Abstract
Introduction
Pilocarpine hydrochloride (pilo) ophthalmic solution has traditionally been used for the treatment of glaucoma, with opportunities to improve the tolerability profile experienced by patients. Pilocarpine hydrochloride ophthalmic solution 1.25% (Vuity™, Allergan, an AbbVie company) was approved in late 2021 for the treatment of adults with presbyopia. This publication describes the properties of the optimized, proprietary vehicle of this new ophthalmic solution developed with the aim of improving tolerability upon instillation.
Methods
An in vitro method determined the time required for the pH of pilo 1.25% in the proprietary vehicle (Optimized Formulation) and a commercially available 1% pilo ophthalmic solution (Generic Formulation) to equilibrate with the pH of simulated tear fluid (STF). In a pilot study, five of the six screened participants received one drop of the Optimized Formulation in one eye and Generic Formulation in the other. Ocular discomfort and vision blur were evaluated for each eye just prior to and at multiple times after drop instillation using visual analog scales (VAS), and adverse events were assessed.
Results
The in vitro method showed that the Optimized Formulation achieved faster pH equilibration than the Generic Formulation. The pilot study revealed that the Optimized Formulation demonstrated less ocular discomfort, vision blur, and adverse events compared to the Generic.
Conclusion
The in vitro and pilot study of the Optimized Formulation indicated that it rapidly equilibrates to the physiologic pH of the tear film, providing greater comfort and tolerability while also minimizing vision blur. Overall, the proprietary vehicle is expected to improve comfort, result in less vision blur, and provide a well-tolerated alternative method to deliver pilo for the treatment of presbyopia when compared to what is commercially available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Unwanted side effects, such as ocular discomfort and vision blur, are often associated with topical ocular therapies. |
There is a need to develop a better tolerated vehicle to deliver some topical ocular therapies. |
What was the hypothesis of the study? |
Is the Optimized Formulation a better tolerated vehicle to deliver pilocarpine when compared to the Generic Formulation? |
What were the study outcomes/conclusions? |
The Optimized Formulation had overall less ocular discomfort, less vision blur, and fewer adverse events compared to the Generic Formulation. |
What has been learned from the study? |
The Optimized Formulation is expected to improve comfort, cause less vision blur, and provide a well-tolerated alternative to currently available ocular pilo medications. |
Introduction
Many challenges exist for the delivery of topical ocular therapeutics, such as anatomical and physiologic barriers and unwanted side effects. Some of the side effects commonly associated with topical ocular drops are ocular discomfort and irritation, redness, inflammation, and vision blur [1, 2]. The side effects could be due to the therapeutic agent itself or one of the additives in the vehicle of the ocular drop [3].
Pilocarpine hydrochloride (pilo) as an ophthalmic solution has traditionally been used to treat glaucoma [4]. Pilo is a miotic that contracts the iris sphincter muscle and ciliary muscles causing pupil constriction and accommodation [5, 6]. It is one of the oldest glaucoma treatments, but due to its side effects, it is not always well tolerated and is currently not often used to manage glaucoma [7,8,9]. As a cyclic ester, pilo is highly susceptible to hydrolysis at a physiologic pH. To stabilize pilo in ophthalmic solution, a low pH (~ 4) is needed [10]. However, at low pH, pilo is protonated or ionized and poorly crosses the cornea [11], which limits its bioavailability [12]. Approved commercially available treatments that contain pilo have been known to cause brow aches, headaches, ocular discomfort, hyperemia, and vision blur upon drop instillation. Examples of ocular surface-related discomforts that patients may experience include burning, stinging, and irritation [8, 13,14,15,16,17]. Previous studies have shown that pilo caused more adverse events (AEs) and had increased discontinuation compared to other glaucoma treatment options [14, 18, 19]. Patients also reported lower quality of life with pilo and a higher preference for another glaucoma treatment option [18]. The low pH of the ophthalmic solution may cause some of these side effects [10].
