Abstract
Ophthalmic viscoelastic devices (OVDs) are currently used in cataract surgery and have significantly improved the safety and effectiveness of this surgical procedure. OVDs are classified according to the zero-shear viscosity and the cohesion-dispersion index in cohesive, dispersive, and viscoadaptives. OVDs create and maintain anterior chamber depth and visibility, protecting the corneal endothelium and other intraocular tissues during surgery. The selection of the most adequate OVD is especially relevant when performing cataract surgery in challenging cases, such as in hard, mature cataracts, flat anterior chamber, pseudoexfoliation syndrome, intraoperative floppy iris syndrome, or glaucoma surgery. In such cases, OVD is crucial for facilitating the surgical procedure and the associated minimal complication rate. The use of a combination of OVDs (soft-shell technique and modifications), the use of blue-colored OVDs, and the combination of sodium hyaluronate with lidocaine have also been described as useful tools in some of these challenging cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This review article presents an overview of ophthalmic viscoelastic devices (OVDs) and their application in difficult cases in ophthalmology |
OVDs in cataract surgery protect ocular structures from mechanical trauma, divide tissue, create space, resolve adhesions, act as a wetting agent, or as an instrument to facilitate the surgical procedure |
Good knowledge of all OVD types is mandatory for ophthalmic surgeons to achieve the best results |
Introduction
In 1934, hyaluronic acid was identified by Karl Meyer and John Palmer (Columbia University, New York) as an isolate from the vitreous body of cows, a fact that is considered to be the beginning of the development of ophthalmic viscoelastic devices (OVDs) for ocular surgery [1]. Indeed, hyaluronic acid is currently considered the first precursor of modern OVDs. This substance is a linear polysaccharide molecule consisting of sodium glucuronate and N-acetylglucosamine that has very good wetting and water binding properties, acting also as a lubricant [1]. A Hungarian chemist, Endre Balazs, later managed to extract pure hyaluronic acid from rooster combs, suggesting the use of this viscoelastic substance in orthopedics and ophthalmology, initially as a vitreous substitute [2].
The first clinical use of sodium hyaluronate 1% during cataract surgery was carried out by Drs. Robert Stegmann and David Miller in 1979 [3]. A short time later (1980–1983), the company Pharmacia started the worldwide marketing of this substance for ocular surgery, obtaining official approval by the US Food & Drug Administration (FDA) [4]. Ophthalmic surgeons, including pioneers such as Steve A. Arshinoff, soon started testing and exploring these substances in the clinical daily routine [5]. Around the same time, Fechner described the use of 1% methylcellulose to maintain the volume of the anterior chamber during cataract surgery, being presented as a cheaper alternative to hyaluronic acid [6].
OVDs are currently used in cataract surgery and have significantly improved the safety and effectiveness of this surgical procedure [7, 8]. Specifically, OVDs create and maintain anterior chamber depth and visibility as well as protect the corneal endothelium and other intraocular tissues during surgery [7, 8]. Currently, there are a growing number of commercially available OVDs, differing in rheologically active polymeric substances, concentrations, and chain lengths [9, 10]. Specifically, differences among OVDs in these factors determine their level of cohesion, viscosity, and elasticity, as well as other physical and chemical properties [10].
The protective effect of OVDs is especially relevant in challenging cases, such as in hard cataract surgery [11] or flat anterior chamber cases [12], minimizing the impact of the surgical procedure on the intraocular tissues and therefore contributing to a faster recovery [7, 8]. The aim of the current narrative review was to compile all the scientific evidence concerning the utilization of OVDs in challenging cases, defining specific uses of these substances and their real clinical benefit.
Types of OVD
Classification of OVDs
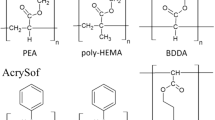
OVDs are a class of non-active, clear, gel-like chemical compounds with viscous and elastic properties [9, 10]. Most OVDs have the same three main components, which are sodium hyaluronate (NaHA), chondroitin sulfate (CS), and hydroxypropyl methylcellulose (HPMC) [9]. Hyaluronate is present in almost all connective tissues of vertebrates and consists of a relatively long linear polysaccharide molecule, playing an important role during embryonic development and growth [13]. Likewise, sodium hyaluronate plays a certain role in intercellular interaction, cell matrix adhesion, cell mobility, and extracellular organization, accelerating the wound healing processes and representing a natural biological wetting substance [13]. CS is a polysaccharide and, like hyaluronic acid, is present primarily in solid tissue parts (e.g., cartilage or corneal stroma) of the extracellular matrix [9]. For its use as an OVD, it is primarily obtained from shark fin cartilage, having a molecular weight of approximately 20,000 Da [9]. Methylcellulose is a polysaccharide that is found in cotton and wood [9], but not in animals or humans, being commonly used as a lubricant owing to its good wetting and coating properties [14]. The human body cannot fully metabolize methylcellulose and therefore residues or remnants can lead to inflammation [15].
