Abstract
Introduction
To assess the anatomical changes taking place in the choroid after a scleral buckle (SB) procedure for retinal detachment repair.
Methods
This cross-sectional study looked at 23 adults with a history of unilateral retinal detachment repaired with a SB or other encircling element. The subjects underwent bilateral Enhanced Depth Spectral Domain Optical Coherence Tomography to image the choroid. The choroidal thickness (CT) was measured, and the non-operative eye was used as an internal control.
Results
CT was measured to be 170.8 ± 60.9 µm (mean ± SD) in eyes with SBs compared to 175.1 ± 61.9 µm in non-operative eyes. There was no statistically significant difference between the two groups (mean 4.3 µm, 95% CI −8.7, 17.3, p value 0.4973, paired t test).
Conclusion
Placement of an SB as part of a surgery to repair retinal detachment did not significantly alter CT at the macula.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The choroid plays an important role in ocular homeostasis and physiology including nutrition, temperature regulation, and emmetropization [1]. Studies in chicken eyes have shown that utilizing plus-diopter lenses to focus an image in front of the retina results in thickening of the choroid over a matter of hours to bring the retina closer to the image [2]. The opposite occurs with minus-diopter lenses, where the image is focused behind the retina. Other studies have suggested similar changes may occur in marmosets as well as humans [1, 3]. The mechanism by which this phenomenon occurs is poorly understood.
Additionally, the choroid has been observed to be thinner in eyes with myopia and with advanced age [4, 5]. In patients with central serous retinopathy, the choroid has been noted to be significantly thicker than those in healthy patients and has been used as a measure for diagnosis [6].
Measurements of the choroid have historically been performed in autopsy using microscopic examination. These methods do not provide an accurate representation of the choroid in vivo as tissue processing can dehydrate and alter the normal structure. Enhanced depth imaging (EDI) with spectral domain optical coherence tomography (SD-OCT) has become a novel method to accurately measure choroidal thickness (CT) in vivo [7]. With this method, the choroid–scleral interface is set to a zero delay, where sensitivity is highest, and the focus is manually placed more posteriorly than in traditional retinal SD-OCT. This allows capture of the full thickness of the choroid and enables more accurate measurements in vivo.
Choroidal blood flow has been previously demonstrated to be altered after retinal detachment repair with scleral buckle (SB), as measured by Doppler flowmetry [8]. In this study, Eshita et al. demonstrated reduced choroidal blood flow in the foveal region. Similarly, a study by Sugawara et al. demonstrated that the foveal choroidal blood flow was transiently decreased after SB surgery because of the increased choroidal vascular resistance but recovered by 12 weeks in patients with retinal detachment without macular involvement [9]. The mechanisms of these changes remain unclear.
Despite the advances in retina-choroidal imaging, we know very little about how changes in the choroidal circulation after SB surgery affect the CT. It is thought that decreased choroidal blood flow increases hemostasis in the choroidal circulation, thus increasing choroidal blood pressure with secondary increase in subfoveal CT [10].
Previous ED-SD-OCT studies have measured CT after SB surgery and found that the subfoveal CT transiently increased afterwards but returned to normal ~1–3 months after surgery [11, 12]. In contrast, Odrobina et al. in 2013 found that the subfoveal CT remained thickened for much longer after SB surgery when using an encircling band [10]. Factors that could alter CT include the extent of the SB, the size and width of the SB, and post-operative inflammation, particularly if cryotherapy was utilized during surgery [11].
This study aims to further investigate the structural changes of the choroid that may occur after placement of an SB as part of retinal detachment repair. With advances in surgical techniques increasing the amount of vitrectomies with decreased utilization of SB surgeries performed today, changes in CT may need to be analyzed separately. Nonetheless, SB is not an abandoned technique, and our findings may be used to help explain a few of the complications associated with SB surgery such as choroidal detachments that can occur in patients with posteriorly positioned SB as well as patients with greater circumferential coverage from the buckle element [13]. Serous detachments in these cases correlated to compression of vortex veins. It is not well understood if subclinical choroidal thickening occurs after an SB procedure. It may also explain the increased incidence of glaucoma after SB placement as a possible result of choroidal changes manifesting from its mechanical presence [14]. Further understanding of these anatomic changes can lead to improvement in techniques to repair retinal detachments with the ultimate goal of improving visual outcome for these patients.