Although pilo is not currently used often to treat glaucoma, miotics, such as pilo, are being investigated as treatment options for presbyopia, with pilo 1.25% (Vuity™; Allergan, an AbbVie company) in an optimized formulation, approved in late 2021, as the first pharmacologic treatment for presbyopia. Presbyopia is a progressive condition in which the eye’s ability to accommodate reduces with increasing age. Accommodation is the ability of the lens to change shape and focus on near objects [20, 21]. Presbyopia affects around 1.8 billion individuals and is a global issue [22]. There are limited treatment options such as surgery or corrective lenses, but dissatisfaction is often expressed with these options [23, 24]. In addition, individuals affected by presbyopia have expressed a preference for an eye drop therapy [24]. Pilo ophthalmic solution 1.25% (Vuity) was developed based on this unmet need for a noninvasive, pharmacologic ocular therapy drop for presbyopia and was reformulated with tolerability in mind. The re-engineered ocular drop was designed to equilibrate rapidly to the pH of the ocular surface, which, in turn, increases the non-ionized pilo, improving bioavailability [12] and reducing the side effects of pilo, such as ocular discomfort and vision blur, upon instillation. Here, we describe the in vitro study and pilot study used to investigate this optimized vehicle.
Methods
An in vitro method and a clinical study were performed to investigate the proprietary vehicle (pHast™ technology, Allergan, an AbbVie company) developed to improve the delivery of pilo.
In Vitro Study
The in vitro method determined the time required for the pH of pilo 1.25% in the proprietary vehicle (hereafter referred to as Optimized Formulation) and a commercially available 1.0% pilo ophthalmic solution (NDC number 61314-0203-15, lot 282976F, manufactured by Sandoz) (hereafter referred to as Generic Formulation) to equilibrate with the pH of simulated tear fluid (STF) [25]. To start, 250 μl of the Optimized Formulation or Generic Formulation was pipetted into the bottom of a 15-ml centrifuge tube, and a micro pH probe was inserted. Approximately 7.5 ml of STF was then gently added, and the system was left undisturbed. The pH was recorded at intervals for a period of 10 min. The intervals were 0, 0.5, and 1 min for the Optimized Formulation and 0, 1, 3, 5, and 10 min for the Generic Formulation.
Clinical Pilot Study
A clinical pilot study was conducted at a single center to determine the in-eye characteristics of two dose strengths of the Optimized Formulation compared to a single dose strength of the Generic Formulation in healthy volunteers. This study was approved by the Alpha Investigational Review Board (San Clemente, CA) and was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All participants provided informed consent. The study consisted of a screening visit and two assessment visits.
Inclusion criteria included being 18 years of age or older, having the ability to follow study instructions and likely to complete all required visits, corrected-distance visual acuity (CDVA) of 20/40 or better in both eyes with correction, intraocular pressure < 21 mmHg in both eyes, and no signs of retinal pathology on dilated fundoscopy. Exclusion criteria included having an active ocular disease, history of retinal detachment or uveitis, females who were pregnant, nursing, or planning a pregnancy, known allergy or sensitivity to any study materials, concurrent use of topical ophthalmic medicals other than artificial tears, diagnosis of any type of glaucoma or ocular hypertension, concurrent enrollment in an investigational drug or device study, and any participant who had or has any condition that, in the investigator’s opinion, may confound the study results. Contact lenses were not worn on the days of assessment visits.
At the first assessment visit, participants received the Generic Formulation with 1.0% pilo in the right eye or left eye and the Optimized Formulation with 1.0% pilo in the contralateral eye. The eye that received the Generic versus Optimized Formulation was determined by a computer randomization method. An Ocular Discomfort and Blurry Vision Questionnaire Visual Analog Scale (VAS) assessment was performed prior to drop instillation (baseline) and 30 s, 1, 1.5, 2, 3, 4, and 5 min after drop instillation. For the VAS assessments, participants were asked to assess vision blur from no vision blur to maximum vision blur and ocular discomfort from no ocular discomfort to maximum ocular discomfort. The participants were asked to mark the place that best captured how each eye felt at that moment on an anchored VAS and then trained study personnel used a ruler to convert the participant’s response to a numerical value (0–100). The VAS assessments were answered simultaneously but independently for both eyes. AEs were also assessed, and biomicroscopy ocular surface examination was performed at baseline and 5- and 60-min following drop instillation. Based on the biomicroscopy examination, conjunctival hyperemia was scored. The second assessment visit was performed the same as the first, except that participants received the Optimized Formulation with 1.25% pilo in the right eye or left eye and the Generic Formulation with 1.0% pilo in the contralateral eye. The concentration of pilo did not increase in the Generic Formulation at the second assessment. Both investigators and participants were masked, and the VAS assessment was administered by a different investigator than those administering the drops.
