Abstract
Introduction
To quantitatively assess visual performance and patient satisfaction during photochromic contact lens (CL) wear in an indoor environment.
Methods
This observational study comprised 82 eyes of 41 healthy subjects (mean age ± standard deviation, 21.7 ± 0.7 years) who had no ophthalmic diseases except for refractive errors at Kitasato University in 2021. We prospectively compared visual acuity, kinetic visual acuity, functional (time-dependent) visual acuity, the maintaining rate of visual acuity, the response time, contrast sensitivity function, higher-order aberrations, and patient satisfaction score for overall vision in such subjects during photochromic and non-photochromic CL wear in such an environment.
Results
The kinetic visual acuity at 30 km/h was 0.32 ± 0.21 and 0.41 ± 0.24 in the photochromic and non-photochromic CL groups, respectively (p = 0.008). The kinetic visual acuity at 60 km/h was 0.32 ± 0.21 and 0.41 ± 0.24, respectively (p = 0.034). The functional visual acuity was 0.00 ± 0.21 and 0.05 ± 0.25, respectively (p = 0.030). The average response time was 1.19 ± 0.15 s and 1.23 ± 0.15 s, respectively (p = 0.029). The patient satisfaction score for overall visual performance was 4.22 ± 0.11 and 3.59 ± 0.68, respectively (p < 0.001). Otherwise, we found no significant differences in visual acuity, the maintaining rate, higher-order aberrations, or contrast sensitivity function (p = 0.116, p = 0.053, p = 0.371, or p = 0.943). We found no apparent complications such as ocular discomfort, superficial punctate keratitis, conjunctival injection, or infectious keratitis during the observation period.
Conclusions
According to our experience, the photochromic CL showed good visual quality, especially in terms of kinetic and functional visual acuities and subsequent high patient satisfaction, even in an indoor environment, suggesting its viability of visual correction not only in daily activities but also in indoor sports activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Photochromic contact lenses (CLs) are helpful for reducing unpleasant visual symptoms, especially under bright light conditions. |
Nevertheless, detailed visual performance and patient satisfaction during photochromic and non-photochromic CL wear have not been fully understood in an indoor situation. |
What was learned from the study? |
The photochromic CL provided better kinetic and functional visual acuities and subsequent high patient satisfaction than the non-photochromic CL even in an indoor situation. Therefore, it is suggested that it is one of the viable options for vision correction in daily practice. |
Introduction
Our visual system is continuously challenged with the sensitivity to adjust to a wide range of light conditions in modern life [1]. Actually, some patients do experience visual discomfort and visual disability, especially under bright light conditions [2]. Tinted spectacle lenses, namely sunglasses, are beneficial for reducing these symptoms under bright light conditions but can also impair visual performance by absorbing near the peak of visible light under mostly scotopic conditions [3]. Corning first introduced photochromic spectacle lenses in 1962 to rectify such disadvantages by filtering in a dose-dependent manner according to the intensity and wavelength of light in the environment [4]. Furthermore, photochromic contact lenses (CLs) have also been reported to be beneficial for reducing these unpleasant visual symptoms, especially under bright light conditions [2, 5,6,7,8,9,10,11,12]. Recently, new photochromic CLs (ACUVUE® OASYS with Transitions™, Johnson & Johnson Vision, Jacksonville, FL, USA) have been approved for clinical use and have become commercially available in Japan. However, to the best of our knowledge, the detailed visual performance in an indoor environment has not been fully elucidated, except for one study [6], since such CLs were essentially designed to use under sunlight conditions in an outdoor environment. Moreover, not only kinetic visual acuity (KVA) but also functional (time-dependent) visual acuity (FVA) during the photochromic CL wear has not so far been investigated in any environment. Considering that such CLs are widely used under outdoor-sunlight and indoor-light conditions, it may give us intrinsic insight into understanding the detailed visual quality of these contact lens wearers from a clinical viewpoint. This study compares the precise visual performance and patient satisfaction between photochromic and non-photochromic CL wearing eyes in an indoor environment in healthy young subjects.
