Abstract
Introduction
The purpose of this non-comparative, prospective, observational study was to evaluate the post-US Food and Drug Administration approval outcomes of epithelium-off, full-fluence, Dresden protocol corneal collagen crosslinking (CXL) for the treatment of progressive keratoconus (KCN) and post-refractive corneal ectasia at a US academic tertiary medical center.
Methods
This study involved 125 eyes of 97 patients with KCN and 13 eyes of 12 patients with post-refractive ectasia which underwent CXL between November 2016 and September 2019. Best spectacle-corrected visual acuity (BSCVA) and corneal topographic parameters were measured preoperatively, at postoperative month 1 (POM-1), and between postoperative months 3 and 24 (POM 3–24).
Results
Best spectacle-corrected visual acuity, flat keratometry, steep keratometry, and mean corneal power worsened at POM-1 (p < 0.01) with a return to preoperative values at POM 3–24. Maximum keratometry (Kmax) steepened at POM-1 and then improved beyond preoperative levels at POM 3–24 (p < 0.01 and p = 0.03, respectively). Pachymetry at the apex and pupil decreased at POM-1 and POM 3–24 (p = 0.03). Pachymetry at the thinnest point decreased at POM-1 and trended toward reduction at POM 3–24 (p < 0.001 and p = 0.06, respectively). Visual and tomographic outcomes were similar between pediatric and adult populations, and between KCN and post-refractive ectasia patients.
Conclusions
Real-world results of CXL in the USA are similar to those reported in prior studies, demonstrating an initial worsening of BSCVA, pachymetry, and keratometry followed by corneal flattening and preservation of visual acuity. Improvements in Kmax and stability in visual acuity were observed over 24 months in children and adults with progressive KCN or post-refractive ectasia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Multiple randomized control trials have confirmed the efficacy of corneal crosslinking for the treatment of progressive keratoconus and post-refractive corneal ectasia. |
Limited studies exist on the effects of corneal crosslinking on the anterior chamber and posterior cornea. Stability in the anterior chamber and a decrease in corneal volume have been observed. |
This study sought to evaluate the post-US Food and Drug Administration approval efficacy of corneal crosslinking at a US academic tertiary medical center for adults and children, with a particular focus on elucidating the effects on the anterior chamber and posterior cornea. |
What was learned from the study? |
In a US academic tertiary medical center, corneal crosslinking led to flattening of maximum keratometry and stability in visual acuity for 24 months in adult and pediatric patients with progressive keratoconus and post-refractive corneal ectasia. |
A decrease in chamber volume was observed after corneal crosslinking, which may occur by a mechanism that is not fully explained by a change in posterior or anterior corneal curvature alone. |
Digital Features
This article is published with digital features to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12962696.
Introduction
Keratoconus (KCN) is a corneal disorder that causes progressive thinning and ectasia, resulting in deterioration of visual acuity from irregular astigmatism [1]. This disease often begins in young adulthood, leading to visual changes that have a great impact on the individual’s quality of life. Similarly, post-refractive ectasia is an iatrogenic complication of refractive surgery which results in a significant refractive error due to progressive stromal thinning and steepening of the cornea [2]. Refractive error and high degrees of irregular astigmatism in these patients are often treated with the use of rigid gas permeable or scleral contact lenses or, in some cases, by intracorneal ring segment implants or conductive keratoplasty; however, these treatments do not correct the underlying ectasia and are unable to halt the progression of the disease [3,4,5]. Left untreated, rapid progression occurs in about 20% of cases [6]. Until the early 2000s, there was no effective treatment to alter the progression of KCN or post-refractive corneal ectasia, eventually requiring patients with advanced, progressive disease to pursue surgery, such as penetrating or deep anterior lamellar keratoplasty, to restore vision. Corneal collagen crosslinking (CXL), developed in Europe by researchers at the University of Dresden in the late 1990s, utilizes ultraviolet light following the application of photosensitizing riboflavin drops to increase the biomechanical strength of the cornea [7]. CXL has the ability to stop the progression in KCN and post-refractive ectasia.