The summary statistics for the Ocular Discomfort and Blurry Vision Questionnaire VAS scores include the mean, standard deviation, and standard error of the mean (SEM) by time point. Biomicroscopy findings were summarized using the mean scores by treatment group. Paired t-tests were also performed for all questionnaire VAS scores comparing the Generic and Optimized Formulations.
Results
In Vitro
In the in vitro study, the pH of the Optimized Formulation started at 4.35 and was able to equilibrate to the predetermined final pH of the mixture of 6.43 within 1 min. The pH of the Generic Formulation started at 4.41 and did not reach the expected final pH value at the end of the 10-min period. The pH only increased to 4.44 by the end of the study (Fig. 1).
Clinical
In the pilot study, a total of six participants were screened, and five participants passed the screening and completed the study. Of the participants who completed the study, three were males and two females, and their ages ranged from 26 to 56 years old.
The mean (SEM) ocular discomfort score was lower for the Optimized Formulation at each time point when compared to the Generic Formulation (Fig. 2a). The overall mean (SEM) ocular discomfort scores were 1.66 (1.02) and 6.04 (3.18) for the Optimized Formulation and Generic Formulation, respectively. The difference was not statistically significant (p = 0.0966). When the Optimized Formulation contained 1.25% of pilo, the mean ocular discomfort score was lower than the Generic formulation (with 1.0% pilo) up until the 2-min time point (Fig. 2b). The overall mean (SEM) ocular discomfort score was lower for the Optimized Formulation, 6.00 (1.96), compared to the Generic Formulation, 10.53 (4.74), but the difference was not significant (p = 0.198).
The mean (SEM) vision blur score at each time point for both the Optimized Formulation 1.0% and Generic Formulation can be seen in Fig. 3a. The scores were lower for the Optimized Formulation at each time point. The overall mean (SEM) vision blur scores following instillation were 3.53 (1.92) and 8.78 (3.48) for the Optimized Formulation and Generic Formulation, respectively, and the Optimized Formulation was significantly lower than the Generic Formulation (p = 0.016). Similarly, the mean vision blur score for each time point was lower at the second assessment when the Optimized Formulation contained 1.25% of pilo and was compared to the Generic Formulation with 1.0% (Fig. 3b). The overall mean (SEM) vision blur scores were 6.85 (3.00) and 12.14 (5.11) for the Optimized Formulation and Generic Formulation, respectively, and the Optimized Formulation was significantly lower than the Generic Formulation (p = 0.049).
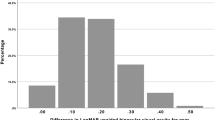
AEs reported included eye pressure/pain, brow ache, vision blur, stinging, itching, and light sensitivity. No serious AEs were reported, and all were mild or moderate in intensity. Only one AE, eye pressure/pain, was reported in an eye that received the Optimized Formulation with 1.0%, while eight AEs were reported in eyes that received the Generic Formulation (Fig. 4a). Similarly, only one AE, brow ache, was reported in an eye that received the Optimized Formulation with 1.25%, and five were reported with the Generic Formulation (Fig. 4b). Based on the biomicroscopy examination at the first assessment, the mean conjunctival hyperemia scores at 5 min following instillation were 0.6 and 0.9 for the Optimized Formulation with 1.0% pilo and Generic Formulation, respectively. Scores were 0.4 and 0.6 for the Optimized Formulation with 1.25% pilo and Generic Formulation, respectively, at the second assessment.
Discussion
The Optimized Formulation with 1.25% pilo achieved faster pH equilibration when diluted with STF compared to the Generic Formulation with 1.0% pilo in the in vitro study. The pilot study demonstrated that overall the administration of the Optimized Formulation produced less ocular discomfort, vision blur, AEs, and hyperemia than the Generic Formulation. Both the 1.0% and 1.25% Optimized Formulation had significantly less vision blur compared to the Generic Formulation.
