Abstract
Patient safety is a primary priority in the conduction of retinal gene therapy trials. An understanding of risk factors and mitigation strategies for post-procedure complications is crucial for the optimization of gene therapy clinical trial protocols. In this review, we synthesize the literature on ocular delivery methods, vector platforms, and treatment-emergent adverse effects in recent gene therapy clinical trials for inherited retinal diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Numerous active and planned clinical trials are investigating the safety of adeno-associated virus (AAV)-mediated gene therapy for inherited retinal diseases (IRDs). |
Treatment-emergent adverse events (TEAEs) are related to the delivery method, vector system, and underlying retinal condition. |
Emphasis should be placed on minimizing subretinal- and intravitreal-related complications, the most common cause of adverse events in completed gene replacement trials. |
Perioperative steroids are used to manage AAV immunogenicity. |
Introduction
Targeted vector-based gene therapy has been rapidly developing over the past decade to halt disease progression and preserve visual function for inherited retinal diseases (IRDs). Recessive retinal disorders may be treated with gene replacement therapy, in which a pathogenic gene is replaced with a functional gene. The landmark approval of Luxturna opened the door for genetic augmentation of other visually devastating inherited disorders [1]. Numerous gene augmentation trials have been completed or are under way for the treatment of several IRDs, including Leber congenital amaurosis, retinitis pigmentosa, choroideremia, achromatopsia, Stargardt disease, Leber hereditary optic neuropathy, and X-linked retinoschisis.
Anatomically accessible and easily monitored with noninvasive imaging, the retina has been an ideal candidate for genetic therapy interventions [2]. Heavily confined and immune-privileged, systemic side effects are typically limited from therapeutic interventions introduced directly into the retina. With a tight blood–retinal barrier (BRB) and immunosuppressive ocular environment, the retina effectively restricts the inflammatory response to potential therapies [3].
Clinicians should stay up to date and implement recommended technique adjustments and protocol modifications to improve patient safety in the numerous ongoing retinal gene therapy trials. Treatment-emergent adverse events (TEAEs) from gene therapy are typically related to the injection procedure and vector platform. This article will review the risk factors for developing these complications and discuss evidence-based recommendations for mitigating these adverse outcomes. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Viral Vectors
Viral vector systems for ocular genetic therapy come with different risk assessments and safety profiles. Most clinical trials for IRDs currently use recombinant adeno-associated viral (AAV) vectors to deliver the normal functional gene of interest into the retina, restoring the visual transduction pathway. AAVs, a single-stranded DNA parvovirus vector, have been preferable to other viral vectors in transducing target cells, as they are nonpathogenic, non-integrating, and longer-lasting [2, 4]. However, they are limited by a small gene-carrying capacity of approximately 4.7 kilobases (kb) [4].
Lentiviral vectors, a type of retrovirus, have a high packing capacity of approximately 8 kb and are capable of transducing multiple cell types, making them more suitable for IRDs with large causative genes such as Stargardt disease and Usher syndrome type 1B [5]. However, insertional mutagenesis is a potentially serious complication of lentiviruses [6]. Nonviral vector platforms may eventually resolve many of the aforementioned obstacles of viral vectors [7].
The introduction of a viral vector agent has the potential to cause a substantial and harmful immune response that reduces visual outcomes. In the general population, there is greater pre-existing immunity against AAV2 relative to other AAV subtypes [8]. AAV5, AAV8, and AAV9 vectors, with the lowest seroprevalence, may be superior constructs in limiting the inflammatory response [8]. Exclusion criteria in clinical trials often include a threshold titer level of neutralizing antibodies (NAbs) against the specific study vector. To reduce the incidence of inflammatory reactions, periprocedural immunomodulatory therapies are increasingly being incorporated into numerous AAV-mediated gene replacement trials.
Administration Routes
Several intraocular approaches are available to deliver the AAV vectors carrying the functional target gene to the damaged retinal cells, including subretinal (SR), intravitreal (IVT), suprachoroidal, and sub-internal limiting membrane (subILM). As the majority of adverse effects in retinal gene therapy trials are directly related to the procedure, we discuss the literature on minimizing procedure-related complications. Tissue properties and cell types are affected differently based on the specific genetic mutation. These properties are important considerations in selecting the injection approach and predicting intra-procedural obstacles. The preferred injection approach is typically uniform for trials treating the same IRD.
Subretinal
Compared to traditional 20-gauge surgery, novel microincision vitrectomy surgery (MIVS) gauge systems have reduced incidence of iatrogenic retinal tears, ocular hemorrhages, astigmatism, and postoperative pain and inflammation [9,10,11,12]. With shorter operating times and enhanced visual outcomes, they have become the predominant platforms for vitrectomies. MIVS include transconjunctival sutureless 23-, 25-, and 27-gauge instrument designs, with the 23-gauge system being the most commonly adopted in gene therapy trials. There are conflicting reports on the rate of intraoperative and postoperative complications among the three main MIVS gauge systems, with most data showing similar safety profiles [13, 14]. A recent comprehensive review comparing 23- and 25-gauge pars plana vitrectomy (PPV) surgery showed an increased rate of overall adverse events for the 23-gauge system [15]. Additionally, 25- and 27-gauge PPV have shown increased intraocular pressure (IOP) stability and decreased conjunctival trauma compared to 23-gauge PPV [16, 17]. Future studies are necessary to clearly validate the most appropriate instrument size for gene therapy trials.
Located between the photoreceptors and retinal pigment epithelial (RPE) cells, the subretinal space is a readily accessible location for the delivery of targeted gene therapy directly to cells of interest. An invasive alternative to intravitreal injections, subretinal injections, allow precise targeting of most outer retinal cell types affected in IRDs [18]. In genetic therapy trials, the subretinal space is accessed through small-gauge PPV surgery followed by vector injection [19]. The specific surgical technique will vary among trials and surgeons. Some trials elect to use a two-step technique where vector injection follows the formation of a subretinal bleb of balanced salt solution (BSS). The BSS parafoveal bleb ensures accurate location for vector injection, minimizing loss of vector into the vitreous and choroid [19]. Small BSS pre-blebs are used for thin retinas, while large pre-blebs are used in diseases with more adhesive foveal areas [19]. Practitioners who opt for a one-step delivery method argue that a one-step approach avoids the risk of excessive retinal stretching and vector reflex associated with the two-step method [20]. Oral corticosteroids are typically started 3 days before surgery, with tapering 2 weeks following the procedure to reduce both procedure- and vector-related inflammation [19].
There are certain known adverse events associated with PPV surgery, including cystoid macular edema (CME) development, retinal detachment, increased IOP, endophthalmitis, ocular hemorrhage, epiretinal membranes, macular hole formation, cataract progression, glaucoma, and hypotony [21]. A few studies have assessed risk factors and the preoperative management of PPV-associated complications. Intraoperatively, surgeons must carefully examine the peripheral retina to identify and treat iatrogenic retinal breaks. Postoperative IOP elevation is a concern that can be effectively reduced with topical prophylactic IOP medications and small gauges intraoperatively [22, 23]. Accurate speed and pressure during vector injection with a controlled foot pedal is necessary to decrease the likelihood of hemorrhage and macular hole formation [18, 24]. Along with the aforementioned optimization of the injection system, macular hole formation may be reduced through preoperative identification of thin retinal areas with optical coherence tomography (OCT) and autofluorescence (AF) imaging [25]. Heavy liquid can be positioned over these areas during injection to prevent opening [25].
