Abstract
Purpose
To evaluate the prognosis of patients with blunt trauma-mediated cyclodialysis cleft and lens subluxation treated by dual capsular tension rings (CTRs) with different preoperative intraocular pressures (IOPs).
Methods
Twenty-five patients with cyclodialysis cleft and lens subluxation after blunt trauma were recruited in this study. They were categorized into the low IOP group (IOP < 10 mmHg) and normal IOP group (between 10 mm and 21 mmHg). A modified CTR (MCTR) or CTR was sutured into the ciliary sulcus, and another MCTR or CTR was implanted in the capsular bag. The prognosis outcome measurements, including BCVA (LogMAR), IOP, UBM, and macular character on OCT, were collected during the regular outpatient follow-up after surgery until the recovery of cyclodialysis cleft was found. Measures of cyclodialysis cleft recovery included successful IOP control (defined as an IOP within 10–21 mmHg), confirmation of cleft closure on UBM, and confirmation of IOL centration under slit-lamp examination. Follow-up period or recovery time was regarded as the duration between discharge from the hospital after the operation and the recovery of cyclodialysis cleft. The longest follow-up period was 1 year.
Results
Cyclodialysis cleft was successfully treated in 21/25 eyes, whereas lens subluxation was treated effectively in all 25 eyes. CTRs and IOLs were stable in all eyes. BCVA (P < 0.001) and IOP (P < 0.001) were significantly improved after surgery. The primary surgical complication included reversible IOP spike in seven eyes. Postoperative BCVA was found to have correlation with the preoperative IOP (P = 0.016), maculopathy (P = 0.002,), and trauma duration (P = 0.046). Worse BCVA (P = 0.037) and more severe grade of maculopathy (P = 0.030) were observed in the low IOP group (14 eyes). In contrast, a better prognosis and greater probability of IOP spike (P = 0.021) were observed in the normal IOP group (11 eyes).
Conclusion
Timely and proper intervention for traumatic cyclodialysis cleft associated with lens subluxation is essential. Lower preoperative IOP is associated with worse prognosis and prolonged recovery time, while caution should be taken in IOP spike monitoring in patients with normal preoperative IOP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Traumatic cyclodialysis coexisting with lens subluxation is rare and complicated. It can further cause hypotony, leading to several associated complications, such as cataracts. Early detection and surgical recovery of ciliary body separation and lens dislocation are helpful in the recovery of visual function. However, the relationship between preoperative intraocular pressure and patient prognosis remains unclear. |
What was learned from the study? |
Timely and proper intervention for traumatic cyclodialysis cleft associated with lens subluxation is essential. Lower preoperative IOP is associated with worse prognosis and prolonged recovery time, while caution should be taken in IOP spike monitoring in patients with normal preoperative IOP. |
Digital Features
This article is published with digital features, including videos to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.18406931.
Introduction
Cyclodialysis cleft occurs because of separation of the longitudinal ciliary muscle fibers from the scleral spur, creating an abnormal and additional pathway for the aqueous humor drainage [1]. Excessive drainage of aqueous humor along with hypofunction of the ciliary body leads to chronic hypotony and associated complications [2]. Reported incidences of blunt trauma-mediated cyclodialysis cleft are between 1 and 11% of all the cases [3]. In addition, the incorrect insertion of the ciliary body from the origin of the lens zonular fibers can cause zonular weakness and lens subluxation [1, 4, 5]. Cyclodialysis itself is a rare condition; traumatic cyclodialysis coexisting with lens subluxation is even more uncommon and complicated. Conservative management does not help in the resolution of lens subluxation in cyclodialysis patients; hence, prompt surgical interventions are necessary. Early detection with accurate intervention helps in restoration of the apposition of the detached ciliary body and dislocated lens, which further aids in the recovery of visual function [6].
