Still, there will be a demand for DALK (deep anterior lamellar keratoplasty) and PK (penetrating keratoplasty) in eyes with keratoconus in cases of treatment failure and subsequent disease progression [6,7,8], cases with Descemet rupture, or in cases with corneal scarring secondary to contact lens use [9]. Although DALK and PK show good visual and topographic long-term results, cases with progressive peripheral corneal thinning and subsequent tilting of the transplant with high astigmatism and loss of vision are observed [10]. Usually, it takes 1–2 decades until an RCK (recurrent keratoconus) is observed. It is still under debate whether the observed changes involve the transplanted tissue itself or if the changes are due to a progression of the disease in the recipient corneal tissue, leading to the clinically observed tomographic changes (Fig. 1).
Although efforts have been made to stop the progression of an RCK by performing a CXL procedure in eyes with a corneal transplant, it might be more effective to perform this procedure at the time of transplantation [11]. By doing so, a loss of vision by RCK and subsequent transplant decentration/tilt might be prevented.
CXL of the peripheral cornea in eyes with planned corneal transplantations might therefore have advantages in terms of long-term stability due to an increased biomechanical stability reducing the risk of RCK. A treatment area between 7 and 11 mm from the apex could be effective for this type of indication, in contrast to the treatment area of the central 9 mm usually used in standard corneal cross-linking procedures.
To date, little is known about the effectiveness of standard CXL protocols on the peripheral cornea. The peripheral cornea is thicker by approximately 40% compared to the center of the cornea [12]. This increased corneal pachymetry requires an adaptation of treatment protocols designed for the central cornea. Further, the extracellular matrix in keratoconic eyes has been shown to be altered in the peripheral cornea, which might affect biomechanical outcomes [13]. Performing CXL on peripheral corneal tissue before keratoplasty can have a twofold effect: preventing ectatic progression of the recipient bed and reducing the likelihood for rejection episodes mediated via reduction of corneal neovascularization, lymphatic tissue, and dentritic cell density [14].
The physiologically thicker tissue in the cornea’s periphery reduces the risk of phototoxic endothelial damage compared to the central cornea. However, irradiation of the peripheral cornea can bear the additional risk of damaging limbal stem cells [15,16,17,18].
With the treatment goals of biomechanical stabilization and reduction of corneal neovascularization in mind, standard treatment protocols are likely not to be sufficient. To achieve an improved treatment effect, optimization of the current treatment protocols is therefore mandatory. The aim of this trial was to evaluate the effect of different CXL treatment protocols on the biomechanical properties and histological changes in peripheral human corneal rims.
Methods
This trial was conducted under approval by the Institutional Review Board of the Medical University of Vienna (1578/2013) in accordance with the Helsinki Declaration of 1964 and all later amendments. The absence of an objection to organ donation was confirmed with the national opting-out registry prior to enucleation by the Eye Bank Vienna. Donor corneas were sourced exclusively from the Eye Bank Vienna. Inclusion and exclusion criteria for donor corneas were closely modelled on the criteria that apply for corneas eligible for transplantation. The average donor age was 59 ± 18.8 years.
A total of 78 corneas were used to conduct this trial, which modulated the total energy applied during pCXL to the peripheral zone (9–11 mm) of the cornea and the oxygen level of the cornea’s environment during treatment. pCXL was performed with 9 mW/cm2 continuous irradiance on 36 enucleated human cadaver corneas that were consecutively assigned to one of three protocols: protocol A applied the standard energy dose (5.4 J/cm2), protocol B applied 7.2 J/cm2, and protocol C applied 10 J/cm2. Each cornea, once designated to a protocol, was treated in thirds: one-third underwent CXL at a standard atmospheric oxygen concentration (21%) (groups A21, B21, and C21), one-third underwent the same CXL treatment in a hyperoxic environment (100% oxygen) (groups A100, B100, and C100), and the remaining third served as a control (Fig. 2). Each cornea was mounted on an artificial chamber which was filled with a 16% dextran–BSS (balanced salt solution) solution at an infusion pressure of 15 mmHg. After mechanical removal of the epithelium, a riboflavin solution (Peschke D, Peschke GmbH, Switzerland) was applied every 2 min for 20 min. A custom UV-impermeable protective guard covering 2/3 of the cornea and the limbus during each treatment ensured that UV-A stray light did not reach areas that were not currently being treated and served as a protective measure for limbal stem cells. CXL duration was adjusted to reach the intended energy dose after filtering by the material of the oxygen bell (measurement performed with Solarmeter Model 4.0, Solartech inc., Ontario, CA).