Differences in the specific properties of each OVD are not only due to differences in chemical composition but also to differences in concentration, molecular weight, and size of the molecular building blocks of the material [9, 10]. The rheological properties of OVDs determine their behavior and the potential benefit of using them in specific situations. The following properties that act synergistically are used to characterize each OVD [10, 16]:
-
Viscosity: it describes the flow resistance of OVD. Viscosity changes with different flow rates. The faster an OVD flows, the more the viscosity decreases. This is measured in the ease of injection of the material and is crucial for the mobilizing effects of OVDs during surgery. It is important to note that the viscosity of an OVD is higher when the molecular weight at low shear rate increases [17].
-
Viscoelasticity: it describes the elastic component of the OVD. Therefore, it represents the ability to return to its original shape after being subjected to an external force.
-
Pseudoplasticity: it is the property of OVDs to change from a highly viscous state at rest to an aqueous state at higher shear rates.
Initially, OVDs were classified into two main groups, cohesive and dispersive, according to their rheological properties (Table 1, Fig. 1) [9]:
-
Cohesive OVDs: they are high-viscosity materials with intramolecular adhesion and entanglement that are particularly useful to create and maintain space in the anterior chamber for a long time [18,19,20,21,22]. Cohesive OVDs form as a mass and they are easier to be removed as a kind of bolus at the end of the surgical procedure [23].
-
Dispersive OVDs: they are low-viscosity materials with good adherence properties to intraocular structures and instruments, providing special protection to the corneal endothelium during phacoemulsification [16, 18,19,20,21,22, 24, 25]. However, they are more fragile as a result of their short molecular chains and consequently are more difficult to be remove after finishing surgery [16, 26]. This may result in postoperative OVD residues in the anterior chamber, which can lead to an increase of intraocular pressure (IOP) [27].
The classical classification of OVDs into cohesive and dispersive describes the intraoperative behavior of the various OVDs due to their rheological properties [9]. This classification was updated considering the analysis of zero-shear viscosity and the cohesion-dispersion index (CDI) [9]. According to this, OVDs are currently classified into four broad categories: cohesive (CDI ≥ 30%asp/mmHg), dispersive (CDI < 30%asp/mmHg), viscoadaptives, and combined agents or dual viscoelastic systems [9].
Cohesive OVDs
As previously mentioned, cohesive OVDs show high viscosity and act like a gel [9]. They can be divided into superviscous (105–106 millions) and viscous (105–106 hundreds of thousands), depending on the range of zero-shear viscosity [9]. Cohesive OVDs adhere well to themselves through intramolecular interactions and can therefore resist cleavage [16]. They generate a certain back pressure, having high surface tension and a high degree of pseudoplasticity due to their high molecular weight with long chains. Therefore, cohesive OVDs are excellent devices to create space and flatten the anterior capsule during capsulorhexis, especially in hyperopic eyes with a flat anterior chamber [16]. Likewise, they can be used to inflate the capsule during the intraocular lens (IOL) implantation process to facilitate a safe insertion of the implant [16]. Examples of commercially available cohesive OVDs are Provisc (Alcon), Healon/Healon GV (Johnson & Johnson Vision), Healon GV (Johnson & Johnson Vision), Pe-Ha-Luron F (Albomed GmbH), Ophteis Bio/FR/ + /MAX (Rayner), Provisc (Medline Industries, Inc.), ArtiVisc/ArtiVisc plus (Ophtec), Biolon (Amring Pharmaceuticals Inc.), Opegan Hi (Santen), HyVisc (MicroVisc), AJL Visc (AJL Ophtalmic), or Amvisc/Amvisc Plus (Bausch & Lomb) (Table 2).
Dispersive OVDs
Dispersive OVDs, owing to their lower viscosity and high coating ability, can coat intraocular structures and better adhere to them by enveloping them like a layer [9]. Their molecules behave separately and form a solution with low pseudoplasticity and surface tension, short chains, and low molecular weight, which acts like honey [9]. As a result of these characteristics, dispersive OVDs remain in place longer, having a better protective effect of the corneal endothelium and other intraocular tissues [9]. Most OVDs are also suitable to lubricate injector cartridges to make the sliding and injection of the folded intraocular lens easier, and can even be applied to the outer parts of the eye (epithelium) if the surgical procedure is very long [9]. Likewise, dispersive OVDs can better divide rooms and compartments, being especially useful after a posterior capsule tear [9]. However, as mentioned above, complete removal of dispersive OVDs from the eye is somewhat more complex and possible residue/OVD remnants may lead to an increase in intraocular pressure [16, 26, 27]. Examples of commercially available dispersive OVDs are Viscoat (Alcon), Healon D (Johnson & Johnson), Pe-Ha-Visco (Albomed GmbH), Opelead (Shisheido), Opegan (Santen), DisCoVisc (Alcon), Biovisc (Sophia Lab), Methylvisc (Rayner), Cellugel (Alcon), Vitrax (Johnson & Johnson), AJL Cell (AJL Ophthalmic), Celoftal (Alcon), Adatocel (Bausch & Lomb), Ocuvis (Vistamex), and OcuCoat (Bausch & Lomb) (Table 2).