Methods
Study Population
The study protocol was registered with the University Hospital Medical Information Network Clinical Trial Registry (000047937). This prospective observational study comprised a total of 82 eyes of 41 consecutive subjects who binocularly wore photochromic CLs (ACUVUE OASYS with Transitions™, Johnson & Johnson Vision) (photochromic CL group) and non-photochromic CLs (ACUVUE OASYS, Johnson & Johnson Vision) (non-photochromic CL group) for 1–2 weeks of daily use between September 2021 and November 2021. All subjects were required to have best-corrected visual acuity of 20/20 or better in each eye with the cylindrical correction being limited to 1 diopter (D) or less. Eyes with any history of ocular surgery, ocular trauma, and other concomitant eye diseases were excluded from the study. This research was approved by the Institutional Review Board at Kitasato University (2021-007) and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants after explaining the nature and possible consequences of the study.
Contact Lens Prescription
We prescribed photochromic and non-photochromic CLs composed of the same polymer matrix and senofilcon A in the study population. Both CLs are silicone hydrogel, 2-week disposable CLs, with a base curve of 8.4 mm or 8.5 mm, a CL diameter of 14.0 mm, a water content of 38%, and an oxygen permeability of 121 Dk/L [9]. According to internal data from the manufacturer, only the addition of the photochromic additive technology was different between the two CLs [8].
Outcome Measures
We randomly measured only one eye for each subject for data analysis. We quantitatively assessed visual acuity at 5 m, using a decimal acuity chart of Landolt rings shown under photopic conditions (600 lx) in an indoor environment, kinetic visual acuity (KVA), functional visual acuity (FVA), ocular higher-order aberrations (HOAs), contrast sensitivity (CS) function, subject satisfaction for the overall vision, and adverse events and complications, during photochromic and non-photochromic CL wear in daily use. All examinations were conducted by experienced ophthalmic technicians who were masked to the clinical condition of the subjects and the preliminary results of the study.
Kinetic Visual Acuity
We measured the KVA using a kinetic visual acuity meter (AS-4Fα, Kowa,
Aichi, Japan) with the best spectacle correction, as described previously [13, 14]. In brief, the participants were instructed to look through the measuring window. They would detect the Landolt ring of 20/60 in a bright white circular shape. The Landolt ring moved towards the subjects from a 50 m distance at a velocity of 30 and 60 km/h. The participants were asked to respond by pressing a joystick when they immediately identified the Landolt ring's orientation. The results were expressed as decimal visual acuity according to the distance of the participant’s response. After 2 practice rounds to reduce mistakes due to unfamiliarity with the test, the participants carried out three trials at two velocities under the same conditions, with a 1-min rest between each set. After converting decimal acuity to logMAR visual acuity, the average value was used for analysis.
Functional Visual Acuity
We also measured the FVA using a functional visual acuity measurement system (AS-28, Kowa, Aichi, Japan) to assess the time-course of continuous changes in visual acuity, as described previously [15,16,17]. In brief, the baseline of visual acuity was primarily determined for each patient. The subjects delineated an automatically presented Landolt ring orientation using a joystick. Optotype size was changed in single steps depending on the patient's responses: the optotype was enlarged when the response was incorrect and reduced when the response was correct. When there was no response within 2 s, the answer was recorded as an error, and the optotype was enlarged. The test was continuously conducted for 1 min under spontaneous blinking. We obtained several quantitative metrics from the FVA measurements, such as the FVA, the visual maintenance ratio (VMR), and the average response time. The FVA was defined as the average of all visual acuity values measured over time. This average value may reflect daily vision more efficiently than the visual acuity measured at a specific time point. The VMR was defined as FVA divided by baseline visual acuity [17].
Ocular Higher-Order Aberrations
We measured ocular higher-order aberrations (HOAs) for a 5-mm pupil using a standard wavefront aberrometer (OPD-Scan II, Nidek, Aichi, Japan). The root-mean-square (RMS) of the third-order Zernike coefficients was utilized to represent third-order aberrations. The RMS of the fourth-order coefficient was used to describe fourth-order aberrations. Total HOAs were calculated as the RMS of the third- and fourth-order coefficients.
Contrast Sensitivity Function
We measured the CS function using a contrast sensitivity unit (Functional Acuity Contrast Test, F.A.C.T., Stereo Optical, Chicago, IL, US) with the best spectacle correction at 45 cm, at 3, 6, 12, and 18 cycles, under photopic (600 lx) and mesopic (10 lx) conditions [18]. Finally, we calculated the area under the log contrast sensitivity function (AULCSF) from the obtained CS data, as described previously [19]. In brief, the log of CS was plotted as a function of log spatial frequency, and third-order polynomials were fitted to the data. The fitting curve was integrated, and the resultant value was defined as the AULCSF.