Various surgical methods are employed for the management of cyclodialysis [7,8,9,10,11], though using a classic surgical procedure of direct cyclopexy can only resolve the problem of cyclodialysis cleft but requires extensive surgical skills [12]. Moreover, after direct cyclopexy, patients still require a secondary intervention for traumatic cataracts, lens subluxation, vitreous prolapse, and so on. Therefore, an innovative and combined surgical method could offer a better interventional option. Gupta et al. [13] used the procedure of placing two capsular tension rings (CTRs) for treating blunt trauma-mediated cataract, zonular dialysis, iridodialysis, and cyclodialysis. We also previously used the method of dual CTRs combined with phacoemulsification while dealing with traumatic cyclodialysis cleft and zonular dialysis [6]. During the procedure, a modified capsular tension ring (MCTR) suturing was pushed toward the maximum height of the cleft, which resulted in the re-attachment of the detached ciliary body to the scleral spur by direct mechanical tamponade. Meanwhile, lens subluxation was treated by phacoemulsification and CTR implantation. This modified surgical intervention was beneficial in reducing patient’s pain, the risk of repeated surgery, and the financial burden. Of note, this technique involved a small incision, use of routine technique, minimal sutures, and fewer complications.
Cyclodialysis cleft can further cause hypotony, leading to several associated complications, such as cataracts, optic disk swelling, refractive changes, retinochoroidal folds, and maculopathy. Interestingly, in our previous study, normal intraocular pressure (IOP) was seen after traumatic cyclodialysis cleft [6]. However, changes in IOP after traumatic cyclodialysis cleft can be attributed to lens dislocation, shallow anterior chamber, anterior segment inflammation, anterior chamber angle closure, vitreous prolapse, peripheral anterior synechiae, and so on. However, during our clinical observation, we noted better best-corrected visual acuity (BCVA) and susceptibility to transient IOP rise in these normal IOP patients.
In the present study, the patients with cyclodialysis cleft and lens subluxation after blunt trauma were categorized into the normal IOP group (preoperative IOP from 10 to 21 mmHg) and low IOP group (preoperative IOP < 10 mmHg). All the patients underwent the same surgical procedure as reported before [6]. The two groups were compared postoperatively for BCVA, IOP spike, and macular changes to determine the differences in prognosis due to different preoperative IOPs.
Methods
Compliance with Ethics Guidelines
All procedures performed on human participants followed the 1964 Declaration of Helsinki and its later amendments after receiving proper approval from the Human Research Ethics Committee of the Eye & ENT Hospital of Fudan University (no. 2020126-1). Furthermore, informed consent was obtained from all participants and the guardians of those under 18 years of age. Informed consent for publication was obtained from all participants.
Patients
The study recruited 25 eligible patients in this prospective case series study, from January 2017 to December 2019, who attended the ophthalmology clinic at the Eye and ENT Hospital of Fudan University, Shanghai, China. Cyclodialysis cleft was diagnosed as previously reported [14]. Inclusion criteria: Patients with cyclodialysis cleft and lens subluxation after blunt trauma who underwent combined insertion of a CTR or MCTR into the ciliary sulcus and another CTR or MCTR into the capsular bag. Exclusion criteria: (1) patients with concomitant vitrectomy for severe ectopia lentis and vitreous prolapse; (2) patients with severe ocular complications such as scleral laceration and choroidal laceration; (3) patients with traumatic maculopathy except for hypotony maculopathy; (4) follow-up loss; (5) history of vision correction surgery, glaucoma, keratoconus, uveitis, or retinal detachment.