Acute infectious endophthalmitis, an infrequent but severe complication of PPV, is linked to pre-existing systemic immunosuppression, pseudophakia, aphakia, and use of topical steroids prior to surgery [26, 27]. Inadequate wound closure leading to ocular hypotony and ingress of surface bacteria is the main predisposing risk factor for endophthalmitis [28]. The proper technique involves conjunctival displacement and angled sclerotomy [27]. Meticulous examination of sclerotomy sites requiring suturing is crucial to preventing leakage and inoculation of flora into the vitreous. Effective and safe techniques for sealing leaking sclerotomies include simple suturing, diathermy, scleral needling, resealable vicryl sutures, and cauterization [29,30,31]. Bacterial contamination in the vitreous from the conjunctiva has been shown to be safely reduced through repeated field irrigation with 0.25% povidone-iodine (PVI) [32]. Additionally, compared to fluid, air and gas are superior final intraocular tamponades for accurate closure of wounds and prevention of postoperative endophthalmitis [33, 34].
Intraoperative and patient-related risk factors for the development of suprachoroidal hemorrhage in PPV include advanced age, male sex, and anticoagulant or antiplatelet medication [35]. Hypotony (intraocular pressure less than 6 mmHg) following MIVS is associated with high myopia, young age, and pseudophakia [36, 37]. Extra caution should be taken for patients with these risk factors. The risk of hypotony following 23- and 25-gauge PPV has been demonstrated to be reduced by utilizing two- and three-step incision methods as well as 25% sulfur hexafluoride (SF6) gas at the conclusion of the procedure [38,39,40].
Recent technological microsurgery accessories have improved patient safety. Intraoperative use of OCT enables enhanced visualization for real-time adjustments of the surgical approach [41]. This is particularly useful in delivering gene therapy, as it facilitates precise confirmation of site injection, retinal bleb creation, and drug dosage [42]. Microscope-integrated OCT (MIOCT) may help prevent complications of inaccurate needle tip placement and repeat subretinal bleb formations such as hemorrhage, cannula tip obstruction, macular hole formation, retinoschisis, and RPE damage [43]. Robotic augmented vitreoretinal surgery has emerged in an effort to improve dexterity and control [44]. The first trial to use robotic-assisted surgery in human patients, the Robotic Retinal Dissection Device trial, demonstrated promising early safety results [45]. As subretinal injections are long procedures, robotic technology has enormous potential in improving outcomes and minimizing complications. Assimilating new technology into PPV will present a host of new technical and operative challenges.
Intravitreal
Intravitreal injections, the most common retinal procedure, involve nonoperative treatments inserted directly into the vitreous cavity. They are simple and efficient, but with limited effectiveness in targeting cells in the posterior segment of the eye due to transduction barriers, the most significant of which is the internal limiting membrane [46, 47]. IVT injection, therefore, is more suitable for targeting inner retinal layers [18]. In the future, potential surgical complications from SR injections may be avoided through novel AAV variants that are able to reach the outer retina after IVT injection [48, 49].
There are certain procedure-related adverse outcomes associated with intravitreal injections. Endophthalmitis is a rare but feared complication associated with IVT injections [50, 51]. In large prospective trials and reviews, post-injection endophthalmitis incidence rates have ranged from 0.028 to 0.056% [52]. Most frequently, organisms identified are coagulase-negative Staphylococcus and Streptococcus species [53]. As these are common upper respiratory tract flora, it is recommended that individuals take droplet contamination precautions such as wearing surgical masks and avoiding communication when injecting to reduce the risk of infection [54, 55]. The use of topical post-injection antibiotics does not reduce the risk of endophthalmitis [56]. Additional precautionary measures include PVI for sterilization of the ocular surface, subconjunctival 2% lidocaine for anesthesia, pre-filled syringes, and utilization of a sterile speculum or splint to minimize exposure of instruments to eyelids and eyelashes [57,58,59,60,61]. PVI should be applied following placement of the eyelid speculum [62].
Other vision-threatening complications include retinal tear/detachment, cataract formation, uveitis, hypotony, and intraocular hemorrhage [63]. Retinal detachment is a rare adverse effect with a prevalence between 0.0 and 0.08% per injection [64]. A proper technique with accurate measurement of the injection site has been demonstrated to reduce the rate of detachments [65, 66]. It is important to clearly discuss signs of retinal detachment (photopsia, peripheral vision loss) with patients for prompt recognition and treatment.
Common post-injection complications include subconjunctival hemorrhage (SCH) and floaters. Hypertensive patients are at a higher risk of developing SCH [67]. Patients should be educated and reassured that these are benign, painless complications that will resolve within days or weeks. A post-injection transient increase in intraocular pressure (IOP) that normalizes within 30 min without intervention is also commonly observed [68]. Pre-injection IOP-lowering therapies are not effective in preventing these transient spikes [69]. There is evidence that high injection volumes, fast injection rates, and smaller-gauge needles are associated with sustained IOP elevation [70, 71]. The status of the optic nerve should be carefully monitored post-injection, especially in patients with pre-existing ocular hypertension and glaucoma.
Certain approaches are available to enhance patient comfort and compliance during IVT injection. An additional staff member, neck pillow, classical music, and verbal notification prior to injection improve overall patient satisfaction [72, 73]. There is no consensus topical anesthetic technique for pain management, but subconjunctival injection of 2% lidocaine may be used for patients more sensitive to pain [74]. Injection into the superior nasal quadrant and topical nonsteroidal anti-inflammatory drug (NSAID) administration post-procedure are associated with less patient discomfort [75, 76].
Multiplicity of infection (MOI), an important consideration for delivery approaches, refers to the ratio of viral particles per total number of transduced target cells. MOI is dependent upon both the underlying disease characteristics and stage [2]. Larger retinal target areas require more viral vectors to reach necessary MOI for effective transduction [2]. A larger vector dose increases undesired dissemination and the potential for a deleterious immune response [2, 18]. This is particularly important in IVT injections that target broader retinal areas. In preclinical models, intravitreal AAV delivery induced a more robust immune response compared to subretinal injection [77]. Relative to SR injection, a longer post-injection course of systemic corticosteroids is typically used to mitigate the inflammatory response [78].
Suprachoroidal
The suprachoroidal space (SCS), an anatomical space between the sclera and choroid, is a novel delivery route that has been under investigation for the administration of therapeutic agents. With greater distribution and unimpeded by the internal limiting membrane, SCS injection allows ocular drug therapy delivery into the posterior segment without vitrectomy or retinotomy [79].
While the SCS may be accessed through catheters, microneedles are a recent minimally invasive and simple alternative [80]. Recent preclinical models of AAV-mediated gene delivery through the SCS are encouraging, but prospective studies are needed to substantiate the safety profile [81]. Reported adverse events from suprachoroidal drug delivery clinical trials include eye pain, anterior chamber inflammation, conjunctival edema, hemorrhage, punctate keratitis, and retinal artery occlusion [82]. Anterior segment- and vitreous cavity-associated complications, including endophthalmitis, cataract formation, and retinal detachment, will theoretically be avoided [83].
