Abstract
Introduction
To compare 1-year outcomes of CO2 laser-assisted sclerectomy surgery (CLASS) alone or combined with phacoemulsification (CLASS + Phaco) in eyes with primary open-angle glaucoma (POAG).
Methods
This was a prospective, comparative, case series study. A total of 46 eyes with POAG underwent CLASS or CLASS + Phaco were followed up for 1 year. The primary outcomes included changes in intraocular pressure (IOP), medication and best corrected visual acuity (BCVA). The secondary outcomes were success rate, functional bleb, postoperative laser intervention and complications.
Results
CLASS alone resulted in a greater IOP reduction compared with CLASS + Phaco. BCVA improved remarkably in CLASS + Phaco group, but there was no difference in BCVA before and after CLASS. The number of antiglaucoma medications significantly decreased at 12 months postoperatively in both groups. Functional blebs were more commonly seen in the CLASS than combination group. The overall success rate was higher in the CLASS than CLASS + Phaco group at 1 year after surgery. The incidence of peripheral anterior synechiae (PAS) in CLASS + Phaco group was significantly lower than that of CLASS alone.
Conclusion
CLASS alone achieved a greater IOP reduction, more common functional bleb formation and a higher success rate compared to CLASS combined with Phaco, while combination surgery yielded a better BCVA improvement and a lower PAS incidence than CLASS alone. Both surgical strategies have favorable safety and efficacy among POAG patients. Combined surgery could be a viable option for patients with co-existing POAG and cataract.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What carry out this study? |
CLASS has been proved to be a safe and effective approach for POAG patients. The available data comparing CLASS alone and combined with Phaco are relatively scarce, especially in Chinese patients. We compared the 1-year outcomes between CLASS and CLASS + Phaco. |
What was learned from the study? |
CLASS alone achieved a greater IOP reduction, more common functional bleb formation and higher success rate than CLASS combined with Phaco, while combination surgery yielded better BCVA improvement and lower PAS incidence than CLASS alone. |
Both surgical strategies have favorable safety and efficacy among POAG patients. Combined surgery could be a viable option for patients with co-existing POAG and cataract. |
Introduction
Glaucoma is the second leading cause of blindness worldwide [1]. It was estimated that, in those aged ≥ 50 years, 3.6 million were blind because of glaucoma in 2020 [2], and the number will increase to 111.8 million by 2040 [3]. Asia accounts for about 60% of the global glaucoma population [4]. POAG is one of the most common forms of glaucoma [3].
There are several risk factors involved in pathogenesis of POAG, including increased IOP, oxidative stress, excitotoxicity, ocular blood flow, etc. [5, 6]. However, lowering IOP is the most effective treatment [1, 5]. This is commonly achieved through medication, laser and surgical modalities [7]. Trabeculectomy (Trab) remains the gold standard for glaucoma surgery [8]. However, due to the risk of potential complications, there has been a substantial decrease in Trab during the past 5 years in China [9]. Nonpenetrating deep sclerectomy (NPDS) is an alternative filtering surgery, which achieves IOP reduction by increasing aqueous outflow through a thin trabeculo-Descemet window (TDW) into a surgically created scleral lake, without penetrating the anterior chamber [10]. However, a long learning curve is required for the technique, and a high incidence of perforation during the procedure results in low popularity of NPDS [11]. CLASS is an optimized approach to NPDS. Using a CO2 laser to ablate the scleral tissue instead of a manual procedure, CLASS is less technically challenging and safer compared with NPDS [12].
The incidence of glaucoma increases with age [13]. Therefore, glaucoma and cataract often co-exist in patients. If IOP cannot be controlled under maximal medication, surgery should be initiated for these patients, and combination surgery seems to be the recommended method [14]. It has been proved that NPDS combined with phacoemulsification (NPDS + Phaco) is superior to NPDS alone owing to greater safety and IOP and medication reduction [15].