Satisfaction Score
We also evaluated the patient satisfaction score for the overall vision, using visual analogue scale (VAS) symptom intensity scores on a scale of 0 (no satisfaction) to 5 (maximum satisfaction) in both groups [20].
Statistical Analysis
We first checked the normality of all data samples by the Shapiro–Wilk test using statistical software (Bellcurve for Excel, Social Survey Research Information Co, Ltd., Tokyo, Japan). Because all data did not fulfill the criteria for normal distribution, the Wilcoxon signed-rank test was applied to compare the data between the two groups. The Fisher’s exact test was also used to compare the percentages between the two groups. Unless otherwise indicated, the results are expressed as mean ± standard deviation, and a value of p < 0.05 was deemed statistically significant.
Results
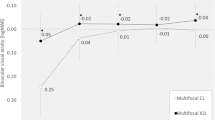
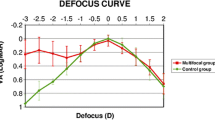
Table 1 shows the baseline demographics of the study population. Table 2 shows the detailed visual performance and subject satisfaction in the photochromic and non-photochromic contact lens groups Kinetic visual acuity (30 and 60 km/h), functional visual acuity, and patient satisfaction score were significantly better in the photochromic CL group than that in the non-photochromic CL group (Wilcoxson signed-rank test, p = 0.008, p = 0.034, p = 0.030, and p < 0.001). The response time was significantly shorter in the photochromic CL group than that in the non-photochromic CL group (p = 0.024). Otherwise, we found no significant differences in visual acuity, the maintaining rate, higher-order aberrations, or contrast sensitivity function (p = 0.116, p = 0.053, p = 0.371, or p = 0.943). We found no apparent complications such as ocular discomfort, superficial punctate keratitis, conjunctival injection, or infectious keratitis during the observation period. Figures 1 and 2 show CS function according to 3, 6, 12, and 18 cycles/degree under bright and mesopic light conditions, respectively. We found no significant differences between the two groups under bright or mesopic light conditions at all spatial frequencies. We found no apparent complications such as ocular discomfort, superficial punctate keratitis, conjunctival injection, or infectious keratitis during the observation period.
Discussion
In the current study, our findings showed that the photochromic CL provided good visual quality, especially in terms of kinetic and functional visual acuities, and subsequent high patient satisfaction, in healthy young subjects. Therefore, our results may support the view that it is one of the viable alternatives for vision correction in daily activities and indoor sports activities. Although we did not confirm the spectral transmittance curve of the photochromic CL, we assume that this CL would be minimally activated in this indoor environment. Thus, the beneficial effect of the photochromic CL in an indoor environment would be much smaller than that in an outdoor environment.
There have so far been only a few studies on this new commercially available photochromic CL (ACUVUE® OASYS with Transitions™) wear in a clinical setting [6, 8, 9]. Renzi-Hammond et al. first showed that this photochromic CL improved visual performance compared with the non-photochromic control across all visual functions tested, even under conditions of exiguous activation [6]. Hammond et al. also showed that both photochromic inactivated and activated CLs reduced signs of dysphotopsia, and two-point thresholds for younger and middle-aged adults compared with a non-photochromic CL difference tended to increase with age [8]. Based on the fact that the older eye has more scatter, the beneficial effect of the photochromic CL in older subjects would be more prominent than that in younger subjects. Buch et al. stated that more than 95% of subjects were successfully fitted with this new photochromic CL based on the professional judgment of physiology, mechanical fitting, comfort, vision, and handling [6].