Viscoadaptive OVDs
A new class of OVDs was introduced with the commercial release of Healon 5 from Johnson & Johnson, a viscoadaptive OVD. These substances behave as super-cohesive viscoelastic substances, exerting pressure and creating more space [9, 27]. They are pseudo-dispersive and ultra-viscous cohesive, with a CDI ≥ 30 (%asp/mmHg) and within a zero-shear viscosity range from 7 to 18 × 106 (tens of millions) [9]. As these OVDs can have different flow rates, they can also offer protection for structures, such as the corneal endothelium [8, 27]. Examples of commercially available viscoadaptive OVDs are Healon 5 (Johnson & Johnson), iVisc (MicroVisc Phaco), and BD MultiVisc (MicroVisc Phaco).
Combination of OVDs or Dual Viscoelastic Systems
Although there are some OVDs that share cohesive and dispersive properties, such as DisCoVisc (Alcon) or Amvisc Plus (Bausch & Lomb) [10, 20, 26, 28], cohesive and dispersive OVDs can be combined directly with the goal of obtaining the advantages of both [29]. The objective of these dual viscoelastic systems is to obtain long-lasting protection of the intraocular structures and corneal endothelium (dispersive characteristics), but also to facilitate the capsulorhexis and IOL implantation as well as its removal at the end of the surgery (cohesive characteristics) [7, 29]. Dual viscoelastic systems incorporate a dispersive OVD and a cohesive OVD in separate syringes [7, 18, 30]. A current example of a DuoVisc system that combines Viscoat (dispersive) and ProVisc (cohesive) is Twinvisc from Carl Zeiss Meditec (a combination of a dispersive and a cohesive OVD, both comprising sodium hyaluronate, in a single syringe separated by a bypass stopper system) or the combination of Healon D with Healon or Healon GV [7, 18, 30].
Another technique for combining OVDs is the soft-shell technique described by Steve A. Arshinoff in 1999 [31]. With this technique, two viscoelastic agents are used simultaneously. First, the dispersive OVD is injected into the eye and the endothelium is coated. Afterwards, the cohesive OVD is injected underneath to smooth the anterior lens capsule and deepen the anterior chamber as well as to push the dispersive OVD further towards the endothelium [31]. If the zonula is weak, the dispersive OVD can divide the eye and push the vitreous body backwards, while the cohesive OVD forms the anterior chamber and keeps it under pressure [31].
OVD Selection in Cataract Surgery
OVDs have become indispensable tools in modern cataract surgery, having a great impact on the success of the surgical procedure and on the IOL preparation/implantation process [7]. Several OVD types can be used for different purposes and at different stages during surgery. For example, the use of a cohesive OVD can help to enlarge a small and unresponsive pupil, to smooth the front capsule [17, 20,21,22,23], and to create space by deepening the anterior chamber, whereas a dispersive OVD is the best option to protect the corneal endothelium over a longer period [8, 19, 21, 22, 24]. A dispersive OVD is also needed when preparing an IOL, lubricating a cartridge, or folding a lens, but it is more difficult to be removed from the eye and more likely to increase the IOP [16, 18, 23, 24, 26]. For these reasons, there are also systems containing both types of OVD, cohesive and dispersive, as previously mentioned [7, 18, 29, 30]. Likewise, there are specific surgical strategies, such as the soft-shell technique [31], which use both OVD types in layers on top of each other. The goal of all these approaches is always to combine the advantages of cohesive and dispersive substances.
The selection of the appropriate OVDs is especially crucial in complex or challenging cases, such as in hard cataracts [11, 32], flat anterior chambers [12], narrow pupils and the pseudoexfoliation syndrome [33], intraoperative floppy iris syndrome [34], disinserted zonular fibers [34], Fuchs endothelial dystrophy [34], small holes in the posterior capsule with protruding vitreous [34], and hypotonic eyes due to previous glaucoma surgeries [35]. Indeed, the type of OVDs used in such cases may determine the success of the surgery, the postoperative outcome, and consequently the overall patient satisfaction. For this reason, it is important to know the OVDs commercially available and to understand their properties, leading to different advantages and disadvantages.
OVD Selection in Hard Cataracts
Cataract surgery in eyes with hard brown cataract or Brunescent and Morgagnian cataracts remains a challenge for eye surgeons because of the higher risk of complications, such as nucleus drop, posterior capsule rupture, corneal burn, and corneal endothelial damage [11, 32]. Of particular relevance are the potential effects of the longer surgical maneuvers and the higher levels of ultrasound energy commonly used in these cases on the corneal endothelium [36, 37]. For this reason, the use of dispersive OVDs seems to be an adequate option to achieve an optimal endothelial protective effect [32], although the use of combined agents may be adequate to facilitate also some surgical steps [38]. Toprak and Yaylali [11] described in 2019 two maneuvers to be used in different steps of phacoemulsification surgery in hard cataracts, providing debulking of the central dense nucleus and preventing posterior capsule rupture. These authors recommended the use of a cohesive OVD to fill the anterior chamber and to protect the corneal endothelium. Likewise, the OVD was used to inflate the capsular bag before IOL insertion, retreating the posterior capsule backward and safety preventing the rupture of this thin layer [11]. Yuan et al. [32] described the use of a cohesive OVD (sodium hyaluronate 1.5% at a molecular weight of 2,000,000 to 2,500,000 Da) to facilitate the extraction of the nucleus of a hard cataract. Specifically, the authors described a technique in which, after dislocation of the nucleus into the anterior chamber and OVD injection to protect the corneal endothelium and expand the capsular bag, the OVD cannula was passed beneath the nucleus, where more OVD was injected to promote its lifting. Subsequently, some pressure was applied to the posterior lip of the tunnel incision by the angle of the OVD needle, which allowed smooth extraction of the nucleus with the efflux of the OVD [32].
