Abstract
Purpose
To qualitatively evaluate the ocular and periocular distribution of 14C-latanoprost following a single intracameral administration or repeated topical ocular administration in beagle dogs and cynomolgus monkeys.
Methods
In the dog study, three animals received an intracameral dose of 14C-latanoprost bilaterally and were euthanized at 1, 2, and 4 h post dose; three control animals received topical 14C-latanoprost bilaterally once daily for 5 days and were euthanized at 1, 4, and 24 h post final dose. Sagittal 40-µm sections of eyes with surrounding tissues were collected and processed for autoradiography. Methods in the monkey study were similar; two animals received a unilateral intracameral dose of 14C-latanoprost.
Results
After intracameral dosing in dogs, radioactivity was concentrated in the cornea, iris, ciliary body, and anterior chamber with no radioactivity detected in the eyelids or other periorbital tissues. After topical dosing, radioactivity was distributed in the bulbar conjunctiva, cornea, anterior chamber, iris, ciliary body, upper and lower eyelids, and periorbital tissues (fat/muscle). After intracameral dosing in monkeys, radioactivity was concentrated in the anterior chamber, cornea, iris, ciliary body, and posteriorly along the uveoscleral outflow pathway; there was no radioactivity in the eyelids or periorbital tissues aside from signal in the nasolacrimal duct, likely from reflux of 14C-latanoprost into the tear film.
Conclusions
Intracameral delivery resulted in more selective target tissue drug exposure. Intracameral drug delivery has potential to reduce ocular surface and periocular adverse effects associated with topical administration of prostaglandin analogues, such as eyelash growth and periorbital fat atrophy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Topical administration is the most common mode of drug delivery for PGAs and other IOP-lowering medications, but poor adherence of patients to topical ocular hypotensive regimens is endemic. |
Intracameral administration may be useful for delivery of PGAs to target tissues for IOP lowering in patients with glaucoma and ocular hypertension. |
The objective of this study was to determine the ocular distribution of 14C-latanoprost following a single intracameral administration or repeated topical ocular administration to beagle dogs and cynomolgus monkeys. |
The results of these studies in dogs and monkeys demonstrate that intracameral PGA dosing delivers drug more selectively to intraocular target tissues compared with topical PGA dosing. |
Intracameral PGA dosing can achieve targeted drug delivery because it bypasses the anatomic and precorneal barriers to drug penetration encountered by topical administration. |
Delivery of PGA by intracameral injection may reduce the potential for side effects associated with topical PGA treatment by limiting PGA distribution to the conjunctiva, eyelids, and periocular tissues. |
Introduction
Topical prostaglandin analogue (PGA) medications including latanoprost, tafluprost, travoprost, and the prostamide bimatoprost are widely used as first-line therapy for lowering intraocular pressure (IOP) in patients with open-angle glaucoma (OAG) and ocular hypertension (OHT) [1]. These medications are well tolerated, systemically safe, and highly efficacious in lowering IOP [1,2,3]. The PGAs typically are administered by instillation of an eye drop once daily.
Topical administration is the most common mode of drug delivery for PGAs and other IOP-lowering medications, but poor adherence of patients to topical ocular hypotensive regimens is endemic [4,5]. Inconvenience, forgetfulness, difficulty in instilling eye drops, the frequency of required dosing, medication cost, and side effects are commonly reported reasons for patient nonadherence to IOP-lowering eye drops [6,7,8]. Furthermore, precorneal factors (tear film, tear turnover, blinking, lacrimal drainage, and induced lacrimation) as well as anatomical barriers (the cornea, conjunctiva, and sclera) limit the delivery of drugs applied topically to the eye to intraocular target tissues [9]. Drug that does not penetrate the eye has the potential to cause ocular surface and periocular side effects, and conjunctival hyperemia, eyelash growth, and iris, eyelid, and periocular skin pigmentation are common side effects of topical PGA treatment [10]. Prostaglandin-associated periorbitopathy (PAP), most likely resulting from periorbital fat atrophy [11], is now also recognized as a side effect of topical PGA treatment [12]. Clinical signs of PAP associated with chronic topical PGA treatment include deepening of the upper eyelid sulcus, enophthalmos, flattening of the lower eyelid bags, and inferior scleral show [13,14].