Peri-injection preparation for intravitreal injection is similar to that for IVT injections. Injection is likewise in the pars plana, in approximately the same site. While there is not enough data on recommended guidelines for preventing adverse events, it is reasonable to believe that similar precautions should be applied.
Sub-Internal Limiting Membrane
In a patient population with fragile retinas, the capability to effectively transduce inner and outer retinal cells of interest without physically stretching the central retina is highly sought after [84]. A novel promising alternative “subILM” injection method was recently proposed in which a vector is delivered into a surgically created space between the retina and ILM [84]. Only in its infancy, future preclinical and clinical studies are necessary to examine subILM injections as a viable alternative to SR and IVT injections.
Recent Gene Replacement Clinical Trials
Safety Evaluation Procedures
The safety profile is related to both the study vector and administration route. Safety evaluations involve full ophthalmic examinations, adverse event reports, laboratory testing, immunogenicity, and biodistribution analysis. Vector immunogenicity is assessed through enzyme-linked immunosorbent assays (ELISA) for antibodies against the specific vector employed. A polymerase chain reaction (PCR) is used to assess systemic biodistribution and viral shedding.
RPE65-Associated Leber Congenital Amaurosis
Leber congenital amaurosis (LCA) is a severe, rapidly progressive IRD characterized by early-onset visual loss and nyctalopia. RPE65, one of many causative genes for LCA, encodes an essential enzyme in the production of 11-cis-retinol during the visual cycle [85]. RPE65-mediated LCA patients were the first to undergo subretinal gene replacement therapy [86]. The SR approach is preferred to specifically target RPE cells.
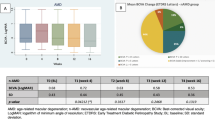
There have been five phase I/II trials and one phase III trial by several groups investigating AAV-mediated replacement of RPE65 in patients with RPE65-mediated LCA. The safety results of an initial open-label phase I trial exploring single, unilateral SR injections of an AAV2 vector carrying RPE65 DNA in 12 LCA patients with RPE65 mutations were favorable and consistent with expected AEs [87]. A follow-on phase I trial of the same patients demonstrated good safety in administration of AAV2-hRPE65v2 to the contralateral, previously untreated eye [88]. Following these two successful trials, a randomized controlled phase III trial of sequential, bilateral SR administration of AAV2-hRPE65v2 in 29 participants was initiated [89]. Of the 29 participants, 20 underwent treatment while the other 9 served as controls for at least 1 year before undergoing therapy. The same vector construct and dose were used in the follow-on and phase III trials. Two-year data for the phase III trial and 4-year results for the phase I follow-on study revealed a positive long-term safety profile that was consistent with known adverse outcomes of the SR approach [90]. The majority of ocular TEAEs were mild in severity, consisting primarily of pain, inflammation, macular hole, maculopathy retinal hemorrhage, conjunctival hyperemia, retinal tear and deposits, dellen, elevated IOP, and cataract. These events predominantly resolved spontaneously or with appropriate treatment. Two serious ocular events were encountered: one participant developed increased IOP and optic atrophy 3 months after treatment for bacterial endophthalmitis, and one participant experienced unresolved central retinal thinning with loss of foveal function [90]. No clinically significant immune response was observed, most likely attributable to a peri- and postoperative steroid regimen [90].
While other phase I/II gene therapy trials have used different vector constructs or modified surgical approaches compared to Maguire and associates, the long-term safety profiles have been consistent with that of Luxturna [91,92,93,94]. A meta-analysis of 82 patients from five phase I/II trials and one phase III trial revealed central retinal thinning in the treated eyes compared to control eyes 2–3 years following intervention [95]. While the etiology is unknown, the authors hypothesized that retinal thinning was a result of iatrogenic retinal detachment induced during the SR procedure [95].
Choroideremia
Choroideremia (CHM) is a slowly progressive X-linked IRD caused by mutations in the CHM gene [96]. Xue and associates conducted a phase I/II dose-escalation trial exploring the safety of unilateral subretinal administration of AAV2.REP1 vector in 14 CHM patients [97]. Two of the fourteen patients experienced significant TEAEs. Surgical difficulties in subretinal bleb formation resulted in a lower dose delivered and retinal thinning in one treated eye. The second significant AE was likely related to a combination of the vector procedure and SR injection, involving substantial ocular inflammation that resolved following systemic steroids. Following these two complications, the clinical team began using an extended postoperative course of corticosteroids, an automated injection system, and intraoperative OCT [97]. There was no incidence of serious AEs or inflammation in the remaining patients after these protocol changes.
An additional phase I trial in six patients over a 2-year period with a higher dose relative to the first trial described reported a favorable safety profile for single SR injection of rAAV2.REP1 [98]. While the optimized injection system described by Xue et al. was used, microscope-integrated OCT was not used to guide subretinal bleb creation [97]. Hyperreflective loci, a serious AE hypothesized to be related to the AAV vector, were observed on OCT in one patient 1 month postoperatively [98]. The loci resolved with systemic corticosteroids, but the patient experienced decreased vision and retinal thinning. Video of the surgical procedure for this subject showed injection of air bubbles into the subretinal space as well as a limited release of subretinal, intraretinal, and vitreous hemorrhage [98]. The rest of the AEs in both phase I trials were mild to moderate in intensity, with the majority resolving spontaneously without significant sequelae. Mild procedure-related ocular AEs in both phase I trials included subconjunctival hemorrhage, discomfort, micropsia, metamorphopsia, blurred vision, flashing lights, and cataract development. Only a few ocular complications were potentially attributable to the study vector, including flashing lights, cataract, and grittiness. Systemically, there was no evidence of vector dissemination or neutralizing AAV antibodies [98].
Two recent phase II trials using the same AAV vector construct corroborated the phase I safety results. Lam et al. described an encouraging 2-year safety profile in six patients SR-injected with high-dose AAV2-REP1 [99]. The authors performed the SR procedure with a standard 23-gauge vitrectomy, MIOCT, and an automated injection system. No serious AEs were noted, with the majority of the complications consistent with expected events following an SR procedure. Mild AEs included subretinal fluid, conjunctival hemorrhage, anterior chamber cells, diplopia, and cataract. A minimal immunologic response to the viral vector with transient shedding and anti-AAV-2 neutralizing antibodies was observed in two separate patients. Two patients with lamellar thinning at baseline developed a macular hole in the damaged retinal areas [99]. To prevent macular hole formation, the authors emphasized use of preoperative OCT in identifying vulnerable retinal areas as well as utilization of MIOCT to minimize unnecessary foveal manipulation [99]. Iatrogenic retinal detachment during sub-foveal bleb formation is difficult in patients with CHM due to excessive areas of subretinal adhesions [25]. Larger BSS parafoveal pre-blebs and perfluorocarbon liquid have been recommended to aid these excessively adhesive areas and prevent unnecessary retinal stretch and vector reflux [19, 100]. A second phase II trial in six men over a 2-year period showed AAV2-REP1 to be well tolerated, with an AE profile similar to the trial conducted by Lam and associates [99, 101]. One patient developed an intraoperative retinal hole that sealed by the conclusion of surgery. No severe or vector-associated AEs were encountered [101]. A randomized phase III trial (NCT03496012) in 140 CHM patients currently under way will help validate the safety of AAV2-REP1.