After CXL was performed, the peripheral corneal ring was dissected from the central button, and differently treated sections were separated. Each third of the peripheral ring (21% oxygen, 100% oxygen, and control) was then subjected to a stress–strain test to 12% using a UStretch device (CellScale, Waterloo, Canada). Throughout this process, corneal hydration was stabilized by performing tests in a bath of 16% dextran solution [19]. After a prestress of 5 × 103 Pa was applied for 100 s, strain was then increased linearly with a velocity of 0.035 mm/s. Stress was measured every 10 ms until a strain of 15% was reached. The force required to achieve 12% strain was recorded as an endpoint.
Additionally, tissue was digested using a 1% collagenase A solution (234 U/mL in Dulbecco’s phosphate-buffered saline; collagenase A from Clostridium histolyticum; Roche, Basel, Switzerland); time to complete digestion was recorded as previously described [20].
Twenty-seven additional corneas (nine corneas per protocol) were processed histologically with TUNEL assay (In Situ Cell Death Detection Kit, Fluorescein, Roche, Basel, Switzerland) after treatment with the described protocols (Fig. 3). DNA strand breaks were quantified using ImageJ software [21], counting intrastromal stained nuclei. The numbers of stained nuclei were compared between groups. Five further corneas per protocol were processed by H&E staining (Fig. 4) and were used for descriptive analysis.
Statistical analyses were performed using SPSS software version 20.0 (IBM Corporation, Armonk, New York, USA). p values below 0.05 were considered statistically significant. Normality was tested using the Kolmogorov–Smirnov test. Mann–Whitney U statistics was used for comparing nonparametric nonmatched groups. The tests were performed using a two-tailed p value of 0.05.
Results
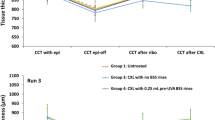
Stress Strain
Stress–strain results showed significant increases in applied force to reach 12% strain in treated specimens that underwent different protocols (p < 0.05), except when comparing results between protocol A and B with 21% oxygen (p = 0.39). With equal energy, supplemental oxygen yielded significant differences in the stress–strain test in protocols B (p < 0.01) and C (p = 0.018) (Fig. 5a). Control tissue was consistently comparable across all corneas (p > 0.05). Comparing protocols B100 to C21, no significant effect could be identified (p = 0.068).
Summary of average stress–strain force (a) and digestion time results (b) observed in this trial and results between varying energy dosages comparing equal oxygen conditions as well as varying oxygen conditions with equal applied energy dosages. Summary of induced number of cell deaths per frame in TUNEL assay staining (c)
Digestion
Comparing protocol A to B, there was no significant difference in time to complete digestion with standard 21% oxygen (p = 0.07). With supplemental oxygen in both protocols, there was a significant increase in time to complete digestion in protocol B compared to protocol A (p = 0.02).
Between protocols B and C, differences in time to compete digestion were significant with and without supplemental oxygen (p ≤ 0.01).
Supplemental oxygen produced significant differences in time to complete digestion within all protocols (A: p = 0.049; B: p = 0.032; C: p = 0.035) (Fig. 5b). Control tissue consistently yielded comparable results between protocols (p > 0.05).
Histology
A continuous increase in positively stained cells was found with increasing energy levels (Fig. 5c). The number of DNA strand breaks (TUNEL assay) in stromal cells yielded significant results in all variations in total energy dosage and oxygen levels (p < 0.05) in most comparisons. Exceptions were that supplemental oxygen did not produce significantly more DNA strand breaks in protocols A or B (p > 0.05).