Since approval for use as a treatment for KCN in Europe in 2003, multiple studies have confirmed the efficacy of CXL in reducing keratometry values for at least 1 year, with minimal complications [8]. Additionally, this method has been found to increase corneal stability and halt progression in eyes with post-refractive corneal ectasia [9]. In 2010, a pre-approval prospective, randomized, controlled trial (RCT) in the USA found improvements in visual acuity, maximum keratometry, and average keratometry 1 year after epithelium-off (epi-off) CXL for the treatment of KCN and post-refractive corneal ectasia [10]. A 2014 RCT performed in Australia found similar results, with sustained improvements for 36 months in maximum keratometry (Kmax) and visual acuity after epi-off CXL [11]. In April of 2016, the US Food and Drug Administration (FDA) approved CXL for the treatment of KCN and post-refractive corneal ectasia, increasing the scope of treatment options for patients in the USA. Pending FDA approval, Hersh and associates performed a prospective, randomized, multicenter controlled clinical trial in the USA and reported that CXL treatment resulted in decreases in maximum keratometry and improvements in visual acuity 1 year after treatment, with minimal adverse findings [12].
Despite the strength of evidence produced in the US clinical trials described above, no follow-up data were published on the post-FDA approval outcomes of epi-off, full-fluence, Dresden protocol CXL in the USA for the treatment of progressive KCN and post-refractive corneal ectasia. Therefore, we performed a prospective, non-comparative cohort study to evaluate the outcomes and variables that may affect the results of CXL at a US academic tertiary medical center. As the procedure has been deemed safe and effective in children, we sought to include pediatric patients in the study to elucidate any differences in outcomes between adult and pediatric populations.
Methods
Approval for this prospective observational study was obtained from the Institutional Review Board at Johns Hopkins University, and the study was conducted in accordance with HIPPA rules (https://www.hhs.gov/hipaa/for-professionals/privacy/index.html). This research adheres to the tenets of the Helsinki Declaration of 1964, and its later amendments. All patients gave informed consent to participate in this study. A patient registry was compiled consisting of a cohort of 125 eyes in 97 consecutive patients with progressive KCN between the ages of 12 and 65 years (mean 24.8, standard deviation [SD]) 8.3 years) that underwent epithelium-off, Dresden protocol CXL between November 2016 and September 2019 at the Wilmer Eye Institute. Additionally, 13 eyes in 12 consecutive patients with post-refractive corneal ectasia between the ages of 18 and 65 years (mean 46.6, SD 11.5 years) were included.
Inclusion criteria comprised progressive disease, defined by the presence of the following: best spectacle-corrected visual acuity (BSCVA) of 20/25 or worse and an increase in Kmax or steep keratometry (K2) based on Pentacam parameters (OCULUS, Arlington, WA, USA) of ≥ 1.0 diopter (D) over ≤ 12 months. Specifically, for patients aged > 25 years, CXL was offered when there was evidence of accelerated progression in a 3–4 month period, as determined by an increase in Pentacam parameters of approximately ≥ 0.4 D for K2 or Kmax, or evidence of increased disease activity around the cone. Patients aged < 25 years with a new diagnosis of KCN were also included in this study; this group of patients was offered CXL immediately if initial Pentacam tomography showed evidence of KCN and BSCVA was 20/25 or worse, due to the higher risk of rapid progression in younger individuals [13].
Exclusion criteria included surgical contraindications, such as corneal thickness < 375 μm at the thinnest point based on Pentacam measurements (except for one case of contact lens-assisted CXL), prior herpetic keratitis, severe full-thickness corneal scarring or opacification, active autoimmune disorders, pregnancy/nursing females, concurrent corneal infection, a history of poor epithelial wound healing, and severe ocular surface disease. Two eyes with intracorneal ring segment implants were excluded from this analysis. Six eyes that received prior CXL at an outside hospital were excluded from this study as well. Overall, this study included only treatment-naïve eyes.
Each study participant’s medical record was reviewed, and the following data were collected: demographic information, pre- and postoperative BSCVA, manifest refraction, and corneal topographic parameters based on Pentacam measurements. The corneal topographic data obtained included flat keratometry (K1), K2, mean keratometry (Km), front Kmax, pachymetry at the apex and thinnest point, astigmatism over the pupillary center, and anterior chamber and corneal volume. Modifying factors were also recorded; these included the presence of atopic disease, duration of disease from diagnosis, family history of KCN or myopia/astigmatism, patient-reported eye rubbing, patient-reported contact lens use, and clinical findings such apical scarring, Vogt striae, and an observed cone. Additionally, the presence of postoperative haze and postoperative complications on slit-lamp biomicroscopy was recorded at all postoperative visits. Snellen visual acuity was converted to logarithm of the minimum angle of resolution (logMAR) equivalents for statistical analysis. Visual acuity of a hand motion was set at 2.3 logMAR and counting fingers at 1.85 logMAR [14, 15].
