Abstract
Despite significant progress in retaining vision for neovascular age-related macular degeneration patients in the era of treatment with intravitreal anti-VEGF agents, there is no universally accepted treatment regimen that defines the frequency of treatment needed to achieve the optimal visual outcomes while simultaneously balancing the burden of long-term, frequent and high-cost treatment. Treat and extend has recently and consistently been used by retina specialists to minimise the financial and psychological costs of the need for frequent treatment with anti-VEGF injections. This is a systematic review that presents evidence from clinical trials and the real world on the utilisation of treat and extend with anti-VEGF intravitreal injections in neovascular age-related macular degeneration, and discusses the experience gained thus far from the utilisation of such regimens to preserve vision when treating patients over the long-term.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Seeking ways to minimise the frequency of treatment for neovascular age-related macular degeneration (nAMD) patients on anti-vascular endothelial growth factor (VEGF) intravitreal injections essentially means addressing the need to individualise treatment without compromising visual outcomes.
The PIER, EXCITE and SUSTAIN studies were the first randomised controlled trials (RCTs) where less-frequent treatment was attempted with ranibizumab [1,2,3]. The first two failed to achieve equal vision outcomes with quarterly injections compared to monthly injections, and the latter was only successful in the PRN (pro re nata or ‘as needed’) phase. In fact, even before phase III trials verified the optimal outcomes of treatment with ranibizumab, there was an attempt to achieve similar outcomes with as-needed injections: the amended open-label extension of phase I/II studies with ranibizumab and a long-term follow-up [4, 5].
The above led to the design of the prospective ProNTO (Prospective Optical Coherence Tomography Imaging of Patients With Neovascular AMD Treated With Intraocular Ranibizumab) study, in which 1- and 2-year visual acuity (VA) outcomes were achieved with fewer injections [6, 7], but there were significantly fewer patients compared to ANCHOR and MARINA [8, 9], there was no control group, and monthly visits were a requirement.
Reports from three studies with more than 2000 participants (CATT, HARBOR, IVAN) [10,11,12] were included in a meta-analysis performed by Schmucker et al. [13] which found that the patients on PRN treatment had slightly but statistically significantly worse BCVA and an increased risk of systemic adverse events compared to those given monthly injections. On the other hand, as Spaide justifiably noted: ‘returning every month for injection and follow-up, is a cost, but also is an emotional and psychological burden for the patient, family, and even the doctor’ [14].
The aim of this article is to offer a systematic review of publications related to studies of the effectiveness and safety of the treat and extend regimen of anti-VEGF intravitreal treatment in nAMD.
Treat and Extend Treatment Protocols Using Different Anti-VEGF Agents
Three types of anti-VEGF medications are currently used to treat nAMD: bevacizumab, ranibizumab and (more recently) aflibercept. As opposed to off-label bevacizumab, which is a VEGF-specific full-length antibody, ranibizumab is a VEGF-specific antibody fragment and aflibercept is a fusion protein that—aside from binding all VEGF-A isoforms—binds VEGF-B and placental growth factor (PIGF). The higher binding affinity of aflibercept may account for its longer duration of action and therefore the need for less-frequent treatment [15]. The VIEW1 and VIEW2 [Intravitreal Aflibercept (VEGF Trap-Eye) in Wet Age-Related Macular Degeneration] trials proved the safety and efficacy of bimonthly intravitreal injections of aflibercept to treat nAMD, and the less-frequently injected aflibercept showed similar functional outcomes to monthly ranibizumab injections [15].
Search Strategy/Methods
We searched PubMed and the Cochrane Database of Systematic Reviews from inception to February 2017 for clinical trials, prospective and retrospective studies, systematic reviews and meta-analyses linked to the treat and extend treatment regimen with anti-VEGF agents in neovascular age-related macular degeneration. We manually searched the references of the retrieved articles as well. Our aim was to at least include those with the largest numbers of participants and the longest follow-up periods. Unpublished data and relevant articles according to expert consensus were not included. Our search was limited to full text articles available in English.
Compliance with Ethics Guidelines
The work described here was based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Prospective Studies/Clinical Trials
Toalster et al. conducted a 12-month, open-label, nonrandomised, multicentre prospective trial using ranibizumab to access an inject and extend regimen using the same entry exclusion criteria as in the PrONTO trial [16]. Intervals between appointments were extended by 2 weeks when no activity was present and were shortened when the disease was active. Activity was defined exactly as in the PrONTO study: (1) visual acuity loss of at least five letters with OCT evidence of fluid in the macula, (2) an increase in OCT central retinal thickness of at least 100 µm, (3) new macular haemorrhage, (4) a new area of classic CNV, or (5) evidence of persistent fluid on OCT at least 1 month after the previous injection [6]. If one or more of the above were met, the disease was considered active and treatment was administered. VA was improved by 1.3 lines compared with baseline at 12 months, which was comparable to the PrONTO study results: a 9.3-letter improvement at 12 months. The average number of injections given by 12 months was 8, and most of the patients had the minimum number of 7 injections, although this was still higher than the 5.6 injections that were required in the PrONTO study.