Methods
This was a cross-sectional study of patients who previously had retinal detachment repair in one eye with an SB, with or without vitrectomy. This study protocol was reviewed and approved by the University of Minnesota Institutional Review Board and Ethics Committee. Eligible patients were recruited who had SB surgery performed to either eye and were over the age of 18. Patients had to be able to successfully complete an OCT exam with an identifiable foveal contour. The patient had to be at least 3 months out after the SB surgery with or without vitrectomy to reduce any confounding effect from post-operative inflammation. Exclusion criteria included any other retinal co-morbidities.
This study protocol was reviewed and approved by the University of Minnesota Institutional Review Board and Ethics Committee. The procedures followed were also in accordance with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
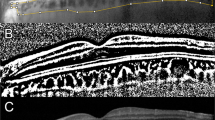
Subjects underwent a complete ophthalmic examination as dictated by their previously scheduled retina visit. In addition, information related to the original repair was collected, including the type of encircling element and the date when the repair took place. The last refraction, or eyeglass prescription at the time of the detachment, was also obtained. The Spectralis® (Heidelberg Engineering, Heidelberg, Germany) SD-OCT was used in the EDI mode to capture the choroid posterior to the macula in both eyes. Two methods were used to measure the CT. In the first method, the OCT image was exported to ImageJ (measurement software available to the public for research purposes through National Institutes of Health). The scaling was corrected within the ImageJ software [15]. The choroidal boundaries were manually traced over a 6 mm length centered directly under the fovea, and the area of the traced choroidal region was calculated by ImageJ (Fig. 1). This area was then divided by the length (6 mm) to obtain the average thickness of the choroid over the 6 mm region. In the second method, “the subfoveal CT,” we measured the CT at a single point directly under the fovea. This was measured as the distance from the hyper-reflective retinal pigment epithelium to the outer choroid under the fovea (Fig. 1).
A sample of choroidal measurements in the first method using ImageJ software. The image was imported from the Spectralis® (Heidelberg Engineering, Heidelberg, Germany) software; the choroid was manually traced as indicated by the large arrows. The double red arrow indicates the second method of measuring the subfoveal choroidal thickness. The choroidal thickness was measured directly under the fovea using the Spectralis software
Statistical measurements were performed using GraphPad Prism version 6.00 for Windows, GraphPad Software, La Jolla, USA. A two-tailed paired t test with a 95% confidence interval was performed. A linear regression analysis was also performed with this software.
Results
Forty subjects recruited at the University of Minnesota Department of Ophthalmology and Visual Neurosciences between September 2011 and June 2012, underwent EDI with SD-OCTs during the recruitment period. Results from a total of 23 subjects were analyzed; there were 2 female and 21 male subjects with an average age of 64 (range 45–80 years). Eleven patients underwent SB, and 12 patients underwent SB with vitrectomy. Subjects were excluded due to poor imaging quality, bilateral SB or obtaining unilateral ocular imaging only.
Of the included patients, using the first method, the average CT in a 6 mm area was 170.8 ± 60.9 µm (mean ± SD) in eyes with SB and 175.1 ± 61.9 µm in the fellow normal eyes without a history of retinal detachment. Using the second method, the average subfoveal CT was 197.5 ± 73.0 and 200.1 ± 80.9 µm in the operative eye and control eye, respectively. p values were obtained from a two-tailed paired t test with a 95% confidence interval comparing the mean thickness in the operative eye to the control eye. For the first method the p value was 0.4973 and for the second method the p value was 0.8211; both methods showed no statistical significance (Table 1). The average intra-subject difference in the CT between eyes using the first method was 4.3 µm and was not statistically significant (95% CI −8.7, 17.3, p value 0.4973, paired t test). The average intra-subject difference in subfoveal CT, the second method, was 2.6 µm and also was not statistically significant (95% CI −21.0, 26.3, p value 0.8211, paired t test).