Surgical Technique
All procedures were performed while strictly adhering to the FDA-approved Dresden protocol using the KXL system with Photrexa® Viscous (riboflavin 5′- phosphate in 20% dextran ophthalmic solution), and when necessary, Photrexa (hypotonic riboflavin 5′- phosphate ophthalmic solution) (both Avedro Inc., Waltham, MA, USA) [12]. At the time of publication of this article, the Avedro KXL system with Photrexa riboflavin solution is the first and only FDA-approved system for CXL in the USA.
Briefly, the CXL procedure began with topical anesthesia, followed by debridement of the central 9-mm corneal epithelium with 20% alcohol. Then, one drop of Photrexa Viscous was instilled topically every 2 min for 30 min. Additional Photrexa Viscous was instilled until the presence of yellow flare was noted in the anterior chamber and corneal thickness was found to be at least 400 μm by ultrasound pachymetry. If a corneal thickness of 400 μm was not achieved, two drops of Photrexa were instilled every 5–10 s until the corneal thickness increased to at least 400 μm. The eye was then irradiated for 30 min at 3 mW/cm2 at a wavelength of 365 nm, centered over the cornea, sparing the limbus and ocular adnexa, using the KXL system. While irradiating the eye, topical instillation of Photrexa Viscous continued every 2 min for the full 30 min. A bandage contact lens was applied to the eye immediately after the procedure and removed approximately 1 week later. Topical antibiotics were provided for 1 week after the procedure and topical steroids for 1 month. One case of contact lens-assisted CXL was performed on an eye with post-refractive ectasia due to corneal thickness of < 340 μm following administration of both Photrexa and Photrexa Viscous [16].
Statistical Analysis
Three time points were included for data analysis: a preoperative visit; a 1-month postoperative visit (POM-1); and a last documented visit that occurred between 3 and 24 months postoperatively (POM 3–24). A period of 3–24 months was chosen to represent a patient’s last postoperative evaluation as the majority of changes in keratometry and visual acuity have been observed to occur within the first 3 months following treatment [12, 17]. Additionally, the presence of the most frequently reported adverse effect, stromal haze, has been shown to peak within the first postoperative month and plateau between 1 and 3 months [18]. A period of 3–24 months also allowed for a larger sample size at the follow-up visits through compensation for any irregular follow-up visits postoperatively. Thus, we sought to have an endpoint that is representative of the known clinical time course of CXL outcomes.
Linear mixed-effects models with robust standard error estimates were used to compare variables (BSCVA, keratometry, and pachymetry) between these three time points. The linear mixed-effects models used indicator variables for visits and included a random intercept for patients to account for the correlation among measures from bilateral CXL patients, as well as a random intercept for eyes to account for the correlation among the measures from the same eye. Subgroup analysis was conducted comparing eyes that received Photrexa Viscous only to those that received Photrexa and Photrexa Viscous. This analysis controlled for the baseline pachymetry at the thinnest point to ensure that group differences in outcomes were not caused by differences in baseline thinnest pachymetry. Additionally, patients aged ≤ 18 years at the first visit (pediatric patients) were compared to those aged > 18 (adult patients) at first visit. Eyes with post-refractive ectasia were compared to those with progressive KCN and no history of refractive surgery treatment. Lastly, eyes that had improvements in visual acuity (improvement in BSCVA by two lines or more from preoperative measurements) at the various postoperative periods were compared to those that did not have improvements in BSCVA following CXL. For the subgroup analyses, interaction terms between visits and the group indicator variables were used as predictors in the mixed-effects models.
For comparing the baseline characteristics in the subgroup analyses, two-sample t tests were used to compare continuous variables. Fisher’s exact test or Pearson’s chi-squared tests were used to compare categorical characteristics. Wilcoxon rank-sum tests were used to compare differences in the duration of disease from initial diagnosis in the various subgroups. Pearson’s correlation coefficient was used to determine if there was a correlation between preoperative pachymetry at the thinnest point and pachymetry at the end of viscous CXL treatment.
To analyze the resolution of postoperative stromal haze, mixed-effects logistic regressions were performed with a random intercept for patients and a random intercept for eyes. Stomal haze at POM-1 was used as a reference, and comparisons were made to the last postoperative visit (POM 3–24) for all eyes and the various subgroups. Eyes with KCN and ≥ 1 year of follow-up were assessed for changes in cornea volume, chamber volume, or anterior chamber depth (ACD) at their last visit relative to preoperative measurements. Linear regression models were adjusted for the preoperative measurements in order to be able to examine the association between the observed changes and other preoperative tomographic variables. A p value < 0.05 was considered to be statistically significant. All analyses were performed using STATA statistical software (v16.0) (StataCorp LLC, College Station, TX, USA) [19].