Abedi et al. published data from a prospective, single-arm study that used a treat and extend regimen with ranibizumab or bevacizumab applied in nAMD patients over a 24-month period [17]. Treatment included 0.5 mg of ranibizumab or 1.25 mg of bevacizumab. After the loading dose of 3 monthly injections, treatment and visit intervals were based on disease activity, i.e. visual acuity of >5 letters from the previous monthly visit, persistent or new haemorrhage on dilated fundus examination, or subretinal or intraretinal fluid on OCT. In the case of active CNV, follow-up visits and anti-VEGF treatments continued every 4 weeks. In the case of no CNV activity, an injection was administered, and the interval to the next visit was extended by 2 weeks up to a maximum of 12 weeks. In the case of reactivation, the interval was shortened by 2 weeks. In a total of 120 patients, 95% of 101 patients who completed 24 months of follow-up lost fewer than 15 letters and almost 30% gained more than 15 letters, which the authors found to be comparable to those of the ANCHOR and MARINA studies. Better baseline vision also meant an increased likelihood of visual loss, and this was the only variable significantly associated with VA change. On the contrary, patients who started off with a low baseline VA were more likely to improve with treatment. On average, only 8.6 and 5.7 injections in the first and second years, compared with 13 and 12 injections for the MARINA patients, were required to achieve a similar VA outcome.
The Lucentis (ranibizumab) Compared to Avastin (bevacizumab) Study (LUCAS) was the first randomised multicentre trial to use a treat and extend protocol [18]. 441 Patients with nAMD at 10 ophthalmological centres in Norway were randomised to receive intravitreal injections of ranibizumab 0.5 mg or bevacizumab 1.25 mg in a 1:1 ratio. Patients were examined and injected every 4 weeks until no signs of active AMD were found. Activity was based on imaging and dilated biomicroscopy. Any fluid on OCT, leakage on FFA or increased lesion size on FFA was defined as active disease. In the case of inactive CNV, a new injection was given and the period to the next treatment was extended by 2 weeks at a time up to a maximum of 12 weeks. In the case of reactivation, the interval was shortened by 2 weeks at a time until the disease was considered to be inactive. The maximum final interval was 2 weeks less than the period when the previous recurrence was observed. At 1 year, bevacizumab and ranibizumab were equivalent when using a treat and extend protocol, and BCVA increased significantly in both groups: the proportion of patients who gained more than 15 letters was similar in both groups. However, among the secondary outcomes, the investigators found a significant difference in interval length between the two drugs: patients on treatment with bevacizumab were more likely to require injections every 4 weeks whereas patients treated with ranibizumab were more likely to be treated every 12 weeks. Additionally, at the end of the 1-year follow-up, it was more likely for patients treated with bevacizumab to have fluid on OCT imaging. The overall improvement in VA was found to be comparable with the CATT study results at 1 year for both types of anti-VEGF with less-frequent treatment.