Although the difference was not statistically significant, ocular discomfort was reduced at every time point when comparing the Optimized Formulation with 1.0% pilo to the Generic Formulation, and the overall VAS scores were lower for the Optimized Formulation at both concentrations. The increased concentration of pilo in the Optimized Formulation (1.25%) may be why the VAS scores were higher at some time points at the second assessment. If the Generic Formulation also had a pilo concentration of 1.25%, the scores could have been lower with the Optimized Formulation for all time points.
The structure of pilocarpine is susceptible to hydrolysis at a physiologic pH; therefore, it is formulated at a pH around 4 for stability. Ocular solutions <pH 6.0 can cause increased discomfort upon instillation [10, 26]. The greater ocular comfort and reduced AEs associated with the Optimized Formulation may be due to its rapid equilibration to the physiologic pH of the tear film. The results from the in vitro study showed that the Optimized Formulation achieved faster pH equilibration, and the pilot study showed that participants had less ocular discomfort and fewer AEs with the Optimized Formulation. Together these results indicate that the rapid equilibration of the re-engineered formulation to the pH of the tear film may have improved the drop comfort and reduced AEs. In addition, the ocular bioavailability of the generic pilo is low (1–3%) [27], given that most of the drug in the tear film is in a protonated or ionized form that poorly crosses the cornea [11]. The immediate rise in pH rapidly increases the non-ionized proportion of pilo on the ocular surface, which may improve bioavailability because of higher membrane permeability [28]. This increased bioavailability translates to effective drug delivery to the anterior segment [10] and may contribute to the long duration of action.
Vision blur can be caused by the disruption of the tear film and ocular surface. As vision blur is often a symptom of the ocular surface disease, dry eye disease, previous dry eye disease studies have demonstrated that tear film irregularities and instabilities can impact optical quality [29,30,31]. The breakup of the tear film can lead to optical aberrations, such as vision blur [32]. Upon application, ocular drops can disrupt the ocular surface and tear film [30, 33, 34]. The rapid pH equilibration of the Optimized Formulation with the STF in the in vitro study indicates that the Optimized Formulation may disrupt the tear film and ocular surface less, resulting in less vision blur.
One limitation of this study is the low number of participants. Although only five participants were included in this study, the proprietary vehicle was also used in both phase 2 and 3 studies, and the safety and tolerability results are aligned with the findings from this study. The phase 2 study used the Optimized Formulation with various concentrations of pilo (0.5–1.5%). Results showed that the rate of AEs such as burning, stinging, vision blur, and headaches were lower compared to previous studies using pilo to treat glaucoma [8, 14,15,16,17]. A participant-reported Ocular Tolerability and Drop Comfort questionnaire showed that the majority reported “none” as the symptom severity level.
Conclusion
Overall, the proprietary vehicle used in the Optimized Formulation is expected to improve comfort, result in less vision blur, and provide a well-tolerated alternative to currently available ocular pilo medications. A re-engineered topical ophthalmic drop (AGN-190584) containing pilocarpine HCl (1.25%) delivered with the proprietary vehicle (pHast™ technology, Allergan, an AbbVie company) has recently been approved for the treatment of presbyopia.
References
Asbell PA, Potapova N. Effects of topical antiglaucoma medications on the ocular surface. Ocul Surf. 2005;3(1):27–40.
Patel A, Cholkar K, Agrahari V, Mitra AK. Ocular drug delivery systems: an overview. World J Pharmacol. 2013;2(2):47–64.
Inoue K. Managing adverse effects of glaucoma medications. Clin Ophthalmol (Auckland, NZ). 2014;8:903–13.
Gupta SK, Niranjan DG, Agrawal SS, Srivastava S, Saxena R. Recent advances in pharmacotherapy of glaucoma. Indian J Pharmacol. 2008;40(5):197–208.
Drummond PD. The effect of light intensity and dose of dilute pilocarpine eyedrops on pupillary constriction in healthy subjects. Am J Ophthalmol. 1991;112(2):195–9.
Skaat A, Rosman MS, Chien JL, Mogil RS, Ren R, Liebmann JM, et al. Effect of pilocarpine hydrochloride on the Schlemm canal in healthy eyes and eyes with open-angle glaucoma. JAMA Ophthalmol. 2016;134(9):976–81.
Lusthaus J, Goldberg I. Current management of glaucoma. Med J Austral. 2019;210(4):180–7.