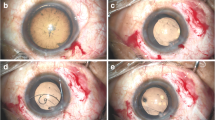
Preoperative Measures
Preoperative data collection included demographic profile, trauma history and duration of trauma, BCVA, IOP, anterior chamber depth (ACD), cyclodialysis cleft size, axial length, and maculopathy. The BCVA measurements were converted to logarithm of the minimal angle of resolution (logMAR) notation. Slit-lamp examination, non-contact tonometer (CT-80, Topcon Medical Systems, Oakland, NJ, USA), B-scan ultrasonography (Aviso, Quantel Médical, Clermont-Ferrand, France), partial coherence interferometry (IOLMaster 500 and 700, Carl Zeiss Meditec AG, Jena, Germany), optical coherence tomography (Spectrialis OCT, Heidelberg Engineering, Heidelberg, Germany), and UBM (MD-300 L, MEDA, Tianjin, China) were performed in all patients. Hypotony maculopathy was diagnosed as described by Costa et al. [15]. For statistical analysis, maculopathy was graded as normal (grade 0), mild chorioretinal folds (grade 1), moderate chorioretinal folds with macular fovea edema (grade 2), and severe macular change such as severe edema and retinal thinning (grade 3) (Fig. 1).
Surgical Plan
All surgeries were performed by the same surgeon (Dr. YX Jiang). The surgical procedure was adopted as described by Jiahui Chen [6]. The operation process is briefly described as follows: Under anesthesia or general anesthesia, an upper transparent corneal tunnel incision and puncture are performed. After standard stopping and chopping or tilting and rolling phacoemulsification techniques and cortical aspiration, the viscous OVD is re-injected into the capsular bag. CTR (Morcher Type 14C, Type 14A or Type 14, GmbH, Germany) or MCTR (Morcher Type 1 L or Type 2C, GmbH, Germany) with perforation preset with 9-0 polypropylene is aligned along the zonular dialysis zone. The capsular bag is implanted to support the zonules, and then a foldable intraocular lens is inserted into the capsule. After zonular dialysis, a 13-mm Morcher Type 2 L CTR (Morcher GmbH, Germany), MCTR, with two perforations is pre-placed into the ciliary sulcus with 10-0 polypropylene, and then the end of the Prolene suture is placed on the sclera and it is tied 1 mm behind the edge of the surgical site. The location of a small hole is pushed to the maximum height of the fissure, which causes the detached ciliary body to be reconnected to the scleral spur via direct mechanical packaging. Furthermore, the cyclodialysis cleft closure was confirmed by gonioscopy at the end of surgery. (Supplementary Material: Surgical video 1 and 2).
Postoperative Outcome Measures
Postoperative follow-up measurements, including BCVA, IOP, UBM, B-scan ultrasonography, and macular character on OCT, were collected during the regular outpatient follow-up after surgery (1 month, 3 months, 6 months, 9 months, and 12 months), until the recovery of cyclodialysis cleft was found in two consecutive follow-ups. Measures of cyclodialysis cleft recovery included a successful IOP control (defined as an IOP within 10–21 mmHg), confirmation of cleft closure on UBM, and confirmation of IOL centration under slit-lamp examination. Follow-up period or recovery time was regarded as the duration between discharge from the hospital after the operation and the recovery of cyclodialysis cleft. The longest follow-up period was 1 year. Eyes with postoperative IOP spikes received antiglaucoma eye drops.
Statistical Analysis
Statistical analyses were performed using SPSS version 26.0 (IBM Corp., Armonk, NY, USA). The data distribution was confirmed by the Shapiro-Wilk test. Quantitative variables were presented as mean ± standard deviation whereas the median (quartiles) and categorical statistics were described in the counts. Independent t-test or Mann-Whitney U-test was applied as appropriate to compare the clinical characteristics between the two groups. Wilcoxon signed rank test or paired t-test was used for pre- and postoperative parameters. Chi-square test or Fisher's exact probability test was used for categorical variables, such as IOP spike and maculopathy, between the two groups. Pearson's or Spearman's correlation analysis was used to explore the relevant factors. The results of two-tailed tests were considered significant at P < 0.05.