Intracameral administration of antibiotics and mydriatics is used routinely during cataract surgery [15,16,17], and this route of drug administration may also be useful for delivery of PGAs to target tissues for IOP lowering in patients with glaucoma and OHT. Intracameral injection of PGAs can potentially deliver drug to target intraocular tissues more efficiently than topical dosing and minimize side effects associated with topical PGA treatment by limiting drug exposure to the ocular surface and periocular tissues [18]. Studies in animal models have shown that an intracameral implant delivering bimatoprost [19,20,21] or another ocular hypotensive medication [22,23,24] including a latanoprost analogue [25] can effectively reduce IOP. The intracameral sustained-release bimatoprost implant (Durysta™) has demonstrated efficacy and tolerability in patients with glaucoma [26] and is now approved by the US Food and Drug Administration for the treatment of OAG or OHT.
Drug distribution after administration can be expected to affect the IOP-lowering efficacy and safety of a PGA delivered intracamerally. The objective of this study was to determine the ocular distribution of 14C-latanoprost following a single intracameral administration or repeated topical ocular administration to beagle dogs and cynomolgus monkeys.
Methods
Animals
All animals were normal on ophthalmic examination. Animals were housed under controlled conditions and received a certified canine or primate diet and water ad libitum. The studies were conducted at Covance Laboratories Inc (Madison, WI, USA) in accordance with the Association for Research in Vision and Ophthalmology (ARVO) statement for the Use of Animals in Ophthalmic and Vision Research. All study procedures were performed in compliance with US Animal Welfare Act regulations.
Methods for Dog Study
Six male purebred treatment-naïve beagle dogs (Covance Research Products, Cumberland, VA or Covance Stock Colony), ages 6–7 months, weighing 9.7–12.1 kg, were used in the study.
Drug
The test compound was 14C-latanoprost (178 mCi/mmol, 98.5% radiopurity). For intracameral injections, on the day of dosing, 30 µL of 14C-latanoprost was dried under a stream of nitrogen and solubilized in 300 µL of vehicle containing 1% polysorbate 80, 0.75% sodium chloride, 0.16% sodium dihydrogen phosphate monohydrate, 0.22% disodium hydrogen phosphate anhydrous, and sterile water. For topical dosing, 14C-latanoprost was prepared in the same vehicle with the addition of 0.02% benzalkonium chloride. On the first day of topical dosing, 48.8 µL of 14C-latanoprost was dried under a stream of nitrogen and solubilized in 2.4 mL of vehicle containing benzalkonium chloride. Aliquots of the solution were frozen at − 20 °C for use on the next 4 days. Drug stability was demonstrated by high-performance liquid chromatography.
Drug Administration
Animals were assigned to two study groups (n = 3 per group). Group 1 received a single bilateral intracameral dose of 14C-latanoprost, and group 2 received a bilateral topical dose of 14C-latanoprost once daily for 5 days. A similar topical dosing regimen of latanoprost has been shown to achieve steady state IOP lowering in glaucomatous beagle dogs [27]. The doses of latanoprost and radioactivity administered to the animals in each group are shown in Table 1.
Animals in the intracameral dosing group were anesthetized with a regimen of oxymorphone, glycopyrrolate, and midazolam, followed by dexmedetomidine. A topical anesthetic was applied to the eyes, and the eyes were then rinsed with an iodine solution followed by a saline rinse. A bilateral dose of 14C-latanoprost was administered intracamerally by a board-certified veterinary ophthalmologist using a syringe and needle. For each administration, the eye was stabilized by grasping the conjunctiva with a fixation forceps, the needle was tunneled through the cornea near the limbus and advanced several millimeters toward the center of the anterior chamber, and a 10-µL dose was injected.