As a modified NPDS, CLASS has been used successfully to treat POAG in recent years [15, 16]. In our previous study, we reported a total success rate of 95.7% at 12 months after CLASS [17]. To date, the available data comparing CLASS alone or combined with Phaco have been relatively scarce. There was only one previous study conducted in Asian glaucoma patients, which indicated equal safety and effectiveness between the two surgical approaches. There is still no conclusion about whether combination surgery is better than CLASS alone, just like with conventional NPDS.
In this study, we compared the 1-year outcomes between CLASS alone and combined with Phaco, expecting to provide some valuable information for surgeons when dealing with patients with co-existing glaucoma and cataract.
Methods
Study Design
This was a prospective, comparative, interventional case series study. All patients were recruited from our eye center between August 2020 to February 2022. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Ethical approval was obtained from the Ethics Committee of the Second Affiliated Hospital of Zhejiang University (2020-ER721).
The inclusion criteria were: patients aged ≥ 18 years, diagnosed with POAG, with uncontrolled IOP under maximum antiglaucoma agents and no other ocular disorders except for cataract. The exclusion criteria were: patients with other systematic or ocular disorders, ocular trauma or secondary glaucoma, or history of any ocular surgery or laser treatment. Patients with a visually significant cataract were assigned to the combination group; otherwise, CLASS alone was advocated. The decision about which procedure to perform was determined by the ophthalmologist and patient after thorough discussion of the risks and benefits of each surgery. Written informed consent was obtained from all the subjects prior to participation.
The patients underwent a baseline examination within 2 days before the surgery and were followed up at 1 week (W), 2 W, 1, 3, 6, 9 and 12 months (M) postoperatively. At each visit, BCVA was examined with the standard logarithmic visual acuity chart and converted to the logarithm of minimum angle of resolution (log MAR) equivalents; IOP was recorded as an average of three consecutive measurements with Goldmann applanation tonometry (GAT AT900, Haag Streit, Köniz, Switzerland); slit-lamp examination, gonioscopy and fundus examination were performed by the same experienced ophthalmologist. Ultrasound biomicroscopy (UBM) was performed at 1, 3, 6, 9 and 12 M and other situations of unexpected IOP elevation. Visual field test (Octopus 900, Haag-Streit, USA) was evaluated at baseline, 6 and 12 M postoperatively. Cataract was graded using the Lens Opacity Classification System III (LOCS III) at the slit-lamp after dilation of the pupil. Severity of glaucoma was assessed by visual field (VF) damage and classified into three categories: early glaucoma (mean defect, MD ≤ 6 dB), moderate glaucoma (6 < MD ≤ 12 dB) and advanced glaucoma (MD > 12 dB) according to the Terminology and Guidelines of Glaucoma (European Glaucoma Society, 5th edition).
Surgical Procedure
All procedures were performed by a single surgeon (KJ Wang) under topical anesthesia with Alcaine (s.a. Alcon-Couvreur n.v., Belgium) and subconjunctival anesthesia with 0.2 ml 2% lidocaine (Zhaohui Pharmaceutical, Shanghai, China).
CLASS
CLASS was performed as described previously [17]. In detail, a fornix-based conjunctival flap was created to expose the sclera, and then a one-third thickness 5 mm × 5 mm scleral flap was made and extended by 1 mm into the clear cornea. Mitomycin C (MMC) (0.4 mg/ml) was applied under the conjunctival and scleral flaps for 3 min, and the area was washed with 20 ml balanced salt solution (BSS). A 4 × 2-mm scleral lake was created at the posterior scleral bed using a commercially available OT-135P2 CO2 laser system (IOPtiMate, IOPtima Ltd., Ramat Gan, Israel), with the depth of approximately 90% scleral thickness. MMC was applied again on the scleral lake for 1 min and washed out by BSS. Then, the CO2 laser beam was applied to ablate the outer wall of Schlemm’s canal until a continuous fluid percolation was observed. Finally, the two corners of the scleral and conjunctival flap were sutured with 10/0 nylon sutures.