Nagasubramanian S. A comparison of the ocular hypotensive efficacy, safety and acceptability of brimonidine 0.2% twice daily versus pilocarpine 2.0% thrice daily as adjunct therapy with beta-blockers. In: Glauoma update VI. Berlin: Springer; 2000. p. 203–8.
Lavik E, Kuehn MH, Kwon YH. Novel drug delivery systems for glaucoma. Eye. 2011;25(5):578–86.
Anderson RA, Cowle JB. Influence of pH on the effect of pilocarpine on aqueous dynamics. Br J Ophthalmol. 1968;52(8):607–11.
Mitra AK, Mikkelson TJ. Mechanism of transcorneal permeation of pilocarpine. J Pharmaceutical Sci. 1988;77(9):771–5.
Birmingham AT, Galloway NR, Spencer SA. A comparison of the pupilloconstrictor effect of pilocarpine solution administered to the conjunctival sac as a single drop or as a continuous infusion in normal subjects. Br J Ophthalmol. 1976;60(8):568–72.
Boger WP 3rd, Steinert RF, Puliafito CA, Pavan-Langston D. Clinical trial comparing timolol ophthalmic solution to pilocarpine in open-angle glaucoma. Am J Ophthalmol. 1978;86(1):8–18.
Hartenbaum D, Maloney S, Vaccarelli L, Liss C, Wilson H, Gormley GJ. Comparison of dorzolamide and pilocarpine as adjunctive therapy in patients with open-angle glaucoma and ocular hypertension. Clin Ther. 1999;21(9):1533–8.
Kaluzny J, Sobecki R, Czechowicz-Janicka K, Kecik D, Kaluzny BJ, Stewart JA, et al. Efficacy and safety of latanoprost versus pilocarpine/timolol maleate fixed combination in patients with primary open-angle glaucoma or ocular hypertension. Acta Ophthalmol. 2008;86(8):860–5.
Laibovitz R, Boyle J, Snyder E, Strohmaier K, Adamsons I. Dorzolamide versus pilocarpine as adjunctive therapies to timolol: a comparison of patient preference and impact on daily life. Clin Ther. 1996;18(5):821–32.
Ozdemir M, Ozdemir G. Comparison of the intraocular pressure lowering effect of latanoprost and carteolol-pilocarpine combination in newly diagnosed glaucoma. Jpn J Ophthalmol. 2003;47(1):72–6.
Laibovitz R, Strahlman ER, Barber BL, Strohmaier KM. Comparison of quality of life and patient preference of dorzolamide and pilocarpine as adjunctive therapy to timolol in the treatment of glaucoma. J Glaucoma. 1995;4(5):306–13.
Strahlman ER, Vogel R, Tipping R, Clineschmidt CM. The use of dorzolamide and pilocarpine as adjunctive therapy to timolol in patients with elevated intraocular pressure. The Dorzolamide Additivity Study Group. Ophthalmology. 1996;103(8):1283–93.
Goertz AD, Stewart WC, Burns WR, Stewart JA, Nelson LA. Review of the impact of presbyopia on quality of life in the developing and developed world. Acta Ophthalmol. 2014;92(6):497–500.
Radhakrishnan H, Charman WN. Age-related changes in static accommodation and accommodative miosis. Ophthalmic Physiol Opt. 2007;27(4):342–52.
Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125(10):1492–9.
Wolffsohn JS, Davies LN. Presbyopia: effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124–43.
Stokes J, Shirneshan E, Graham CA, Paulich M, Johnson N. Exploring the experience of living with and treating presbyopia. Virtual poster presented at: American Academy of Optometry Annual Meeting 2020; October 7, 2020. https://www.aaopt.org/detail/knowledge-base-article/psychometric-evaluation-of-the-near-vision-presbyopia-taskbased-questionnaire-using-phase-2b-clinical-trial-data. Accessed 24 Feb 2022.
Marques MRC, Loebenberg R, Almukainzi M. Simulated biological fluids with possible application in dissolution testing. Dissolut Technol. 2011;18(3):15–28.
Januleviciene I, Siaudvytyte L, Barsauskaite R. Ophthalmic drug delivery in glaucoma—a review. Pharmaceutics. 2012;4(1):243–51.