In contrast to prior uncontrolled analyses of treat and extend regimens, the Treat-and-Extend Protocol in Patients with Wet Age-Related Macular Degeneration (TREX-AMD) [19] was a direct prospective comparison of monthly and treat and extend dosing. This was a phase IIIb, multicentre, randomised, controlled clinical trial where 60 treatment-naïve nAMD patients were randomised 1:2 to the monthly or TREX cohort at enrolment. All patients received a loading dose of three four-weekly ranibizumab injections and were then treated, according to randomisation, with either monthly ranibizumab or TREX ranibizumab. In the TREX cohort, intervals varied from 4 to 12 weeks. There were one- and two-week increments in the interval between visits (and treatments) depending on the resolution of intraretinal or subretinal fluid on SD OCT and on the resolution of subretinal or intraretinal haemorrhage. Three episodes of recurrent disease activity at a given interval meant that treatment was continued at the next shortest interval for three consecutive visits, and then the TREX protocol was re-initiated. One-year post hoc analysis of TREX-AMD indicated a difference in means between cohorts of 1.3 ETDRS letters and standard deviations of 6.1 and 10.9 ETDRS letters for the monthly and TREX cohorts, respectively. Mean BCVA gains were similar between cohorts: at month 12, 15% and 25% had gained 15 ETDRS letters or more in the monthly and TREX cohorts, respectively. No patient in the monthly cohort lost more than 5 ETDRS letters, and 8% in the TREX cohort lost 10 letters (3% lost 37 letters because of progressive macular atrophy). At month 12, the mean number of treatments administered was 13.0 and 10.1 for the monthly and TREX cohorts, respectively (p < 0.0001). Mean VA gains in the monthly and TREX cohorts at month 12 were consistent with gains in the ANCHOR, MARINA, VIEW1 and VIEW2 trials as well as with outcomes in the study by Abedi et al. described above. The two-year outcomes of the study were recently published, and findings were similar for the monthly and the T&E cohorts regarding VA gains [20]. Apart from the presence of a control group which consisted of patients treated monthly, this study had another obvious strength: the consideration of a longitudinally dynamic maximum extension of intervals between treatments. The investigators tried to find out whether the previous maximum interval could be further lengthened instead of using the static two-week interval used in all previous studies. As the authors commented, interval duration may be related to the wide range of individual VEGF suppression times and subsequently to an individual’s maximum tolerated dosing interval. In addition, they noted that both experimental and clinical data showed that the need for anti-VEGF retreatment was reproducible for one individual [21, 22]. In the Long-term Follow-Up of Intravitreal Aflibercept Injection (IAI) for Neovascular Age-Related Macular Degeneration (nAMD) in an Open-Label Extension of the VIEW1 Study, in which 323 patients were enrolled, the mean range of injections between weeks 96 and 192 was 9.6. The proportions of patients who gained ≥0 and ≥15 letters from the VIEW1 baseline were 83% and 37%, respectively, at week 96, and 72% and 30%, respectively, at week 192. The most common serious ocular adverse events were retinal haemorrhage (0.6%) and reduced visual acuity (0.6%). Visual benefits achieved with anti-VEGF therapy during 2 years of VIEW1 were maintained by continued treatment with aflibercept over a period of two years in the extension study [23]. De Croos et al. presented the outcomes of the Aflibercept Treat and Extend Therapy for Neovascular Age-Related Macular Degeneration (ATLAS) study [24]. Forty eyes of 40 treatment-naïve participants with nAMD entered this multicentre, prospective, open-label study. Patients were treated every 4 weeks until no signs of macular exudation were present, based on clinical examination and OCT. The treatment extension interval was 2 weeks up to a maximum of 16 weeks. A median BCVA improvement of 11 letters (p < 0.001) was recorded during the first year with an average of 8 injections. A BCVA improvement of 11 letters was sustained during the second year (p < 0.001) with an average of 5.9 injections. A 12-week interval was achieved in 35% of the patients during the first year and in 41% of the patients during the second year. In a prospective database observational trial conducted in Australia, Essex et al. analysed longitudinal data obtained from routine clinical practices in order to describe clinical outcomes during the maintenance phase of treat and extend management of nAMD [25]. They defined the maintenance phase as ‘the period after the first clinician-reported grading of inactivity’. All clinicians agreed to declare lesions as active if there were features such as sub- or intraretinal fluid or new haemorrhage based on fundoscopy, optical coherence tomography and (less frequently) fluorescein angiography. Only practices that exclusively used a treat and extend protocol were eligible for inclusion in the study. There was also a requirement for at least 12 months of follow-up from the first grading of inactivity. The number of injections required to inactivate the lesion was recorded prior to study entry. They classified VA change at each visit as a loss of >0 letters or 15 letters from the previous visit. 2096 eyes were included in the analysis. The mean follow-up after a lesion was first found to be inactive was approximately 40 months. 50% reactivated within the first year of the maintenance phase and 36% reactivated more than once. The most common reactivation interval was 8 weeks and the risk of reactivation at each visit rose with increasing interval; substantially so beyond 12 weeks. There was double the risk of VA loss as the treatment interval increased, especially beyond 16 weeks. As in the LUCAS study, investigators noted that in this study there was no consistent association between the first failing treatment interval and future VA. Therefore, shortening the treatment interval was not associated with poorer VA. One of the main conclusions of this study was that there was still some improvement in visual acuity, at least during the first few months of what was considered to be the maintenance phase. One of the pitfalls of this study, as in most real-world data studies, was that a large proportion of the patients were lost to follow-up (30% were lost at 24 months and 55% at 36 months), which should be taken into account when interpreting the results. The authors finally suggested there was general agreement on the best management—monthly injections until inactivation—and that further management was subject to ‘innumerable subtle variations in the approach that clinicians use’. The above studies retrieved from the literature as described in our search strategy are summarised in Table 1, as are some of their important findings.