In a case series, Miyata and coauthors [38] demonstrated the safety and efficacy of corneal endothelial protection using the soft-shell technique (Healon + Viscoat) in hard-nucleus cataract eyes undergoing phacoemulsification surgery. Fasce and colleagues [39] confirmed in a randomized controlled clinical trial that the use of a viscoadaptive OVD (BD Multivisc) was as effective as the soft-shell technique (Biolon + Viscoat) in protecting the corneal endothelium in Fuchs dystrophy during phacoemulsification in patients with hard lens nucleus.
Moreover, it has been shown that viscodissection (rather than hydrodissection) in cases with very loose zonules (e.g., pseudoexfoliation, posttraumatic) is a safe and effective technique, minimizing the risk of zonulolysis.
Blue-Colored OVDs in Eyes with Mature, Dense Cataracts and Pseudoexfoliation
The pseudoexfoliation syndrome (PSX) is a complex age-related disorder characterized by the progressive accumulation of abnormal extracellular pseudoexfoliative material in ocular tissues, including the ciliary body, iris, iridocorneal angle, and lens capsule [40]. This may complicate the performance of cataract surgery due to pupillary abnormalities generated by this condition, such as significant miosis and a limitation of the dynamic pupillary pattern [40]. Indeed, iris hooks or Malyugin rings are sometimes needed for a mechanical pupil dilation allowing the surgeon to have an adequate visualization of the anterior segment [41]. A new tool to facilitate the surgical procedure in eyes with PSX and not reacting pupils is the use of an OVD combined with a staining agent [33]. Currently, there is only one commercially available system based on this concept that combines a sodium hyaluronate OVD with trypan blue, Pe-Ha-Blue® PLUS (Albomed GmbH, Schwarzenbruck, Germany). It is available in a prefilled syringe to allow for the simultaneous administration of the OVD and staining agent in one single step [33]. The aim of this blue-colored OVD is to deepen the anterior chamber, to protect the corneal endothelium, and simultaneously to stain the capsule, facilitating the creation of the continuous curvilinear capsulorhexis and surgery, and consequently minimizing the time needed for the procedure. A recent comparative case series has demonstrated that the use of this blue-colored OVD in PSX eyes with not reacting pupils can provide a statistically significant time gain in terms of surgery duration compared to the use of a standard clear OVD, with additional potential benefits in surgeon satisfaction, postoperative corrected distance visual acuity and IOP, as blue OVD remnants can be identified and removed more easily [33].
OVDs in Eyes with Intraoperative Floppy Iris Syndrome
In 2005, Chang and Campbell first described the intraoperative floppy iris syndrome (IFIS) in patients with benign prostatic hyperplasia and systemic administration of alpha-A1 adrenoceptor antagonist tamsulosin [42]. This condition is characterized by a loss of the iris muscle tone leading to significant pupil constriction despite pupil dilatation with standard mydriatic drugs before the initiation of cataract surgery. IFIS can lead to an increased complication rate in this type of eye surgery due to fluttering and billowing of the iris stroma caused by ordinary intraocular fluid flows, a marked tendency for the iris to prolapse toward the side port incisions, and progressive constriction of the pupil during surgery [43]. All these signs are accompanied by suboptimal pupillary dilation in response to preoperative mydriatic protocols [42]. In addition, pupillary stretching techniques are ineffective because of the floppy, easily stretched nature of the pupil margin [42, 44]. Since incision leakage through the clear-cornea incisions can further promote the IFIS effect, tight incisions and longer tunnels are essential in these cases when performing cataract surgery [44].
Chang recommended the use of iris hooks or other mechanical devices intraoperatively for pupillary dilation, such as the Malyugin ring [45]. However, a failure to detect IFIS before the performance of the capsulorhexis might make the use of these instruments more difficult [45]. Chang and Campbell found Healon 5 (Johnson & Johnson, Santa Ana, CA) to be useful in IFIS, not mentioning the use of more elaborate multiple-OVD techniques [42]. Steve A. Arshinoff described the use of OVD combinations in IFIS following two different techniques, tri-soft shell (TST) [34] and ultimate soft-shell technique (USST) [46]. As previously mentioned, the soft-shell technique consists of using two viscoelastic agents simultaneously to achieve a better iris stabilization during the entire procedure [31]. With this technique, the anterior chamber is first covered with a dispersive OVD by 75%. Afterwards, a cohesive OVD is injected onto the surface of the anterior lens capsule in the middle of the anterior chamber, maintaining the boundary between the cohesive and dispersive OVD at the pupil edge. This maneuver pushes the dispersive OVD up and out and stops the movement of the pupil (rigid OVD roof) [31].
