Abstract
Introduction
The aim of this study was to analyze the changes in corneal spherical aberration following regular ablation (RA) and wavefront-guided (WFG) ablations in photorefractive keratectomy (PRK) and laser-assisted in situ keratomileusis (LASIK).
Methods
A retrospective analysis was performed on the eyes that underwent femtosecond LASIK or PRK between January 2016 and December 2018. Changes in the corneal spherical aberration were measured preoperatively and postoperatively with a high-resolution Scheimpflug camera system, and they were correlated with the attempted correction and all other tomography parameters.
Results
Of the 3826 eyes that were reviewed, 484 eyes met the inclusion criteria and were enrolled in the study. Seventy-four eyes underwent PRK and 410 eyes underwent LASIK. The LASIK and PRK subgroups were similar in terms of the general demographics, preoperative higher-order aberrations, and manifest spherical equivalent. The changes in spherical aberration were significantly correlated with the attempted correction in both LASIK (y = –0.35x and R2 = 0.42 for myopic WFG; y = –0.18x and R2 = 0.19 for myopic RA; y = –0.44x and R2 = 0.49 for hyperopic WFG; y = –0.53x and R2 = 0.69 for hyperopic RA) and PRK (y = –0.20x and R2 = 0.25 for myopic WFG; y = –0.37x and R2 = 0.44 for myopic RA). No other preoperative parameters except corneal asphericity, axial length, and anterior chamber depth were significantly correlated with the changes in the spherical aberration.
Conclusions
LASIK correction had a higher induction of spherical aberration compared with that of PRK, and the beneficial effect of the WFG treatment on spherical aberration was mainly visible in the PRK-treated eyes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Studies directly comparing high-order aberrations between surface ablation and LASIK are mostly inconclusive, and a vast majority have been conducted using mechanical microkeratomes. In the present study, flap creation was femtosecond laser-assisted. |
The creation of a flap in the cornea weakens the lamellar micro-structure; therefore, more spherical aberrations are expected in LASIK rather than in photorefractive keratectomy (PRK). In fact, LASIK correction had a higher induction of spherical aberration compared with that of PRK. |
If there is a clear correlation between spherical aberration changes and attempted correction in LASIK and PRK, the induction of spherical aberration is poorly predictable. |
Introduction
Photorefractive keratectomy (PRK) and laser-assisted in situ keratomileusis (LASIK) have been widely used to correct refractive errors for more than 20 years; however, they induce higher-order aberrations (HOAs), potentially leading to the deterioration of vision quality. Long-term studies are relatively few and mostly focused on the refractive outcomes [1, 2], while studies directly comparing HOAs between surface ablation and LASIK are mostly inconclusive and a vast majority have been conducted using mechanical microkeratomes [1,2,3,4].
The configuration of the corneal stroma in the lamellae plays a pivotal role in the biomechanical behavior after laser vision correction and, ultimately, in the induction of spherical aberrations. Indeed, beyond the theory of fluence correction at the corneal periphery (so-called cosine effect) [5], Reinstein et al. demonstrated stromal thickening at the periphery of a myopic ablation [6], leading to spherical aberrations. This phenomenon was adequately described by Cynthia Roberts, postulating that the cornea should be considered as a series of stacked rubber bands (lamellae) with sponges between the layers (interlamellar spaces filled with extracellular matrix), rather than a piece of plastic [7].
To address the induction and reduce the level of some preexisting HOAs, wavefront-guided (WFG) treatments have been made available [8, 9], but concerns regarding their greater efficacy in the control of aberrations remain. In the present study, we retrospectively analyzed the long-term changes in corneal spherical aberrations in patients who underwent LASIK or PRK with regular or WFG ablations.
Methods
This study was conducted at the Centro Oculistico Bresciano (Brescia, Italy) in accordance with the ethical principles of the Declaration of Helsinki and was approved by the local ethics committee (Spedali Civili di Brescia), as well as by the Institutional Review Board. A retrospective analysis was conducted on several thousand eyes treated for myopia and hyperopia of spherical equivalent ranging from –11.125 to 5.75 D, between January 2016 and December 2018. Patients not targeted for emmetropia and with a history of an ocular disease, previous corneal or intraocular surgery, wound healing disorders, and connective tissue diseases were excluded from the study. Written informed consent was obtained from all participants at the time of the intervention.