Other sub-analyses were done on both methods of determining the CT. The measurements were subdivided by encircling element width that would be in direct contact with the sclera to analyze whether CT was affected by the width of the element. There was no correlation identified, with an r squared value of 0.07145, indicating that there was no significant difference in CT when comparing wider versus thinner elements using both methods (Fig. 2, showed data from method 1). The time after surgery was evaluated as a factor in contributing to CT. The difference between eyes was evaluated versus the time after surgery in years using both methods (Fig. 3, showed data from method 1). There was no correlation identified with an r squared value of 0.03638. The age of the patient at the time of the EDI with SD-OCT was analyzed versus the CT (Fig. 4, showed data from method 1). There was a trend towards thinning of the choroid in both the surgical and the control eyes with aging using both methods. The spherical equivalent of phakic patients was analyzed in relation to CT. Cases where the patient was pseudophakic were excluded. In the surgical eyes, there was a trend towards thinner choroid in high myopic patients (Fig. 5a, showed data from method 1). There was no trend noted in the control eyes (Fig. 5b, showed data from method 1). All figures are based on the results from measuring the CT as an average over 6 mm. However, the subfoveal thickness data allow the same conclusions to be drawn (figures not shown). On the surgical eyes, the type of surgery (SB vs. SB with vitrectomy) was also analyzed, and there was no statistically significant difference in CT between either technique.
Discussion
In this study, two methods were used for CT measurement because previous studies measured CT as either an average thickness of a certain length of choroid on either side of the fovea or a point measurement directly under the fovea [10–12, 16]. In our study, both methods produced the same conclusions. There was no statistically significant difference in CT between eyes receiving SB and fellow control eyes. The width of the encircling element that was used also did not affect the CT. Our data suggest that there are no chronic changes in CT at the macula in response to or occurring after an SB surgery as it is performed with modern retinal detachment surgery. This study also confirms previously observed trends in CT including more myopic spherical equivalent directly correlated with decreasing CT and advanced age inversely correlated with CT.
These results may be a reflection of the progress made in surgical repair of retinal detachments. Surgical techniques have evolved, including the size of SB utilized, the degree of indentation, and positioning of the SB. Also, the introduction of pars plana vitrectomy has augmented these changes, allowing for better results with fewer complications. Many of these innovations help to minimize compression of vortex veins in modern day SB repair. Involvement of vortex veins has been thought to contribute to choroidal detachments. Prior studies have suggested that there is a reduced choroidal blood flow in patients who underwent SB, and the width and size of the material may affect a change in the choroidal circulation with increased subfoveal thickness [10].
Previous studies have examined CT after SB surgery with conflicting results. Kimura et al. observed a transient increase in CT after segmental SB. They used a 5 mm silicone sponge (No. 506) and measured the CT directly under the fovea [11]. The average size of the SB was 107° ± 38.8°. They measured CT preoperatively and again at 1 week, 1 month, and 3 months in the operated eyes and non-operated fellow eyes. At 1 week and 1 month, there was a significant increase in CT in the operated eye compared to the preoperative CT in the operated eye. After 3 months there was no significant difference between the preoperative and postoperative subfoveal CT in the operated eye. No significant difference was found between the operated eye compared to the control fellow eye before and 1 week after surgery [11].
Similarly, Miura et al. measured the subfoveal CT after SB surgery without an encircling band [12]. They used either a 7 mm silicone tire (No. 276) or a 5 mm silicone sponge (No. 506). Before surgery, CT measurements were taken in the operated eye and the fellow eye. Measurements were again taken at 1, 2, and 4 weeks after surgery. No significant difference in CT between operated and non-operated eyes was observed before or after SB surgery. In the operated eye, the CT temporarily increased, but returned to normal 4 weeks after surgery [12].
In contrast, Odrobina et al. analyzed the subfoveal CT of 48 patients who underwent SB with encircling band in unilateral macula-off retinal detachments compared to the fellow eye and found a statistically significant increase in subfoveal CT after SB with an encircling band (a 3.5 mm, No. 41 band). It was a retrospective study that measured patients at least 6 months after surgery with the operative eye being compared to the fellow non-operative eye [10].
Our results match the findings of Kimura et al. and Miura et al., showing no significant difference between the operative and fellow eye [11, 12]; however, our study design differed in that patients were measured at least 3 months after surgery, thus, the potential transient increase in CT earlier than 3 months was not assessed. Our study included various encircling bands to explore the effects of the width from a variety of SB. While an SB could potentially compress the vortex veins, leading to reduced blood flow and an increased CT, our results do not support this theory. However, our overall sample size and the sample size for different elements used were small, therefore, it is difficult to draw definitive conclusions due to low statistical power. Another limitation in our study was the lack of data before surgery that could help to understand any possible changes in CT secondary to retinal detachment.