CLASS + Phaco
After pupillary dilation and topical anesthesia, a fornix-based conjunctival flap was created to expose the sclera, and then a one-third thickness limbus-based 5 × 5-mm scleral flap was made and extended by 1 mm into the clear cornea. MMC (0.4 mg/ml) was applied under the conjunctival and scleral flaps for 3 min and washed with 20 ml BSS. A 1.0-mm side incision was performed, and the viscoelastic material was injected into the anterior chamber. After that, a 1.8-mm corneal incision was made, and a 5.0-mm-diameter capsulotomy was performed with a capsulorhexis forceps. After hydrodissection, a standard phacoemulsification was performed using the Stellaris system (Stellaris; Bausch & Lomb, Rochester, New York), followed by cortex removal using automated irrigation/aspiration and final intraocular lens (IOL) implantation in the capsular bag. Corneal incisions were hydrated with balanced salt solution for watertightness. Then, CLASS procedure was performed as we mentioned above until the end of the surgery.
Postoperative Management
For both groups, tobramycin and dexamethasone were prescribed postoperatively four times a day (QID) for 1 month, and pilocarpine eyedrops were used QID for 3 months. Postoperative interventions were described as previously [17]. At each visit, if PAS at the filtrating area was confirmed by gonioscopy and UBM examination, a Nd:YAG laser synechiolysis was performed in clinic to remove iris obstruction and reopen the filtration site. If the postoperative IOP raised above the desired target IOP or the evidence of scleral reservoir reduction was observed by UBM examination, a Nd:YAG laser goniopuncture (LGP) was performed immediately in clinic to enhance the IOP-lowing effect. IOP was measured within 10 min after laser intervention to confirm the IOP-lowing effect. IOP values before laser intervention were included for mean IOP evaluation at each time point, and IOP values after laser intervention were included for success criteria. In patients with iris incarceration, surgical repositioning was carried out to pull the prolapsed iris centrally. Subconjunctival injection of 5-fluorouracil (5-FU, 0.2 ml, 25 mg/ml) and needling were conducted in the presence of scarring up in the filtrating area to inhibiting fibroblast proliferation for some patients.
Therapeutic Outcomes and Success Criteria
The efficacy evaluation included the IOP reduction, changes in antiglaucoma medications before and after surgery and success rate. Fixed combination medications were recorded as two types of agents. The safety assessment consisted of BCVA and visual field (MD) changes, proportions of postoperative interventions and any intra- and postoperative complications.
“Complete success” (CS) was defined as 5 ≤ IOP < 18 mmHg and ≥ 20% IOP reduction from the baseline, without hypotensive medications or any interventions (including laser treatment, surgical repositioning or needling). “Qualified success” (QS) referred to IOP values within the above criteria after postoperative interventions or with hypotensive medications. “Failure” (F) was defined as IOP < 5 mmHg or > 18 mmHg despite postoperative intervention or hypotensive medications, or < 20% IOP reduction from the baseline or underwent additional glaucoma surgery within 1 year.
Statistical Analysis
Statistical analyses were performed with the GraphPad Prism version 9.0 software (GraphPad Software Incorporation, San Diego, CA, USA). The sample size was calculated based on a power calculation (power = 0.80; P = 0.05) using IOP reduction% at 1 year after surgery obtained in a previous study [22], and 21 eyes per group were considered well suited for the purpose of this study. Quantitative data were expressed as mean values ± standard deviation (mean ± SD). Normality was tested by means of D’Agostino and Pearson normality test. The Kruskal-Wallis test followed by Dunn’s post-hoc analysis were used to compare IOP values and medications before and after surgery. The Wilcoxon matched-pairs signed rank test was applied to compare changes of BCVA and mean defect (MD) from baseline. The Mann-Whitney U test was used to compare parameters between the two groups. The chi-squared test was used to compare incidence of complications between the two groups. The cumulative probability of success was illustrated using Kaplan-Meier survival curves, and log-rank test was used for group comparisons. P value < 0.05 was considered statistically significant.
Results
Baseline Characteristics
A total of 56 patients were initially recruited, and 46 of them, who completed surgical treatment (n = 23 in each group) and the 1-year follow-up data collection, were finally included for analysis (Fig. 1). Demographic data and baseline characteristics are described in Table 1.