Eyes with a scotopic pupil diameter greater than 6.5 mm were selected to undergo WFG ablation and were scanned with ocular aberrometry (iDesign; Johnson & Johnson Surgical Vision; Santa Ana, CA, USA) to obtain the customized WFG pattern.
Preoperative and postoperative scans were obtained with the same Pentacam-AXL system (Oculus Optikgeräte Inc, Wetzlar, Germany), and all the parameters obtained from the Pentacam examinations, including the axial length, were automatically exported into .csv files for analysis using the Call-All function for data export. Spherical aberration was measured at a 6 mm diameter.
Inclusion Criteria and Surgical Procedure
All procedures were performed by the same surgeon (AR) using the VISX STAR S4 IR excimer laser platform (Johnson & Johnson Surgical Vision, Santa Ana, CA, USA), and the treatment goal for all surgeries was emmetropia. Selection of eyes for analysis were based on the following criteria: (1) no previous corneal surgery, (2) Pentacam-AXL scan at the 24-month follow-up, (3) an optical zone of 6.5 mm, (4) a fifth-generation IntraLase FS Laser (150 kHz; Johnson & Johnson Surgical Vision; Santa Ana, CA, USA) used to create flaps in the LASIK-treated eyes; (5) flap diameter of 9.0 mm and intended flap thickness of 100 µm.
A raster pattern was used with the hinge located in the superior position, with an energy of 0.8 µJ/spot and a spot-line separation of 6 × 6 µm. The hinge and side-cut angles were set at 48° and 70°, respectively. The pocket software was enabled to decrease the occurrence of dense bubbles at the interface. In the PRK-treated eyes, the epithelium was mechanically removed using a spatula up to a diameter of 8 mm, and laser ablation was subsequently performed. Thereafter, a cellulose sponge loaded with 0.02% mitomycin C solution was placed on the ablated corneal tissue for 20 s, followed by copious irrigation with a chilled and balanced salt solution. A soft bandage contact lens was applied until complete epithelialization was achieved. Postoperative medication for both LASIK and PRK included topical moxifloxacin 0.5% (Vigamox; Alcon Laboratories Inc., Ft. Worth, TX, USA) four times a day for 5 days; additionally, a combination of netilmicin and dexamethasone eye drops (Netildex; Sifi Spa, Aci Sant'Antonio, Italy) was administered four times a day for 2 weeks.
Statistical Analyses
All data were normally distributed according to the Shapiro–Wilk test (P > 0.05). A Pearson correlation test was run to find any possible relationship between spherical aberration change and all the pre- and post-operative parameters. To visually compare the changes and correlations between different types of variables (aberrations and spherical equivalent in groups with different metrics and variances), all sample variables were standardized. Standardization did not alter the original correlation index between the variables. Comparisons between the groups were performed with a two-tailed, unpaired t-test. All statistical analyses were performed using Microsoft Excel 365 (Microsoft Corporation, Redmond, WA, USA) and RStudio (RStudio PBC, Boston, MA, USA), and a P value < 0.05 was considered statistically significant. Results are reported as mean ± standard deviation.
Results
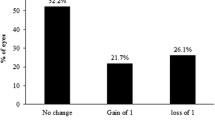
Of the 3826 eyes that were reviewed, a total of 484 eyes met the inclusion criteria and were enrolled for the study (Fig. 1). Specifically, 74 and 410 eyes underwent PRK and LASIK, respectively. Baseline characteristics are shown in Table 1. No significant differences were present between the subgroups.
LASIK Myopic Eyes: WFG Ablation Versus Regular Ablation
Both groups demonstrated a linearly increasing trend for spherical aberration (Table 2 and Fig. 2). The changes in spherical aberration were significantly correlated with the preoperative spherical equivalent for both WFG (Pearson’s r = –0.64; P < 0.001) and regular (Pearson’s r = –0.48; P < 0.001) ablations. The slope of the correlation was higher for WFG treatment, although no significant difference was noted in the spherical aberration changes between the two groups (P = 0.92).