Retrospective/Real-World Studies
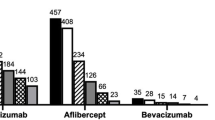
Arnold et al. analysed anonymised data from the Fight Retinal Blindness (FRB) registry, which were captured during routine clinical practice [26]. 1198 Treatment-naïve nAMD eyes included in this observational study had been treated with intravitreal injections by 19 ophthalmologists throughout Australia and New Zealand using a T&E protocol, and had a follow-up of at least 24 months. All three drugs (bevacizumab, ranibizumab and aflibercept) were used either as monotherapy or as a combination of at least two anti-VEGF agents, apart from aflibercept, which was never used as monotherapy in the eyes included in this study. Ranibizumab was the predominant drug during the studied period. There was a mean of 7.5 injections per eye in the first year and 5.5 in the second, giving a mean of 13.0 injections per eye over 24 months. The mean number of visits was only slightly greater than the number of injections: 7.9 in the first year and 6.7 in the second year.
To account for an effect of patients lost to follow-up on outcomes, the investigators compared the change in mean VA in the study cohort with that for eyes that had <24 months of follow-up but otherwise met the study inclusion criteria. They found that mean initial VA of the 1198 eyes that completed the 24-month follow-up was significantly better than that of the eyes with <24 months of follow-up (p = 0.001), while there was no difference between the lesion types for eyes with 24 months of follow-up and those with shorter follow-up periods. The interval between treatments was classified as 4, 5–6, 7–8, 9–15, or 16 weeks. Eyes were not treated at every visit in this study, as might be expected in a strict T&E protocol. Vision of 20/40 was achieved by 27% at baseline, increasing to 45% at 2 years post treatment initiation. Moderate (15-letter) loss of vision was avoided by 90% in this study. The investigators commented on the 35% of eyes that were lost to follow-up, had a worse baseline VA, and were not included in the main analysis: they suggested that, with experience, practitioners learned to distinguish between eyes for which treatment was worth pursuing and eyes for which further treatment was futile based on the initial response. They also noted that the majority of patients were lost to follow-up in the second year and not earlier. The mean VA improvement for those eyes was similar to that for the group that continued for 2 years. The authors of the relevant paper concluded that—unlike in clinical trials—their patient study group was unselected, and that real-world data demonstrated that a T&E regimen can produce good results with fewer visits than other regimens.
Mrejen et al. published the outcomes of a retrospective study of a consecutive series of 374 treatment-naïve patients with nAMD in one or both eyes who were treated with an anti-VEGF treat and extend regimen with a maximum follow-up of 72 months [27]. Among other parameters, they recorded the type of anti-VEGF agent and the retention rate, which refers to the proportion of patients who were not lost to follow-up or who switched to another treatment strategy before final data collection. They classified neovascular lesions according to fluorescein findings, but they also used the anatomical classification based on FA and OCT: type 1, sub-RPE; type 2, subretinal; type 3, intraretinal; type 4, mixed lesions. Eyes with polypoidal choroidal vasculopathy (PCV) were considered to be a form of type 1 CNV. Cases with multiple lesion types were identified as mixed CNV, and each component was recorded. Readers graded the location and overall size of each lesion.
Among these 374 patients, 185 patients (210 eyes) met the eligibility criteria. The mean follow-up was 42 months and the retention rate for the entire cohort was 63% over the 6-year time period. The retention rate was 100% at 1 year, 83% at 2 years, 61% at 3 years, 42% at 4 years, 26% at 5 years and 13% at 6 years. They found that visual benefits obtained at 6 months were largely maintained long-term at 3, 4 and 6 years. At 5 years, they observed that there was a decline in mean VA such that it approached the baseline VA, which appeared to be inconsistent with the rest of the curve. They also noted one isolated point at 6 years that showed a mean visual gain of 0.1626, which was again inconsistent with the rest of the curve. The authors explained these inconsistencies by invoking the small number of patients with a long-term follow-up and the biased retention of patients with better VA outcomes. Baseline and 6-month VA were positively correlated with VA at all time points. Number of injections and anatomic classification were consistently and independently correlated with visual acuity at all time points. Eyes with type 1 CNV started with a better baseline VA, followed by types 3, 2 and 4 (mixed) CNV, and this sequence remained true at 1, 2, 3 and 4 years. The visual results by neovascular lesion type at 5 and 6 years were not detailed due to the small number of patients in each subgroup. Subfoveal neovascular lesions were more likely to show visual improvement than extrafoveal lesions. On average, patients in this study received injections every 6.3 weeks (8.3 injections per year). The number of intravitreal anti-VEGF injections was positively correlated with visual outcome. Changes in the treatments available during the long-term follow-up period account for one of the limitations of this study. The authors of the relevant paper commented that choice of drug may not have been independent of baseline characteristics and may have contributed to the final visual outcome. However, there were no sound statistically significant conclusions regarding the type of anti-VEGF. Overall, they suggested that the anatomic classification of neovascular lesions based on multimodal imaging AMD was the most clinically meaningful and useful for guiding individualised therapeutic dosing strategies including T&E.