Efficacy Evaluation
Changes in IOP
Both CLASS alone and CLASS + Phaco groups led to significant IOP reduction postoperatively (Fig. 2A). Although there was no significant difference in the mean IOP between the two groups at 12 M after surgery, CLASS alone resulted in a greater IOP reduction compared with CLASS + Phaco (Table 2, 54.5% vs 26.2%, P < 0.01).
Changes in Antiglaucoma Medications
Antiglaucoma medication was discontinued for all patients at the early stage after surgery. During the 12 M follow-up period, we preferred to use laser intervention or needling to deal with IOP elevation rather than antiglaucoma medications. As shown in Fig. 1B and Table 2, the number of medications significantly decreased at 12 M postoperatively for both CLASS and CLASS + Phaco group (P < 0.01, compared with baseline).
Association of Bleb and IOP
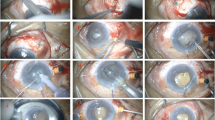
Comparing the two groups, functional blebs were more common in patients after CLASS (14/23, 60.9%) than in patients after CLASS + Phaco (2/23, 8.7%, Fisher’s exact test, P < 0.01, Table 3 and Fig. 3). There was no significant difference in relevant parameters between patients with and without bleb in CLASS + Phaco group. However, in CLASS group, the final IOP at 12 M was significantly lower and the IOP reduction% was higher in patients with bleb than in patients without bleb (P < 0.05). Meanwhile, patients with bleb had fewer medications at 12 M after CLASS (P < 0.05).
Comparison of function bleb in CLASS combined with or without Phaco. Slit-lamp examination (A1–C1) and ultrasound biomicroscopy (UBM) examination (A2–C2) of patients without bleb in CLASS + Phaco group; slit-lamp examination (D1–F1) and UBM examination (D2–F2) of patients with functional bleb in CLASS group
Success Rate
Supplementary Table 1 showed the success rate at each time point in both groups after surgery. The overall success rate (CS + QS %) was higher in CLASS group than in CLASS + Phaco group at each time point after surgery. At 12 M after surgery, the CS% and QS% were 69.6% and 26.1% in CLASS group, while only 34.8% CS% and 17.4% QS% were explored in CLASS + Phaco group.
Figure 4 showed the Kaplan-Meier plots of the cumulative probability of complete success (A) and qualified success (B) in both groups during the 1-year follow-up. IOP values after laser intervention were included for analysis. Failure was defined as IOP > 18 mmHg or IOP reduction < 20% from baseline at any time-point, and qualified success in Kaplan-Meier survival analysis was defined as 5 ≤ IOP < 18 mmHg and ≥ 20% IOP reduction from the baseline with or without antiglaucoma medication (CS + QS). The estimated complete success rate was 60.9% in CLASS group and 26.1% in CLASS + Phaco group (P = 0.01), and the estimated qualified success rate at 12 M was 87.0% in CLASS group and 32.5% in CLASS + Phaco group, with statistical significance (P < 0.01).
Safety Assessment
Changes in Visual Acuity and Visual Field
Postoperatively, BCVA improved remarkably in CLASS + Phaco group, but there was no significant difference in BCVA before and after CLASS. The mean defect (MD) of visual field remained unchanged for both CLASS and CLASS + Phaco group at 1 year postoperatively (Table 2).
Incidence of PAS
Comparing the two groups, the total incidence of PAS in CLASS + Phaco group (5/23, 21.7%) was significantly lower than in CLASS group (17/23, 73.9%, P < 0.01, Supplementary Table 2). During the 1-year follow-up, the PAS incidence ranged from 0 to 47.8% in CLASS alone group, with a peak occurring at 1 month postoperatively. Only 0 to 8.7% of PAS incidence was found in CLASS + Phaco group (Table 4).
Scleral Reservoir Reduction
In CLASS group, 7/23 (30.4%) patients developed scleral reservoir reduction during the 1-year follow-up period, and LGP treatment was performed to enhance the IOP-lowing effect (Supplementary Table 2). As for CLASS + Phaco group, 8/23 (34.8%) patients underwent LGP treatment. There was no significant difference in the proportion of eyes treated with LGP between the two groups (Table 4, P > 0.05).