Jain N, Verma A, Jain N. Formulation and investigation of pilocarpine hydrochloride niosomal gels for the treatment of glaucoma: intraocular pressure measurement in white albino rabbits. Drug Deliv. 2020;27(1):888–99.
Shinno K, Kurokawa K, Kozai S, Kawamura A, Inada K, Tokushige H. Effect of solution pH on distribution of ophthalmically administered brimonidine in posterior ocular tissues in pigmented rabbits. Ophthalmol Ther. 2019;8(2):271–7.
Gouvea L, Waring GO, Brundrett A, Crouse M, Rocha KM. Objective assessment of optical quality in dry eye disease using a double-pass imaging system. Clin Ophthalmol (Auckland, NZ). 2019;13:1991–6.
Koh S, Tung CI, Inoue Y, Jhanji V. Effects of tear film dynamics on quality of vision. Br J Ophthalmol. 2018;102(12):1615.
Yu A-Y, Lu T, Pan A-P, Lin D-R, Xu C-C, Huang J-H, et al. Assessment of tear film optical quality dynamics. Invest Ophthalmol Vis Sci. 2016;57(8):3821–7.
Montés-Micó R. Role of the tear film in the optical quality of the human eye. J Cataract Refract Surg. 2007;33(9):1631–5.
Koh S, Maeda N, Ikeda C, Takai Y, Fujimoto H, Oie Y, et al. Effect of instillation of eyedrops for dry eye on optical quality. Invest Ophthalmol Vis Sci. 2013;54(7):4927–33.
Lu N, Lin F, Huang Z, He Q, Han W. Changes of corneal wavefront aberrations in dry eye patients after treatment with artificial lubricant drops. J Ophthalmol. 2016;2016:1342056.
Acknowledgements
Funding
This research was supported by Allergan plc, Dublin, Ireland (prior to its acquisition by AbbVie Inc.). Employees of AbbVie participated in the research, interpretation of data, review of the manuscript, and the decision to submit for publication. The journal’s Rapid Service Fee was funded by Allergan.
Authorship
All authors met the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. Neither honoraria nor payments were made for authorship.
Author Contributions
All authors contributed to the study conception and design. Jaya Giyanani, Yumna Shabaik, Jeff Penzner, and Anuradha Gore contributed to the data collection. All authors contributed to data interpretation, and critically reviewed and approved the final manuscript.
Medical Writing and Other Acknowledgements
Statistical analysis was provided by Tudor Tepelus, PhD of AbbVie Inc. Writing and editorial assistance was provided to the authors by Stephanie Kuwahara, PhD, of AbbVie and Evidence Scientific Solutions, Inc, Philadelphia, PA, funded by AbbVie. AbbVie and authors thank the participants and investigators participating in the clinical trial.
Disclosures
Jaya Giyanani, Yumna Shabaik, Jeff Penzner, Anuradha Gore, and Michael Robinson are full time employees of AbbVie Inc and may hold stock. Mitchell Jackson has consulted for Allergan (an AbbVie company) and Visus, and is a shareholder of Visionary Venture Fund and ACE Vision Group. George Waring has consulted for Allergan (an AbbVie company).
Compliance with Ethics Guidelines
The clinical study was approved by the Alpha Investigational Review Board (San Clemente, CA) and was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All subjects provided informed consent to participate in the study.
Data Availability
The clinical trial data can be requested by any qualified researchers who engage in rigorous, independent scientific research, and will be provided following review and approval of a research proposal and Statistical Analysis Plan (SAP) and execution of a Data Sharing Agreement (DSA). Data requests can be submitted at any time, and the data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvie.com/our-science/clinical-trials/clinical-trials-data-and-information-sharing/data-and-information-sharing-with-qualified-researchers.html.
Prior Presentation
The data in this manuscript were presented at Advancing Pharmaceutical Science, Careers, and Community (AAPS) 2020 and New Technologies and Treatment in Eye Care 2020 meetings.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jackson, M.A., Giyanani, J., Shabaik, Y. et al. In Vitro and In-Eye Comparison of Commercial Pilocarpine Ophthalmic Solution and an Optimized, Reformulated Pilocarpine for Presbyopia Treatment. Ophthalmol Ther 11, 869–879 (2022). https://doi.org/10.1007/s40123-022-00482-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00482-2