A total of 212 eyes from 189 consecutive patients with treatment-naïve nAMD were retrospectively included in a study by Rayess et al. that evaluated the outcome of treat and extend anti-VEGF for up to 3 years of follow-up [28]. Patients were treated with monthly (4–5 weeks) intravitreal injections of either bevacizumab or ranibizumab until no signs of CNV activity were detected on slit-lamp biomicroscopy and spectral domain OCT. Beyond this point, patient visits and treatments were extended by 2 weeks or were shortened by 2 weeks if signs of CNV activity reappeared. The mean follow-up period was 1.88 years. The minimum follow-up for all eyes included was 1 year, with 57% and 28% of eyes completing 2 and 3 years of follow-up, respectively. At 1 year of follow-up, 95% of patients had lost <3 BCVA lines, whereas 96% and 92% of patients lost <3 BCVA lines at 2 and 3 years of follow-up, respectively. 36%, 31% and 36% gained >3 BCVA lines following 1, 2 and 3 years of treatment, respectively. At year 1, 52% of patients had persistent CNV activity based on spectral-domain OCT findings. Following 2 and 3 years of treatment, 52% and 53% of patients (respectively) were CNV active. In this study, on average, patients received 7.6 injections in the first year, 5.7 injections in the second year, and 5.8 injections in the third year. It was shown that, overall, a significant gain in visual acuity was achieved with fewer visits and injections. Among the weaknesses of this study was the large difference between the number of patients who completed 1 year of follow-up and the number of patients who completed 2 or 3 years of follow-up.
A recent electronic case review of consecutive treatment-naive nAMD patients treated with aflibercept over 2 years using a treat and extend approach in year 2 with a maximum treatment-interval extension of 3 months was conducted by Eleftheriadou et al. in the UK [29]. This was the first real-world study to evaluate long-term VA- and OCT-based retinal morphology outcomes of this anti-VEGF agent for treating nAMD in a clinical setting in treatment-naïve eyes. Although there was variability in the treatment pattern due to the involvement of a large number of clinicians, there was a secondary analysis of outcomes for the subgroup of eyes that had received treatment as per the VIEW trial treatment paradigm for year 1 followed by a treat and extend approach to treatment in year 2, in which there were no VA or type of CNV related exclusion criteria. 94 eyes were included in the 2-year follow-up outcome analysis; almost 10% had lost 15 ETDRS letters by the end of the follow-up period and 22% had gained 15 letters or more. The investigators attributed the visual loss of 15 letters or more to the presence of foveal atrophy, subretinal fibrosis or retinal pigment epithelial tears. There was a subgroup analysis of visual acuity change at 1 and 2 years, with a mean gain of VA 7.3 letters (p < 0.001) at 1 year and 7.1 letters from baseline at 2 years (p < 0.001). The mean number of Eylea injections during 2 years was 13.5. They also found no significant differences when they compared functional and anatomical outcomes of eyes with residual fluid to those of eyes with no fluid at the end of the first year and the end of the second year of follow-up. Overall, they found their results to be comparable to those for the VIEW trial, and they concluded that implementing aflibercept treatment with fixed dosing in year 1 followed by a treat and extend treatment paradigm as standard care in clinical practice results in excellent visual acuity and retinal morphologic outcomes over 2 years.