H&E staining showed nucleus scarcity in superficial stromal layers as a result of CXL treatment. Total nucleus eradication in any stromal depth could not be observed at any of the applied energy dosages in this trial. However, a marked increase in the depth of nucleus scarcity in accordance with increases in applied energy could be observed consistently (Fig. 4). In corneas treated with 10 J/cm2, nuclei were rare even in deep stromal layers.
Discussion
Recurrent keratoconic progression of a previously functional transplant is associated with high levels of astigmatism, thinning of recipient or donor cornea, and even acute hydrops [10]. These changes can have a detrimental effect on visual acuity. Large diameter repeat keratoplasties with increased risk for rejection might be necessary to restore vision in these cases. To our knowledge, this study is the first to evaluate the effect of different CXL protocols on the peripheral corneal. Adapting existing CXL protocols to suit the conditions of the cornea’s periphery and the altered treatment goals can largely contribute to the treatment’s success and in turn patients’ long-term benefit from keratoplasty.
Effect on Biomechanical Stabilization of Peripheral Corneal Tissue
The standard fluence applied with CXL (5.4 J/cm2) is effective in stabilizing the central corneal tissue in most cases [22]. Yet, when performed on the cornea’s periphery, no significant increases in rigidity (Young’s modulus) could be observed with the protocol A21 (5.4 J/cm2) in this trial (Table 1). Protocol A100 prolonged the time to complete digestion but did not increase Young’s modulus significantly. This study therefore provides evidence that the standard fluence used for corneal cross-linking with 9 mW/cm2 irradiance does not achieve a significant change in the biomechanical properties in the peripheral cornea, underscoring the necessity for higher-fluence pCXL.
Increasing the fluence to 7.2 J/cm2 (B21) did not result in a significant increase of stress–strain measurements. Protocol B100, however, showed a significant increase in biomechanical stability in stress–strain and digestion tests compared to protocol A100. Supplemental oxygen further increased tissue stability within protocol B (B21:B100), raising both rigidity in stress–strain tests and time to complete digestion. Stability and resistance to digestion significantly increased when the applied energy was further raised from 7.2 to 10 J/cm2 under normoxic conditions (B21; C21). Further increases were observed under hyperoxic conditions.
Accordingly, there appears to be a benefit to increasing the fluence to 7.2 J/cm2 with 100% oxygen or to 10 J/cm2 in order to achieve a significant effect in terms of biomechanical stability when treating the peripheral 9–11 mm of human corneal tissue. Although long-term studies after CXL in keratoconic eyes showed stability of the disease for up to a decade, long-term trails will have to show if this remains true for cases after peripheral CXL and corneal transplantation [22].
Effect on a Cellular Level
After CXL according to protocol A, the histological effect appears to be limited to the superficial stromal layers, leaving most of the stroma unaffected by the treatment. This finding parallels the results of tissue stability test results. Superficial treatment will likely have a limited effect on deeper structures and be ineffective in treating deep corneal neovascularization and lymphatic vessels [14, 23].
The histological images obtained from corneas treated with protocol B show a considerable increase in effect compared to protocol A, yet treatment appears to spare the deep stromal layers. This is demonstrated in a relative increase in nucleus density towards the deeper stroma in H&E staining and DNA strand breakage rarity in deeper stroma TUNEL assay processing compared to more superficial stromal layers. The marked increase in DNA strand breaks is indicative of an increase in corneal alterations as a response to CXL with 7.2 J/cm2 as opposed to 5.4 J/cm2.
When the applied energy was raised from 7.2 to 10 J/cm2, the depth of dense DNA strand breakage appeared to reach deep stromal levels. Histological images from corneas treated according to protocol C show a very pronounced and deep CXL effect, particularly after treatment according to protocol C100. A deep effect on a cellular basis could be effective in terms of treatment of corneal neovascularization and lymphatic vessels.