Intra- and Postoperative Complications
In CLASS group, one eye (4.3%) exhibited intraoperative micro-perforation. This patient developed iris incarceration and underwent surgical repositioning at 2 M after surgery. Subconjunctival injection of 5-FU and needling were performed in one patient (4.3%). One patient (4.3%) developed shallow anterior chamber. No other complications were observed.
In CLASS + Phaco group, uneventful CLASS and cataract surgery were performed for all patients. Subconjunctival injection of 5-FU and needling were performed in one patient (4.3%). No other complications were observed.
Discussion
In this study, we presented a comparison of safety and efficacy in POAG patients who underwent CLASS alone or combined with Phaco. The results showed that CLASS alone achieved a greater IOP reduction, more common functional bleb and higher success rate compared with CLASS + Phaco. Meanwhile, combination surgery showed a better BCVA improvement and a lower PAS incidence than CLASS alone. Medication reduction, proportion of LGP interventions and complications were comparable in both groups during the 1-year follow-up.
CLASS is a modified NPDS, which has been used in POAG patients for decades and has attracted increasing attention in China during recent years [16, 18]. It has been proved to be as efficient as NPDS in terms of IOP-lowing effect [18]. Compared with traditional Trab, CLASS also showed similar IOP-lowing effect in Chinese POAG patients [19]. As for combination surgery, previous reports about 1-year outcomes of CLASS combined with or without Phaco were summarized in Table 5. Yu et al. reported a 39% IOP reduction in a group of Chinese POAG patients after CLASS + Phaco [20]. Villavicencio et al. demonstrated that CLASS + Phaco achieved a greater IOP reduction compared with Trab + Phaco (45.2% vs 37.7%) [21]. However, only 6.7% IOP reduction in combination group was reported by Ho et al. in 2021, which was significantly lower than in CLASS group (40.6%) [22]. In our study, a greater IOP reduction was found in CLASS alone group compared with combination group (54.5% vs 26.2%). The differences in baseline IOP and sample size might contribute to the inconsistency with previous studies.
Success rate was a common index to evaluate the long-term effect of a surgery. The definition of success in our study was modified based on previous studies [23] to distinguish the proportion of patients transformed from QS to CS after postoperative Nd:YAG laser intervention [17]. The overall success rate (CS + QS%) in our study was consistent with the qualified success rate (QS%) in previous studies. Comparing CLASS alone and Class + Phaco, the success rate in standalone group was significantly higher than in combination group in our current study, which was consistent with a previous Singapore study [22]. The 1-year success rate of combination surgery varied significantly among previous studies. Villavicencio et al. reported a success rate of 97.2% in a Caucasian population [21]. A study by Rajia et al. reported similar results in a group of Indian patients, with a CS% of 85.7% and a QS% of 92.3% at 1 year after CLASS + Phaco [24]. In contrast, only 46.4% qualified success was reported by Ho et al. in Asian glaucoma patients from Singapore [22]. However, Yu et al. reported an overall success rate of 88.0% in a Chinese population [20]. Our study yielded similar results in CLASS group, but a lower CS% and QS% in CLASS + Phaco group. The inconsistency could stem from several factors. First, the response of scleral tissue to laser may be different between Chinese and Caucasian patients [23]. Second, most of the patients recruited in our study were advanced glaucoma patients. A longer-term usage of multiple antiglaucoma medications might lead to a greater inflammatory reaction and higher scarring tendency [25]. In addition, success rate was calculated based on baseline IOP in our study (IOP reduction of ≥ 20% from baseline). The baseline IOP in CLASS group was significantly higher than in combination group. Some patients in the CLASS + Phaco group had a baseline IOP within the normal range under maximum medications and reached a target IOP without medications after surgery, which would be categorized as a failure, due to a < 20% IOP reduction. These factors might result in a lower postoperative success rate in CLASS + Phaco group.