Results
This study included 138 eyes. Preoperative data were collected in 137 eyes, and data at POM-1 and at POM 3–24 were collected in 96 and 114 eyes, respectively, for a total of 350 visits in this study. Seventy-seven visits were reported at POM-3, 54 visits at POM-6, 40 visits at POM-12, 16 at POM-18, and six at POM-24 (collectively POM 3–24). Patient and eye characteristics are described in Tables 1 and 2, respectively. Metrics describing the severity of disease presentation in all eyes are given in Table 3. Overall, this study encompassed patients with mild to severe, progressive, KCN or post-refractive ectasia. No differences in initial disease severity were observed between patients with progressive KCN and those with post-refractive ectasia or between adult and pediatric patients (Table 4).
Overall CXL Outcomes
Best spectacle-corrected visual acuity, measured in logMAR, worsened in all treated eyes at POM-1 in comparison to preoperative values (p = 0.007; Table 5), but this decrease was followed by a return to preoperative vision levels by the last recorded visit (p = 0.55). An increase from preoperative K1, K2, and Km was observed at POM-1 (p < 0.001), with a return to values similar to those recorded at baseline at the last recorded visit. Additionally, Kmax showed an increase from preoperative values at POM-1 (p < 0.001), but subsequently fell to values lower than those at baseline at the last recorded visit (p = 0.03). Pachymetry at the pupil and apex decreased from preoperative values at both POM-1 and the last recorded visit (p < 0.001 and p = 0.02, and p < 0.001 and p = 0.006, respectively). Pachymetry at the thinnest point was reduced at POM-1 compared to preoperative thickness and showed a trend toward reduction from preoperative thickness by the last visit (p < 0.001 and p = 0.06, respectively). A reduction in chamber volume was also observed in the POM 3- to 24-month period (p < 0.001).
Differences Between Progressive KCN and Post-Refractive Ectasia
Patients with post-refractive ectasia were on average older than those with KCN (p < 0.001); however, this was primarily due to the minimum age of eligibility for laser refractive surgery and the longer interval between the surgery and development of ectasia. Patients with KCN were more likely to have a history of eye rubbing than those with post-refractive ectasia (p = 0.035). Patients with post-refractive ectasia were found to have a longer duration of disease from initial diagnosis, as expected, when compared to patients with progressive KCN (p = 0.03). KCN patients more commonly reported the use of rigid gas permeable and soft contact lenses than those with post-refractive ectasia (p = 0.04). Patients with KCN were more likely to have apical scarring and Fleischer rings at initial presentation compared to patients with post-refractive ectasia (p = 0.04 and 0.04, respectively).
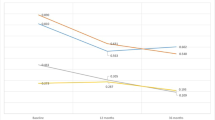
There were no differences in preoperative BSCVA between KCN eyes and eyes with post-refractive ectasia, nor were there differences in the change from baseline at any time point between these two groups (see Table 6; Fig. 1a). Compared to preoperative values, at POM-1 eyes with KCN had a greater increase in K2 and Kmax than eyes with post-refractive ectasia (p = 0.03 and p = 0.02, respectively). However, there was no difference between the two groups in terms of the change in K2 and Kmax from the preoperative visit to the last visit (see Table 6; Fig. 1b, c). Compared to eyes with KCN, eyes with post-refractive ectasia had a significantly lower preoperative chamber volume (p = 0.03) and a greater decrease in spherical equivalence at POM-1 (p = 0.02). No other significant differences were observed between these two groups.
Comparisons between adult eyes (patient aged > 18 years), pediatric eyes (patient aged ≤ 18 years), all eyes with progressive keratoconus, and all eyes with post-refractive ectasia for best spectacle-corrected visual acuity in logMAR equivalents (a) steep keratometry (K2) (b), maximum keratometry (Kmax) (c), and pachymetry at the thinnest point (d). Error bars correspond to the standard error for each value
Differences in Pediatric Patients
As expected, adult patients were found to have a longer median duration of disease from initial diagnosis, on average, when compared to pediatric patients (mean [interquartile range]: 1.0 [0.1, 5.0] vs. 0.5 [0, 1.5] years; p = 0.032). When all eyes of pediatric patients (≤ 18 years) were compared to those of adult patients (> 18 years), the former were found to have greater preoperative astigmatism over the pupillary center (p = 0.007; Table 7). There was no difference in the amount of change from preoperative astigmatism at any postoperative time point between these two groups. Also, there were no other observed preoperative or outcome differences between age groups regarding BSCVA, K1, K2, Km, Kmax, pachymetry at the apex, pachymetry at the thinnest point, or chamber volume (see Table 7; Fig. 1a–d).
