Abstract
Introduction
Asymptomatic retinal emboli have been associated with diabetes, the presence of significant carotid artery stenosis (≥70%) and an increased risk of stroke. However, there is no clear guidance on how best to investigate and manage patients found to have asymptomatic retinal emboli. Therefore, this study aimed to assess the incidence of significant carotid artery stenosis in patients found to have asymptomatic retinal emboli at diabetic retinopathy screening, and to examine disease management approaches among these patients.
Methods
Patients with new retinal emboli visible at diabetic retinopathy screening were referred to a medical retinopathy clinic and underwent examinations according to a standardized protocol, including carotid Doppler ultrasound and echocardiography. Case notes of patients referred between January 2013 and April 2014 were reviewed. Results of investigations, medication changes and the number of patients who underwent relevant surgical interventions were noted.
Results
Retinal emboli were present in 44 of 13,643 people screened (0.32%). Full data were available for 39 patients. Twenty-two patients (56%) had relevant medication changes. Nine (23%) patients had significant carotid artery stenosis. One underwent carotid endarterectomy, and eight received maximal medical therapy.
Conclusion
Significant carotid artery stenosis was not uncommon in patients with incident retinal emboli at retinal screening. The referral and investigation protocols identified individuals at risk of cerebrovascular events and led to optimized management. Pathways utilizing Doppler ultrasound and physician referral should be more widely implemented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retinal screening provides an opportunity to not only identify diabetic retinopathy, but also to investigate additional retinal pathology such as retinal emboli, which have been associated with an increase in all-cause and stroke-related mortality in the general population [1]. The Beaver Dam Eye Study showed a higher prevalence of retinal emboli in patients with diabetes, with a statistically significant odds ratio of 2.39 [2].
Definitive guidance is lacking regarding the use of investigations such as carotid Doppler ultrasound and echocardiography for patients with asymptomatic retinal emboli [3, 4]. Significant carotid artery stenosis (stenosis ≥70%) has been found in individuals with retinal emboli [3–5], with a reported risk of stroke of 3.6–13% per year, depending on the presence or absence of symptoms [6, 7]. In addition, there are no clear guidelines as to the optimal management of patients with asymptomatic retinal emboli found on routine retinal imaging. The current literature suggests that this group of patients should undergo an assessment of cardiovascular risk factors and that physicians should be involved in the care of these patients [3, 4]. However, implementation of this approach appears to be limited.
Therefore, this study aimed to assess the incidence of significant carotid artery stenosis among diabetic patients with asymptomatic retinal emboli found at annual photographic screening, and to examine the investigations and disease management carried out as a result. Such information may help to determine monitoring and disease management approaches that are most beneficial in the care of this group of patients.
Methods
Referral Pathway
Annual digital retinal photography for all patients with diabetes was established in the Sunderland and South Tyneside area in 2002. Images are graded according to national guidelines based on the severity of diabetic retinopathy. If a retinal embolus is identified, the patient is referred to a specialist physician-led clinic. Patients are assessed to determine the presence of symptoms as a result of the retinal embolus or any carotid bruits, and then under appropriate examinations, including carotid Doppler ultrasound and echocardiography in all patients, according to a defined protocol. If a patient is found to have stenosis of 70% or greater in one carotid artery, a multidisciplinary team consisting of vascular surgeons, radiologists, vascular ultrasound technicians, and stroke and diabetes physicians discusses the possibility of surgical intervention, including carotid endarterectomy or stenting. Twenty-four hour ambulatory blood pressure monitoring (24-h ABPM) is obtained if blood pressure in the clinic is suboptimal.
Study Design
The study was designed as a retrospective case note review of patients referred to this service between January 2013 and April 2014. Data were collected from medical notes and hospital e-records using a pre-designed pro forma, which included risk factors for cardiovascular disease, cardiovascular comorbidity, previous cerebrovascular events with corresponding Doppler results, baseline blood pressure (BP), body mass index (BMI), glycated hemoglobin (HbA1c), lipid profile, 24-h ABPM, and outcomes after discussion with the multidisciplinary cardiovascular assessment team. Results of any relevant imaging studies were noted, as well as changes in medical treatment and surgical interventions. In order to determine whether individuals with elevated blood pressure, HbA1c or total cholesterol received appropriate medication changes, these parameters were defined as blood pressure greater than 140/90 mmHg, HbA1c greater than 53 mmol/mol and total cholesterol greater than 5 mmol/L.