Stargardt Disease
Stargardt disease (STGD), the most common form of juvenile macular degeneration, presents in young adolescents with a progressive decline in central vision [102]. Mutations in the ABCA4 gene, an encoder of a photoreceptor ATP-binding transporter, are the most common culprits in recessive STGD [103]. The gene size of ABCA4 exceeds the carrying capacity of AAV, requiring the use of dual-AAV, lentiviral, and nonviral platforms [104,105,106]. Sanofi initiated a study investigating intravitreal delivery of a lentiviral vector carrying ABCA4 in 22 subjects (NCT01367444). The study was terminated due to review of clinical development priorities, but preliminary 1-year safety results were promising, with subjects experiencing 125 mild to moderate adverse events [107]. Sanofi is conducting a second long-term dose-escalation phase I/II trial investigating SR injection of a lentivirus carrying ABCA4 (SAR422459) in 27 participants (NCT01736592).
Retinitis Pigmentosa
Retinitis pigmentosa (RP) is a genetically diverse group of rod-cone dystrophies that begins with rod photoreceptor impairment, eventually culminating in degeneration of both rod and cone photoreceptors [108]. Clinically, patients will experience nyctalopia followed by a progressively constricting visual field and loss of central vision. Gene replacement strategies have been applied in MERTK-associated RP and X-linked retinitis pigmentosa (XLRP).
Mutations in MERTK (MER Proto-Oncogene, Tyrosine Kinase), an essential gene in the regulation of RPE phagocytosis, are implicated in RP [109]. Ghazi et al. investigated the safety of SR administration of rAAV2-VMD2-hMERTK in six patients with MERTK-related RP [110]. They reported no systemic toxicities and only a few mild TEAEs, including filamentary keratitis, submacular fluid, and cataract formation [110]. Notably, one patient developed oscillopsia following a shallow detachment of the fovea intraoperatively. There is no consensus on the mechanism behind this unusual complication in this patient [110]. Unlike most other gene therapy trials, the protocol involved a 20-gauge vitrectomy and no perioperative steroids.
X-linked retinitis pigmentosa, the most severe form of RP, is characterized by profound night blindness and visual loss in early childhood [111]. RPGR (Retinitis Pigmentosa GTPase Regulator), the major XLRP gene, has been the primary target in gene replacement studies [112]. A recent phase I/II trial investigated the SR administration of an AAV vector encoding codon-optimized human RPGR (AAV8-coRPGR) in 18 XLRP patients with mutations in RPGR over a 6-month period [113]. They reported no severe ocular or systemic toxicities. Only mild corticosteroid-responsive subretinal inflammation was linked to the viral vector, with other transient AEs such as hemorrhage, uveitis, subretinal fluid, corneal abrasion, pain, and suture granuloma linked to the surgical approach [113].
Achromatopsia
Achromatopsia is a slowly progressive congenital retinal disorder that primarily affects cone photoreceptor function [114]. Patients typically present in early infancy with photophobia, nystagmus, and hemeralopia. Of the six known causative variants, mutations in cyclic nucleotide-gated channel alpha and beta 3 (CNGA3 and CNGB3) genes are responsible for the majority of achromatopsia cases [115].
The first human trial investigated the safety of SR delivery of an AAV8 vector for complete CNGA3-linked achromatopsia over a 12-month period [116]. In a limited cohort of nine patients, safety results were favorable, with only mild ocular and systemic AEs consistent with expected complications of the SR injection. Procedure-related ocular AEs that were transient or responsive to treatment included conjunctival injection and chemosis, foreign body sensation, corneal erosion, and hemorrhage [116]. There were two cases of mild pigmentary changes that did not resolve. Potential vector-linked AEs were steroid-responsive hyper-reflective spots and iridocyclitis [116].
LHON
Leber hereditary optic neuropathy (LHON), the most common inherited mitochondrial disorder, causes early-onset severe binocular loss of central vision [117]. LHON is caused by point mutations in mitochondrial DNA (mtDNA) encoding subunits of electron transport chain complex I, the most common of which is G11778A in the NADH dehydrogenase subunit (ND4) gene [118]. An IVT approach is typically used in LHON gene therapy trials to target the more accessible layer of affected retinal ganglion cells.
Wan and associates conducted a phase I trial evaluating the safety of IVT-delivered rAAV2 carrying ND4 DNA (rAAV2-ND4) in nine LHON patients with the G11778A mutation [78]. To account for the increased immunogenicity in IVT administration, a 9-week course of corticosteroids was used to minimize the inflammatory response. Additionally, patients who had anti-AAV2 neutralizing antibodies at baseline were excluded from the study. Seven-year follow-up demonstrated an excellent safety profile, with no AEs and no significant immune response [119].
An additional 2-year study in 14 LHON patients explored the safety of a single, unilateral IVT injection of a self-complementary AAV2-ND4 vector [AAV2(Y444,500,730F)-P1ND4v2] [120]. All participants had AAV2-neutralizing antibodies prior to treatment, but a steroid regimen was not part of the intervention protocol. Two patients developed transient anterior uveitis 2 months following injection, with serum NAbs increasing in one of these participants. All other ocular AEs, including elevated IOP, keratitis, and subconjunctival hemorrhage, were directly connected to the IVT injection procedure [120].
GenSight Biologics conducted a 2-year dose-escalation phase I/II trial of rAAV2/2-ND4 in 13 LHON patients, showing a favorable safety profile, with the majority of ocular AEs mild in severity and responsive to appropriate therapy without sequelae [121]. IVT injection-related AEs encountered included subconjunctival hemorrhage, keratitis, and ocular hypertension. Two patients developed moderate elevation of IOP, with one of the patients not receiving prophylactic IOP-lowering medications prior to injection [121]. AEs believed to be related to AAV2-ND4 vector included anterior chamber inflammation, punctate serous detachment, vitritis, and eye pain. Similar to the study described by Guy et al., peri-injection immunosuppression was excluded from the protocol design [120, 121]. Ocular inflammation, the most commonly observed AE, was reported to be non-dose-dependent, with only one case of serious intensity [122]. While there was no clear association in this small sample size between patients with higher baseline NAb levels and intensity of intraocular inflammation, the patient with the highest baseline NAb levels experienced the most severe anterior inflammation [122]. Before larger studies elucidate further risk factors for ocular inflammation, clinicians should pay greater attention to patients with higher baseline immune reactivity against the AAV vector and consider peri-injection corticosteroids. GenSight Biologics is currently conducting two phase III trials evaluating the safety and efficacy of rAAV2/2-ND4 (GS010) (NCT02652767, NCT02652780). Press releases from the 96-week follow-ups corroborated early encouraging safety results describing adverse events linked mostly to the injection procedure [123, 124].