Use of Photrexa Viscous Only Versus Photrexa and Photrexa Viscous
This study was conducted on 89 eyes that required Photrexa and Photrexa Viscous treatment and on 44 eyes that required treatment with only Photrexa Viscous. There were no differences in demographic or clinical findings on biomicroscopy between eyes that required the use of both Photrexa and Photrexa Viscous and those only requiring Photrexa Viscous. No differences were observed preoperatively or postoperatively in BSCVA between these two groups. While controlling for baseline pachymetry at the thinnest point, eyes that received only Photrexa Viscous had a higher preoperative K1, K2, Km, and Kmax than eyes that were treated with both Photrexa Viscous and Photrexa (p = 0.019, 0.018, 0.017, and 0.014, respectively). Eyes treated with both Photrexa Viscous and Photrexa had a greater increase in astigmatism at POM-1, compared to preoperative values (p = 0.04); however, there was no difference in the change in astigmatism between the two groups by months 3–24 (p = 0.36). Eyes that received both Photrexa and Photrexa Viscous had a greater decrease in corneal volume by POM-1 (p = 0.008). When controlling for preoperative pachymetry at the thinnest point, no differences in pachymetry were observed between the two groups preoperatively or postoperatively. There was a positive correlation observed between preoperative pachymetry at the thinnest point and pachymetry at the end of viscous Photrexa treatment (Pearson’s correlation coefficient 55%, p < 0.001).
Effects of Baseline Characteristics on Postoperative Visual Acuity
Eyes with apical scarring had a statistically insignificant trend toward improvement in visual acuity at POM-1 and were more likely to have improved at the last postoperative visit (p = 0.051 and 0.006, respectively).
Stromal Haze and Postoperative Complications
Haze formation was a common postoperative occurrence. At POM-1, we observed haze in 88 of 126 eyes (69.8%), and by the last postoperative visit (POM 3–24), 55 of 116 eyes (47.4%) had residual haze. Compared to POM-1, the occurrence of stromal haze was less likely at the last visit between months 3 and 24 (odds ratio [OR] 0.232, 95% confidence interval [CI] 0.117, 0.461). When adjusting for baseline characteristics (K2, Kmax, pachymetry at the thinnest point), the occurrence of haze remained less likely at POM 3–24 (OR 0.237, 95% CI 0.119, 0.472). However, the ORs did not change with individual adjustments for baseline characteristics K2, Kmax, or pachymetry at the thinnest point (p = 0.59, 0.43, and 0.36, respectively). The ORs of persistent corneal haze were similar between adult and pediatric eyes, between eyes with KCN and those with post-refractive ectasia, and between eyes receiving only Photrexa viscous and those requiring both Photrexa and Photrexa viscous (p = 0.71, 0.16, and 0.74, respectively).
Postoperative complications were rare but included one case of delayed epithelial healing, four cases of hypertrophied epithelium that required localized epithelial debridement, two cases of sterile infiltrates, and two cases of transient corneal edema. Complications did not lead to increased morbidity, and all patients recovered with stable outcomes at the end of follow-up.
Anterior Chamber Changes
The following postoperative comparisons involved 47 eyes with KCN and at least 1 year of follow up. For every 1-µm increase in preoperative pachymetry at the pupil, the difference between preoperative and postoperative corneal volume increased by 0.02 mm3 (r = 0.02, p = 0.005). A difference in chamber volume was associated with the preoperative corneal volume: for every cubic millimeter increase in preoperative corneal volume, the difference in chamber volume was 0.99 mm3 lower (p = 0.008).
Preoperative posterior keratometry was positively associated with the change in corneal volume: for each 1-D increase in preoperative posterior K1, the change in corneal volume increased by 3.87 mm3 (p = 0.034). Similar trends were observed for preoperative posterior K2 (1-D increase led to 3.235-mm3 increase in corneal volume; p = 0.064) and preoperative posterior Km (1-D increase led to 3.765-mm3 increase in corneal volume; p = 0.04).