Patients who did not attend the clinic on three occasions were excluded. The study was designated as a service review and, as such, did not require ethical approval. This article does not contain any new studies with human or animal subjects performed by any of the authors.
Incidence of Retinal Emboli
To determine the incidence of retinal emboli among individuals with diabetes in the local area, all cases identified between January 2013 and March 2014 were used as the numerator. The number of patients screened during the study period was used as the denominator.
Statistics
Mean values and standard deviations for baseline characteristics of the cohort were calculated using Microsoft Excel software.
Results
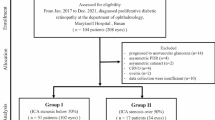
Forty-five eyes of 44 patients were identified from screening images as having new retinal emboli during the study period, all of whom had type 2 diabetes. Five patients were excluded from the study: four failed to attend the clinic, and one patient died of pneumonia during follow-up. Therefore, data from 39 patients were analyzed. A retinal embolus was present in the right eye in 25 patients and in the left eye in 14. Three patients had multiple emboli. Two patients had two emboli in one eye, and another patient had an embolus in both the left and right eyes. Further details of the cohort are given in Table 1.
During the course of the study, 13,643 individuals underwent retinal screening in the trust, which resulted in an incidence of retinal emboli in individuals with diabetes in Sunderland of 0.32% (32 in 10,000). At the initial clinic appointment, all patients were confirmed to be asymptomatic, although one patient experienced an episode of amaurosis fugax while under medical clinic review. During the study period, there were no separate referrals from the ophthalmology department as a result of detecting asymptomatic retinal emboli in diabetic patients.
Seventy-two percent (28/39) of the patients were men. Twenty-one percent (8/39) were current smokers, and 8% (3/39) were ex-smokers. Ischemic heart disease was present in 12/39 (31%), with 6/39 (12%) having previously undergone coronary artery bypass surgery. Twelve percent had a history of myocardial infarction, and 6/39 (12%) had suffered a stroke prior to the detection of the retinal embolus.
Eight patients (21%) were found to have significant carotid artery stenosis or complete occlusion on carotid Doppler ultrasound (Table 2). Doppler ultrasound was conducted at a mean of 13 days after the first appointment. Nine patients underwent carotid angiography after Doppler ultrasound to confirm the level of stenosis. Five of the nine angiograms were performed at the recommendation of the cardiovascular assessment team. The other four angiograms were performed to confirm complete occlusion in one carotid artery, and these patients were referred directly from the clinic. One angiogram identified more extensive stenosis than was found on the Doppler ultrasound. This patient had recurrent transient ischemic attacks (TIAs) after medical clinic review commenced, and was found to have 50–60% carotid artery stenosis on Doppler ultrasound. However, the angiogram subsequently showed occlusion of 80%, and the patient was then considered for carotid endarterectomy. Therefore, one patient was found to have significant carotid artery stenosis through angiography rather than Doppler ultrasound, meaning that nine patients (23%) overall were found to have significant carotid artery stenosis. All 44 patients received an echocardiogram, 43 of which were normal. One showed findings not considered relevant to embolic disease, but further cardiac investigations were carried out.
One patient underwent carotid endarterectomy (Table 2). This patient was initially found to have asymptomatic carotid stenosis and an asymptomatic retinal embolus. After surgical assessment, endarterectomy was discussed, but the patient declined intervention and was managed medically. Six months later, however, he experienced a retinal TIA, was re-referred, and underwent endarterectomy 9 days later.
The four patients considered for carotid stenting or carotid endarterectomy all had significant carotid artery stenosis without complete occlusion. One patient underwent carotid endarterectomy. Two patients declined surgery, and another was unable to lie flat to undergo angiography to further assess the extent of carotid artery stenosis. Therefore, these three patients received maximal medical therapy. The five patients with complete occlusion of one carotid artery also received maximal medical therapy (Table 2).
In total, 56% of the group had one or more changes made to medication (Table 2). The most common medication change was the addition of an antiplatelet agent, which occurred in 7/39 (18%) patients (Table 3). Twenty-one percent (8/39) received changes to lipid-lowering medication, 12/39 (31%) had changes to anti-hypertensive medication, and 6/39 (16%) had changes to diabetes medications (Table 3). Seven individuals underwent 24-h ambulatory blood pressure monitoring (24-h ABPM), with four patients receiving changes to anti-hypertensive medication as a result and three patients having normal 24-h ABPM.