XLRS
X-linked retinoschisis (XLRS), caused by mutations in the RS1 gene, is characterized by inner retinal layer splitting and typically young men presenting with variable visual disturbances [125, 126]. RS1 mutations result in a dysfunctional retinoschisin protein destabilizing cell adhesion among retinal cell layers [127]. As these patients are prone to developing retinal detachments and other surgery-related complications, investigators have chosen to use an IVT approach instead of the typical SR technique to target the cells of interest and to avoid potential detachments. A phase I/IIa study assessed the safety of RS1 AAV (AAV8-RS1) administered by intravitreal injection in eight participants over an 18-month span [128]. Overall, treatment was well tolerated, with mild AEs likely linked to the vector including corticosteroid-responsive anterior chamber and vitritis. Notably, one patient underwent vitrectomy for post-inflammatory posterior vitreous detachment complicated by a retinal tear and vitreous hemorrhage [128]. AEs related to the IVT procedure included iridocyclitis, photopsia, keratic precipitates, and elevated IOP [128].
Conclusions
As the era of gene therapy moves forward, there should be a focus on minimizing adverse events through continued refinement of delivery method, ancillary technology, and prophylactic measures. Complications may be inevitable, but clinical trial investigators and surgeons should be aware of the potential serious adverse events, risk factors, and perioperative strategies for each individual patient. Ophthalmologists and clinical trial principal investigators should carefully inform patients of the possibilities of these complications and assuage any pre-procedural anxiety.
Based on current results, there are minimal vector-related side effects, with treatment complications mostly related to the delivery approach. In this new and ever-evolving field, it is essential for clinicians to continue sharing technique modifications to maximize outcomes and minimize adverse events. Future large-scale gene therapy trials and data sets will refine these protocols and establish long-term safety profiles.
References
FDA. FDA approves novel gene therapy to treat patients with a rare form of inherited vision loss. In: https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm589467.html. Accessed July 16, 2020.
Ong T, Pennesi ME, Birch DG, et al. Adeno-associated viral gene therapy for inherited retinal disease. Pharm Res. 2019;36:34.
Zhou R, Caspi RR. Ocular immune privilege. F1000 Biol Rep. 2010;2:3.
Han Z, Conley SM, Naash MI. AAV and compacted DNA nanoparticles for the treatment of retinal disorders: challenges and future prospects. Invest Ophthalmol Vis Sci. 2011;52:3051–9.
Zufferey R, Dull T, Mandel RJ, et al. Self-inactivating lentivirus vector for safe and efficient in vivo gene delivery. J Virol. 1998;72:9873–80.
Romano G, Marino IR, Pentimalli F, et al. Insertional mutagenesis and development of malignancies induced by integrating gene delivery systems: implications for the design of safer gene-based interventions in patients. Drug News Perspect. 2009;22:185–96.
Kelley RA, Conley SM, Makkia R, et al. DNA nanoparticles are safe and nontoxic in non-human primate eyes. Int J Nanomed. 2018;13:1361–79.
Boutin S, Monteilhet V, Veron P, et al. Prevalence of serum IgG and neutralizing factors against adeno-associated virus (AAV) types 1, 2, 5, 6, 8, and 9 in the healthy population: implications for gene therapy using AAV vectors. Hum Gene Ther. 2010;21:704–12.
Neffendorf JE, Gupta B, Williamson TH. Intraoperative complications of patients undergoing small-gauge and 20-gauge vitrectomy: a database study of 4,274 procedures. Eur J Ophthalmol. 2017;27:226–30.
Mentens R, Stalmans P. Comparison of postoperative comfort in 20 gauge versus 23 gauge pars plana vitrectomy. Bull Soc Belge Ophtalmol. 2009;311:5–10.
Kellner L, Wimpissinger B, Stolba U, et al. 25-gauge vs 20-gauge system for pars plana vitrectomy: a prospective randomised clinical trial. Br J Ophthalmol. 2007;91:945–8.
Inoue Y, Kadonosono K, Yamakawa T, et al. Surgically-induced inflammation with 20-, 23-, and 25-gauge vitrectomy systems: an experimental study. Retina. 2009;29:477–80.
Nam Y, Chung H, Lee JY, et al. Comparison of 25- and 23-gauge sutureless microincision vitrectomy surgery in the treatment of various vitreoretinal diseases. Eye. 2010;24:869–74.
Veritti D, Sarao V, Lanzetta P. A propensity-score matching comparison between 27-gauge and 25-gauge vitrectomy systems for the repair of primary rhegmatogenous retinal detachment. J Ophthalmol. 2019;2019:3120960.
Igelman AD, Johnson JA, Taylor SC, et al. Postoperative complication rates in 23- vs 25-gauge pars plana vitrectomy. J VitreoRetin Dis. 2018;2:272–5.
Ho LY, Garretson BR, Ranchod TM, et al. Study of intraocular pressure after 23-gauge and 25-gauge pars plana vitrectomy randomized to fluid versus air fill. Retina. 2011;31:1109–17.
Charles S, Ho AC, Dugel PU, et al. Clinical comparison of 27-gauge and 23-gauge instruments on the outcomes of pars plana vitrectomy surgery for the treatment of vitreoretinal diseases. Curr Opin Ophthalmol. 2020;31:185–91.
Ochakovski GA, Bartz-Schmidt KU, Fischer MD. Retinal gene therapy: surgical vector delivery in the translation to clinical trials. Front Neurosci. 2017;11:174.
Davis JL, Gregori NZ, MacLaren RE, et al. Surgical technique for subretinal gene therapy in humans with inherited retinal degeneration. Retina. 2019;39:S2–S8.
Fan KC, Yannuzzi NA, Patel NA, et al. Surgical techniques for the subretinal delivery of pediatric gene therapy. Ophthalmol Retina. 2020;4:644–5.
Shields RA, Ludwig CA, Powers MA, et al. Postoperative adverse events, interventions, and the utility of routine follow-up after 23-, 25-, and 27-gauge pars plana vitrectomy. Asia-Pac J Ophthalmol. 2019;8:36–42.
Alexander P, Michaels L, Newsom R. Is day-1 postoperative review necessary after pars plana vitrectomy? Eye (London, England). 2015;29:1489–94.
Ahn SJ, Woo SJ, Ahn J, et al. Comparison of postoperative intraocular pressure changes between 23-gauge transconjunctival sutureless vitrectomy and conventional 20-gauge vitrectomy. Eye. 2012;26:796–802.
Kwon HJ, Kwon OW, Song WK. Semiautomated subretinal fluid injection method using viscous fluid injection mode. Retina. 2019;39:S174–S176176.
Xue K, Groppe M, Salvetti AP, et al. Technique of retinal gene therapy: delivery of viral vector into the subretinal space. Eye (Lond). 2017;31:1308–16.
Park JC, Ramasamy B, Shaw S, et al. A prospective and nationwide study investigating endophthalmitis following pars plana vitrectomy: incidence and risk factors. Br J Ophthalmol. 2014;98:529.
Bhende M, Raman R, Singh N, et al. Risk factors for endophthalmitis after pars plana vitrectomies in a Tertiary Eye Institute in India. Ophthalmol Retina. 2018;2:779–84.
Gupta OP, Maguire JI, Eagle RC Jr, et al. The competency of pars plana vitrectomy incisions: a comparative histologic and spectrophotometric analysis. Am J Ophthalmol. 2009;147(243–50):e1.
Reibaldi M, Longo A, Reibaldi A, et al. Diathermy of leaking sclerotomies after 23-gauge transconjunctival pars plana vitrectomy: a prospective study. Retina. 2013;33:939–45.