PAS was a common complication after CLASS. The incidence of PAS ranged from 0.0 to 30.7% among previous studies, with a higher rate of PAS in Chinese compared with Caucasian patients [17]. In our study, the incidence of postoperative PAS was significantly lower in combination group than in CLASS alone. As we know, the TDM has a narrow and thin membrane near the iris root. A high prevalence of narrow angles (36.9%) was found in mainland population aged > 50 years [26], which might contribute to the high risk of PAS after CLASS. Cataract surgery can deepen anterior chamber and increase the width of anterior chamber angle in Chinese subjects [27]. Meanwhile, a younger age and higher baseline IOP also increased the risk of PAG in CLASS group. We speculate that these may be reasonable explanations for the lower incidence of PAS in combination group.
The mechanism of IOP reduction after NPDS is complicated. There may be several aqueous humor drainage pathways, including subconjunctival bleb, trabecular meshwork, intrascleral outflow and suprachoroidal outflow [28]. It has been reported that the subconjunctival and suprachoroidal pathway may be the main mechanisms to achieve IOP reduction after CLASS [29]. In our study, functional bleb was more common in CLASS group than in combination group (60.9% vs 8.7%), which contributed to a greater IOP-lowing effect. In a 5-year comparison study, there were more eyes with a significantly higher and more extensive bleb in the trabeculectomy group than in the phacotrabeculectomy group [30]. So far, to our knowledge, this is the first study evaluating the filtering bleb and exploring the mechanisms of IOP reduction between CLASS alone and combined with Phaco, which deserves further attention.
Study Limitations
The study has certain limitations. First, this was a prospective, interventional case series study, without age-matched control and randomized assignment. Selection bias resulted in a significant difference in several baseline parameters, which might affect the outcomes between the two groups. Second, a limited sample size was included in our study, and the 1-year follow-up period was relatively short to provide strong evidence in glaucoma studies. Furthermore, bleb assessment using Moorfields bleb grading system (MBGS) or the Indiana Bled Appearance grading scale (IBAGS) was not included in our study. Therefore, we advocate that a large-scale, multi-center, randomized controlled trial (RCT) should be conducted to verify the safety and effectiveness comparing CLASS alone and combined with Phaco. UBM examination combined with clinical grading scale can provide more useful information and help to evaluate the mechanisms after CLASS in our future study.
Conclusion
In summary, this study contributes a novel comparison between CLASS alone and CLASS + Phaco. Our results suggested that both surgical strategies have favorable safety and efficacy for POAG patients. CLASS alone achieved greater IOP reduction, more common functional bleb formation and higher success rate, while CLASS + Phaco yielded better BCVA improvement and lower PAS incidence. Combined surgery could be a viable option for patients with co-existing POAG and cataract.
References
Quigley HA. Glaucoma. Lancet. 2011;377(9774):1367–77. https://doi.org/10.1016/S0140-6736(10)61423-7.
Blindness GBD, Vision Impairment C, Vision Loss Expert Group of the Global Burden of Disease S. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9(2):e144–60. https://doi.org/10.1016/S2214-109X(20)30489-7.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–90. https://doi.org/10.1016/j.ophtha.2014.05.013.
Reis TF, Paula JS, Furtado JM. Primary glaucomas in adults: epidemiology and public health—a review. Clin Exp Ophthalmol. 2022;50(2):128–42. https://doi.org/10.1111/ceo.14040.
Erichev VP, Khachatryan GK, Khomchik OV. Current trends in studying pathogenesis of glaucoma. Vestn Oftalmol. 2021;137(5. Vyp. 2):268–74. https://doi.org/10.17116/oftalma2021137052268.
Wu X, Katarzyna K, Liu X, et al. Role of ocular blood flow in normal tension glaucoma. Adv Ophthalmol Pract Res. 2022. https://doi.org/10.1016/j.aopr.2022.100036.
Fujita A, Hashimoto Y, Matsui H, Yasunaga H, Aihara M. Recent trends in glaucoma surgery: a nationwide database study in Japan, 2011–2019. Jpn J Ophthalmol. 2022;66(2):183–92. https://doi.org/10.1007/s10384-021-00898-6.