Corneal neovascularization and lymphatic vessels in the peripheral cornea are major risk factors for transplant failure due to rejection episodes. Several treatment methods have been proposed to reduce corneal vessels and to reduce corneal lymphatic vessels prior to corneal transplantation. A relatively new approach has been made with the attempt to perform a corneal cross-linking procedure to the peripheral cornea with this indication profile [14, 23, 24]. It has been shown that this approach can lead to a reduction of corneal neovascularization in humans and a reduction of lymphatic vessels in an animal model. Adapting CXL protocols to accommodate the characteristics of peripheral corneal tissue might improve treatment success with these indications by enabling an adequate treatment depth to be reached. This trial showed that with increased total energy the depth of cellular damage increases considerably. Therefore, an increased treatment effect concerning corneal vessels might be anticipated with protocol C21/100 compared to protocol A21/100 or B21/100.
Additionally, a reduction of dentritic cells in the recipient cornea prior to transplantation might reduce the risk for rejection mediated by the indirect rejection pathway in high-risk situations. While dendritic cells are found predominantly in the anterior stroma, macrophages are also found in the posterior stoma [25]. Though considerably less potent at initiating and modulating secondary immune responses, macrophages are key effector cells in immune regulation and angiogenesis, which is a defining predictive marker for transplant survival [26,27,28]. Lymphatic vessels can be found in superficial as well as deep stromal layers in vascularized corneal tissue [29]. Thus, reaching deep stromal levels with pCXL could considerably dampen both dendritic cell-mediated secondary, antigen-specific adaptive immune responses as well as macrophage-induced immune responses and angiogenesis.
Protocol C induced cell death in deep stromal layers seen in both TUNEL assays as well as H&E-stained images. The presence of intact nuclei in deep stromal layers in H&E-stained specimens implies that these layers and the endothelium are spared from cell death-inducing radiation even in protocol C100, yet do not verify endothelial safety. An applied fluence of 10 J/cm2 in normoxic surroundings produced pronounced cellular changes and the endothelium did not show increased levels of staining in the TUNEL assay, yet definitive differentiation from deep stromal DNA breakage was not possible. To ensure treatment safety, there is an argument to be made for choosing protocols C21 or B100, which showed excellent treatment effects with larger margins of preserved stromal nuclei in this trial. Although in the setting of an operating room, supplying an oxygen-goggle to the patient to allow hyperoxic pCXL to be performed could be a feasible adjustment, additional costs for consumables need to be taken into consideration.
This trial’s limitations are largely due to the process of tissue preparation (dehydration, freezing/paraffinization), which makes it impossible to determine the exact depth of cell damage from the histological images produced in this trial. Results of this trial can therefore be applied to ectatic corneas only with caution and with verification of adequately high peripheral pachymetry measurements prior to treatment. Irradiation energy was chosen at 9 mW/cm2 in all treatment protocols, as this is the most widely used and accessible irradiation intensity. According to earlier work, this energy setting strikes a compromise between treatment speed and effectiveness [30].
Conclusions
This trial showed promising results in adapting CXL treatment protocols to suit peripheral human corneal tissue and varying treatment goals. When aiming for maximum stabilization and treatment depth, standard CXL fluence achieves insufficient effects in the peripheral cornea. Summarizing our results, in terms of maximization of the treatment effect for biomechanical stability and effect at the cellular level, treatment with protocols B100 or C21 at an irradiance of 9 mW/cm2 appear to be highly effective.
References
Godefrooij DA, Gans R, Imhof SM, Wisse RPL. Nationwide reduction in the number of corneal transplantations for keratoconus following the implementation of cross-linking. Acta Ophthalmol. 2016;94(7):675–8. https://doi.org/10.1111/aos.13095.
Hersh PS, Greenstein SA, Fry KL. Corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011;37(1):149–60. https://doi.org/10.1016/j.jcrs.2010.07.030.
Raiskup F, Theuring A, Pillunat LE, Spoerl E. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg. 2015;41(1). https://journals.lww.com/jcrs/Fulltext/2015/01000/Corneal_collagen_crosslinking_with_riboflavin_and.8.aspx.
Sandvik GF, Thorsrud A, Råen M, Østern AE, Sæthre M, Drolsum L. Does corneal collagen cross-linking reduce the need for keratoplasties in patients with keratoconus? Cornea. 2015;34(9). https://journals.lww.com/corneajrnl/Fulltext/2015/09000/Does_Corneal_Collagen_Cross_linking_Reduce_the.1.aspx.