Arana LA, Moreira ATR, Grandinetti AA, et al. Novel vicryl releasable suture technique to close leaking sclerotomies in a transconjunctival vitrectomy. Retina. 2019;39(Suppl 1):S108–S111111.
Felfeli T, Altomare F, Mandelcorn ED. Sutureless closure of 23-and 25-gauge leaking sclerotomies with the scleral needling technique. Retina. 2020;40:838–44.
Shimada H, Nakashizuka H, Hattori T, et al. Reduction of vitreous contamination rate after 25-gauge vitrectomy by surface irrigation with 0.25% povidone–iodine. Retina. 2013;33:143–51.
Yamane S, Kadonosono K, Inoue M, et al. Effect of intravitreal gas tamponade for sutureless vitrectomy wounds: three-dimensional corneal and anterior segment optical coherence tomography study. Retina. 2011;31:702–6.
Chiang A, Kaiser RS, Avery RL, et al. Endophthalmitis in microincision vitrectomy: outcomes of gas-filled eyes. Retina. 2011;31:1513–7.
Chandra A, Xing W, Kadhim MR, et al. Suprachoroidal hemorrhage in pars plana vitrectomy: risk factors and outcomes over 10 years. Ophthalmology. 2014;121:311–7.
Woo SJ, Park KH, Hwang J-M, et al. Risk factors associated with sclerotomy leakage and postoperative hypotony after 23-gauge transconjunctival sutureless vitrectomy. Retina. 2009;29:456–63.
Mimouni M, Abualhasan H, Derman L, et al. Incidence and risk factors for hypotony after 25-gauge pars plana vitrectomy with nonexpansile endotamponade. Retina. 2020;40:41–6.
Shimozono M, Oishi A, Kimakura H, et al. Three-step incision for 23-gauge vitrectomy reduces postoperative hypotony compared with an oblique incision. Ophthalmic Surg Lasers Imaging. 2011;42:20–5.
Inoue M, Shinoda K, Shinoda H, et al. Two-step oblique incision during 25-gauge vitrectomy reduces incidence of postoperative hypotony. Clin Exp Ophthalmol. 2007;35:693–6.
Barak Y, Heroman JW, Schaal S. Use of 25% sulfur hexafluoride gas mixture may minimize short-term postoperative hypotony in sutureless 25-gauge pars plana vitrectomy surgery. Clin Ophthalmol (Auckland, NZ). 2013;7:423–6.
Ehlers JP, Dupps WJ, Kaiser PK, et al. The Prospective Intraoperative and Perioperative Ophthalmic ImagiNg with Optical CoherEncE TomogRaphy (PIONEER) study: 2-year results. Am J Ophthalmol. 2014;158:999–1007.
Gregori NZ, Lam BL, Davis JL. Intraoperative use of microscope-integrated optical coherence tomography for subretinal gene therapy delivery. Retina. 2019;39(Suppl 1):S9–s12.
Vasconcelos HM, Lujan BJ, Pennesi ME, et al. Intraoperative optical coherence tomographic findings in patients undergoing subretinal gene therapy surgery. Int J Retina Vitreous. 2020;6:13.
Roizenblatt M, Edwards TL, Gehlbach PL. Robot-assisted vitreoretinal surgery: current perspectives. Robot Surg (Auckland). 2018;5:1–11.
MacLaren R. World first for robot eye operation. https://www.ox.ac.uk/news/2016-09-12-world-first-robot-eye-operation. Accessed July 16, 2020.
Igarashi T, Miyake K, Asakawa N, et al. Direct comparison of administration routes for AAV8-mediated ocular gene therapy. Curr Eye Res. 2013;38:569–77.
Dalkara D, Kolstad KD, Caporale N, et al. Inner limiting membrane barriers to AAV-mediated retinal transduction from the vitreous. Mol Ther. 2009;17:2096–102.
Dalkara D, Byrne LC, Klimczak RR, et al. In vivo-directed evolution of a new adeno-associated virus for therapeutic outer retinal gene delivery from the vitreous. Sci Transl Med. 2013;5:189ra76.
Gamlin PD, Alexander JJ, Boye SL, et al. SubILM injection of AAV for gene delivery to the retina. Methods Mol Biol (Clifton, NJ). 2019;1950:249–62.
Sampat KM, Garg SJ. Complications of intravitreal injections. Curr Opin Ophthalmol. 2010;21:178–83.
Avery RL, Bakri SJ, Blumenkranz MS, et al. Intravitreal injection technique and monitoring: updated guidelines of an expert panel. Retina. 2014;34:S1–S18.
Patel SN, Gangaputra S, Sternberg P Jr, et al. Prophylaxis measures for postinjection endophthalmitis. Surv Ophthalmol. 2020;65:408–20.
Fileta JB, Scott IU, Flynn HW Jr. Meta-analysis of infectious endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents. Ophthalmic Surg Lasers Imaging Retina. 2014;45:143–9.
Lau PE, Jenkins KS, Layton CJ. Current evidence for the prevention of endophthalmitis in anti-VEGF intravitreal injections. J Ophthalmol. 2018;2018:8567912.
Wen JC, McCannel CA, Mochon AB, et al. Bacterial dispersal associated with speech in the setting of intravitreous injections. Arch Ophthalmol. 2011;129:1551–4.
Storey P, Dollin M, Pitcher J, et al. The role of topical antibiotic prophylaxis to prevent endophthalmitis after intravitreal injection. Ophthalmology. 2014;121:283–9.
Grzybowski A, Kanclerz P, Myers WG. The use of povidone-iodine in ophthalmology. Curr Opin Ophthalmol. 2018;29:19–32.
Fineman MS, Hsu J, Spirn MJ, et al. Bimanual assisted eyelid retraction technique for intravitreal injections. Retina. 2013;33:1968–70.
Munro M, Williams GR, Ells A, et al. Lid splinting eyelid retraction technique: a minimised sterile approach for intravitreal injections. Br J Ophthalmol. 2018;102:1254–8.
Tustin A, Kim SJ, Chomsky A, et al. Antibacterial properties of 2% lidocaine and reduced rate of endophthalmitis after intravitreal injection. Retina. 2014;34:935–42.
Storey PP, Tauqeer Z, Yonekawa Y, et al. The impact of prefilled syringes on endophthalmitis following intravitreal injection of ranibizumab. Am J Ophthalmol. 2019;199:200–8.
Levinson JD, Garfinkel RA, Berinstein DM, et al. Timing of povidone-iodine application to reduce the risk of endophthalmitis after intravitreal injections. Ophthalmol Retina. 2018;2:654–8.
Jager RD, Aiello LP, Patel SC, et al. Risks of intravitreous injection: a comprehensive review. Retina. 2004;24:676–98.
Karabag RY, Parlak M, Cetin G, et al. Retinal tears and rhegmatogenous retinal detachment after intravitreal injections: its prevalence and case reports. Dig J Ophthalmol. 2015;21:8.
Knecht PB, Michels S, Sturm V, et al. Tunnelled versus straight intravitreal injection: intraocular pressure changes, vitreous reflux, and patient discomfort. Retina (Philadelphia, Pa). 2009;29:1175–81.