Animals in the topical dosing group received a topical 30-µL dose in both eyes once daily for 5 days at the same time each day. The dose was administered onto the cornea of the eye via a micropipette. After the dose was administered, the upper and lower eyelids were held together gently to distribute the dose across the eye.
Sample Collection
Animals were euthanized with sodium pentobarbital at designated time points after drug administration. The three animals that received intracameral 14C-latanoprost were euthanized at 1, 2, and 4 h after dosing; the three animals that received topical 14C-latanoprost were euthanized at 1, 4, and 24 h after the last dose. Following euthanasia, the animals were exsanguinated, the head was shaved, and the eyelids on both eyes were sutured open such that the palpebral conjunctiva were visible and outward facing. Left eyes were enucleated, trimmed of excess tissue, rinsed with saline, blotted dry, and flash-frozen in liquid nitrogen for 15–20 s before storage at − 20 °C. Right eyes were kept in situ following euthanasia to ensure that periorbital tissues would be preserved for imaging drug distribution. Right eyes with surrounding structures were removed and frozen in a hexane/dry ice bath for 30–120 min, blotted dry, placed on dry ice or stored at − 70 °C for at least 12 h, stored at − 20 °C, and then were shipped on dry ice to QPS, LLC (Newark, DE, USA) for autoradiography.
The clinical dosing regimen for latanoprost eye drops is once-daily administration, and ocular samples from animals assigned to the group receiving 5 days of once-daily topical administration were collected at 1, 4, and 24 h post final dose to cover the entire dosing interval. The timing of tissue sampling after intracameral delivery differed because aqueous humor outflow in normal beagle dogs is estimated to be 4–6 µL/min [28], and with an estimated anterior chamber volume of 0.4–0.77 mL [28], the entire volume of aqueous humor is expected to be turned over within 3 h. Therefore, ocular samples from animals assigned to the intracameral dose group were collected at 1, 2, and 4 h post dose.
Autoradiography
Frozen samples containing right eyes and surrounding structures in situ were embedded in 2% carboxymethylcellulose, frozen into blocks, and sectioned on a cryomicrotome at − 20 °C. An aliquot of blood containing 14C was injected into each block before sectioning as a marker to aid in the alignment of sections with autoradiographs. Serial 40-μm sections were taken in the sagittal plane at intervals of 0.5 mm through half of each eye (for eyes that had received intracameral 14C-latanoprost administration, the half of the eye that included the injection site). Sections were selected that included the following areas/structures to be analyzed: ciliary body, lens, anterior and posterior chambers, sclera, anterior and posterior uvea, iris, cornea, and bulbar and palpebral conjunctiva. The sections were collected on adhesive tape (Scotch 8210; 3M, Maplewood, MN, USA) and were air-dried in the cryomicrotome for at least 48 h, then were mounted on a cardboard backing and wrapped with a thin plastic wrap to avoid contamination of the imaging plate.
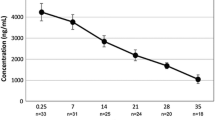
The sections and calibration standards at 10 different concentrations (0.0003–5.3825 μCi/g) were then exposed to a 14C-sensitive phosphor imaging plate (Fuji Biomedical, Stamford, CT) in light-tight cassettes for 4 days at room temperature. Quantification was performed by image densitometry; a standard curve was constructed from nominal concentrations of 14C-calibration standards. Concentrations of radioactivity were expressed as microcuries per gram (μCi/g) and converted to microgram equivalents of 14C-latanoprost per gram sample (μg equiv/g). The lower limit of quantitation was 0.830 ng equiv/g.
Methods for Monkey Study
Two female drug-naïve cynomolgus monkeys (Covance Research Products, Cumberland, VA or Covance Stock Colony), ages 3–4 years, weighing 2.7–3.4 kg, were used in the study.