With regard to photochromic CLs, Buch et al. [5] found no apparent evidence of concerns with either driving performance or vision while wearing photochromic CLs. However, the sample size was relatively small. Renzi-Hammond et al. [2] demonstrated that the photochromic CL is a viable means of improving aspects of optimal vision in a complex environment, especially in terms of photostress recovery, glare disability, glare discomfort, and chromatic contrast thresholds. They found that the improvement in glare disability, glare discomfort, and chromatic contrast was about half of what we had previously seen using similar measures but an activated photochromic lens (improvements around 15% vs. around 30%) [10]. In addition, Hammond et al. showed that the photochromic CL improved the ability to resolve the separation of two small bright points of light and that this effect was reduced in magnitude but still apparent even when the photochromic CL was not activated [7]. Interestingly, Alabi et al. and Moon et al. found, using CL and spectacle lens photochromic bench, respectively, that the temperature can influence both the activation and deactivation of photochromic lenses such that the higher the temperature, the greater the light transmission [11, 12]. However, the clinical usefulness or the feasibility of the photochromic CL has not been fully elucidated, except for one study, in an indoor environment [6]. Moreover, the detailed visual performance, such as the KVA or the FVA, has not so far been evaluated. Our findings indicate that the photochromic CL is superior to the non-photochromic CL in indoor visual quality, especially in terms of kinetic and functional visual acuities and subsequent high patient satisfaction, even in an indoor environment. It has been reported that short-wave light had an exaggerated effect on light-induced discomfort [21]. Although we have no clear explanation for this discrepancy at this time, we speculate that the lower transmission rate in the wavelength of around 400 nm might be beneficial for reducing various light discomforts, even in an indoor light conditions. We also speculate that this advantage of the photochromic CL over the non-photochromic CL will become more apparent in an outside sun-light environment [6, 7] or in middle-aged patients [8]. To our knowledge, this is the first published study to directly compare the detailed visual performance and patient satisfaction between the photochromic and non-photochromic CL-wearing eyes. We believe that this information is simple but clinically helpful for grasping the real-world condition of such promising CL treatments even in an indoor environment. Moreover, it will be beneficial for improving indoor visual quality in daily activities and sports activities. We are currently conducting a new study on the detailed visual performance and patient satisfaction during the photochromic CL wear in outdoor sun-light conditions, presumably because the advantages of the photochromic CL over the non-photochromic CL may become more prominent in an outdoor environment.
There are several limitations to this study. Firstly, all study participants were young in consideration of the preference for CL wear. The participants were mostly composed of our university students. Hammond et al. showed that the photochromic CL reduced the signs of dysphotopsia and two-point thresholds for younger and middle-aged adults and that the differences tended to increase with age [8]. A further study with various ages is necessary to clarify this point. Secondly, we performed this study in a single-arm, unmasked fashion, primarily due to the ethical consideration and the subjective easiness of identifying the type of CLs. Therefore, some study bias may exist, especially in terms of subjective outcomes. It would be ideal to perform a randomized controlled trial to confirm the authenticity of the results. Thirdly, we did not precisely control the degree of the light filtering and the activation of the photochromic CLs in the present study. However, we believe that this study reflects the actual status of visual quality more accurately since the photochromic CL will be widely used in an outside situation and an indoor situation in daily practice.
Conclusion
In summary, our results showed that the photochromic CL provided good visual quality, especially in terms of kinetic and functional visual acuities and subsequent high patient satisfaction, even in an indoor environment, in a healthy young population. Accordingly, our results may support the view that it is one of the viable alternatives for vision correction in daily activities and indoor sports activities.
References
Laughlin SB. Retinal information capacity and the function of the pupil. Ophthalmic Physiol Opt. 1992;12(2):161–4.
Renzi-Hammond L, Buch JR, Cannon J, Hacker L, Toubouti Y, Hammond BR. A contra-lateral comparison of the visual effects of a photochromic vs non- photochromic contact lens. Cont Lens Anterior Eye. 2020;43(3):250–5.
Huang L, Seiple W, Park RI, Greenstein VC, Holopigian K, Naidu SS, Stenson SM. Variable tinted spectacle lenses: a comparison of aesthetics and visual preference. CLAO J. 2001;27(3):121–4.
Dürr H, Bouas-Laurent H. Photochromism: molecules and systems. Hoboken: Elsevier; 2003.
Buch JR, Toubouti Y, Cannon J. Randomized crossover trial evaluating the impact of senofilcon a photochromic lens on driving performance. Optom Vis Sci. 2020;97(1):15–23.
Renzi-Hammond LM, Buch JR, Hacker L, Cannon J, Hammond BR Jr. The effect of a photochromic contact lens on visual function indoors: a randomized. Controlled Trial Optom Vis Sci. 2020;97(7):526–30.