Storey PP, Pancholy M, Wibbelsman TD, et al. Rhegmatogenous retinal detachment after intravitreal injection of anti-vascular endothelial growth factor. Ophthalmology. 2019;126:1424–31.
Yun C, Oh J, Hwang SY, et al. Subconjunctival hemorrhage after intravitreal injection of anti-vascular endothelial growth factor. Graefes Arch Clin Exp Ophthalmol. 2015;253:1465–70.
Lemos V, Cabugueira A, Noronha M, et al. Intraocular pressure in eyes receiving intravitreal antivascular endothelial growth factor injections. Ophthalmologica. 2015;233:162–8.
Frenkel MP, Haji SA, Frenkel RE. Effect of prophylactic intraocular pressure-lowering medication on intraocular pressure spikes after intravitreal injections. Arch Ophthalmol. 2010;128:1523–7.
Yannuzzi NA, Patel SN, Bhavsar KV, et al. Predictors of sustained intraocular pressure elevation in eyes receiving intravitreal anti-vascular endothelial growth factor therapy. Am J Ophthalmol. 2014;158(319–27):e2.
Pang CE, Mrejen S, Hoang QV, et al. Association between needle size, postinjection reflux, and intraocular pressure spikes after intravitreal injections. Retina. 2015;35:1401–6.
Gomez J, Koozekanani DD, Feng AZ, et al. Strategies for improving patient comfort during intravitreal injections: results from a survey-based study. Ophthalmol Ther. 2016;5:183–90.
Chen X, Seth RK, Rao VS, et al. Effects of music therapy on intravitreal injections: a randomized clinical trial. J Ocul Pharmacol Ther. 2012;28:414–9.
Shiroma HF, Takaschima AKK, Farah ME, et al. Patient pain during intravitreal injections under topical anesthesia: a systematic review. Int J Retina Vitreous. 2017;3:23.
Karimi S, Mosavi SA, Jadidi K, et al. Which quadrant is less painful for intravitreal injection? A prospective study. Eye. 2019;33:304–12.
Popovic MM, Muni RH, Nichani P, et al. Topical nonsteroidal anti-inflammatory drugs for pain resulting from intravitreal injections: a meta-analysis. Ophthalmol Retina. 2020;4:461–70.
Li Q, Miller R, Han P-Y, et al. Intraocular route of AAV2 vector administration defines humoral immune response and therapeutic potential. Mol Vis. 2008;14:1760–9.
Wan X, Pei H, Zhao M-J, et al. Efficacy and safety of rAAV2-ND4 treatment for Leber’s hereditary optic neuropathy. Sci Rep. 2016;6:21587.
Kansara V, Muya L, Wan CR, et al. Suprachoroidal delivery of viral and nonviral gene therapy for retinal diseases. J Ocul Pharmacol Ther. 2020;36:384–92.
Patel SR, Berezovsky DE, McCarey BE, et al. Targeted administration into the suprachoroidal space using a microneedle for drug delivery to the posterior segment of the eye. Invest Ophthalmol Vis Sci. 2012;53:4433–41.
Yiu G, Chung SH, Mollhoff IN, et al. Suprachoroidal and subretinal injections of AAV using transscleral microneedles for retinal gene delivery in nonhuman primates. Mol Ther Methods Clin Dev. 2020;16:179–91.
Yeh S, Kurup SK, Wang RC, et al. Suprachoroidal injection of triamcinolone acetonide, CLS-TA, for macular edema due to noninfectious uveitis: a randomized, phase 2 study (DOGWOOD). RETINA. 2019;39:1880–8.
Del Amo EM, Rimpela AK, Heikkinen E, et al. Pharmacokinetic aspects of retinal drug delivery. Prog Retin Eye Res. 2017;57:134–85.
Boye SE, Alexander JJ, Witherspoon CD, et al. Highly efficient delivery of adeno-associated viral vectors to the primate retina. Hum Gene Ther. 2016;27:580–97.
Redmond TM, Yu S, Lee E, et al. Rpe65 is necessary for production of 11-cis-vitamin A in the retinal visual cycle. Nat Genet. 1998;20:344–51.
Maguire AM, Simonelli F, Pierce EA, et al. Safety and efficacy of gene transfer for Leber's congenital amaurosis. N Engl J Med. 2008;358:2240–8.
Maguire AM, High KA, Auricchio A, et al. Age-dependent effects of RPE65 gene therapy for Leber's congenital amaurosis: a phase 1 dose-escalation trial. Lancet. 2009;374:1597–605.
Bennett J, Wellman J, Marshall KA, et al. Safety and durability of effect of contralateral-eye administration of AAV2 gene therapy in patients with childhood-onset blindness caused by RPE65 mutations: a follow-on phase 1 trial. Lancet (London, England). 2016;388:661–72.
Russell S, Bennett J, Wellman JA, et al. Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial. Lancet. 2017;390:849–60.
Maguire AM, Russell S, Wellman JA, et al. Efficacy, safety, and durability of voretigene neparvovec-rzyl in RPE65 mutation–associated inherited retinal dystrophy: results of phase 1 and 3 trials. Ophthalmology. 2019;126:1273–85.
Pennesi ME, Weleber RG, Yang P, et al. Results at 5 years after gene therapy for RPE65-deficient retinal dystrophy. Hum Gene Ther. 2018;29:1428–37.
Bainbridge JWB, Mehat MS, Sundaram V, et al. Long-term effect of gene therapy on Leber's congenital amaurosis. N Engl J Med. 2015;372:1887–97.
Testa F, Maguire AM, Rossi S, et al. Three-year follow-up after unilateral subretinal delivery of adeno-associated virus in patients with Leber congenital amaurosis type 2. Ophthalmology. 2013;120:1283–91.
Le Meur G, Lebranchu P, Billaud F, et al. Safety and long-term efficacy of AAV4 gene therapy in patients with RPE65 Leber congenital amaurosis. Mol Ther. 2018;26:256–68.
Wang X, Yu C, Tzekov RT, et al. The effect of human gene therapy for RPE65-associated Leber's congenital amaurosis on visual function: a systematic review and meta-analysis. Orphanet J Rare Dis. 2020;15:49.
Seabra M, Brown M, Goldstein J. Retinal degeneration in choroideremia: deficiency of Rab geranylgeranyl transferase. Science. 1993;259:377–81.
Xue K, Jolly JK, Barnard AR, et al. Beneficial effects on vision in patients undergoing retinal gene therapy for choroideremia. Nat Med. 2018;24:1507–12.
Dimopoulos IS, Hoang SC, Radziwon A, et al. Two-year results after AAV2-mediated gene therapy for choroideremia: the Alberta experience. Am J Ophthalmol. 2018;193:130–42.
Lam BL, Davis JL, Gregori NZ, et al. Choroideremia gene therapy phase 2 clinical trial: 24-month results. Am J Ophthalmol. 2019;197:65–73.
MacDonald IM, Moen C, Duncan JL, et al. Perspectives on gene therapy: choroideremia represents a challenging model for the treatment of other inherited retinal degenerations. Transl Vis Sci Technol. 2020;9:17.