Drug and Drug Administration
For intracameral injections, the test compound and procedures used were similar to those described above for the dog study. A 204-µL aliquot of 14C-latanoprost was dried and solubilized in 2.00 mL of vehicle. Two monkeys were anesthetized with a regimen of ketamine, glycopyrrolate, and dexmedetomidine. After application of a topical anesthetic to both eyes, the eyes were rinsed with an iodine solution followed by a saline rinse, and finally, additional drops of topical anesthetic were applied. A 10-µL dose of 14C-latanoprost was administered intracamerally, to the right eye only, by a board-certified veterinary ophthalmologist using a syringe and needle, with the same procedure as described above in dogs.
Sample Collection and Autoradiography
Monkeys were euthanized with an overdose of sodium pentobarbital and exsanguination at 0.5 and 4 h post intracameral dose. Following euthanasia, both eyes were rinsed with saline, and the eyelids were sutured open. The head was removed from the body with the eyes in situ and was frozen in a hexane/dry ice bath for 15 min, then was drained, dried, placed in a labeled bag, and stored at − 70 °C for at least 12 h. The head was then embedded in chilled carboxymethylcellulose, frozen into a block, and stored at − 20 °C in preparation for autoradiographic analysis. Standards fortified with 14C radioactivity were placed into the frozen block and used for monitoring the uniformity of section thickness.
Serial cross sections, collected up to 43 levels using the initial injection site as a reference, were collected on adhesive tape at 20-µm thickness using a Leica CM 3600 cryomicrotome. Sections were dried at − 20 °C. A representative section from each level of interest was mounted, tightly wrapped with plastic film, and exposed on a phosphor imaging screen with standards for calibration of the imaging analysis software. Screens were exposed for 7 days and scanned using the Storm system (Amersham Biosciences, Sunnyvale, CA, USA). InterFocus Imaging Ltd (Cambridge, England) MCID™ Analysis software was used to create a calibrated standard curve and determine tissue concentrations, which were interpolated from each standard curve as nanocuries per gram and converted to µg equiv/g. The lower limit of quantitation was 2.36 ng equiv/g.
Three-Dimensional (3D) Rendering
The autoradiography images were rendered into 3D images/movies. A customized methodology was developed by the Moats Laboratory at The Saban Research Institute of Children’s Hospital Los Angeles to accomplish the segmentation and alignment of the autoradiography images. The pre-processed stack images were exported to Amira Software (Thermo Fisher Scientific, Waltham, MA, USA) for 3D rendering to visualize the monkey images.
Results
Dog Study
All animals appeared healthy after dosing. Both the intracameral and topical ocular doses of 14C-latanoprost were well tolerated with no effects observed other than transient hyperemia.
Figure 1 shows representative sections and autoradiographs from in situ eyes of animals that received five daily topical doses of 14C-latanoprost. Radioactivity appeared to be diffusely distributed throughout the anterior portion of the eye at 1, 4, and 24 h after the last dose. Radioactivity was present in the bulbar conjunctiva, cornea, anterior chamber, iris, ciliary body, upper and lower eyelids, and periorbital tissues (fat and muscle) after topical administration (Fig. 1).
Representative sections of fresh-frozen eyes in situ (right) and corresponding autoradiographs (left) from beagle dogs that received five daily topical ophthalmic bilateral administrations of 14C-latanoprost. Eyes in situ were collected at 1 and 4 h after the last administration. Annotations identify tissues and areas of interest
Representative sections and autoradiographs from in situ eyes of animals that received a single intracameral dose of 14C-latanoprost are shown in Fig. 2. Radioactivity was concentrated in ocular tissues including the cornea, iris, ciliary body, and anterior chamber after intracameral dosing. There was a diminution of signal in the anterior segment from 1 to 4 h post intracameral dose. No radioactivity was detected in the eyelids or other periorbital tissues after intracameral dosing.
Representative sections of fresh-frozen eyes in situ (right) and corresponding autoradiographs (left) from beagle dogs that received a single bilateral intracameral administration of 14C-latanoprost. Eyes in situ were collected at 1, 2, and 4 h after the administration. Annotations identify tissues and areas of interest
Radioactivity in anterior uvea and sclera was detected only sporadically on autoradiography with both dosing routes. Distribution of radioactivity to the posterior eye, including the retina, was negligible after both topical and intracameral dosing.