Results
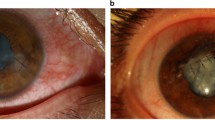
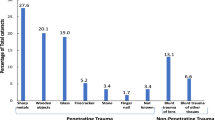
Twenty-five eyes of 25 patients were enrolled in the present study (Fig. 2). The baseline characteristics between the two groups are presented in Table 1. Significant difference was observed in the IOP and macular change parameters only at baseline. During the procedure, one MCTR or CTR was successfully sutured into the ciliary sulcus, whereas another MCTR or CTR was implanted in the capsular bag after phacoemulsification. In this study, all patients were followed up for 3 to 12 months, with an average of 7.55 ± 4.03 months: low IOP group: 7.89 ± 2.53 (range: 6–12 months); normal IOP group 7.21 ± 3.13 (range: 3–11 months). Within 1 year after surgery, the cyclodialysis cleft was closed in 21 eyes (84%). Although clefts remained in four eyes at 1-year follow-up, no surgical intervention was required. CTRs and IOLs were stable in all the patients (25 eyes, 100.0%). At the final follow-up examination, BCVA improved from 1.1 ± 0.8 LogMAR before surgery to 0.2 ± 0.4 LogMAR after surgery (P < 0.001). IOP was also significantly increased from 9.6 ± 2.8 mmHg preoperatively to 13.1 ± 3.5 mmHg at the last postoperative follow-up (P < 0.001). First day post-surgery IOP spike was detected in seven eyes (28.0%), which was reversible and could be controlled by anti-glaucoma drugs. However, mild-to-severe maculopathy occurred in 16 patients (64%). Importantly, postoperative BCVA had a significant correlation with preoperative IOP (P = 0.016, r = − 0.486), maculopathy (P = 0.002, r = 0.596), and trauma duration (P = 0.046, r = − 0.420). Of note, no other serious complications were observed during the follow-up period.
Postoperative comparisons between the two groups are shown in Table 2. Postoperatively, significant differences were seen in BCVA, IOP, IOP spike ratio, and maculopathy. However, in both groups, BCVA and IOP were significantly improved (Fig. 3a, b).
In the normal IOP group, the postoperative BCVA was better (P = 0.037), while the incidence of IOP spike was significantly higher than in the low IOP group (6/11 vs. 1/14, P = 0.021). However, no significant correlation was observed between the IOP spike and BCVA for the normal IOP group (P = 0.147). Moreover, no case of a persistent elevated IOP was seen in this group; also patients without IOP spike maintained stable IOPs during the follow-up.
In the low IOP group, postoperative BCVA was comparatively poor (P = 0.037), with more severe postoperative macular change (P = 0.030). IOP recovery time also varied from 1 week to 6 months, and only four eyes reverted to normal IOP within 1 month postoperatively. Three eyes had low IOP (7.8 mmHg, 8.0 mmHg, 8.1 mmHg, respectively) until the last follow-up. However, IOP recovery time did not have an association with age (P = 0.617), duration of trauma (P = 0.660), preoperative IOP (P = 0.839), or cleft extension (P = 0.534).
Discussion
In the current study, 25 eyes with cyclodialysis cleft and lens subluxation were surgically treated with dual CTR implantation. Overall surgical results were satisfying; however, the prognosis of normal preoperative IOPs differed from that for low preoperative IOPs.
Cyclodialysis combined with lens subluxation is a rare but intricate situation. When and how to operate are worth exploring. Conflicting views exist on the surgical intervention timing for treating cyclodialysis cleft. Ormerod [5] suggested that IOP restoration within 2 months was associated with better prognosis, whereas Jing et al. [4] advised closing the cyclodialysis as soon as possible after the diagnosis. While many reported significant visual recoveries after many years of cyclodialysis onset, the longest documented interval was 30 years [16, 17]. Agrawal and Hwang [16, 18] found no correlation between the duration of hypotony and final visual acuity in these patients. In the present study, a significant correlation was observed between the postoperative BCVA and time of trauma. Based on the findings, we suggest a prompt intervention for cyclodialysis cleft, especially if it is accompanied by lens subluxation.