Our findings are contrary to the findings of Odrobina et al. [10]. Both of the methods used in our study measured CT in patients months after SB surgery and lacked a preoperative measurement. While Odrobina et al. used a single type of band, our study included multiple types. A larger study with data before and after surgery using multiple types of encircling elements would help to further clarify if there are any significant differences.
Conclusions
Based on the results in our study, there does not appear to be a significant difference in CT in eyes that have undergone SB when compared to fellow eyes. Furthermore, although the sample size was small, there did not appear to be an association with element/band size and CT.
References
Zhu X, Park TW, Winawer J, Wallman J. In a matter of minutes, the eye can know which way to grow. IOVS. 2005;46:2238–41.
Schaeffel F, Feldkaemper M. Animal models in myopia research. Clin Exp Optom. 2015;98(6):507–17.
Troilo D, Nickla DL, Wildsoet CF. Choroidal thickness changes during altered eye growth and refractive state in primate. IOVS. 2000;41:1249–58.
Li XQ, Larsen M, Munch IC. Subfoveal choroidal thickness in relation to sex and axial length in 93 Danish university students. Invest Ophthalmol Vis Sci. 2011;52:8438–41.
Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009;147:811–5.
Imamura Y, Fujiwara R, Margolis R, et al. Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina. 2009;29:1469–73.
Spaide RF, Koizumi H, Pozzoni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008;146:496–500.
Eshita T, Shinoda K, Kimura I, et al. Retinal blood flow in the macular area before and after scleral buckling procedures for rhegmatogenous retinal detachment without macular involvement. Jpn J Ophthalmol. 2004;48(4):358–63.
Sugawara R, Nagaoka T, Kitaya N, Fujio N, et al. Choroidal blood flow in the foveal region in eyes with rhegmatogenous retinal detachment and scleral buckling procedures. Br J Ophthalmol. 2006;90(11):1363–5.
Odrobina D, Laudańska-Olszewska I, Gozdek P, Maroszyński M, Amon M. Influence of scleral buckling surgery with encircling band on subfoveal choroidal thickness in long-term observations. BioMed Res Int. 2013. doi:10.1155/2013/586894
Kimura M, Nishimura A, Yokogawa H, et al. Subfoveal choroidal thickness change following segmental scleral buckling for rhegmatogenous retinal detachment. Am J Ophthalmol. 2012;154:893–900.
Miura M, Arimoto G, Tsukahara R, Nemoto R, Iwasaki T. Choroidal thickness after scleral buckling. Ophthalmology. 2012;119(7):1497–8.
Parker AJ, Maggiano JM, Aaberg TM, Meredith TA, Reeser FH, Kingham JD. Serous choroidal detachment after retinal detachment surgery. Arch Ophthalmol. 1983;101:1221–4.
Kreiger AE, Hodgkinson BJ, Frederick AR, Smith TR. The results of retinal detachment surgery analysis of 268 operations with a broad scleral buckle. Arch Ophthalmol. 1971;86:385–94.
Rasband WS. ImageJ, U. S. National Institutes of Health, Bethesda, Maryland. 1997–2014. http://imagej.nih.gov/ij/. Accessed 8 Nov 2016.
Branchini L, Regatieri CV, Flores-Moreno I, Baumann B, Fujimoto JG, Duker JS. Reproducibility of choroidal thickness measurements across three spectral domain optical coherence tomography systems. Am Acad Ophthalmol. 2012;119:119–23.
Acknowledgments
Sponsorship and article processing charges for this study were funded by the University of Minnesota Foundation, Minnesota Lions Vision Foundation, and an unrestricted grant to the Department of Ophthalmology and Visual Neurosciences from the Research to Prevent Blindness (RPB), New York, NY, USA.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosures
Sandra R. Montezuma, Peter H. Tang, Cory J. Miller, Alla Kelly, Frederik J.G.M. van Kuijk, Paul Drayna and Dara D. Koozekanani declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethics guidelines
All procedures were in accordance with the ethical standards of the University of Minnesota Institutional Review Board and Ethics Committee on human experimentation and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/B295F0607B6F2E0B.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Montezuma, S.R., Tang, P.H., Miller, C.J. et al. The Effect of Scleral Buckling Surgery on Choroidal Thickness Measured by Enhanced Depth Optical Coherence Tomography: A Cross-Sectional Study. Ophthalmol Ther 5, 215–222 (2016). https://doi.org/10.1007/s40123-016-0060-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-016-0060-8