Hammond BR, Buch J, Hacker L, Cannon J, Toubouti Y, Renzi-Hammond LM. The effects of light scatter when using a photochromic vs. non-photochromic contact lens. J Optom. 2020;13(4):227–34.
Hammond BR, Buch J, Sonoda L, Renzi-Hammond L. The effects of a senofilcon a contact lens with and without a photochromic additive on positive dysphotopsia across age. Eye Contact Lens. 2021;47(5):265–70.
Buch JR, Sonoda L, Cannon JL. Lens fitting and subjective acceptance of senofilcon A with photochromic additive on a neophyte population. Cont Lens Anterior Eye. 2021;44(4): 101369.
Renzi-Hammond L, Buch JR, Cannon J, et al. A contra-lateral comparison of the visual effects of a photochromic vs non-photochromic contact lens. Cont Lens Anterior Eye. 2019;43:250–5.
Alabi EB, Simpson TL, Harris T, Whitten K. Determining the spectral transmittance of photochromic contact lenses. Cont Lens Anterior Eye. 2021;44(5): 101406.
Moon BY, Kim SY, Yu DS. Differences in the optical properties of photochromic lenses between cold and warm temperatures. PLoS ONE. 2020;15(5): e0234066.
Kato S, Shimizu K, Igarashi A, Kawamorita T. Kinetic visual acuity, stereopsis, and ocular deviation with an implantable collamer lens. J Cataract Refract Surg. 2019;45(12):1777–81.
Iehisa I, Negishi K, Ayaki M, Tsubota K. Kinetic visual acuity is correlated with functional visual acuity at higher speeds. BMJ Open Ophthalmol. 2019;4(1): e000383.
Hiraoka T, Hoshi S, Okamoto Y, Okamoto F, Oshika T. Mesopic functional visual acuity in normal subjects. PLoS ONE. 2015;10(7): e0134505.
Ozeki N, Yuki K, Shiba D, Tsubota K. Evaluation of functional visual acuity in glaucoma patients. J Glaucoma. 2017;26(3):223–6.
Hiraoka T, Miyata K, Hayashidera T, Iida M, Takada K, Minami K, Oshika T. Influence of intraocular lens subsurface nanoglistenings on functional visual acuity. PLoS ONE. 2017;12(3): e0173574.
Boxer Wachler BS, Durrie DS, Assil KK, Krueger RR. Role of clearance and treatment zones in contrast sensitivity: significance in refractive surgery. J Cataract Refract Surg. 1999;25(1):16–23.
Applegate RA, Howland HC, Sharp RP, Cottingham AJ, Yee RW. Corneal aberrations and visual performance after radial keratotomy. J Refract Surg. 1998;14:397–407.
Lim AT, Edis G, Kranz H, Mendelson G, Selwood T, Scott DF. Postoperative pain control: contribution of psychological factors and transcutaneous electrical stimulation. Pain. 1983;17(2):179–88.
Stringham JM, Fuld K, Wenzel AJ. Action spectrum for photophobia. J Opt Soc Am A Opt Image Sci Vis. 2003;20(10):1852–8.
Acknowledgements
We thank Masashi Ozaki, Natsu Furuta, Takumi Aoki, and all study participants for their involvement in the study.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. No funding or sponsorship was received for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Kazutaka Kamiya and Shuya Suzuki were involved in the design and conduct of the study, Kazutaka Kamiya, Shuya Suzuki, and Fusako Fujimura were involved in the collection, management, analysis, and interpretation of data, and all authors were involved in preparation, review, and final approval of the manuscript.
Disclosures
Kazutaka Kamiya, Shuya Suzuki, and Fusako Fujimura declare that they have no conflict of interest related to this work.
Compliance with Ethics Guidelines
This research was approved by the Institutional Review Board at Kitasato University (2021-007) and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants after explaining the nature and possible consequences of the study.
Data Availability
The datasets analysed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kamiya, K., Suzuki, S. & Fujimura, F. Effect of Photochromic Contact Lens Wear on Indoor Visual Performance and Patient Satisfaction. Ophthalmol Ther 11, 1847–1855 (2022). https://doi.org/10.1007/s40123-022-00552-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00552-5