Abstract
Introduction
To evaluate the short-term safety and efficacy of the EVO implantable collamer lens (ICL) using a customized implanting orientation design based on ultrasound biomicroscope (UBM) measurement.
Methods
The prospective case series included 310 eyes of 158 patients treated with ICL. To achieve an optimal vault, an ICL of specific size was chosen and implanted in a customized orientation according to assessment of sulcus-to-sulcus (STS) diameters, distance between STS plane and crystalline lens (STSL), the morphology of ciliary sulcus (MCS), anterior chamber depth (ACD), and white-to-white (WTW). With the new design, there were 138 eyes with a non-horizontal orientation and 172 eyes with a horizontal orientation of the ICL. Refractive and ICL vault statuses were followed up for 1 day and 1 month postoperatively.
Results
The safety index at 1 month was 1.34 ± 0.17 for the non-horizontally implanted group and 1.33 ± 0.16 for the horizontally implanted group; the efficacy index was 1.21 ± 0.18 for the non-horizontally implanted group and 1.18 ± 0.16 for the horizontally implanted group. All eyes achieved an uncorrected distance visual acuity of 0.10 logMAR or better. No significant difference in endothelial cell density was observed between the preoperative value (2792.6 ± 247.6 cells/mm2) and value at 1 month postoperatively (2744.2 ± 243.3 cells/mm2), and no cataract or anterior subcapsular opacification was observed. Ideal vault (250–750 μm) was achieved in 84% of eyes (260/310).
Conclusion
The customized ICL design of implanting orientation based on UBM measurement provides good safety, efficacy, and vault predictability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? | |
To achieve clinically safe and desirable outcomes, the ICL must be accurately and stably placed in the ciliary sulcus with an appropriate vault. An insufficient or excessive vault remains a risk factor for complications. | |
The traditional ICL sizing based on white-to-white (WTW) diameter and anterior chamber depth (ACD) is not good enough to achieve an optimal postoperative vault for each individual. | |
The study assumed that an ideal vault can be achieved by customizing the ICL orientation and evaluated the short-term outcomes of ICL using a customized implanting orientation design based on ultrasound biomicroscopy (UBM) measurement. | |
What was learned from the study? | |
The customization of implanting orientation could safely and effectively manage the vault. | |
The sulcus-to-sulcus (STS) diameters, distance between STS plane and crystalline lens, and ciliary sulcus morphology should also be considered during design. |
Introduction
The Visian implantable collamer lens (ICL; STAAR Surgical, Monrovia, CA, USA) is a widely used posterior chamber phakic intraocular lens. The implantation of the ICL has been accepted as a safe, effective, and predictable surgical procedure for correcting a wide range of refractive errors with good visual and optical quality [1, 2]. However, to achieve clinically safe and desirable outcomes, the ICL must be accurately and stably placed in the ciliary sulcus with an appropriate vault. Although the safety of the ICL with a central port (EVO ICL, Model V4c) is better than the previous Model V4, an insufficient vault may still increase the risk of anterior subcapsular cataract, while an excessive vault remains a risk factor for complications, such as secondary glaucoma and endothelial damage [3]. Currently, the optimal sizing of the ICL and management of the postoperative vault remains a challenge for ICL surgeons.
Traditionally, ICL sizing has been based on white-to-white (WTW) corneal diameter and anterior chamber depth (ACD), as proposed by the manufacturer (STAAR Surgical); however, the performance of the formula is not good enough to achieve an optimal vault for each individual [4]. Additional ocular biometric parameters measured by ultrasound biomicroscopy (UBM), such as the sulcus-to-sulcus (STS) diameter and distance between STS plane and anterior crystalline lens surface (STSL), were reported to be correlated with the vault and could be applied for the optimization of ICL sizing [5, 6]. Furthermore, since the EVO ICL comes in only four sizes (12.1 mm, 12.6 mm, 13.2 mm, and 13.7 mm), the surgeon has to select a size closest to the optimal size, which may limit the design of a custom ICL for an individual eye.