Monkey Study
The 3D reconstruction of autoradiographs from sections taken at 0.5 h post single intracameral dose showed that radioactivity was concentrated in the anterior chamber, cornea, iris, and cilary body of the dosed eye (Fig. 3a). Radioactivity was also present in the uveoscleral outflow pathway, and in larger drainage pathways such as the superior ophthalmic vein (Fig. 3a). Some radioactivity was located in the nasolacrimal duct and nasal turbinates, and likely resulted from reflux of some of the injected dose into the tear film. However, no radioactivity was detected in the eyelids or other periorbital tissues. In the reconstruction of autoradiographs from sections taken at 4 h after the intracameral dose, radioactivity was concentrated in the anterior chamber of the dosed eye with less intensity compared with 0.5 h. Radioactivity was absent from the eyelids and periorbital tissues (Fig. 3b).
Images of 3D reconstructions of the distribution of radioactivity in cynomolgus monkeys at a 0.5 h and b 4 h after a single intracameral administration of 14C-latanoprost. Phosphor imaging autoradiographs of cross sections of the animal heads were used to develop the 3D reconstructions. 3D 3-dimensional, arrow nasolacrimal duct, arrowhead superior ophthalmic vein, asterisk anterior chamber
The full 3D reconstructions of the distribution of radioactivity at 0.5 h and 4 h after the intracameral dose are shown in Supplementary Video 1 and Supplementary Video 2, respectively.
Supplementary Video 1. Video of the 3D reconstruction of the distribution of radioactivity in a cynomolgus monkey at 0.5 h after a single intracameral administration of 14C-latanoprost. 3D = 3-dimensional (MP4 7598 kb)
Supplementary Video 2. Video of the 3D reconstruction of the distribution of radioactivity in a cynomolgus monkey at 4 h after a single intracameral administration of 14C-latanoprost. 3D = 3-dimensional (MP4 4928 kb)
Discussion
Autoradiography was used in this study to qualitatively evaluate the distribution and concentration of radioactivity in dog eyes that were administered 14C-latanoprost by a single intracameral injection or daily topical instillation. After the intracameral dose, radioactivity was concentrated in the cornea, iris, ciliary body, bulbar conjunctiva, and anterior chamber, whereas after 5 days of topical dosing, radioactivity was concentrated in the cornea and bulbar conjunctiva, and was distributed more diffusely in other anterior ocular tissues. Radioactivity in the eyelids and periorbital tissue was detected only after topical dosing. Data in the monkey study were confirmatory with no signal detected in the eyelids or orbit after intracameral administration of 14C-latanoprost.
The eyes of beagle dogs are similar to human eyes in anatomic and physiologic characteristics [28], and therefore, the beagle dog is a useful model for the evaluation of ocular drug distribution. Drug distribution to the ciliary body is important for the PGA class of topical ocular hypotensive medications, because these drugs decrease IOP by increasing uveoscleral outflow [29]. As the mechanism of action of topical PGAs may also involve an increase in aqueous outflow through the conventional pathway [29], distribution of drug to the anterior chamber adjacent to the trabecular meshwork is also relevant. The distribution of radioactivity seen in this study after intracameral and topical administration of 14C-latanoprost to dogs shows that intracameral dosing can more selectively deliver PGA to target tissues for IOP lowering. Furthermore, the absence of radioactivity detected in the eyelids and periorbital tissues after intracameral dosing suggests that intracameral administration may be associated with a reduced incidence of some side effects associated with topical administration of PGAs, such as eyelash changes and PAP.
The delivery of therapeutic agents via topical administration may be influenced by the use of accompanying procedures such as punctal occlusion or eyelid closure, which could help increase the concentration and duration of stay of an agent in the anterior chamber and reduce either systemic or off-target exposure [30]. In the present dog study, the upper and lower eyelids of each treated eye were gently held together to distribute the dose across the eye and implement a form of eyelid closure after topical administration of the test compound. The marked presence of radioactivity in the eyelids and periocular tissues with these measures might reinforce the finding that intracameral delivery yields favorable localization of therapeutic agents compared with topical administration.