The USST is a modification of the soft-shell technique consisting of compartmentalizing the anterior chamber using low-viscosity fluids, such as balanced salt solution or trypan blue, in combination with a viscoadaptive OVD, such as Healon 5 (sodium hyaluronate 2.3%) or I-Visc Phaco (sodium hyaluronate 2.5%) [46]. The use of this technique facilitates the surgical procedure owing to the effect of the viscoadaptive OVD and OVD removal at the end of the procedure [46]. In 2006, a combination variant of the soft-shell technique and USST was described, in which the flow parameters were adjusted [47]. The TST approach is a generalization of all these previously described soft-shell concepts [34]. The first step is to inject the dispersive OVD through the phaco-incision to form a central mound on the anterior capsule surface, stopping the injection once the anterior chamber is approximately 20–25% full. After this, a cohesive or viscoadaptive OVD is injected beneath the dispersive OVD onto the anterior capsule, displacing the dispersive OVD upward against the endothelial surface of the cornea. The injection of the second OVD is continued until the pupil stops dilating and before the eye becomes firm. With these maneuvers, a low-viscosity protective outer dispersive OVD shell is generated that encircles a cohesive or a viscoadaptive OVD pressurizing and stabilizing the inner shell previously created. Injection of balanced salt solution or lidocaine-phenylephrine is then performed slowly beneath the viscoadaptive OVD to create a continuous low-viscosity fluid on the lenticular surface, with the pupillary margin as the peripheral border. Consequently, the viscoadaptive shell is displaced upwards acting as a central bridge [34]. With this procedure, maximum control over the operative environment is achieved in IFIS eyes, minimizing the incidence of complications [34].
Use of OVDs with Lidocaine
Local anesthetic agents block the conduction of nerve impulses by acting directly on voltage-gated sodium channels. Intracameral injection of lidocaine affects all nerve fibers in the anterior chamber to some degree, causing anesthesia and akinesia of the iris. Several studies showed that the use of intracameral injection of lidocaine 1% as coadjuvant medication helps to achieve pupil dilatation [48, 49]. The intracameral anesthesia effect and OVD function maintenance of the anatomical space and protection of surrounding tissues were also combined in one single step [50,51,52,53]. One example of this type of combined system is VisThesia (Carl Zeiss Meditec, Jena, Germany) which combines 2% lidocaine and 0.3% sodium hyaluronate (volume 0.4 ml) provided in individual plastic blister packs [50,51,52]. This type of system may provide more comfort to patients, making the application of the anesthetic easy [50]. In fact, there is some scientific evidence of the superiority of the use of VisThesia compared to the conventional procedure in terms of intraoperative pain [50]. Some colleagues have reported a greater increase in macular thickness with the use of VisThesia [50] as well as a greater reduction of corneal endothelial cell density compared to the use of conventional OVDs [50, 51]. But results are contradictory with some other authors that showed no greater reduction of endothelial cell count with the use of VisThesia [52]. In 2008, Auffarth GU and Borkenstein AF presented at the annual conferences of ESCRS (Berlin) and DGII (Heidelberg) the results of their prospective safety study and showed no negative effect on endothelial cell count. More research is still needed to confirm the potential benefits and risks of the use of viscoanesthesia in cataract surgery as well as the most appropriate indications for this modality of OVD.
OVDs in Flat Anterior Chamber After Glaucoma Surgery
The formation of a significantly flat anterior chamber is a complication associated with eyes that have had previous glaucoma surgery [54]. One condition leading to this situation is the presence of overfiltration after trabeculectomy with mitomycin C, which has been shown to have an incidence of around 24% [54]. The persistence of a flat anterior chamber in the eye can cause further complications, such as peripheral anterior synechiae or endothelial dysfunction [54]. For this reason, this condition must be treated, for which various pharmacologic (atropine, phenylephrine, and in selected cases orally administered acetazolamide) and surgical options are available [55, 56]. One of these options is the injection of OVD into the anterior chamber, first described in 1982 by Fisher et al. [57] using sodium hyaluronate. Some years later, the successful use of a viscoadaptive OVD (Healon 5) to treat a flat anterior chamber after trabeculectomy was reported [58], as well as the application of dispersive OVDs [12]. However, the long-term success rate with OVD injection in these cases has been demonstrated to be relatively low [12]. For this reason, combinations of OVD with other stabilizing substances have been tested, such as the combination of Healon and sulfur hexafluoride [59].
From the prophylactic perspective, intracameral injection of 2% hydroxypropyl methylcellulose during trabeculectomy has been shown to maintain the anterior chamber depth, minimizing complications related to anterior chamber shallowing after trabeculectomy [60].
OVDs in Combined Procedures (DSEK, DALK)
In this relatively new field OVD is used for protection of corneal endothelium during posterior lamellar graft preparation and viscodissection.