We also examined the number of individuals with a history of stroke or TIA and the number of individuals who suffered strokes or TIAs after the detection of the retinal embolus. In total, ten patients (26%) experienced a cerebrovascular event either before or after detection of the retinal embolus. Four patients had a stroke or TIA between the time they were first seen and the time they were discharged from the clinic, and all were individuals who were found to have significant stenosis before having a stroke or TIA. The mean duration of clinic follow-up was 8 months. No patients suffered a stroke or TIA between discharge and case note review.
Discussion
Referral Pathway
The results of our study suggest that a targeted medical evaluation and optimization of cerebrovascular risk factors should be carried out in individuals with asymptomatic retinal emboli found on retinal screening. Unlike several other reported pathways [3–5], our pathway leads to physician referral from retinal screening, which avoids delay in implementing any necessary medical or surgical management for these patients. Hadley et al. reported that detection of retinal emboli through retinal screening led to a direct referral for carotid Doppler ultrasound and subsequent multidisciplinary review with ophthalmologists, radiologists and vascular surgeons to consider surgical options [5]. This approach does result in individuals receiving surgery that they may not otherwise have had. Referral of individuals with asymptomatic retinal emboli to ophthalmology departments also may not be useful [4]. Neither of these approaches directly addresses the potential need to improve a patient’s medical management. Ahmed et al. [3] described a pathway whereby individuals found to have asymptomatic retinal emboli at retinal screening were referred back to their primary care physicians, which did lead to changes in medical therapy, and a similar proportion of patients underwent carotid endarterectomy, but there was no standard protocol for investigation or management once the individual had been referred to primary care [3]. In contrast, our pathway offers a standardized approach to the investigation and management of this patient group.
Incidence and Prevalence of Retinal Emboli
The incidence of retinal emboli among our patient cohort was 0.32% over a period of 15 months. Other studies have reported a cumulative incidence of 1.5–2.9% over 10 years [8, 9], which is similar to our finding. In the first year of the screening program, the prevalence of retinal emboli in the local area was 1.5% (personal communication with DHW Steel). The prevalence of retinal emboli has been examined in several groups, and ranged from 0.4% to 1.9% [2, 3, 5, 10–12]. However an important characteristic of this cohort is that all patients had diabetes, which was shown to affect the prevalence of retinal emboli in a large population study [2]. Retinal emboli were reported at a prevalence of 0.85% [5] and 1.9% [3] in two studies based on retinal screening populations, which is also broadly similar to our prevalence for the local area.
Twenty-nine percent of the cohort was either a current or ex-smoker (Table 1). Because smoking has been associated with an increased incidence of retinal emboli [11, 12], smoking cessation services should be included in clinical pathways. Thirty-eight percent of our patients had experienced myocardial infarction or ischemic heart disease, both of which have also been associated with an increased prevalence of retinal emboli [13].
Utility of Investigations
The proportion of the cohort found to have significant carotid artery stenosis on carotid Doppler ultrasound was broadly similar to that in other studies, which reported an incidence of 12.5% [5] and 22% [3]. The lower incidence found by Hadley et al. [5] could reflect the larger number of patients in the study. Carotid artery stenosis of 70% or greater is considered significant, and carotid endarterectomy is reported to be of benefit in reducing the risk of stroke if the patient is symptomatic and the carotid artery is not fully occluded [14]. Carotid endarterectomy in patients with one fully occluded carotid artery was shown to provide no benefit over maximal medical therapy in two randomized controlled trials [14–16]. For patients with non-significant stenosis and a recent history of TIA or stroke, maximal medical therapy is recommended, given the risk of further stroke caused by surgery [14–16]. In the Asymptomatic Carotid Surgery Trial, carotid endarterectomy was shown to reduce the risk of stroke in asymptomatic individuals under the age of 75 with significant carotid artery stenosis [17].