The ciliary sulcus is vertically oval and the STS diameter and STSL vary radially [7, 8]. Therefore, we assume that an ideal vault can be achieved by customizing not only the ICL size but also the ICL orientation. For eyes requiring the implantation of a toric ICL (TICL), the optimal refractive outcomes could be obtained by ordering the TICL with the exact cylinder axis at the customized axis. Herein, we report the results of what is, to our knowledge, the first prospective study to assess the efficacy and safety of EVO ICL implantation using a customized implanting orientation based on UBM measurement.
Methods
Patient Selection and Study Design
This prospective interventional case series study was performed at the Eye and ENT Hospital of Fudan University (Shanghai, China). The study adhered to the tenets of the Declaration of Helsinki, in accordance with the local regulatory requirements. The protocols were approved by the Ethics Committee of the Fudan University Eye and ENT Hospital Review Board (No. 2016038). All patients provided signed informed consent before enrolment.
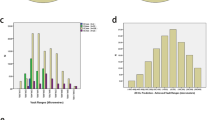
We recruited 310 eyes of 158 patients who underwent the implantation of the EVO ICL for myopia and/or myopic astigmatism using a customized design of implanting orientation based on comprehensive assessment of anterior segment anatomy. The inclusion criteria were (1) age of 20–40 years; (2) a stable refractive error (change no greater than 0.50 D/year) for at least 2 years; (3) corrected visual acuity (CDVA) worse than 0.2 logMAR and spherical equivalent (SE) less myopic than − 18.0 D; (4) ACD at least 2.8 mm (measured from the endothelium); (5) endothelial cell density (ECD) at least 2000 cells/mm2. Exclusion criteria were other pre-existing ocular diseases, history of ocular surgery/trauma/systemic diseases involving the eyes, or severe mental disorders. The patient demographics and the distribution of preoperative anterior segment parameters are presented in Table 1 and in the Supplementary Material (Supplementary Fig. 1).
Determination of ICL
The EVO ICL power calculation (STAAR Surgical) was performed using a modified vertex formula based on the ICL Power Calculation Software (http://en.informer.com/icl-power-calculation-software/, version 3.0). A TICL was selected for eyes with astigmatism beyond 1.0 DC or 1/10 of spherical error, and for the eyes which could gain two or more lines of the CDVA after correcting astigmatism.
The standard size of the lens was chosen on the basis of ACD and WTW (Pentacam HR, Type 70,900; Oculus Optikgeräte GmbH, Wetzlar, Germany) according to the STAAR Company online calculator and horizontal placement was defined as 22.5° or less of rotation from the horizontal meridian. The difference between the horizontal STS and WTW diameters (hSTS − WTW; Compact Touch STS UBM, Quantel Medical, France) was the main factor to consider, while the distance between the STS plane and anterior crystalline lens surface (STSL, UBM) and the morphology of ciliary sulcus (MCS, UBM) were secondary factors. The MCS was evaluated using the ratio of the width of the ciliary sulcus recess to the maximum iris thickness near the pupil margin (IT3). When the ratio was between 0.5 and 1, the MCS was defined as normal; when it was greater than 1, the MCS was defined as wide; otherwise, the MCS was defined as narrow (Supplementary Fig. 2).
Non-horizontal implantation with the same size of ICL is considered to provide a mild adjustment of an expected vault. Thus, we designed a set of sequential options with a combination of the ICL size and implantation orientation, instead of ICL size alone (Fig. 1). When hSTS − WTW was mildly larger than the average level, the standard size was considered too small for the eye and the option was lifted by one level, i.e., non-horizontal implantation with a larger ICL size. When hSTS − WTW was mildly smaller than the average level, the standard size was expected to be too large for the eye and the option was reduced by one level, i.e., non-horizontal implantation with the standard size will be chosen. When the hSTS − WTW was much larger/smaller than the average level, the original option was increased/reduced by two levels. After the size and orientation were adjusted according to hSTS − WTW, if there was still one of the “plus” signs (1. large STSL, 2. wide MCS) present, the option was increased by an extra level. For non-horizontal implantation, the ICL orientation was determined on the basis of the axis in which the STS − WTW was closest to the average when the standard size was chosen or the STS − WTW was closest to the average ± 0.5 when the larger/smaller size was chosen. The ICL cylinder axis was determined on the basis of the preoperative axis of astigmatism and the aiming axis of the ICL implanting orientation. The post-rotation ICL has its cylinder axis equal to the preoperative axis of astigmatism.