Conclusions
OVDs in cataract surgery protect ocular structures from mechanical trauma, divide tissue, create space, resolve adhesions, act as a wetting agent, or as an instrument to facilitate the surgical procedure. OVDs can be classified as cohesive, dispersive, or viscoadaptive according to the level of viscosity and cohesion. There are also systems combining different OVDs or combining an OVD with other substances (anesthetic, trypan blue) that are commonly used for the most challenging cases to minimize the complication rate. The use of dispersive OVDs or combined agents seems to be the most optimal option to ensure adequate corneal endothelial protection in cases of hard cataract. Specifically, the soft-shell technique (sequential injection of a dispersive and a cohesive OVD) has been shown to be useful in eyes with a hard lens nucleus with and without Fuchs dystrophy. Concerning the blue-colored OVDs (Pe-Ha-Blue® PLUS), they have been successfully used in eyes with PSX or eyes with non-reacting pupils to facilitate a safe procedure, reducing the surgical time and minimizing toxic effects to the endothelium in these complex cases. Other challenging cases where the use of OVD is crucial are eyes with IFIS, where multiple-OVD techniques, such as the soft-shell, USST, or TST, are the best option to achieve complete control over the operative environment. Finally, the potential beneficial effect on the control of intraoperative pain with injection of a combination of OVD and lidocaine was also investigated, showing good results regarding the degree of pain control achieved. Good knowledge of all OVD types is mandatory for the ophthalmic surgeon to achieve the best results.
References
Kosiński J, Jarecki J, Przepiorka-Kosińska J, Ratajczak M. Hyaluronic acid in orthopedics. Wiad Lek. 2020;73:1878–81.
Balazs EA. Physical chemistry of hyaluronic acid. Fed Proc. 1958;17:1086–93.
Higashide T, Sugiyama K. Use of viscoelastic substance in ophthalmic surgery—focus on sodium hyaluronate. Clin Ophthalmol. 2008;2:21–30.
Food and Drug Administration (FDA). Healon, Healon GV, Healon5 products sodium hyaluronate ophthalmic viscoelastic devices. Regulation number: 886.4275, 01/14/1983.
Arshinoff SA, Hofmann I. Prospective, randomized trial of Microvisc and Healon in routine phacoemulsification. J Cataract Refract Surg. 1997;23:761–5.
Fechner PU, Fechner MU. Methylcellulose and lens implantation. Br J Ophthalmol. 1983;67:259–63.
Malvankar-Mehta MS, Fu A, Subramanian Y, Hutnik C. Impact of ophthalmic viscosurgical devices in cataract surgery. J Ophthalmol. 2020;2020:7801093. https://doi.org/10.1155/2020/7801093.
Van den Bruel A, Gailly J, Devriese S, Welton NJ, Shortt AJ, Vrijens F. The protective effect of ophthalmic viscoelastic devices on endothelial cell loss during cataract surgery: a meta-analysis using mixed treatment comparisons. Br J Ophthalmol. 2011;95:5–10.
Arshinoff SA, Jafari M. New classification of ophthalmic viscosurgical devices-2005. J Cataract Refract Surg. 2005;31:2167–71.
Watanabe I, Hoshi H, Sato M, Suzuki K. Rheological and adhesive properties to identify cohesive and dispersive ophthalmic viscosurgical devices. Chem Pharm Bull. 2019;67:277–83.
Toprak I, Yaylali V. “Crack, reduce, and implant”: a safe phaco technique in a case with hard brown cataract. Case Rep Med. 2019;2019:9043417. https://doi.org/10.1155/2019/9043417.
Hosoda S, Yuki K, Ono T, Tsubota K. Ophthalmic viscoelastic device injection for the treatment of flat anterior chamber after trabeculectomy: a case series study. Clin Ophthalmol. 2013;7:1781–5.
Balazs EA. Hyaluronan as an ophthalmic viscoelastic device. Curr Pharm Biotechnol. 2008;9:236–8.
Prinz A, Fennes C, Buehl W, Findl O. Efficacy of ophthalmic viscosurgical devices in maintaining corneal epithelial hydration and clarity: in vitro assessment. J Cataract Refract Surg. 2012;38:2154–9.
Behera UC, Sivakumar RR, Prajna L, Agrawal N, Rajan RP. Epiretinal deposits post cataract extraction. Retin Cases Brief Rep. 2013;7:359–61.
Arshinoff SA, Wong E. Understanding, retaining, and removing dispersive and pseudodispersive ophthalmic viscosurgical devices. J Cataract Refract Surg. 2003;29:2318–23.
Watanabe I, Mirumachi H, Konno H, Suzuki K. Evaluation of rheological properties of cohesive ophthalmic viscosurgical devices composed of sodium hyaluronate with high molecular weight. Yakugaku Zasshi. 2019;139:1121–8.
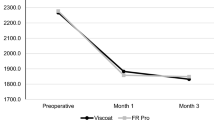
Auffarth GU, Auerbach FN, Rabsilber T, et al. Comparison of the performance and safety of 2 ophthalmic viscosurgical devices in cataract surgery. J Cataract Refract Surg. 2017;43:87–94.