Barthelmes et al. recently reported the 24-month outcomes of a real-world retrospective study of patients receiving aflibercept as the only anti-VEGF treatment in a T&E regimen for 212 treatment-naive eyes with nAMD, of which 136 eyes completed the 24-month follow-up, 60 eyes did not complete the 24-month follow-up, and 16 eyes switched to ranibizumab prior to the completion of the 24 months [30]. The proportion of eyes with good vision (≥20/40) was higher among the completers, and there was no difference in the size or the type of the CNV lesion between the completer and the noncompleter groups. A mean of 7.8 injections were received in the first year, which dropped to 5.7 injections in the second year for completers. 98% of the eyes which initially had a visual acuity of 70 ETDRS letters maintained this acuity 24 months after initiating treatment, and a loss of 15 letters was avoided by 93% of the eyes that completed follow-up. An interesting finding was that eyes for which treatment had been switched had a higher baseline visual acuity and a higher proportion with good vision. The mean visual acuity change for eyes lost to follow-up was +3.9 letters, which did not differ between completers and noncompleters. As the authors suggested, dropping out did not seem to be due to poor visual outcomes. They commented on differences in treatment interval between aflibercept and ranibizumab, especially during the second year of treatment, in which intervals appeared to be longer when treating with aflibercept in their study as opposed to previous studies where ranibizumab was predominantly used for treatment. However, such comparisons may not be valid due to the different time periods that drove patients to certain anti-VEGF choices, but also because direct comparison between the two anti-VEGF agents has not been attempted.
Smaller Scale Real-World Studies
Smaller scale retrospective studies in terms of number of participants and/or length of follow-up have been also published. Investigators have analysed the clinical and economic impacts of treat and extend regimens with anti-VEGF in nAMD and concluded that significant visual acuity gains could be achieved using this regime, along with fewer visits and treatments and a significantly lower annual medical cost, without incurring alarming ocular or systemic adverse events [31,32,33]. Some of them have also addressed the impacts of different lesion types on the outcome of the T&E regime and the impacts of specific anti-VEGF agents [33,34,35].
In most of the above studies there was no control group (i.e. there were no head to head comparisons between different treatment regimens or between all of the different types of anti-VEGF agents), and the length of follow-up is relatively short. The reasons for the loss of patients to follow-up were not always thoroughly investigated, and the withdrawal of nonresponders from treatment may have contributed to outcomes that are biased towards study groups who respond well to treatment, especially in studies with long follow-up periods. On the other hand, aflibercept, the anti-VEGF agent with perhaps the longest duration of action, was not the anti-VEGF used by physicians in most of the studies, as it became available later. Long-term outcomes of a T&E regimen using this agent are only now beginning to get published.
The above studies retrieved from the literature as described in our search strategy and some of their important findings are summarised in Table 2.
Future Considerations
There is no standard regimen regarding the frequency of anti-VEGF injections for nAMD after the loading dose of three injections. However, there is a well-documented need to address the risk of visual loss because of undertreatment as well as the need to reduce costs and the psychological/emotional burden on patients and their families. The outcomes of all the studies discussed in this article—in terms of the benefits of treat and extend regimens—are encouraging, as it seems that the number of injections and visits can be reduced without negatively affecting visual function. In addition to designing future prospective RCT trials to adequately evaluate the effectiveness and safety of T&E regimens in nAMD, we need to keep up to date with the outcomes of large real-world series and current prospective trials such as the VITAL study (Individualizing Therapy for Neovascular Age-Related Macular Degeneration with Aflibercept), a 24-month phase IV study evaluating the outcomes of aflibercept therapy using a capped treat and extend approach in year 2 in eyes with active nAMD (Clinical Trials gov. identifier NCT02441816).
There are questions that remain answered, in addition to issues arising from the inherent limitations of addressing just one aspect of a complex disease (namely neovascularisation) in which vision loss may arise due to the interplay of a range of pathogenic factors. For example, when is the right time to shorten intervals in the context of a treat and extend treatment plan? According to most of the studies discussed above, the most common reason has been the accumulation of new fluid or persistent fluid on SD-OCT imaging that detects fluid accumulation prior to the appearance of a new haemorrhage or a new CNV [16]. With the advent of OCT angiography, the detection of vessel characteristics of treated CNV based on the ability to image blood flow may add to our understanding of the development and progress of neovascular lesions treated with anti-VEGF. It may additionally elucidate the alterations in the morphology of the remaining vascular bed that Spaide noted when he described the signs of vascular abnormalisation with antiangiogenic therapy for CNV [36].
None of the studies described above demonstrated a concerning increase in the frequency of serious systemic adverse events (SAEs) when using any anti-VEGF agent in the context of a treat and extend regimen. However, as R. Avery noted, because of the inclusion of the outcomes of the LUCAS trial (as extracted from a presentation in which it appeared that serious cardiovascular effects were more frequent with ranibizumab than with bevacizumab) in a Cochrane meta-analysis, the previous belief that bevacizumab poses a significant risk of systemic SAEs changed to a belief that the risk posed by bevacizumab is nonsignificant [37]. However, following the full publication of the LUCAS outcomes, the risk shifted again from nonsignificant to significant with bevacizumab. The author of the correspondence suggested that small numerical differences may easily alter the significance of events. We therefore suggest caution when interpreting the results using statistics rather than by proving differences that are relevant to different drug pharmacokinetic profiles and when making serious assumptions about the safety of anti-VEGF agents used in any treatment regimen, including T&E.