PRK Myopic Eyes: WFG Ablation Versus Regular Ablation
An increase in spherical aberration with a linear trend, was observed for both groups (Table 2 and Fig. 3). The changes in spherical aberration were significantly correlated with the preoperative spherical equivalent for both WFG (Pearson’s r = –0.30; P = 0.02) and regular (Pearson’s r = –0.67; P < 0.001) ablation groups. The slope of the correlation was higher for regular ablation than for WFG ablation (y = 0.369x with R2 = 0.44 and y = 205x with R2 = 0.25, respectively), and a significant difference was observed in the spherical aberration changes between the two groups (P = 0.008).
LASIK vs. PRK in Myopic Eyes
Considering both WFG and regular ablation subgroups, an increase in spherical aberration was observed for both LASIK and PRK groups, with a polynomial trend (second-order; Table 2 and Fig. 4), with no statistical difference between them (P = 0.16). The WFG subgroup, however, showed a greater increase in spherical aberration for LASIK (Pearson’s r = –0.64; P < 0.001) patients compared to PRK (Pearson’s r = –0.3; P = 0.02; Fig. 5).
LASIK Hyperopic Eyes: WFG Ablation Versus Regular Ablation
Both the WFG and regular ablation groups showed a significant reduction in spherical aberration, with a linear trend (Table 2 and Fig. 6). The changes in spherical aberration were significantly correlated with the preoperative spherical equivalent for both WFG (Pearson’s r = –0.7; P < 0.001) and regular ablation (Pearson’s r = –0.83; P < 0.001). No significant difference was observed in the spherical aberration changes between the two groups (P = 0.92).
Correlation Between Spherical Aberration and Other Parameters
Among all the parameters computed using the Pentacam, the only preoperative variables significantly correlating with the spherical aberration change were, obviously, axial length and anterior chamber depth. No other pre- or postoperative variable had a significant correlation with the spherical aberration change, including age or corneal morphological parameters such as central corneal thickness and corneal diameter (Table 3).
Discussion
The present study demonstrates the correlations between spherical aberration changes and attempted correction in LASIK and PRK procedures for myopia and hyperopia, with regular and WFG ablations. The occurrence of HOAs following laser vision correction for refractive errors has been reported in many studies. Typically, myopic ablations induce positive spherical aberration (each diopter of myopic correction induces approximately 0.1 µm of spherical aberration) and hyperopic treatments mainly induce negative spherical aberration [10].
The laser–tissue interaction is a complex phenomenon, as the cornea is not like a piece of plastic; it is inherently aspheric and is covered by the epithelium with its remodeling laws. Modern wavefront-optimized ablation profiles pre-compensate for spherical aberration by removing more stromal tissue at the periphery to preserve the prolate shape of the cornea, while WFG treatments are, theoretically, designed to measure and treat both lower-order aberrations and HOAs. A clear reduction in tissue ablation of 10–15% in the corneal periphery was demonstrated by Mrochen and Seiler, even with a 6.5-mm optical zone [5]. This occurs because the laser beam interfaces the periphery of the optical zone at an oblique angle, thereby resulting in a larger area exposed to light with higher reflectance, lowering the beam radiant exposure (fluence) below the ablation threshold. However, other notable phenomena occur with photoablation. The cornea undergoes considerable biomechanical changes following laser surgery, as demonstrated by Reinstein et al. [6]. Myopic ablation removes central stromal tissue and releases tension, resulting in retraction from the center of the cornea, associated with central thinning and peripheral thickening of the stromal layers [6]. Furthermore, abrupt discontinuity of the stromal shape at the ablation edge promotes remodeling of the epithelium that extends into the optical zone. These phenomena diminish the size of the optical zone and increase spherical aberration.
The LASIK procedure itself, just by the creation of flap, is responsible for corneal weakening and induction of HOAs. Marshall et al. [11] demonstrated a corneal weakening related to the depth of the flap cut, with strain increasing by 9% and 32% at 90 µm and 160 µm, respectively. Similar changes, 9% and 33%, were observed following the execution of side cuts alone at the same depths. Contrastingly, strain increase following delamination alone revealed no relationship with depth, increasing by merely 5%. Additionally, the location of the flap hinge with the healing processes along the edges of the flap has been reported to play a role in inducing comatic aberrations [12, 13]. Moreno-Barriuso et al. [14] suggested that most spherical aberration induced by LASIK is due to laser ablation and not the microkeratome cut. However, the amount of spherical aberration has been reported to increase with the level of attempted refractive correction [15]. This has been well-demonstrated in our study, with a linear or polynomial (second-order) trend in both myopic and hyperopic corrections. Particularly, for myopic corrections, the polynomial trend observed in patients who underwent LASIK and PRK treatments was similar when considered collectively (y = 0.037x2 with R2 = 0.30 and y = 0.03x2 with R2 = 0.33, respectively), while considering only the WFG subgroup, the correlation slope was higher for LASIK than for PRK (y = –0.347x with R2 = 0.42 and y = –0.205x with R2 = 0.24, respectively). This difference can be explained by the reduced increase in HOAs in WFG ablation [10, 16], thereby cleaning at least part of the ablation-related HOAs and ultimately showing predominantly the spherical aberrations coming from the flap creation, although a thin flap of 100 µm was cut.