Flowchart of the customized implanting orientation design based on comprehensive assessment of anterior segment anatomy. ACD anterior chamber depth, MCS morphology of ciliary sulcus, STS sulcus-to-sulcus diameter, STSL distance between STS plane and anterior crystalline lens surface, WTW white-to-white diameter, hSTS − WTW the difference between the horizontal STS and WTW diameters
According to the aforementioned criteria, 109 eyes were implanted with ICLs of the standard size non-horizontally, 29 eyes with ICLs in the greater size non-horizontally, 64 eyes with ICLs in the smaller size horizontally, 97 eyes with ICLs in standard size horizontally, and 11 eyes with ICLs in the greater size horizontally.
Surgical Procedures
Before the surgery, the surgeon marked the zero horizontal axis and the attended axis at a slit lamp while the patient was sitting upright to avoid potential cyclotorsion while lying supine. The one-step technique was conducted as previously described [1]. Briefly, ICL V4c was implanted with an injector cartridge via a 3-mm clear corneal incision, and a moderate viscoelastic agent (1.7% sodium hyaluronate; Bausch & Lomb, China) was injected into the anterior chamber. ICL V4c was placed in the posterior chamber and the viscoelastic agent was removed using Ringer’s lactate solution by irrigation only. Supplementary Fig. 3A shows an intraoperative photograph.
After implantation, patients received topical 0.5% levofloxacin four times daily for 7 days, 1.0% prednisolone acetate four times daily for 4 days, and pranoprofen four times daily for 14 days.
Main Refractive and Biometric Measures
Each patient underwent eye examinations before and 1 day and 1 month after the surgery. The main parameters were (1) uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), and manifest refraction; (2) axial length (IOL Master, Carl Zeiss Meditec), intraocular pressure (IOP, Canon Full Auto Tonometer TX-F; Canon, Tokyo, Japan), and ECD (EM-4000, TOMEY; Nagoya, Japan); (3) corneal topography, WTW, and ACD (Pentacam); (4) STS diameter and STSL were measured as previously described [6] in both horizontal and vertical meridian and the MCS was evaluated (preoperatively, UBM); (5) horizontal vault of the ICL (postoperatively, CASIA2 swept-source OCT, TOMEY).
Statistical Analysis
The data were analyzed using R version 3.6.2 (R Project for Statistical Computing, http://cran.rproject.org). Continuous variables were presented as mean ± standard deviation (SD), and categorical variables were presented as frequency and percentage. The eye-level continuous variables at different time points were compared using a generalized estimation equation (GEE). Statistical significance was set at p value of less than 0.05.
Results
Safety
All procedures and postoperative follow-ups were uneventful; no complications were noted during the 1-month follow-up. The mean safety indices (postoperative CDVA/preoperative CDVA) were 1.34 ± 0.17 and 1.33 ± 0.16 in the non-horizontally implanted group and horizontally implanted group, respectively. None of the eyes lost one or more lines of CDVA (Fig. 2a). There was no significant difference between preoperative ECD value (2792.6 ± 247.6 cells/mm2) and the value 1 month after the surgery (2744.2 ± 243.3 cells/mm2, p = 0.06). At 1 month, all eyes were normotensive with an IOP of less than 22 mmHg.
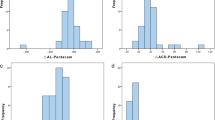
Refractive outcomes at 1 month of implantable collamer lens (ICL) using a customized non-horizontal or horizontal implanting orientation based on comprehensive assessment of anterior segment anatomy. a Changes in Snellen lines of corrected distance visual acuity (CDVA); b cumulative postoperative uncorrected distance visual acuity; c postoperative UDVA versus preoperative CDVA; d spherical equivalent (SE) refraction; e, f attempted versus achieved SE refraction after ICL implantation using a non-horizontal (e) or horizontal (f) implanting orientation
Efficacy
One month after the surgery, the efficacy indices (postoperative UDVA/preoperative CDVA) were 1.21 ± 0.18 and 1.18 ± 0.16 in the non-horizontally implanted group and horizontally implanted group. All eyes had a postoperative UDVA of 0.10 logMAR or better (Fig. 2b). Ninety-seven percent of the eyes in the non-horizontally implanted group (134/138) and 98% of the eyes in the horizontally implanted group (169/172) achieved a UDVA equal to or better than the preoperative CDVA (Fig. 2c).