Finally, as per recent articles on the risk of ‘geographic atrophy’ and its possible association with anti-VEGF treatment [38, 39], T&E may also alleviate concerns about VA loss due to macular atrophy arising from anti-VEGF overtreatment compared with monthly injections. However, given that PRN regimens may reduce the risk of incident geographic atrophy compared to T&E due to the lower number of injections involved, the benefits of T&E should be carefully weighed against possible adverse outcomes.
References
Abraham P, Yue H, Wilson L. Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular agerelated macular degeneration: PIER study year 2. Am J Ophthalmol. 2010;150:315–24.
Schmidt-Erfurth U, Eldem B, Guymer R, et al. Efficacy and safety of monthly versus quarterly ranibizumab treatment in neovascular age-related macular degeneration: the EXCITE Study. Ophthalmology. 2011;118:831–9.
Holz FG, Amoaku W, Donate J, Guymer RH, Kellner U, Schlingermann RO, et al. Safety and efficacy of a flexible dosing regimen of ranibizumab in neovascular age-related macular degeneration: the SUSTAIN study. Ophthalmology. 2011;118(4):663–71.
Heier JS, Antoszyk AN, Pavan PR, et al. Ranibizumab for treatment of neovascular age-related macular degeneration: a phase I/II multicenter, controlled, multidose study. Ophthalmology. 2006;113(642):e1–4.
Rosenfeld PJ, Heier JS, Hantsbarger G, et al. Tolerability and efficacy of multiple escalating doses of ranibizumab (Lucentis) for neovascular age-related macular degeneration. Ophthalmology. 2006;113(632):e1.
Fung AE, Lalwani GA, Rosenfeld PJ, et al. An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol. 2007;143:566–83.
Lalwani GA, Rosenfeld PJ, Fung AE, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular agerelated macular degeneration: year 2 of the PrONTO study. Am J Ophthalmol. 2009;148:43–58.
Brown DM, Michels M, Kaiser PK, et al. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology. 2009;116:57–65.
Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–31.
Comparison of Age-Related Macular Degeneration Treatments Trial (CATT) Research Group, Martin DF, Maguire MG, et al. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology. 2012;119(7):1388–98.
Ho AC, Busbee BG, Regillo CD, et al. Twenty-four-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology. 2014;121(11):2181–92.
Inhibition of VEGF in Age-Related Choroidal Neovascularization (IVAN) Study Investigators, Chakravarthy U, Harding SP, Rogers CA, et al. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology. 2012;119(7):1399–411.
Schmucker CM, Rucker G, Sommer H, et al. Treatment as required versus regular monthly treatment in the management of neovascular age-related macular degeneration: a systematic review and metaanalysis. PLoS One. 2015;10(9):e0137866.
Spaide R. Ranibizumab according to need: a treatment for age-related macular degeneration AJO. 2007;143:679–80.
Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119:2537–48.
Toalster N, Russell M, Ng P. A 12-month prospective trial of inject and extend regimen for ranibizumab treatment of age-related macular degeneration. Retina. 2013;33:1351–8.
Abedi F, Wickremasinghe S, Islam AF, Inglis KM, Guymer RH. Anti-VEGF treatment in neovascular age-related macular degeneration: a treat-and-extend protocol over 2 years. Retina. 2014;34:1531–8.
Berg K, Pedersen TR, Sandvik L, Bragadóttir R. Comparison of ranibizumab and bevacizumab for neovascular age-related macular degeneration according to LUCAS treat-and-extend protocol. Ophthalmology. 2015;122:146–52.
Wykoff CC, Croft DE, Brown DM, et al. Prospective trial of treat-and-extend versus monthly dosing for neovascular age-related macular degeneration: TREX-AMD 1-year results. Ophthalmology. 2015;122:2514–22.
Wykoff CC, Ou WC, Brown DM, et al. Randomized trial of treat-and-extend versus monthly dosing for neovascular age-related macular degeneration: 2-year results of the TREX-AMD study. doi:10.1016/j.oret.2016.12.004.
Muether PS, Hermann MM, Droge K, et al. Long-term stability of vascular endothelial growth factor suppression time under ranibizumab treatment in age-related macular degeneration. Am J Ophthalmol. 2013;156(989–993):e982.