Cutler Peck CM, Joos ZP, Zaugg BE, et al. Comparison of the corneal endothelial protective effects of Healon-D and Viscoat. Clin Experiment Ophthalmol. 2009;37:397–401.
Bissen-Miyajima H. In vitro behavior of ophthalmic viscosurgical devices during phacoemulsification. J Cataract Refract Surg. 2006;32:1026–31.
Maár N, Graebe A, Schild G, Stur M, Amon M. Influence of viscoelastic substances used in cataract surgery on corneal metabolism and endothelial morphology: comparison of Healon and Viscoat. J Cataract Refract Surg. 2001;27:1756–61.
Holzer MP, Tetz MR, Auffarth GU, Welt R, Völcker HE. Effect of Healon5 and 4 other viscoelastic substances on intraocular pressure and endothelium after cataract surgery. J Cataract Refract Surg. 2001;27:213–8.
Auffarth GU, Holzer MP, Visessook N, Apple DJ, Völcker HE. Removal times for a dispersive and a cohesive ophthalmic viscosurgical device correlated with intraocular lens material. J Cataract Refract Surg. 2004;30:2410–4.
Yildirim TM, Auffarth GU, Son H-S, Khorammia R, Munro DJ, Merz PR. Dispersive viscosurgical devices demonstrate greater efficacy in protecting corneal endothelium in vitro. BMJ Open Ophthalmol. 2019;4:e000227.
Kretz FTA, Limberger IJ, Auffarth GU. Corneal endothelial cell coating during phacoemulsification using a new dispersive hyaluronic acid ophthalmic viscosurgical device. J Cataract Refract Surg. 2014;40:1879–84.
Oshika T, Okamoto F, Kaji Y, et al. Retention and removal of a new viscous dispersive ophthalmic viscosurgical device during cataract surgery in animal eyes. Br J Ophthalmol. 2006;90:485–7.
Tognetto D, Cecchini P, Ravalico G. Survey of ophthalmic viscosurgical devices. Curr Opin Ophthalmol. 2004;15:29–32.
Modi SS, Davison JA, Walters T. Safety, efficacy, and intraoperative characteristics of DisCoVisc and Healon ophthalmic viscosurgical devices for cataract surgery. Clin Ophthalmol. 2011;5:1381–9.
Tognetto D, Cecchini P, D’Aloisio R, Lapasin R. Mixed polymeric systems: new ophthalmic viscosurgical device created by mixing commercially available devices. J Cataract Refract Surg. 2017;43:109–14.
Rainer G, Stifter E, Luksch A, Menapace R. Comparison of the effect of Viscoat and DuoVisc on postoperative intraocular pressure after small-incision cataract surgery. J Cataract Refract Surg. 2008;34:253–7.
Arshinoff SA. Dispersive-cohesive viscoelastic soft shell technique. J Cataract Refract Surg. 1999;25:167–73.
Yuan X, Song H, Hua X, Wilhelmus KR, Tang X. Ophthalmic viscosurgical device-assisted sutureless-incision cataract surgery for a hard nucleus or mature cataract. J Cataract Refract Surg. 2014;40:517–20.
Borkenstein AF, Borkenstein EM. Evaluation of a novel blue-colored ophthalmic viscoelastic device applied during phacoemulsification in eyes with pseudoexfoliation syndrome. Case Rep Ophthalmol. 2019;10:101–9.
Arshinoff SA, Norman R. Tri-soft shell technique. J Cataract Refract Surg. 2013;39:1196–203.
Oyakawa I, Hayashi T, Shimizu T, Kato N. Modified Descemet’s stripping automated endothelial keratoplasty: the use of ophthalmic viscoelastic devices in hypotonic eyes that had undergone glaucoma filtering surgeries. Case Rep Ophthalmol Med. 2018;2018:9387810.
Kim EC, Byun YS, Kim MS. Microincision versus small-incision coaxial cataract surgery using different power modes for hard nuclear cataract. J Cataract Refract Surg. 2011;37:1799–805.
Fakhry MA, El Shazly MI. Torsional ultrasound mode versus combined torsional and conventional ultrasound mode phacoemulsification for eyes with hard cataract. Clin Ophthalmol. 2011;5:973–8.
Miyata K, Nagamoto T, Maruoka S, Tanabe T, Nakahara M, Amano S. Efficacy and safety of the soft-shell technique in cases with a hard lens nucleus. J Cataract Refract Surg. 2002;28:1546–50.
Fasce F, Spinelli A, Bolognesi G, Rossi M, Gemma M. Comparison of BD Multivisc with the soft shell technique in cases with hard lens nucleus and Fuchs endothelial dystrophy. Eur J Ophthalmol. 2007;17:709–13.
Tekin K, Kiziltoprak H, Sekeroglu MA, Yetkin E, Bayraktar S, Yilmazbas P. Static and dynamic pupil characteristics in pseudoexfoliation syndrome and glaucoma. Clin Exp Optom. 2020;103:332–8.
Borkenstein AF, Borkenstein EM. Patient and surgeon satisfaction levels after using an acrylic, hydrophobic, monofocal IOL and the Malyugin ring in pseudoexfoliation syndrome patients. J Ophthalmol. 2018;2018:3843098.