Predictability
Ninety-four percent of the eyes with non-horizontally placed ICL (130/138) and 95% of the eyes with horizontally placed ICL (163/172) had an SE within ± 0.5 D. All eyes within ± 1.0 D (Fig. 2d). Ninety-four percent of the eyes with non-horizontally placed ICL (130/138) and 95% of the eyes with horizontally placed ICL (163/172) were within ± 0.5 D of the attempted SE correction, and all eyes were within ± 1.0 D (Fig. 2e, f).
Astigmatism Correction
Astigmatism in 84% of the eyes with non-horizontally placed non-toric ICLs (56/67) was within ± 0.5 DC, and that in all of the eyes was within ± 1.0 DC. Astigmatism in 87% of the eyes with horizontally placed non-toric (80/92) was within ± 0.5 DC, and that in 97% of the eyes (89/92) was within ± 1.0 DC (Fig. 3a).
Astigmatism correction of implantable collamer lens (ICL) using a customized non-horizontal or horizontal implanting orientation. a, b Refractive astigmatism of non-toric (a) and toric ICL (TICL, b); c, d attempted versus achieved correction of astigmatic vectors (corneal plane) after TICL implantation using a non-horizontal (c) or horizontal (d) implanting orientation; e, f angle of error (degrees) after TICL implantation using a non-horizontal (e) or horizontal (f) implanting orientation
Regarding the TICL, residual astigmatism in 89% of eyes with non-horizontally placed TICLs (63/71) was within ± 0.5 DC, and that in all of the eyes was within ± 1.0 DC. Residual astigmatism in 89% of eyes with horizontally placed TICLs (71/80) was within ± 0.5 DC, and that in 98% of the eyes (78/80) was within ± 1.0 DC (Fig. 3b). In the group of the smaller size, horizontally placed ICLs, two eyes had astigmatism of 1.25 DC but the slit lamp examination showed that the deviation from the planned orientation of implantation was less than 5°. The scatter plots of target-induced astigmatism (TIA) versus surgically induced astigmatism (SIA) are shown in Fig. 3c, d. The astigmatism correction index (SIA/TIA) was 0.99 ± 0.22 in the non-horizontally implanted group and 0.93 ± 0.17 in the horizontally implanted group. An angle of error within ± 15° was in 97% of eyes (147/151) (Fig. 3e, f).
Vault
An ideal horizontal vault (250–750 μm) was achieved in 260 eyes (84%) 1 month after the surgery (Fig. 4 and Supplementary Figs. 3B–E). The vault in 13 eyes (4%) ranged from 150 to 250 μm and that in 34 eyes (11%) ranged from 750 to 1200 μm. Three eyes (1%) with vault greater than 1200 μm were observed in two non-horizontally placed ICLs in the standard size and one horizontally placed ICL in the larger size. All three eyes showed normal IOP and no evidence of chamber angle closure. No eye had a vault of less than 150 μm. No cataract or anterior subcapsular opacification was observed.
Discussion
The optimization of the EVO ICL sizing has been studied extensively [9, 10]; however, a customized design for each individual eye remains a challenge because there are only four available sizes of the ICL. In this study, we reported a novel ICL design, i.e., a customized design of implanting orientation based on UBM measurement, evaluated its short-term outcomes, and demonstrated its practical value for clinical treatment.