Mantel I, Dei A, Iglesias K, et al. Prospective study evaluating the predictability of need for retreatment with intravitreal ranibizumab for age-related macular degeneration. Ger J Ophthalmol. 2013;251:697–704.
Marcus DM. Long-term follow-up of intravitreal injection for neovascular age-related macular degeneration in an open-label extension of the VIEW 1 Study. Abstract presented at the Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting; 2014 May 4–8; Orlando.
DeCroos FC, Reed DC, Adam MK, et al. Prospective, multicentre investigation of aflibercept treat and extend therapy for neovascular age related macular degeneration (ATLAS study): one and two year results. Abstract presented at: the Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting; 2016 May 1–6; Seattle.
Essex RW, Nguyen V, Walton R, et al. Treatment patterns and visual outcomes during the maintenance phase of treat-and-extend therapy for age-related macular degeneration. Ophthalmology. 2016;123:2393–400. doi:10.1016/j.ophtha.2016.07.012.
Arnold JJ, Campain A, Barthelmes D, et al. Two-year outcomes of “treat and extend” intravitreal therapy for neovascular age-related macular degeneration. Ophthalmology. 2015;122:1212–9.
Mrejen S, Jung JJ, Chen C, et al. Long-term visual outcomes for a treat and extend anti-vascular endothelial growth factor regimen in eyes with neovascular age-related macular degeneration. J Clin Med. 2015;4:1380–402.
Rayess N, Houston SK 3rd, Gupta OP, Ho AC, Regillo CD. Treatment outcomes after 3 years in neovascular age-related macular degeneration using a treat-and-extend regimen. Am J Ophthalmol. 2015;159:3–8.
Eleftheriadou M, Vazquez-Allfageme C, Citu CM, et al. Long-term outcomes of aflibercept treatment for neovascular age-related macular degeneration in a clinical setting. Am J Ophthalmol. 2017;174:160–8.
Barthelmes D, Nguyen V, Daien V, et al. Two year outcomes of 'Treat and Extend' intravitreal therapy using aflibercept preferentially for neovascular age related macular degeneration. Retina. 2017. doi:10.1097/IAE.0000000000001496.
Gupta OP, Shienbaum G, Patel AH, Fecarotta C, Kaiser RS, Regillo CD. A treat and extend regimen using ranibizumab for neovascular age-related macular degeneration clinical and economic impact. Ophthalmology. 2010;117:2134–40.
Shienbaum G, Gupta OP, Fecarotta C, Patel AH, Kaiser RS, Regillo CD. Bevacizumab for neovascular age-related macular degeneration using a treat-and-extend regimen: clinical and economic impact. Am J Ophthalmol. 2012;153:468–73.
Oubraham H, Cohen SY, Samimi S, et al. Inject and extend dosing versus dosing as needed: a comparative retrospective study of ranibizumab in exudative age-related macular degeneration. Retina. 2011;31:26–30.
Engelbert M, Zweifel SA, Freund KB. “Treat and extend” dosing of intravitreal antivascular endothelial growth factor therapy for type 3 neovascularization/retinal angiomatous proliferation. Retina. 2009;29:1424–31.
Engelbert M, Zweifel SA, Freund KB. Long-term follow-up for type 1 (subretinal pigment epithelium) neovascularization using a modified “treat and extend” dosing regimen of intravitreal antivascular endothelial growth factor therapy. Retina. 2010;30:1368–75.
Spaide RF. Optical coherence tomography angiography signs of vascular abnormalization with antiangiogenic therapy for choroidal neovascularization. doi:10.1016/j.ajo.2015.04.012.
Avery RL. Re: Berg et al.: Comparison of ranibizumab and bevacizumab for neovascular age-related macular degeneration according to LUCAS treat-and-extend protocol. Ophthalmology. 2016;123:e14–6.
Grunwald J, Daniel E, Huang J, et al. Risk of geographic atrophy in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2014;121:150–61.
Xu L, Mrejen S, Jung JJ. Geographic atrophy in patients receiving anti-vascular endothelial growth factor for neovascular age-related macular degeneration. Retina. 2015;35:176–86.
Acknowledgments
The authors are supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
No funding or sponsorship was received for the publication of this article.
The named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
M. Gemenetzi and P.J. Patel have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/6D08F06045CB4DE0.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Gemenetzi, M., Patel, P.J. A Systematic Review of the Treat and Extend Treatment Regimen with Anti-VEGF Agents for Neovascular Age-Related Macular Degeneration. Ophthalmol Ther 6, 79–92 (2017). https://doi.org/10.1007/s40123-017-0087-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-017-0087-5