Changes in the anterior chamber depth (ACD) were associated with keratometry. For each 1-D increase in preoperative K2, the anterior chamber depth increase from its pre-operative value was 0.01 mm (p = 0.041). This association was also true for pre-operative astigmatism (1-D increase led to 0.03-mm increase in ACD; p = 0.021) and for pre-operative pachymetry at the pupil (1-µm increase led to a 0.0023-mm decrease in ACD; p = 0.011), at the apex (1-µm increase led to a 0.0020-mm decrease in ACD; p = 0.008), and at the thinnest point (1-µm increase led to a 0.0018-mm decrease in ACD; p = 0.018).
Additionally, the changes in preoperative and postoperative ACD were associated with similar differences in anterior K2: a 1-mm increase in the change in ACD was associated with a 5.31-D increase in K2 (p = 0.056).
Discussion
Corneal crosslinking has proven to be a promising treatment option for patients with progressive KCN. The safety and efficiency of this treatment has been reported in a growing body of literature and demonstrated in RCTs worldwide. However, real-world data outside of the scope of these highly controlled RCTs are lacking in the USA and would be of benefit as complementary to the findings observed in these clinical trials. In the study reported here, we looked at more than 100 eyes to determine if the results observed in clinical practice with the only US FDA-approved CXL treatment system mirror the results found in the clinical trials leading to its approval.
In this study, a patient registry was compiled, consisting of data on keratometry, pachymetry, visual acuity, and complications, to assess the effects of CXL treatment in patients with progressive KCN and those with post-refractive corneal ectasia. Overall, in treated eyes, BSCVA and keratometry values (K1, K2, and Km) were observed to worsen at POM-1, when compared to preoperative values, followed by an improvement toward and stabilization around preoperative values in POM 3–24. A similar trend was observed in Kmax, with an initial worsening at POM-1, which was followed by an improvement to values below preoperative levels at the last visit. This phenomenon has been reported to be reproducible and has been confirmed in prior randomized controlled clinical trials in the USA following CXL treatment [10, 12]; it is believed to reflect the natural history of epithelial and wound healing [20]. We observed an overall decrease in pachymetry at the apex and pupil at POM-1 and POM 3–24, as well as a decrease in pachymetry at the thinnest point at POM-1 with a subsequent trend toward decreasing values by the last visit. These early changes in pachymetry may be the result of corneal epithelial remodeling that has been observed by optical coherence tomography early after CXL in eyes with KCN and corneal ectasia [21]. This early remodeling may also be a possible explanation for the observed changes in BSCVA. However, late changes in pachymetry are most likely indicative of stromal compaction after CXL.
Studies explaining the effects of CXL on anterior chamber parameters and the posterior cornea are limited; however, prior studies have shown stability in the anterior chamber and a decrease in corneal volume after CXL [22,23,24]. Based on 47 eyes, we found an overall decrease in chamber volume by the last visit and observed a decrease in corneal volume at POM-1. Our novel findings suggest that crosslinking may affect the geometry and the depth of the anterior chamber, which may affect these patients later in life when they become candidates for cataract surgery. Specifically, eyes with higher corneal volumes preoperatively tended to undergo more change in their anterior chamber volume. Flatter posterior corneas were associated with an increase in the change in anterior chamber depth. Changes in anterior depth were also associated with the change in anterior keratometry. These findings illustrate that the effects of crosslinking may not be limited only to the cornea.
Despite differences in the etiology of KCN and post-refractive ectasia, the treatment modality remains the same. As with previous studies, we found that the use of CXL resulted in similar long-term improvements in patients with progressive KCN and those with post-refractive ectasia [12, 17]. Additionally, we found a greater magnitude of postoperative change in K2 and Kmax over the clinical course of eyes with KCN compared to those with post-refractive ectasia. These findings suggest that epithelial remodeling may play a more significant role in wound healing in corneas with KCN than in those with ectasia. Further study to determine the biomechanical and clinical factors that explain this difference in response may be warranted. Nonetheless, the overall clinical outcomes of CXL remain favorable, and CXL continues to be a promising treatment for both groups of patients.
We sought to identify prognostic factors for improvement in visual acuity. In this context, we found that eyes with preoperative apical scarring were more likely to show improvements in visual acuity by the last postoperative visit than those without apical scarring. This observation suggests that in eyes with apical scaring there may be more room for improvement in visual acuity after initial corneal remodeling [25,26,27].
Our pediatric population had greater severity of keratometric astigmatism at the outset of the study compared to our adult patients; however, there was no statistical difference in disease severity at presentation in terms of other tomographic parameters (K2, Km, Kmax, and pachymetry at the thinnest point). Another encouraging finding is that visual and tomographic outcomes were similar for both patient populations. These findings support early intervention in pediatric patients to prevent additional damage; they also suggest that at least in a subset of pediatric patients, most of the disease activity happens in childhood, followed by relative remission in adulthood.