IOP reduction is the focal point for the cyclodialysis cleft. However, occurrence of normal IOP in patients with cyclodialysis and zonular dialysis might occur because of the mixed etiology, which reduces the outflow of aqueous humor from the trabecular meshwork. Of note, preoperative IOP was higher in the present study than in previous reports [16, 19, 20]; however, only a few patients met the criteria for “statistical” hypotony [21]. Therefore, we chose the lower limit of normal IOP (10 mmHg) based on the grouping standard to investigate the clinical outcomes in different preoperative IOPs.
The etiopathogenesis of traumatic maculopathy has been suggested to be due to a combination of hemodynamic forces that lead to vascular damage of the nerve fiber layer (such as hypotony maculopathy) and direct mechanical forces that lead to photoreceptor and retinal pigment epithelium destruction (such as choroidal ruptures, submacular hemorrhages, traumatic macular holes, and photoreceptor and retinal pigment epithelium injury). In this study, we evaluate the outcome of patients with blunt trauma-mediated cyclodialysis cleft and lens subluxation treated by dual CTRs in different preoperative IOPs. Except for hypotony maculopathy, patients with another traumatic maculopathy were excluded. Hypotony maculopathy is caused by inward scleral wall collapse, causing redundancy of the choroid and retina, which eventually leads to chorioretinal folds, vascular tortuosity, and disc edema, especially at the macula [15]. Although preoperative IOPs were not “typical” hypotony in our study, hypotony maculopathy was observed in our patients, especially in the low IOP group. OCT parameter was helpful and convenient for diagnosing hypotonous maculopathy. Murta suggested that vision loss probably happens because of the distortion and misalignment of photoreceptors [20]. Based on our observation, severe maculopathy such as irreversible macular edema and retinal thinning could cause complete loss of vision, while mild chorioretinal folds imposed a minor threat to BCVA. Some patients had visual acuity better than 15/25 despite the mild chorioretinal folds seen during follow-up. Of note, hypotony maculopathy was more severe and persistent in the low than normal IOP group, which resulted in worse BCVA.
IOP recovery was expected after closure of the cyclodialysis cleft. However, lower preoperative IOP patients required a long time to return to the normal range, whereas some patients had hypotony until our last follow-up at 6 months post-surgery. No significant factor was observed for IOP recovery time in the current study. The recovery and stability of IOP after cyclodialysis surgery are subtle processes, which mainly depend on restoring the ciliary body as well as the trabecular meshwork and eventual balance of secretion and aqueous humor outflow.
Sometimes, closure of the cyclodialysis cleft leads to a painful and unexpected IOP spike. However, in the present study, the incidence of IOP spike following surgical intervention was much lower than in the previous reports [11, 16], since our technique was minimally invasive and least interruptive to the anterior chamber angle. The incomplete recovery of trabecular meshwork function following the restoration of aqueous humor production by the ciliary body causes IOP spike [1]. Patients with normal IOP might conserve more residual aqueous humor secretion function or have severe anterior segment inflammation preoperatively. The immediate postoperative functional recovery in combination with inflammation might lead to an IOP spike, which can be easily controlled and hence does produce significant damage to the optic nerve. However, with the functional recovery of the trabecular meshwork, the IOP generally returns to the normal range [22]. Therefore, preoperatively normal IOP patients have a greater probability of IOP spike. Moreover these patients had satisfactory prognosis, confirming that such transient spikes cause little to no damage to the eye. According to Murta et al. and Kato et al., IOP spike eventually plays a positive role in flattening retinal and choroidal folds and in re-attachment of the ciliary body to the scleral spur [20, 23]. In our study, the IOP spike's impact on choroidal detachment was also explored. Although there was a differential tendency in the recovery time of choroidal detachment in patients with or without IOP spike, no significant difference was observed, probably because of the relatively small sample size.
The present study had the limitation of small sample size and short follow-up time as some patients were lost to follow-up because of COVID-19. Also, considering the rarity of cyclodialysis cleft, most of the other published papers are single case reports. However, precise expertise in this rare disease requires larger samples and long-term observations. Also, if we had a larger sample size, a multivariable model could be considered.