Chang DF, Campbell JR. Intraoperative floppy iris syndrome associated with tamsulosin. J Cataract Refract Surg. 2005;31:664–73.
Haridas A, Syrimi M, Al-Ahmar B, Hingorani M. Intraoperative floppy iris syndrome (IFIS) in patients receiving tamsulosin or doxazosin-a UK-based comparison of incidence and complication rates. Graefes Arch Clin Exp Ophthalmol. 2013;251:1541–5.
Chang DF, Braga-Mele R, Mamalis N, et al. ASCRS White Paper: clinical review of intraoperative floppy-iris syndrome. J Cataract Refract Surg. 2008;34:2153–62.
Chang DF. Use of Malyugin pupil expansion device for intraoperative floppy-iris syndrome: results in 30 consecutive cases. J Cataract Refract Surg. 2008;34:835–41.
Arshinoff SA. Using BSS with viscoadaptives in the ultimate soft-shell technique. J Cataract Refract Surg. 2002;28:1509–14.
Arshinoff SA. Modified SST-USST for tamsulosin-associated intraoperative [corrected] floppy-iris syndrome. J Cataract Refract Surg. 2006;32:559–61.
Lundberg B, Behndig A. Intracameral mydriatics in phacoemulsification cataract surgery. J Cataract Refract Surg. 2003;29:2366–71.
Lee JJ, Moster MR, Henderer JD, Membreno JH. Pupil dilation with intracameral 1% lidocaine during glaucoma filtering surgery. Am J Ophthalmol. 2003;136:201–3.
Moschos MM, Chatziralli IP, Sergentanis TN. Viscoat versus Visthesia during phacoemulsification cataract surgery: corneal and foveal changes. BMC Ophthalmol. 2011;11:9.
Perone JM, Popovici A, Ouled-Moussa R, Herasymyuk O, Reynders S. Safety and efficacy of two ocular anesthetic methods for phacoemulsification: topical anesthesia and viscoanesthesia (VisThesia). Eur J Ophthalmol. 2007;17:171–7.
Poyales-Galan F, Pirazzoli G. Clinical evaluation of endothelial cell decrease with VisThesia in phacoemulsification surgery. J Cataract Refract Surg. 2005;31:2157–61.
Pandey SK, Werner L, Apple DJ, Izak AM, Trivedi RH, Macky TA. Viscoanesthesia. Part III: removal time of OVD/viscoanesthetic solutions from the capsular bag of postmortem human eyes. J Cataract Refract Surg. 2003;29:563–7.
Ono T, Yuki K, Shiba D, Abe T, Kouyama K, Tsubota K. Postoperative flat anterior chamber: incidence, risk factors, and effect on the long-term success of trabeculectomy. Jpn J Ophthalmol. 2013;57:520–8.
Monteiro de Barros DS, Kuntz Navarro JBV, Mantravadi AV, et al. The early flat anterior chamber after trabeculectomy: a randomized, prospective study of 3 methods of management. J Glaucoma. 2009;18:13–20.
Tunç Y, Tetikoglu M, Kara N, Sagdık HM, Özarpaci S, Elçioğlu MN. Management of hypotony and flat anterior chamber associated with glaucoma filtration surgery. Int J Ophthalmol. 2015;8:950–3.
Fisher YL, Turtz AI, Gold M, Cohen BZ, Uram M. Use of sodium hyaluronate in reformation and reconstruction of the persistent flat anterior chamber in the presence of severe hypotony. Ophthalmic Surg. 1982;13:819–21.
Hoffman RS, Fine IH, Packer M. Stabilization of flat anterior chamber after trabeculectomy with Healon5. J Cataract Refract Surg. 2002;28:712–4.
Geyer O, Segev E, Steinberg JM, Buckman G. Stabilization of post-trabeculectomy flat anterior chamber with Healon and sulfur hexafluoride. J Cataract Refract Surg. 2003;29:2026–8.
Agarwal HC, Anuradha VK, Titiyal JS, Gupta V. Effect of intraoperative intracameral 2% hydroxypropyl methylcellulose viscoelastic during trabeculectomy. Ophthalmic Surg Lasers Imaging. 2005;36:280–5.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded privately without external subsidies by the main author (AFB).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Andreas F Borkenstein was the leading author, designed the concept of the review article and wrote the draft of the manuscript. Eva-Maria Borkenstein and Boris Malyugin critically reviewed the manuscript and contributed significantly to the final manuscript.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Disclosures
Andreas F Borkenstein, Eva-Maria Borkenstein have no proprietary or commercial interest in the medical devices that are involved in this manuscript and confirm that they have nothing to disclose. Boris Malyugin has a financial interest in Malyugin-modified CTR and the Malyugin ring pupil expansion device. Microsurgical Technology Inc. (USA) - Royalties.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Borkenstein, A.F., Borkenstein, EM. & Malyugin, B. Ophthalmic Viscosurgical Devices (OVDs) in Challenging Cases: a Review. Ophthalmol Ther 10, 831–843 (2021). https://doi.org/10.1007/s40123-021-00403-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-021-00403-9