Wittig-Silva C, Chan E, Islam FMA, Wu T, Whiting M, Snibson GR. A randomized, controlled trial of corneal collagen cross-linking in progressive keratoconus: three-year results. Ophthalmology. 2014;121(4):812–21. https://doi.org/10.1016/j.ophtha.2013.10.028.
Chanbour W, El Zein L, Younes MA, Issa M, Warhekar P, Chelala E, Jarade E. Corneal cross-linking for keratoconus and post-LASIK ectasia and failure rate: a 3 years follow-up study. Cureus. 2021;13(11):e19552–e19552. https://doi.org/10.7759/cureus.19552.
Lenk J, Herber R, Oswald C, Spoerl E, Pillunat LE, Raiskup F. Risk factors for progression of keratoconus and failure rate after corneal cross-linking. J Refract Surg. 2021;37(12):816–23. https://doi.org/10.3928/1081597X-20210830-01.
Vinciguerra R, Fossati G, Sorrentino T, et al. Corneal cross-linking for progressive keratoconus in patients older than 40 years: long-term follow-up. J Refract Surg. 2021;37(5):338–42. https://doi.org/10.3928/1081597X-20210210-01.
Barr JT, Wilson BS, Gordon MO, et al. Estimation of the incidence and factors predictive of corneal scarring in the collaborative longitudinal evaluation of keratoconus (CLEK) study. Cornea. 2006;25(1). https://journals.lww.com/corneajrnl/Fulltext/2006/01000/Estimation_of_the_Incidence_and_Factors_Predictive.3.aspx.
Yoshida J, Murata H, Miyai T, et al. Characteristics and risk factors of recurrent keratoconus over the long term after penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol. 2018;256(12):2377–83. https://doi.org/10.1007/s00417-018-4131-5.
Ziaei M, Gokul A, Vellara H, Patel D, McGhee CN. Peripheral cornea crosslinking before deep anterior lamellar keratoplasty. Med Hypothesis Discov Innov Ophthalmol J. 2020;9(2):127–34.
Fieß A, Marx-Groß S, Wasielica-Poslednik J, et al. Peripheral corneal thickness and associated factors—results from the population-based German Gutenberg Health Study. Acta Ophthalmol. 2021. https://doi.org/10.1111/aos.15057.
Alkanaan A, Barsotti R, Kirat O, Almubrad T, Khan A, Akhtar S. Ultrastructural study of peripheral and central stroma of keratoconus cornea. Br J Ophthalmol. 2017;101(6):845–50. https://doi.org/10.1136/bjophthalmol-2016-309834.
Schaub F, Hou Y, Zhang W, Bock F, Hos D, Cursiefen C. Corneal crosslinking to regress pathologic corneal neovascularization before high-risk keratoplasty. Cornea. 2021;40(2). https://journals.lww.com/corneajrnl/Fulltext/2021/02000/Corneal_Crosslinking_to_Regress_Pathologic_Corneal.3.aspx.
Moore JE, Schiroli D, Moore CBT. Potential effects of corneal cross-linking upon the limbus. Biomed Res Int. 2016;2016:5062064. https://doi.org/10.1155/2016/5062064.
Moore JE, Atkinson SD, Azar DT, et al. Protection of corneal epithelial stem cells prevents ultraviolet A damage during corneal collagen cross-linking treatment for keratoconus. Br J Ophthalmol. 2014;98(2):270–4. https://doi.org/10.1136/bjophthalmol-2013-303816.
Richoz O, Tabibian D, Hammer A, Majo F, Nicolas M, Hafezi F. The effect of standard and high-fluence corneal cross-linking (CXL) on cornea and limbus. Invest Ophthalmol Vis Sci. 2014;55(9):5783–7. https://doi.org/10.1167/iovs.14-14695.
Vimalin J, Gupta N, Jambulingam M, Padmanabhan P, Madhavan HN. The effect of riboflavin–UV-A treatment on corneal limbal epithelial cells—a study on human cadaver eyes. Cornea. 2012;31(9). https://journals.lww.com/corneajrnl/Fulltext/2012/09000/The_Effect_of_Riboflavin_UV_A_Treatment_on_Corneal.15.aspx.