Conclusions
To conclude, our method using dual CTRs to treat cyclodialysis cleft associated with lens subluxation was found to be safe and effective; however, prompt intervention is recommended. Patients with different preoperative IOPs had different prognoses. Therefore, informed consent for low IOP subjects should include a long recovery time and dissatisfaction with visual function recovery.
References
Gonzalez-Martin-Moro J, Contreras-Martin I, Munoz-Negrete FJ, Gomez-Sanz F, Zarallo-Gallardo J. Cyclodialysis: an update. Int Ophthalmol. 2017;37:441–57. https://doi.org/10.1007/s10792-016-0282-8.
Ioannidis AS, Barton K. Cyclodialysis cleft: causes and repair. Curr Opin Ophthalmol. 2010;21:150–4. https://doi.org/10.1097/ICU.0b013e3283366a4d.
Grosskreutz C, Aquino N, Dreyer EB. Cyclodialysis. Int Ophthalmol Clin. 1995;35:105–9. https://doi.org/10.1097/00004397-199503510-00011.
Jing Q, Chen J, Chen J, Tang Y, Lu Y, Jiang Y. Cionni-modified capsular tension ring for surgical repair of cyclodialysis after trabeculectomy: a case report. BMC Ophthalmol. 2017;17:196. https://doi.org/10.1186/s12886-017-0582-4.
Ormerod LD, Baerveldt G, Sunalp MA, Riekhof FT. Management of the hypotonous cyclodialysis cleft. Ophthalmology. 1991;98:1384–93. https://doi.org/10.1016/s0161-6420(91)32121-3.
Chen J, Lan L, Tang Y, Lu Y, Jiang Y. Placement of dual capsular tension rings for the combined management of traumatic cyclodialysis cleft and zonular dialysis. Eye Vis (Lond). 2020;7:54. https://doi.org/10.1186/s40662-020-00219-x.
Xu WW, Huang YF, Wang LQ, Zhang MN. Cyclopexy versus vitrectomy combined with intraocular tamponade for treatment of cyclodialysis. Int J Ophthalmol. 2013;6:187–92. https://doi.org/10.3980/j.issn.2222-3959.2013.02.16.
Yuen NS, Hui SP, Woo DC. New method of surgical repair for 360-degree cyclodialysis. J Cataract Refract Surg. 2006;32:13–7. https://doi.org/10.1016/j.jcrs.2005.05.035.
Gupta S, Sagar P, Gogia V, Khokhar S, Dada T. Dual endotemponade for extensive long-standing cyclodialysis using sulcus-fixated cionni ring and PCIOL. J Glaucoma. 2016;25:e284-287. https://doi.org/10.1097/IJG.0000000000000334.
Mardelli PG. Closure of persistent cyclodialysis cleft using the haptics of the intraocular lens. Am J Ophthalmol. 2006;142:676–8. https://doi.org/10.1016/j.ajo.2006.05.027.
Popovic M, Shareef S, Mura JJ, Valenzuela F, Gonzalez Martin-Moro J, Schlenker MB, Barton K, Munoz-Negrete F, Razeghinejad MR, Ahmed IIK. Cyclodialysis cleft repair: a multi-centred, retrospective case series. Clin Exp Ophthalmol. 2019;47:201–11. https://doi.org/10.1111/ceo.13378.
Selvan H, Gupta V, Gupta S. Cyclodialysis: an updated approach to surgical strategies. Acta Ophthalmol. 2019;97:744–51. https://doi.org/10.1111/aos.14210.
Gupta S, Selvan H, Shakrawal J, Gupta V. One-step management of post-traumatic triple dialysis using two rings. Eur J Ophthalmol. 2019;29:9–13. https://doi.org/10.1177/1120672118803520.
Gonzalez Martin-Moro J, Munoz-Negrete FJ, Rebolleda G, Lara Medina J, Garcia-Feijoo J. Ultrasonic biomicroscopic findings after spontaneous resolution of a traumatic cyclodialysis. Arch Soc Esp Oftalmol. 2003;78:211–4.