Although dogs are useful models for the evaluation of ocular drug distribution, their aqueous outflow systems differ from those in humans. In contrast, the orbital anatomy of cynomolgus monkeys and humans is very similar [31], and the aqueous drainage apparatus in cynomolgus monkeys is anatomically similar to that in humans [32]. To confirm that intracameral administration has a greater targeted tissue effect, cynomolgus monkeys were also used. As results from a previous study showed that drug is present in the eyelids of monkeys after topical PGA administration [33], we decided to only use intracameral administration in monkeys for this study. The results from the 3D rendition of the autoradiography in the monkey were very similar to the autoradiography results in the beagle dog. After intracameral administration, drug exposure was mainly limited to the anterior segment (the anterior chamber, cornea, iris, and ciliary body), as well as posterior drainage vessels, which was expected as the aqueous drains through the uveoscleral pathway and episcleral veins. Importantly, there was no eyelid or orbit exposure. These results indicate that there is a localized distribution of radioactivity when 14C-latanoprost is administered intracamerally.
The results of our study are consistent with those of the recently reported drug distribution study of the intracameral sustained-release bimatoprost implant in beagle dogs [18]. In the bimatoprost implant study, the maximal concentration of bimatoprost in the iris-ciliary body was 4 log units higher after implant (15 µg bimatoprost) administration than after 7 days of once-daily topical administration of bimatoprost 0.03% [18]. In another study in beagle dogs, the intracameral bimatoprost implant was shown to cause selective dilation of episcleral aqueous outflow vessels [19], in contrast to the generalized vasodilation that causes ocular surface hyperemia after topical PGA administration in dogs [34], consistent with the suggestion that intracameral PGA dosing may be associated with reduced occurrence of ocular surface and periocular side effects.
An advantage of the use of autoradiography in this study is that drug distribution could be evaluated more precisely in discrete tissues compared with drug distribution studies using isolated tissues. Radioactivity distribution in tissues including the eyelids and periorbital tissues was evaluated qualitatively. A limitation of the use of autoradiography to evaluate drug distribution in the present study is that the molecular identity of the radioactivity present in tissue sections (i.e., latanoprost, latanoprost acid, or other metabolite) could not be determined.
Conclusion
The results of these studies in dogs and monkeys demonstrate that intracameral PGA dosing delivers drug more selectively to intraocular target tissues compared with topical PGA dosing. Intracameral PGA dosing can achieve targeted drug delivery because it bypasses the anatomic and precorneal barriers to drug penetration encountered by topical administration. Delivery of PGA by intracameral injection may reduce the potential for side effects associated with topical PGA treatment by limiting PGA distribution to the conjunctiva, eyelids, and periocular tissues.
References
Eyawo O, Nachega J, Lefebvre P, et al. Efficacy and safety of prostaglandin analogues in patients with predominantly primary open-angle glaucoma or ocular hypertension: a meta-analysis. Clin Ophthalmol. 2009;3:447–56.
Inoue K. Managing adverse effects of glaucoma medications. Clin Ophthalmol. 2014;8:903–13.
Aptel F, Denis P. Balancing efficacy and tolerability of prostaglandin analogues and prostaglandin-timolol fixed combinations in primary open-angle glaucoma. Curr Med Res Opin. 2011;27:1949–58.
Olthoff CM, Schouten JS, van de Borne BW, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005;112:953–61.
Yeaw J, Benner JS, Walt JG, Sian S, Smith DB. Comparing adherence and persistence across 6 chronic medication classes. J Manag Care Pharm. 2009;15:728–40.
Mansouri K, Iliev ME, Rohrer K, Shaarawy T. Compliance and knowledge about glaucoma in patients at tertiary glaucoma units. Int Ophthalmol. 2011;31:369–76.