Bell K, de Padua Soares Bezerra B, Mofokeng M, et al. Learning from the past: mitomycin C use in trabeculectomy and its application in bleb-forming minimally invasive glaucoma surgery. Surv Ophthalmol. 2021;66(1):109–123. https://doi.org/10.1016/j.survophthal.2020.05.005.
Qiao C, Zhang H, Cao K, Investigators for the Chinese Glaucoma Study C, et al. Changing trends in glaucoma surgery over the past 5 years in China. J Glaucoma. 2022. https://doi.org/10.1097/IJG.0000000000002004.
Elhofi A, Helaly HA. Non-penetrating deep sclerectomy versus trabeculectomy in primary congenital glaucoma. Clin Ophthalmol. 2020;14:1277–85. https://doi.org/10.2147/OPTH.S253689.
Mendrinos E, Mermoud A, Shaarawy T. Nonpenetrating glaucoma surgery. Surv Ophthalmol. 2008;53(6):592–630. https://doi.org/10.1016/j.survophthal.2008.08.023.
Dai L, Li AL, Yu L, Ye J. Reply: efficacy and safety of CO2 laser-assisted sclerectomy surgery for glaucoma: a systematic review and meta-analysis. Arq Bras Oftalmol. 2021;84(4):418–20. https://doi.org/10.5935/0004-2749.202100111.
Zagidullina AS, Aznabaev BM, Zulkarneev RK. Factor analysis of the risk of developing primary open-angle glaucoma. Vestn Oftalmol. 2022;138(1):23–30. https://doi.org/10.17116/oftalma202213801123.
Bilgin G, Karakurt A, Saricaoglu MS. Combined non-penetrating deep sclerectomy with phacoemulsification versus non-penetrating deep sclerectomy alone. Semin Ophthalmol. 2014;29(3):146–50. https://doi.org/10.3109/08820538.2013.874466.
Xiao JY, Liang AY, Wang YL, Cheng GW, Zhang MF. Efficacy and safety of non-penetrating glaucoma surgery with phacoemulsification versus non-penetrating glaucoma surgery: a meta-analysis. Int J Ophthalmol. 2021;14(12):1970–8. https://doi.org/10.18240/ijo.2021.12.24.
Zhang Y, Mao J, Zhou Q, et al. Comparison of long-term effects after modified CO2 laser-assisted deep sclerectomy and conventional trabeculectomy in Chinese primary open-angle glaucoma. Ophthalmol Ther. 2022;11(1):321–31. https://doi.org/10.1007/s40123-021-00413-7.
Chen M, Gu Y, Yang Y, Zhang Q, Liu X, Wang K. Management of intraocular pressure elevation after CO2 laser-assisted sclerectomy surgery in patients with primary open-angle glaucoma. Front Med (Lausanne). 2021;8: 806734. https://doi.org/10.3389/fmed.2021.806734.
Greifner G, Roy S, Mermoud A. Results of CO2 laser-assisted deep sclerectomy as compared with conventional deep sclerectomy. J Glaucoma. 2016;25(7):e630-638. https://doi.org/10.1097/IJG.0000000000000187.
Zhang H, Tang Y, Yan X, et al. CO2 laser-assisted deep sclerectomy surgery compared with trabeculectomy in primary open-angle glaucoma: two-year results. J Ophthalmol. 2021;2021:6639583. https://doi.org/10.1155/2021/6639583.
Yu X, Chen C, Sun M, et al. CO2 laser-assisted deep sclerectomy combined with phacoemulsification in patients with primary open-angle glaucoma and cataract. J Glaucoma. 2018;27(10):906–9. https://doi.org/10.1097/IJG.0000000000001056.
Villavicencio J, Baltodano F, Jiménez IMR, et al. Comparative clinical results of phacoemulsification combined with CO2 laser-assisted sclerectomy vs phacoemulsification combined with trabeculectomy in patients with open-angle glaucoma. Clin Exp Ophthalmol. 2017. https://doi.org/10.4172/2155-9570.1000749.
Ho DCW, Perera SA, Hla MH, Ho CL. Evaluating CO2 laser-assisted sclerectomy surgery with mitomycin C combined with or without phacoemulsification in adult Asian glaucoma subjects. Int Ophthalmol. 2021;41(4):1445–54. https://doi.org/10.1007/s10792-021-01707-2.