Costa VP, Arcieri ES. Hypotony maculopathy. Acta Ophthalmol Scand. 2007;85:586–97. https://doi.org/10.1111/j.1600-0420.2007.00910.x.
Agrawal P, Shah P. Long-term outcomes following the surgical repair of traumatic cyclodialysis clefts. Eye (Lond). 2013;27:1347–52. https://doi.org/10.1038/eye.2013.183.
Chadha N, Lamba T, Belyea DA, Merchant KY. Indirect cyclopexy for treatment of a chronic traumatic cyclodialysis cleft with hypotony. Clin Ophthalmol. 2014;8:591–4. https://doi.org/10.2147/OPTH.S55938.
Hwang JM, Ahn K, Kim C, Park KA, Kee C. Ultrasonic biomicroscopic evaluation of cyclodialysis before and after direct cyclopexy. Arch Ophthalmol. 2008;126:1222–5. https://doi.org/10.1001/archopht.126.9.1222.
Sen A, Joshi R, Kashikar R, Jain T. Novel technique for traumatic cyclodialysis repair with phacoemulsification and Cionni’s ring implantation. Indian J Ophthalmol. 2019;67:1748–50. https://doi.org/10.4103/ijo.IJO_394_19.
Murta F, Mitne S, Allemann N, Paranhos Junior A. Direct cyclopexy surgery for post-traumatic cyclodialysis with persistent hypotony: ultrasound biomicroscopic evaluation. Arq Bras Oftalmol. 2014;77:50–3. https://doi.org/10.5935/0004-2749.20140013.
Wang Q, Thau A, Levin AV, Lee D. Ocular hypotony: a comprehensive review. Surv Ophthalmol. 2019;64:619–38. https://doi.org/10.1016/j.survophthal.2019.04.006.
Shentu X, Zhu Y, Tang Y. Closure of a persistent cyclodialysis cleft using the haptics of a normal-sized intraocular lens. BMJ Case Rep. 2011. https://doi.org/10.1136/bcr.07.2011.4555.
Kato T, Hayasaka S, Nagaki Y, Matsumoto M. Management of traumatic cyclodialysis cleft associated with ocular hypotony. Ophthalmic Surg Lasers. 1999;30:469–72.
Acknowledgements
Funding
This study was supported by the Shanghai Science and Technology Commission (grant no. 20Y119110), the Shanghai Science and Technology Commission (Scientific Innovation Action Plan, grant no. 18411965200), the National Key R&D Program (grant no. 2018YFC0116004), and the National Natural Science Foundation of China (grant no. 82070943).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Concept and design: Yongxiang Jiang; statistical analysis: Li Ning, Yinuo Wen, Tianhui Chen, Lina Lan, ZeXu Chen, and Yongxiang Jiang; drafting the manuscript: Li Ning, Ying Yang, Tianhui Chen, and Yongxiang Jiang.
Disclosures
Li Ning, Yinuo Wen, Lina Lan1, Ying Yang, Tianhui Chen, ZeXu Chen, Jiahui Chen, and Yongxiang Jiang have nothing to disclose.
Compliance with Ethics Guidelines
All procedures performed on human participants followed the 1964 Declaration of Helsinki and its later amendments after receiving proper approval from the Human Research Ethics Committee of the Eye & ENT Hospital of Fudan University (no. 2020126-1). Informed consent was obtained from all participants and the guardians of those under 18 years of age. Informed consent for publication was obtained from all participants.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 88074 KB)
Supplementary file2 (MP4 145199 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ning, L., Wen, Y., Lan, L. et al. Effect of Different Preoperative Intraocular Pressures on the Prognosis of Traumatic Cyclodialysis Cleft Associated with Lens Subluxation. Ophthalmol Ther 11, 689–699 (2022). https://doi.org/10.1007/s40123-022-00468-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00468-0