Dreer LE, Girkin CA, Campbell L, Wood A, Gao L, Owsley C. Glaucoma medication adherence among African Americans: program development. Optom Vis Sci. 2013;90:883–97.
Newman-Casey PA, Robin AL, Blachley T, et al. The most common barriers to glaucoma medication adherence: a cross-sectional survey. Ophthalmology. 2015;122:1308–16.
Gaudana R, Ananthula HK, Parenky A, Mitra AK. Ocular drug delivery. AAPS J. 2010;12:348–60.
Alm A, Grierson I, Shields MB. Side effects associated with prostaglandin analog therapy. Surv Ophthalmol. 2008;53(Suppl 1):S93–105.
Jayaprakasam A, Ghazi-Nouri S. Periorbital fat atrophy—an unfamiliar side effect of prostaglandin analogues. Orbit. 2010;29:357–9.
Di Staso S, Agnifili L, Cecannecchia S, Di Gregorio A, Ciancaglini M. In vivo analysis of prostaglandins-induced ocular surface and periocular adnexa modifications in patients with glaucoma. In Vivo. 2018;32:211–20.
Filippopoulos T, Paula JS, Torun N, Hatton MP, Pasquale LR, Grosskreutz CL. Periorbital changes associated with topical bimatoprost. Ophthalmic Plast Reconstr Surg. 2008;24:302–7.
Nakakura S, Yamamoto M, Terao E, et al. Prostaglandin-associated periorbitopathy in latanoprost users. Clin Ophthalmol. 2015;9:51–6.
Bowen RC, Zhou AX, Bondalapati S, et al. Comparative analysis of the safety and efficacy of intracameral cefuroxime, moxifloxacin and vancomycin at the end of cataract surgery: a meta-analysis. Br J Ophthalmol. 2018;102:1268–76.
Vazquez-Ferreiro P, Carrera-Hueso FJ, Barreiro-Rodriguez L, et al. Effectiveness of intracameral phenylephrine in achieving mydriasis and reducing complications during phacoemulsification: a systematic review and meta-analysis. J Ocul Pharmacol Ther. 2017;33:735–42.
Brandsdorfer A, Patel SH, Chuck RS. The role of perioperative nonsteroidal anti-inflammatory drugs use in cataract surgery. Curr Opin Ophthalmol. 2019;30:44–9.
Seal JR, Robinson MR, Burke J, Bejanian M, Coote M, Attar M. Intracameral sustained-release bimatoprost implant delivers bimatoprost to target tissues with reduced drug exposure to off-target tissues. J Ocul Pharmacol Ther. 2019;35:50–7.
Lee SS, Burke J, Shen J, et al. Bimatoprost sustained-release intracameral implant reduces episcleral venous pressure in dogs. Vet Ophthalmol. 2018;21:376–81.
Lee SS, Almazan A, Decker S, et al. Intraocular pressure effects and mechanism of action of topical versus sustained-release bimatoprost. Transl Vis Sci Technol. 2019;8:15.
Lee SS, Dibas M, Almazan A, Robinson MR. Dose-response of intracameral bimatoprost sustained-release implant and topical bimatoprost in lowering intraocular pressure. J Ocul Pharmacol Ther. 2019;35:138–44.
Chou SF, Luo LJ, Lai JY, Ma DH. On the importance of Bloom number of gelatin to the development of biodegradable in situ gelling copolymers for intracameral drug delivery. Int J Pharm. 2016;511:30–43.
Lai JY, Luo LJ. Chitosan-g-poly(N-isopropylacrylamide) copolymers as delivery carriers for intracameral pilocarpine administration. Eur J Pharm Biopharm. 2017;113:140–8.
Kim J, Kudisch M, da Silva NRK, et al. Long-term intraocular pressure reduction with intracameral polycaprolactone glaucoma devices that deliver a novel anti-glaucoma agent. J Control Release. 2018;269:45–51.
PolyActiva Pty Ltd. Enabling drug delivery from medical devices: treatment of glaucoma. 2020. https://polyactiva.com/products/glaucoma-program/. Accessed Feb 1, 2020.