Our clinical intuition led us to suggest that children do better than adults in terms of improvement in vision. Although our results do not demonstrate a statistical difference in the change in BSCVA between the adult and pediatric populations from the preoperative visit to the last recorded visit, the graph shown in Fig. 1a suggests that at least in some cases, there is a greater improvement in BSCVA in children. We presume that the lack of statistical significance is likely driven by a few cases in which visual acuity remained constant or worsened.
Stromal haze is a common occurrence in KCN eyes and post-refractive ectasia eyes, and a similar incidence of haze in both has been observed in previous large trials (57% of KCN eyes, 68% of post-refractive ectasia eyes) [12, 17]. Similar to these trials, we found the natural history of corneal haze was to peak at POM-1, with a subsequent resolution of haze [18]. A previous publication suggested that eyes with steeper and thinner corneas preoperatively, typical of more advanced KCN, were more likely to develop persistent postoperative stromal haze [28]. Our results do not show such an association. Additionally, our results do not demonstrate any predilection for persistent haze in patients with post-refractive ectasia, patients of a younger age, or patients that required the use of both Photrexa and Photrexa Viscous (vs. those requiring only Photrexa viscous).
The main limitation of this study is the lack of consistent follow-up through the extended postoperative period. Not every patient was able to follow the recommended follow-up schedule in this prospective study (1, 3, 6, and 12 months postoperatively and annually thereafter), thus certain visits were scattered at different postoperative time points. The reasons for this included patient financial constraints and geographic limitations that prevented patients from returning for frequent visits. This limitation was mitigated by clustering data into three time periods: a preoperative visit, a postoperative visit at 1 month (POM-1), and a last postoperative visit that occurred between months 3 and 24 (POM 3–24). Prior RCTs have shown that the majority of flattening of the corneal curvature occurs within the first month of CXL, and visits following that period are reflective of increasing corneal stability [12, 17]. Thus, it was deemed reasonable to group outcomes recorded after the third postoperative month.
Conclusions
This study provides further evidence that epithelium-off, full-fluence, Dresden protocol corneal crosslinking provides similar efficacy in the real world as it does in the RCTs that were conducted in the USA for its approval as a treatment of progressive KCN and post-refractive corneal ectasia. We have confirmed that this treatment leads to improvement (flattening) in maximum keratometry (Kmax), as well as stability in visual acuity over 24 months in children and adults with progressive KCN or post-refractive ectasia. Additionally, our findings suggest that the shrinkage of the anterior chamber that is observed following CXL may occur from geometric changes other than anterior/posterior corneal flattening alone.
References
Davidson AE, Hayes S, Hardcastle AJ, Tuft SJ. The pathogenesis of keratoconus. Eye (Lond). 2014; 28(2):189–95. https://doi.org/10.1038/eye.2013.278.
Binder PS. Ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2003;29:2419–29.
Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–22.
Kato N, Toda I, Kawakita T, Sakai C, Tsubota K. Topography-guided conductive keratoplasty: treatment for advanced keratoconus. Am J Ophthalmol. 2010;150(481–489):e1.
Kymionis GD, Siganos CS, Kounis G, Astyrakakis N, Kalyvianaki MI, Pallikaris IG. Management of post-LASIK corneal ectasia with intacs inserts: one-year results. Arch Ophthalmol Am Med Assoc. 2003;121:322–6.
Tuft SJ, Moodaley LC, Gregory WM, Davison CR, Buckley RJ. Prognostic factors for the progression of keratoconus. Ophthalmology. 1994;101:439–47.
Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a–induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7.
Ashwin PT, McDonnell PJ. Collagen cross-linkage: a comprehensive review and directions for future research. Br J Ophthalmol. 2010;94:965–70.
Hafezi F, Kanellopoulos J, Wiltfang R, Seiler T. Corneal collagen crosslinking with riboflavin and ultraviolet A to treat induced keratectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2007;33:2035–40.
Hersh PS, Greenstein SA, Fry KL. Corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011;37:149–60.
Wittig-Silva C, Chan E, Islam FMA, Wu T, Whiting M, Snibson GR. A randomized, controlled trial of corneal collagen cross-linking in progressive keratoconus: three-year results. Ophthalmology. 2014;121:812–21.
Hersh PS, Stulting RD, Muller D, et al. United States multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment. Ophthalmology. 2017;124:1259–70.