Fischer MD, Ochakovski GA, Beier B, et al. Efficacy and safety of retinal gene therapy using adeno-associated virus vector for patients with choroideremia: a randomized clinical trial. JAMA Ophthalmol. 2019;137:1247–54.
Rotenstreich Y, Fishman GA, Anderson RJ. Visual acuity loss and clinical observations in a large series of patients with Stargardt disease. Ophthalmology. 2003;110:1151–8.
Allikmets R, Singh N, Sun H, et al. A photoreceptor cell-specific ATP-binding transporter gene (ABCR) is mutated in recessive Stargardt macular dystrophy. Nat Genet. 1997;15:236–46.
McClements ME, Barnard AR, Singh MS, et al. An AAV dual vector strategy ameliorates the Stargardt phenotype in adult Abca4−/− mice. Hum Gene Ther. 2019;30:590–600.
Han Z, Han Z, Conley SM, et al. DNA nanoparticle-mediated ABCA4 delivery rescues Stargardt dystrophy in mice. J Clin Investig. 2012;122:3221–6.
Sun D, Schur RM, Sears AE, et al. Non-viral gene therapy for Stargardt disease with ECO/pRHO-ABCA4 self-assembled nanoparticles. Mol Ther. 2020;28:293–303.
Wilson DJ, Sahel JA, Weleber RG, et al. One year results of a phase I/IIa study of SAR422459 in patients with Stargardt macular degeneration (SMD). Investig Ophthalmol Vis Sci. 2017;58:3385.
Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. Lancet. 2006;368:1795–809.
Feng W, Yasumura D, Matthes MT, et al. Mertk triggers uptake of photoreceptor outer segments during phagocytosis by cultured retinal pigment epithelial cells. J Biol Chem. 2002;277:17016–22.
Ghazi NG, Abboud EB, Nowilaty SR, et al. Treatment of retinitis pigmentosa due to MERTK mutations by ocular subretinal injection of adeno-associated virus gene vector: results of a phase I trial. Hum Genet. 2016;135:327–43.
Talib M, van Schooneveld MJ, Thiadens AA, et al. Clinical and genetic characteristics of male patients with rpgr-associated retinal dystrophies: a long-term follow-up study. Retina. 2019;39:1186–99.
Wu Z, Hiriyanna S, Qian H, et al. A long-term efficacy study of gene replacement therapy for RPGR-associated retinal degeneration. Hum Mol Genet. 2015;24:3956–70.
Cehajic-Kapetanovic J, Xue K, Martinez-Fernandez de la Camara C, et al. Initial results from a first-in-human gene therapy trial on X-linked retinitis pigmentosa caused by mutations in RPGR. Nat Med. 2020;26:354–9.
Michaelides M, Hunt DM, Moore AT. The cone dysfunction syndromes. Br J Ophthalmol. 2004;88:291–7.
Hirji N, Aboshiha J, Georgiou M, et al. Achromatopsia: clinical features, molecular genetics, animal models and therapeutic options. Ophthalmic Genet. 2018;39:149–57.
Fischer MD, Michalakis S, Wilhelm B, et al. Safety and vision outcomes of subretinal gene therapy targeting cone photoreceptors in achromatopsia: a nonrandomized controlled trial. JAMA Ophthalmol. 2020;138:643–51.
Yu-Wai-Man P, Griffiths PG, Brown DT, et al. The epidemiology of Leber hereditary optic neuropathy in the North East of England. Am J Hum Genet. 2003;72:333–9.
Yu-Wai-Man P, Turnbull DM, Chinnery PF. Leber hereditary optic neuropathy. J Med Genet. 2002;39:162–9.
Yuan J, Zhang Y, Liu H, et al. Seven-year follow-up of gene therapy for leber’s hereditary optic neuropathy. Ophthalmology. 2020;127:1125–7.
Guy J, Feuer WJ, Davis JL, et al. Gene therapy for Leber hereditary optic neuropathy: low- and medium-dose visual results. Ophthalmology. 2017;124:1621–34.
Vignal C, Uretsky S, Fitoussi S, et al. Safety of rAAV2/2-ND4 gene therapy for Leber hereditary optic neuropathy. Ophthalmology. 2018;125:945–7.
Bouquet C, Vignal Clermont C, Galy A, et al. Immune response and intraocular inflammation in patients with leber hereditary optic neuropathy treated with intravitreal injection of recombinant adeno-associated virus 2 carrying the ND4 gene: a secondary analysis of a phase 1/2 clinical trial. JAMA Ophthalmol. 2019;137:399–406.
GenSight. GenSight Biologics reports sustained efficacy and safety at 96 weeks in RESCUE Phase III clinical trial of GS010 for the treatment of Leber Hereditary Optic Neuropathy (LHON). Accessed Sept 23, 2019.
GenSight. Sustained bilateral improvement from GenSight Biologics' REVERSE Phase III clinical trial represents transformative therapeutic benefit for patients, Key Opinion Leaders conclude. Accessed June 15, 2020.
Pimenides D, George ND, Yates JR, et al. X-linked retinoschisis: clinical phenotype and RS1 genotype in 86 UK patients. J Med Genet. 2005;42:e35.
Molday RS, Kellner U, Weber BH. X-linked juvenile retinoschisis: clinical diagnosis, genetic analysis, and molecular mechanisms. Prog Retinal eye Res. 2012;31:195–21212.
Vijayasarathy C, Sui R, Zeng Y, et al. Molecular mechanisms leading to null-protein product from retinoschisin (RS1) signal-sequence mutants in X-linked retinoschisis (XLRS) disease. Hum Mutat. 2010;31:1251–60.
Cukras C, Wiley HE, Jeffrey BG, et al. Retinal AAV8-RS1 gene therapy for X-linked retinoschisis: initial findings from a phase I/IIa trial by intravitreal delivery. Mol Ther. 2018;26:2282–94.
Acknowledgements
Funding
This work was supported by the Jonas Children’s Vision Care and Bernard & Shirlee Brown Glaucoma Laboratory, the National Institutes of Health [P30EY019007, R01EY018213, R01EY024698, R01EY026682, R21AG050437], National Cancer Institute Core [5P30CA013696], Foundation Fighting Blindness [TA-NMT-0116-0692-COLU], New York State [SDHDOH01-C32590GG-3450000], the Research to Prevent Blindness (RPB) Physician-Scientist Award, and unrestricted funds from RPB, New York, NY, USA. S.H.T. is a member of the RD-CURE Consortium and is supported by Kobi and Nancy Karp, the Crowley Family Fund, the Alcon Research Institute, the Rosenbaum Family Foundation, the Tistou and Charlotte Kerstan Foundation, the Schneeweiss Stem Cell Fund, and the Gebroe Family Foundation. No funding or sponsorship was received for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Yan Nuzbrokh, Alexis S. Kassotis, Sara D. Ragi, Ruben Jauregui and Stephen H. Tsang declare they have no conflicts of interest.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12709016.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/ .
About this article
Cite this article
Nuzbrokh, Y., Kassotis, A.S., Ragi, S.D. et al. Treatment-Emergent Adverse Events in Gene Therapy Trials for Inherited Retinal Diseases: A Narrative Review. Ophthalmol Ther 9, 709–724 (2020). https://doi.org/10.1007/s40123-020-00287-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-020-00287-1