Seiler TG, Fischinger I, Senfft T, Schmidinger G, Seiler T. Intrastromal application of riboflavin for corneal crosslinking. Invest Ophthalmol Vis Sci. 2014;55(7):4261–5. https://doi.org/10.1167/iovs.14-14021.
Lammer J, Laggner M, Pircher N, Fischinger I, Hofmann C, Schmidinger G. Endothelial safety and efficacy of ex vivo collagen cross-linking of human corneal transplants. Am J Ophthalmol. 2020;214:127–33. https://doi.org/10.1016/j.ajo.2020.02.024.
Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9(7):671–5. https://doi.org/10.1038/nmeth.2089.
Salman A, Ali A, Rafea S, et al. Long-term visual, anterior and posterior corneal changes after crosslinking for progressive keratoconus. Eur J Ophthalmol. 2021. https://doi.org/10.1177/11206721211052878.
Zhu Y, Reinach PS, Ge C, et al. Corneal collagen cross-linking pretreatment mitigates injury-induced inflammation, hemangiogenesis and lymphangiogenesis in vivo. Transl Vis Sci Technol. 2021;10(5):11. https://doi.org/10.1167/tvst.10.5.11.
Hou Y, Le VNH, Tóth G, et al. UV light crosslinking regresses mature corneal blood and lymphatic vessels and promotes subsequent high-risk corneal transplant survival. Am J Transplant. 2018;18(12):2873–84. https://doi.org/10.1111/ajt.14874.
Hamrah P, Liu Y, Zhang Q, Dana MR. The corneal stroma is endowed with a significant number of resident dendritic cells. Invest Ophthalmol Vis Sci. 2003;44(2):581–9. https://doi.org/10.1167/iovs.02-0838.
Adams D. Macrophage activation. In: Roitt IM, Delves PJ, editors. Encyclopedia of immunology. San Diego; 1998. p. 1020–26.
Pavli P, Hume DA, Van De Pol E, Doe WF. Dendritic cells, the major antigen-presenting cells of the human colonic lamina propria. Immunology. 1993;78(1);132–141. https://pubmed.ncbi.nlm.nih.gov/8436399.
Steinman RM. The dendritic cell system and its role in immunogenicity. Annu Rev Immunol. 1991;9:271–96. https://doi.org/10.1146/annurev.iy.09.040191.001415.
Cursiefen C, Schlötzer-Schrehardt U, Küchle M, et al. Lymphatic vessels in vascularized human corneas: immunohistochemical investigation using LYVE-1 and podoplanin. Invest Ophthalmol Vis Sci. 2002;43(7):2127–35.
Hammer A, Richoz O, Arba Mosquera S, Tabibian D, Hoogewoud F, Hafezi F. Corneal biomechanical properties at different corneal cross-linking (CXL) irradiances. Invest Ophthalmol Vis Sci. 2014;55(5):2881–4. https://doi.org/10.1167/iovs.13-13748.
Acknowledgements
Funding
No funding was received in connection with this trial. The journal’s Rapid Service fee was funded by the Medical University of Vienna.
Author Contributions
All authors contributed to the original study conception and design. Material preparation, data collection and analysis were performed by Ruth Donner, and Maria Laggner. The first draft of the manuscript was written by Ruth Donner and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Ruth Donner, Maria Laggner, Julia Aschauer, Jan Lammer and Gerald Schmidinger confirm that they have competing interests to disclose.
Compliance with Ethics Guidelines
This trial was conducted under approval by the Institutional Review Board of the Medical University of Vienna (1578/2013), respecting all applicable ethical guidelines in accordance with the Helsinki Declaration of 1964 and all later amendments. The absence of an objection to organ donation was confirmed with the national opting-out registry prior to enucleation by the Eye Bank Vienna.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Donner, R., Laggner, M., Aschauer, J. et al. Identification of Treatment Protocols for Effective Cross-Linking of the Peripheral Cornea: An Experimental Study. Ophthalmol Ther 11, 2057–2066 (2022). https://doi.org/10.1007/s40123-022-00564-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00564-1