As the creation of the LASIK flap itself increases the induction of HOAs, some surgeons support the idea that customized ablation is best performed using surface ablation [10, 14]. This is consistent with the results of the present study, as the beneficial effect of the WFG ablation over regular ablation was only visible in PRK-treated eyes (y = –0.369x with R2 = 0.44 and y = 0.205x with R2 = 0.25, respectively). This is another indirect confirmation of the large amount of spherical aberration induced by flap creation, as the beneficial effect of WFG diminishes when considering that of LASIK-treated eyes. The efficacy of WFG iDesign treatments with surface ablation for irregular and ectatic corneas was previously reported by our group [8] in accordance with the results of a similar study by Shaheen et al. [17].
Although all analyzed subgroups demonstrated a significant correlation between attempted correction and spherical aberration change, a low predictability (relatively low R2 value) was observed for all the correlations. This variance is probably explained by the numerous aforementioned factors leading to an increase in spherical aberration, making the projection of the postoperative aberration difficult compared to the extremely high predictability of the refractive treatments. No other preoperative parameters correlated significantly with the changes in the spherical aberration. Further studies are required to better understand the underlying factors influencing spherical aberration changes, particularly to target the sweet spot of ± 0.6 µm required by newer presbyopia-correcting algorithms [18,19,20].
Our study has a few limitations. First, the sample size, although quite large, of the eyes in the PRK subgroups was relatively small; second, the instrument utilized for scanning—the Pentacam HR—had limited repeatability for assessing HOAs, being a Scheimpflug camera.
Conclusion
The attempted correction with both LASIK and PRK significantly correlated with the change in spherical aberration in both the WFG and regular ablation subgroups. LASIK correction was responsible for higher induction of spherical aberration compared with PRK, and the beneficial effect of WFG treatment on spherical aberration was only visible in the PRK-treated eyes. No other preoperative parameter significantly correlated with the change in spherical aberration.
References
Jahadi Hosseini SHR, Abtahi SMB, Khalili MR. Comparison of higher order aberrations after wavefront-guided LASIK and PRK: one year follow-up results. J Ophthalmic Vis Res. 2016;11(4):350–7.
Ivarsen A, Hjortdal J. Seven-year changes in corneal power and aberrations after PRK or LASIK. Invest Ophthalmol Vis Sci. 2012;53(10):6011–6.
Slade SG, Durrie DS, Binder PS. A prospective, contralateral eye study comparing thin-flap LASIK (sub-Bowman keratomileusis) with photorefractive keratectomy. Ophthalmology. 2009;116(6):1075–82.
Randleman JB, Perez-Straziota CE, Hu MH, White AJ, Loft ES, Stulting RD. Higher-order aberrations after wavefront-optimized photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2009;35(2):260–4.
Mrochen M, Seiler T. Influence of corneal curvature on calculation of ablation patterns used in photorefractive laser surgery. J Refract Surg. 2001;17(5):S584-587.
Reinstein DZ, Silverman RH, Raevsky T, Simoni GJ, Lloyd HO, Najafi DJ, et al. Arc-scanning very high-frequency digital ultrasound for 3D pachymetric mapping of the corneal epithelium and stroma in laser in situ keratomileusis. J Refract Surg. 2000;16(4):414–30.
Roberts C. The cornea is not a piece of plastic. J Refract Surg. 2000;16(4):407–13.
Russo A, Faria-Correia F, Rechichi M, Festa G, Morescalchi F, Semeraro F. Topography/wavefront-guided photorefractive keratectomy combined with crosslinking for the treatment of keratoconus: preliminary results. J Cataract Refract Surg. 2021;47(1):11–7.