Wagner H, Barr JT, Zadnik K. Collaborative longitudinal evaluation of keratoconus (CLEK) study: methods and findings to date. Contact Lens Anterior Eye. 2007;30:223–32.
Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997;13:388–91.
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the Freiburg visual acuity test. Investig Ophthalmol Vis Sci. 2006;47:1236–40.
Jacob S, Kumar DA, Agarwal A, Basu S, Sinha P, Agarwal A. Contact lens-assisted collagen cross-linking (CACXL): a new technique for cross-linking thin corneas. J Refract Surg. 1995;2014(30):366–72.
Hersh PS, Stulting RD, Muller D, et al. U.S. Multicenter clinical trial of corneal collagen crosslinking for treatment of corneal ectasia after refractive surgery. Ophthalmology. 2017;124:1475–84.
Greenstein SA, Fry KL, Bhatt J, Hersh PS. Natural history of corneal haze after collagen crosslinking for keratoconus and corneal ectasia: Scheimpflug and biomicroscopic analysis. J Cataract Refract Surg. 2010;36:2105–14.
StataCorp. Stata statistical software: release 16. College Station: StataCorp LLC; 2019.
Greenstein SA, Shah VP, Fry KL, Hersh PS. Corneal thickness changes after corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011;37:691–700.
Rocha KM, Rocha KM, Perez-Straziota CE, Stulting RD, Randleman JB. Epithelial and stromal remodeling after corneal collagen cross-linking evaluated by spectral-domain OCT. J Refract Surg. 1995;2014(30):122–7.
De Bernardo M, Capasso L, Lanza M, et al. Long-term results of corneal collagen crosslinking for progressive keratoconus. J Optom. 2015;8:180–6.
Toprak I, Yildirim C. Scheimpflug parameters after corneal collagen crosslinking for keratoconus. Eur J Ophthalmol. 2013;23:793–8.
Shafik Shaheen M, Lolah MM, Piñero DP. The 7-year outcomes of epithelium-off corneal cross-linking in progressive keratoconus. J Refract Surg. 1995;2018(34):181–6.
Barr J, Zadnik K, Wilson B, et al. Factors associated with corneal scarring in the collaborative longitudinal evaluation of keratoconus (CLEK) study. Cornea. 2000;19:501–7.
Shehata AEM, Foster JW, Jun AS, Soiberman US. The correlation between corneal findings and disease severity in keratoconus per Scheimpflug corneal tomography. J Ophthalmol. 2020;2020:4130643.
Koller T, Pajic B, Vinciguerra P, Seiler T. Flattening of the cornea after collagen crosslinking for keratoconus. J Cataract Refract Surg. 2011;37:1488–92.
Raiskup F, Hoyer A, Spoerl E. Permanent corneal haze after riboflavin-UVA-induced cross-linking in keratoconus. J Refract Surg. 1995;2009(25):S824–828.
Acknowledgements
The authors would like to thank all patient participants for their involvement in this study.
Funding
This study was supported by National Eye Institute Grant K08EY027474, Wilmer Biostatistics Core Grant EY01765, and philanthropic grants from Debbie Colson and Jeffrey Williams, Dr. Ellen A. Cherniavsky, Hymowitz Family Foundation, Mr. and Mrs. Tyrone Throop, and the Kahn Foundation. The journal’s Rapid Service Fee was funded by internal funds at Johns Hopkins University.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Kraig S. Bower and Uri S. Soiberman are senior co-authors.
Prior Presentation
An abstract of this study was accepted for presentation at the 2020 Association for Research in Vision and Ophthalmology (ARVO) (May 2020) and published in Investigative Ophthalmology and Visual Science.
Disclosures
Derick O. Ansah, Jiangxia Wang, Kevin Lu, Samir Jabbour, Kraig S. Bower and Uri S. Soiberman have nothing to disclose.
Compliance with Ethics Guidelines
Approval for this prospective observational study was obtained from the Institutional Review Board at Johns Hopkins University, and the study was conducted in accordance with HIPPA rules (https://www.hhs.gov/hipaa/for-professionals/privacy/index.html). This research adheres to the tenets of the Helsinki Declaration of 1964, and its later amendments. All patients gave informed consent to participate in this study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12962696.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ansah, D.O., Wang, J., Lu, K. et al. Post-FDA Approval Results of Epithelium-Off, Full-Fluence, Dresden Protocol Corneal Collagen Crosslinking in the USA. Ophthalmol Ther 9, 1023–1040 (2020). https://doi.org/10.1007/s40123-020-00306-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-020-00306-1