In the current study, more ocular parameters and ICL implanting orientation were considered as variables to achieve an optimal vault. STSL, a parameter indicative of the anterior surface protrusion of the crystalline lens, has been proven to affect the postoperative ICL vault, and eyes with a high STSL tend to have low vaults [6]. The characteristics of the posterior chamber, especially the ciliary sulcus and ciliary body, are also important factors for the vault [11]. A large STS, wide MCS, or flat ciliary process will result in a lower vault than expected. Therefore, these parameters should be included in this concern. Furthermore, the manufacturer recommended that the ICL should not be rotated by more than 22.5° from the horizontal meridian. However, for specific eyes, ICLs of existing sizes with minimized rotation may not ensure an optimal vault. The STS diameter varies radially, and the vertical STS diameter is normally greater than the horizontal STS [7, 8]. In two patients who required reoperation due to an excessive vault, the vault decreased after rotation of the lens to a vertical orientation [12, 13], suggesting that the vault could be lower when the ICL is implanted vertically. We further assumed that the vault varied when the lens was placed in a different meridian. Therefore, a customized implanting orientation of the ICL was designed on the basis of the previously mentioned parameters to provide an optimized vault. An oblique or vertical orientation with a standard size was designed to reduce the expected vault. An oblique or vertical orientation with a larger size was designed to increase the expected vault to a moderate degree. To the best of our knowledge, this is the first study to report the outcome of non-horizontal ICL implantation.
When determining the ICL size and implanting orientation, the difference between horizontal STS and WTW diameters (STS − WTW) is the main concern. Lee et al. reported that STS − WTW was negatively correlated with the ICL vault, and the ICL size − STS diameter had a stronger correlation with the ICL vault than the ICL size − WTW [5]. Thus, the ICL size and orientation should be adjusted when STS − WTW is too large or small. In addition, the morphology of the crystalline lens, ciliary sulcus, and ciliary body should also be considered. Notably, in most cases only if there is a great difference between vertical and horizontal STS diameters, the design of non-horizontal placement would effectively decrease the vault; this may also occur when there is a great difference between vertical and horizontal STSL, noting that larger vertical STSL might further reduce the vault. Additionally, a wide MCS might also reduce the vault because of the potential posterior dislocation of ICL haptics.
In this study, neither a contact between the ICL and the crystalline lens nor a narrow anterior chamber angle was observed, suggesting that extreme underestimation or overestimation of ICL size did not occur. The vault in 84% of eyes was achieved in the range of 250–750 μm. This is higher than the rate of the ICL in Trancón’s study [14] (53%) and Qi’s research [15] (76.6%) using the conventional manufacturer WTW/ACD-based sizing. Nakamura et al. applied NK-formula V2 to select the size of ICLs and 91.2% of the eyes showed moderate vaults (250–1000 μm) [10], which was similar to our results (93%). Measuring the STS diameter in other different meridians, such as at 30°, 45°, 60°, 120°, 135°, and 150°, could be helpful in improving the rate of an optimal vault in the group of non-horizontally placed ICLs. Although the vault in 4% of the eyes was lower than 250 μm, no vault lower than 150 μm was detected. Gonvers et al. observed anterior subcapsular cataract after ICL V4 only in eyes with vaults less than 90 μm and recommended 150 μm as the lower limit of target vaulting [16]. The design of the central port in EVO ICLs further reduced the risk of complications caused by a low vault [17]. Yang et al. observed a slight increase in the anterior average lens density, without anterior capsular cataract formation, in 62 eyes 4 years after the implantation of the EVO ICL [18]. Three eyes were found with a vault slightly greater than 1200 μm; however, the postoperative anterior chamber angle was greater than 12°, and thus the relatively large vault was safe. Furthermore, it was reported that the vault decreased over time and the decrease in vaulting was pronounced in eyes with greater initial vaulting [19]. Thus, a longer follow-up period is required for these eyes. Although most of the ICL implantations using the new method have satisfying outcomes, the prediction of postoperative vaults here was partly based on clinical experience and it was difficult for novices to determine the critical points and weights of each parameter. Therefore, future studies on new formulas for the design of ICL implanting orientation are recommended.
The outcome of CDVA (safety index 1.34 ± 0.17 for the non-horizontally implanted group and 1.33 ± 0.16 for the horizontally implanted group) demonstrated that the new customized design of the ICL implanting orientation is safe for correcting myopia. Shimizu et al. reported a safety index of 1.11 ± 0.23 at 1 month after implantation of ICL V4c using the standard WTW/ACD-based sizing [20] and Miao et al. reported a safety index of 1.33 ± 0.22 at 3 months post-surgery [21], indicating that the safety of the new design is not inferior to that of the standard design. Moreover, no loss of ECD was observed. This finding, while preliminary, suggests that additional rotation required for non-horizontal implantation may not lead to secondary corneal endothelial damage. Since the follow-up duration was quite short, the long-term change of ECD is unclear.