Moussa S, Dexl AK, Krall EM, Arlt EM, Grabner G, Ruckhofer J. Visual, aberrometric, photic phenomena, and patient satisfaction after myopic wavefront-guided LASIK using a high-resolution aberrometer [Internet]. vol. 10, Clinical Ophthalmology. Dove Press; 2016. pp. 2489–96. https://www.dovepress.com/visual-aberrometric-photic-phenomena-and-patient-satisfaction-after-my-peer-reviewed-fulltext-article-OPTH. Accessed 5 Dec 2020.
Customized Laser Vision Correction | Mazen M. Sinjab | Springer [Internet]. https://www.springer.com/gp/book/9783319722627. Accessed 2 Jan 2021.
Knox Cartwright NE, Tyrer JR, Jaycock PD, Marshall J. Effects of variation in depth and side cut angulations in LASIK and thin-flap LASIK using a femtosecond laser: a biomechanical study. J Refract Surg. 2012;28(6):419–25.
Ig P, Gd K, Si P, Cs S, Ma T, Ai P. Induced optical aberrations following formation of a laser in situ keratomileusis flap. J Cataract Refract Surg. 2002;28(10):1737–41.
Porter J, MacRae S, Yoon G, Roberts C, Cox IG, Williams DR. Separate effects of the microkeratome incision and laser ablation on the eye’s wave aberration. Am J Ophthalmol. 2003;136(2):327–37.
Moreno-Barriuso E, Lloves JM, Marcos S, Navarro R, Llorente L, Barbero S. Ocular aberrations before and after myopic corneal refractive surgery: LASIK-induced changes measured with laser ray tracing. Invest Ophthalmol Vis Sci. 2001;42(6):1396–403.
Martínez CE. Effect of pupillary dilation on corneal optical aberrations after photorefractive keratectomy. Arch Ophthalmol. 1998;116(8):1053.
Schallhorn SC, Farjo AA, Huang D, Boxer Wachler BS, Trattler WB, Tanzer DJ, et al. Wavefront-guided LASIK for the correction of primary myopia and astigmatism a report by the American Academy of Ophthalmology. Ophthalmology. 2008;115(7):1249–61.
Shaheen MS, Shalaby Bardan A, Piñero DP, Ezzeldin H, El-Kateb M, Helaly H, et al. Wave front-guided photorefractive keratectomy using a high-resolution aberrometer after corneal collagen cross-linking in keratoconus. Cornea. 2016;35(7):946–53.
Rocha KM, Vabre L, Chateau N, Krueger RR. Expanding depth of focus by modifying higher-order aberrations induced by an adaptive optics visual simulator. J Cataract Refract Surg. 2009;35(11):1885–92.
Reinstein DZ, Archer TJ, Gobbe M. LASIK for myopic astigmatism and presbyopia using non-linear aspheric micro-monovision with the carl zeiss meditec MEL 80 platform. J Refract Surg. 2011;27(1):23–37.
Ganesh S, Brar S, Gautam M, Sriprakash K. Visual and refractive outcomes following laser blended vision using non-linear aspheric micro-monovision. J Refract Surg. 2020;36(5):300–7.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article. The journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Andrea Russo: study concept, design and main surgeon; Ottavia Filini: statistics and data analysis; Chiara Salvalai: drafting and reviewing the manuscript; Alessandro Boldini: data entry and drafting the manuscript; Giulia Festa: drafting the manuscript; Luisa Delcassi: study design; Francesco Morescalchi and Francesco Semeraro: reviewing the manuscript.
Disclosures
Andrea Russo, Ottavia Filini, Chiara Salvalai, Alessandro Boldini, Giulia Festa, Luisa Delcassi, Francesco Morescalchi, and Francesco Semeraro have nothing to disclose.
Compliance with Ethics Guidelines
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and was approved by the local Ethics Committee (Spedali Civili di Brescia) as well as by the Institutional Review Board.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Russo, A., Filini, O., Salvalai, C. et al. Two-Year Changes in Corneal Spherical Aberration After Laser-Assisted In Situ Keratomileusis and Photorefractive Keratectomy in Regular and Wavefront-Guided Ablations. Ophthalmol Ther 10, 1003–1014 (2021). https://doi.org/10.1007/s40123-021-00392-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-021-00392-9