Yick DWF, Lee JWY, Tsang S, Yeung BYM, Yuen CYF. Preliminary results of CO2 laser-assisted sclerectomy surgery (CLASS) in the treatment of advanced glaucoma in a Chinese population. Medicine (Baltimore). 2016;95(45): e5294. https://doi.org/10.1097/MD.0000000000005294.
Raja SV, Ponnat AK, Balagiri K, Pallamparthy S. Retrospective analysis of the comparison between carbon dioxide laser-assisted deep sclerectomy combined with phacoemulsification and conventional trabeculectomy with phacoemulsification. Indian J Ophthalmol. 2021;69(10):2741–5. https://doi.org/10.4103/ijo.IJO_3310_20.
Servat JJ, Bernardino CR. Effects of common topical antiglaucoma medications on the ocular surface, eyelids and periorbital tissue. Drugs Aging. 2011;28(4):267–82. https://doi.org/10.2165/11588830-000000000-00000.
Lee RY, Chon BH, Lin SC, He M, Lin SC. Association of ocular conditions with narrow angles in different ethnicities. Am J Ophthalmol. 2015;160(3):506-515 e501. https://doi.org/10.1016/j.ajo.2015.06.002.
Zheng Q, Hu M, Li ZL, Chang PJ, Zhao YE. Assessment of anterior chamber angle changes after phacoemulsification with swept-source OCT. Int J Ophthalmol. 2021;14(10):1527–32. https://doi.org/10.18240/ijo.2021.10.08.
Johnson DH, Johnson M. Glaucoma surgery and aqueous outflow: how does nonpenetrating glaucoma surgery work? Arch Ophthalmol. 2002;120(1):67–70. https://doi.org/10.1001/archopht.120.1.67.
Yan X, Zhang H, Li F, Ma L, Geng Y, Tang G. Surgical site characteristics after CLASS followed by ultrasound biomicroscopy and clinical grading scale: a 2-year follow-up. Eye (Lond). 2021;35(8):2283–93. https://doi.org/10.1038/s41433-020-01235-w.
Lam D, Wechsler DZ. Five-year outcomes of trabeculectomy and phacotrabeculectomy. Cureus. 2021;13(1): e12950. https://doi.org/10.7759/cureus.12950.
Acknowledgements
The authors thank all the patients for their participation and contributions. We also thank Xiaoning Yu for assistance in statistical analysis.
Funding
This study was supported by National Natural Science Foundation of China (no. 82171045) and Zhejiang Provincial Public Welfare Technology research project (no. LGF20H120003). The Rapid Service Fee was also covered by the funding.
Authorship
Min Chen, Naiji Yu, Chunlian Huang, Qi Zhang, Xin Liu, Kaijun Wang. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work and have given their approval for the version to be published.
Author Contributions
Min Chen and Naiji Yu: design and concept of study, and drafting and revision of manuscript; Chunlian Huang: data collection and analysis; Qi Zhang and Xin Liu: data collection and interpreting results. Kaijun Wang: design and concept of study and performing operation. All authors listed have made a substantial contribution to the work and approved it for publication.
Disclosures
Min Chen, Naiji Yu, Chunlian Huang, Qi Zhang, Xin Liu and Kaijun Wang declare that they have no competing interests.
Compliance with Ethics Guidelines
The studies involving human participants were reviewed and approved by Ethics Committee of the Second Affiliated Hospital of Zhejiang University (2020-ER721). Written informed consent was obtained from all the subjects prior to participation and for publication of the accompanying images in this study. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
The original contributions presented in the study are included in the article/supplementary material; further information is available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chen, M., Yu, N., Huang, C. et al. CO2 Laser-Assisted Sclerectomy Surgery Alone or Combined with Phacoemulsification in Primary Open-Angle Glaucoma: Comparison of 1-Year Outcomes. Ophthalmol Ther 11, 1719–1733 (2022). https://doi.org/10.1007/s40123-022-00539-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00539-2