The customized design of the EVO ICL showed good visual outcomes at 1 month (efficacy index 1.21 ± 0.18 for the non-horizontally implanted group and 1.18 ± 0.16 for the horizontally implanted group). The efficacy index at 1 month postoperatively in Shimizu’s study was 0.96 ± 0.28 [20], which was similar to our outcomes. Regarding astigmatism correction, all eyes undergoing TICL implantation were designed to have astigmatism fully corrected, and most eyes had a postoperative cylindrical error no greater than 0.50 D. However, two eyes had a postoperative cylinder of 1.25 DC, which was attributed to incision-induced corneal astigmatism based on the corneal topography.
This study had some limitations. First, the patients were followed up for only 1 month. Further studies with long follow-up periods should be undertaken to investigate the long-term safety and rotational stability after non-horizontal implantation. Second, the predictability of the vault was evaluated semiquantitatively and the long-term change in the vault is also an important issue for future research.
Conclusion
The EVO ICL using a customized implanting orientation design based on UBM measurement provides good safety, efficacy, and vault predictability. It could be a readily available method to manage the ICL vault for patients who may not achieve an optimal vault by using the standard WTW/ACD-based sizing.
References
Wei R, Li M, Zhang H, et al. Comparison of objective and subjective visual quality early after implantable collamer lens V4c (ICL V4c) and small incision lenticule extraction (SMILE) for high myopia correction. Acta Ophthalmol. 2020;98:e943–50.
Brar S, Gautam M, Sute SS, Pereira S, Ganesh S. Visual and refractive outcomes with the eyecryl phakic toric IOL versus the visian toric implantable collamer lens: results of a 2-year prospective comparative study. J Refract Surg. 2021;37:7–15.
Garcìa-Feijoó J, Hernández-Matamoros JL, Castillo-Gómez A, et al. Secondary glaucoma and severe endothelial damage after silicone phakic posterior chamber intraocular lens implantation. J Cataract Refract Surg. 2004;30:1786–9.
Nam SW, Lim DH, Hyun J, Chung E-S, Chung T-Y. Buffering zone of implantable collamer lens sizing in V4c. BMC Ophthalmol. 2017;17:260.
Lee D-H, Choi S-H, Chung E-S, Chung T-Y. Correlation between preoperative biometry and posterior chamber phakic visian implantable collamer lens vaulting. Ophthalmology. 2012;119:272–7.
Kojima T, Yokoyama S, Ito M, et al. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. 2012;153(632–7):637.e1.
Petermeier K, Suesskind D, Altpeter E, et al. Sulcus anatomy and diameter in pseudophakic eyes and correlation with biometric data: evaluation with a 50 MHz ultrasound biomicroscope. J Cataract Refract Surg. 2012;38:986–91.
Biermann J, Bredow L, Boehringer D, Reinhard T. Evaluation of ciliary sulcus diameter using ultrasound biomicroscopy in emmetropic eyes and myopic eyes. J Cataract Refract Surg. 2011;37:1686–93.
Igarashi A, Shimizu K, Kato S, Kamiya K. Predictability of the vault after posterior chamber phakic intraocular lens implantation using anterior segment optical coherence tomography. J Cataract Refract Surg. 2019;45:1099–104.
Nakamura T, Isogai N, Kojima T, Yoshida Y, Sugiyama Y. Optimization of implantable collamer lens sizing based on swept-source anterior segment optical coherence tomography. J Cataract Refract Surg. 2020;46:742–8.
Chen Q, Tan W, Lei X, et al. Clinical prediction of excessive vault after implantable collamer lens implantation using ciliary body morphology. J Refract Surg. 2020;36:380–7.
Matarazzo F, Day AC, Fernandez-Vega Cueto L, Maurino V. Vertical implantable collamer lens (ICL) rotation for the management of high vault due to lens oversizing. Int Ophthalmol. 2018;38:2689–92.