Lewis RA, Christie WC, Day DG, et al. Bimatoprost sustained-release implants for glaucoma therapy: 6-month results from a phase I/II clinical trial. Am J Ophthalmol. 2017;175:137–47.
Gelatt KN, MacKay EO. Effect of different dose schedules of latanoprost on intraocular pressure and pupil size in the glaucomatous Beagle. Vet Ophthalmol. 2001;4:283–8.
Ferrell Ramos M, Attar M, Stern ME, et al. Safety evaluation of ocular drugs. In: Faqi AS, editor. A comprehensive guide to toxicology in nonclinical drug development. 2nd ed. London: Academic; 2016. p. 757–811.
Toris CB, Gabelt BT, Kaufman PL. Update on the mechanism of action of topical prostaglandins for intraocular pressure reduction. Surv Ophthalmol. 2008;53(Suppl 1):S107–120.
Flach AJ. The importance of eyelid closure and nasolacrimal occlusion following the ocular instillation of topical glaucoma medications, and the need for the universal inclusion of one of these techniques in all patient treatments and clinical studies. Trans Am Ophthalmol Soc. 2008;106:138–48.
Gonnering RS, Dortzbach RK, Erickson KA, Kaufman PL. The cynomolgus monkey as a model for orbital research. I. Normal anatomy. Curr Eye Res. 1984;3:529–40.
Bouhenni RA, Dunmire J, Sewell A, Edward DP. Animal models of glaucoma. J Biomed Biotechnol. 2012;2012:692609.
Woodward DF, Krauss AH, Chen J, et al. Pharmacological characterization of a novel antiglaucoma agent, bimatoprost (AGN 192024). J Pharmacol Exp Ther. 2003;305:772–85.
Chen J, Dinh T, Woodward DF, et al. Bimatoprost: mechanism of ocular surface hyperemia associated with topical therapy. Cardiovasc Drug Rev. 2005;23:231–46.
Acknowledgements
Funding
This study was sponsored by Allergan (prior to its acquisition by AbbVie). The Rapid Service Fee was funded by AbbVie Inc.
Medical Writing, Editorial, and Other Assistance
Writing and editorial assistance were provided to the authors by Stephanie Kuwahara, PhD, of AbbVie Inc., Irvine, CA, and Evidence Scientific Solutions, Inc, Philadelphia, PA, and funded by AbbVie Inc. Covance Laboratories (Madison, WI) conducted the monkey study, and also dosed animals and collected samples for analysis in the dog study. QPS, LLC (Newark, DE) processed the samples and performed the autoradiography in the dog study.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. Neither honoraria nor payments were made for authorship.
Prior Presentation
This manuscript is based on work previously presented at the Association for Research in Vision and Ophthalmology (ARVO) 2016 Annual Meeting (May 1–5, 2016) in Seattle, WA, USA and the American Glaucoma Society 2020 Annual Meeting (February 27–March 1, 2020) in Washington, DC, USA.
Disclosure
Jie Shen, Michael R. Robinson, and Mayssa Attar are employees of AbbVie Inc. Rex A. Moats and Harvey A. Pollack declare that they have no conflict of interest.
Compliance with Ethics Guidelines
Animal procedures were carried out in accordance with the Association for Research in Vision and Ophthalmology (ARVO) statement for the Use of Animals in Ophthalmic and Vision Research. All animal procedures were performed in compliance with US Animal Welfare Act regulations.
Data Availability
The datasets generated during and/or analyzed during the current study are available from AbbVie Inc on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
This article is published with digital features to facilitate understanding of the article. You can access the digital features on the article’s associated Figshare page. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12662183.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shen, J., Moats, R.A., Pollack, H.A. et al. Distribution of 14C-Latanoprost Following a Single Intracameral Administration Versus Repeated Topical Administration. Ophthalmol Ther 9, 929–940 (2020). https://doi.org/10.1007/s40123-020-00285-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-020-00285-3