Srirampur A, Mansoori T, Balijepalli P, Gadde AK. Management of anisocoria and high vault in an eye with implantable collamer lens. Indian J Ophthalmol. 2020;68:3070–2.
Trancón AS, Manito SC, Sierra OT, Baptista AM, Serra PM. Determining vault size in implantable collamer lenses: preoperative anatomy and lens parameters. J Cataract Refract Surg. 2020;46:728–36.
Meng-ying Qi, Qian C, Qing-yan Z. The effect of the crystalline lens on central vault after implantable collamer lens implantation. J Refract Surg. 2017;33:519–23.
Gonvers M, Bornet C, Othenin-Girard P. Implantable contact lens for moderate to high myopia: relationship of vaulting to cataract formation. J Cataract Refract Surg. 2003;29:918–24.
Packer M. Meta-analysis and review: effectiveness, safety, and central port design of the intraocular collamer lens. Clin Ophthalmol. 2016;10:1059–77.
Yang W, Zhao J, Zhao J, et al. Changes in anterior lens density after Implantable Collamer Lens V4c implantation: a 4-year prospective observational study. Acta Ophthalmol. 2020. https://doi.org/10.1111/aos.14584.
Alfonso JF, Fernández-Vega L, Lisa C, Fernandes P, González-Meijome J, Montés-Micó R. Long-term evaluation of the central vault after phakic Collamer® lens (ICL) implantation using OCT. Graefes Arch Clin Exp Ophthalmol. 2012;250:1807–12.
Shimizu K, Kamiya K, Igarashi A, Shiratani T. Early clinical outcomes of implantation of posterior chamber phakic intraocular lens with a central hole (Hole ICL) for moderate to high myopia. Br J Ophthalmol. 2012;96:409–12.
Miao H, Chen X, Tian M, Chen Y, Wang X, Zhou X. Refractive outcomes and optical quality after implantation of posterior chamber phakic implantable collamer lens with a central hole (ICL V4c). BMC Ophthalmol. 2018;18:141.
Acknowledgements
We thank the participants of the study. We thank Dr. Qingyang Liu and Yilin Xu for their contribution to this paper. We thank Dr. Yudong Jiang for editing and figure preparation.
Funding
The Rapid Service Fee and a professional language editing service was funded by Provincial High-level University Construction Project (DGF501035/006/003), National Natural Science Foundation of China (Grant No. 81770955), Joint Research Project of New Frontier Technology in Municipal Hospitals (SHDC12018103), Major clinical research project of Shanghai Shenkang Hospital Development Center (SHDC2020CR1043B), Project of Shanghai Xuhui District Science and Technology (2020–015).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Concept and design: Peijun Yao, Xingtao Zhou, Xiaoyang Wang, Lin Wang and Xiaodong Zhou were responsible for the concept and design. Data collection was carried out by Ruoyan Wei, Mingrui Cheng, Lingling Niu, Lin Wang, Xiumei Luo, Meiyan Li, Xiaodong Zhou, Xiaoying Wang, Xingtao Zhou, and Peijun Yao. Statistical analysis was conducted by Ruoyan Wei. Ruoyan Wei and Mingrui Cheng drafted the manuscript. Peijun Yao, Lingling Niu, and Xingtao Zhou revised the manuscript.
Disclosures
Ruoyan Wei, Mingrui Cheng, Lingling Niu, Lin Wang, Xiumei Luo, Meiyan Li, Xiaodong Zhou, Xiaoying Wang, Xingtao Zhou, and Peijun Yao have nothing to disclose.
Compliance with Ethics Guidelines
The study adhered to the tenets of the Declaration of Helsinki. The protocols were approved by the Ethics Committee of the Fudan University EENT Hospital Review Board (No. 2016038).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wei, R., Cheng, M., Niu, L. et al. Outcomes of the EVO ICL Using a Customized Non-horizontal or Horizontal Implanting Orientation Based on UBM Measurement: A Pilot Study. Ophthalmol Ther 11, 1187–1198 (2022). https://doi.org/10.1007/s40123-022-00498-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00498-8