Cardiac sources of retinal emboli are usually calcified valves or rheumatic heart disease [18, 19]. In our study group, we found no abnormalities on echocardiography that could be considered a potential source for retinal emboli. Other studies have not used echocardiography in all patients [3–5]. In one study, valvular disease—which could act as a source—was found on echocardiography in about 9% of patients with retinal emboli [3]. Our study suggests that echocardiography may not be required in all patients with retinal emboli. However, the best method for selecting patients to receive echocardiography is not clear.
The existing literature suggests that angiography has not been used extensively for investigation of individuals with retinal emboli. Confirmation of stenosis findings using angiograms may be warranted for patients with 60% stenosis or more on Doppler ultrasound, in order to prevent individuals with significant stenosis from being missed and therefore not being considered for further surgical intervention. Similarly, angiography may be useful for confirmation of total occlusion.
There are several limitations to this study. The number of patients studied was small, and the period during which patients with incident retinal emboli were identified was short. Therefore, the management of relatively few patients forms the basis of recommendations presented here. The follow-up time for all patients after discharge was brief, and other cerebrovascular events after discharge might have been identified if follow-up periods had been longer and had been the same length of time for all individuals.
Conclusions
Here we propose a pathway for the investigation and management of individuals with diabetes found to have retinal emboli on annual retinal screening. This pathway enables the identification of individuals eligible for surgical intervention before a cerebrovascular event occurs. It is important that individuals with asymptomatic retinal emboli are reviewed by a physician to improve medical management of cardiovascular risk factors. In addition, Doppler ultrasound should be performed for every patient, because significant carotid artery stenosis could be found, and may be amenable to surgical or medical management. Echocardiography did not show obvious sources of retinal emboli, suggesting that this investigation may not always be necessary. Larger studies with long-term follow-up are needed to further assess the utility of the proposed pathway.
References
Wang JJ, Cugati S, Knudtson MD, Rochtchina E, Klein R, Klein BEK, et al. Retinal arteriolar emboli and long-term mortality: Pooled data analysis from two older populations. Stroke. 2006;37(7):1833–6.
Klein R, Klein BE, Jensen SC, Moss SE, Meuer SM. Retinal emboli and stroke: the beaver dam eye study. Arch Ophthalmol. 1999;117(8):1063–8.
Ahmed R, Khetpal V, Merin LM, Chomsky AS. Case series: Retrospective review of incidental retinal emboli found on diabetic retinopathy screening: Is there a benefit to referral for work-up and possible management? Clin Diabetes. 2008;26(4):179–82.
Wilde C, Rathore D, Chen H-C. A retrospective review of the management of asymptomatic retinal emboli identified during diabetic retinopathy screening: a case of inappropriate referral? Br J Diabetes Vasc Dis. 2010;10(3):126–9.
Hadley G, Earnshaw JJ, Stratton I, Sykes J, Scanlon PH. A potential pathway for managing diabetic patients with arterial emboli detected by retinal screening. Eur J Vasc Endovasc Surg. 2011;42(2):153–7.
North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325(7):445–53.
Inzitari D, Eliasziw M, Gates P, Sharpe BL, Chan RKT, Meldrum HE, Barnett HJ. The Causes and Risk of Stroke in Patients with Asymptomatic Internal-Carotid-Artery Stenosis. N Engl J Med. 2000;342(23):1693–701.
Cugati S, Jie JW, Rochtchina E, Mitchell P. Ten-year incidence of retinal emboli in an older population. Stroke. 2006;37(3):908–10.
Klein R, Klein BEK, Moss SE, Meuer SM. Retinal emboli and cardiovascular disease: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc. 2003;101:173–80 (discussion 180–2).
Cheung N, Lim L, Wang JJ, Islam FMA, Mitchell P, Saw SM, et al. Prevalence and Risk Factors of Retinal Arteriolar Emboli: The Singapore Malay Eye Study. Am J Ophthalmol. 2008;146(4):620–4.
Hoki SL, Varma R, Lai MY, Azen SP, Klein R. Prevalence and Associations of Asymptomatic Retinal Emboli in Latinos: The Los Angeles Latino Eye Study (LALES). Am J Ophthalmol. 2008;145(1):143–8.
Mitchell P, Wang JJ, Li W, Leeder SR, Smith W. Prevalence of Asymptomatic Retinal Emboli in an Australian Urban Community. Stroke. 1997;28(1):63–6.
Klein R, Klein BEK, Moss SE, Meuer SM. Retinal Emboli and Cardiovascular Disease. 2013;121:1063–8.
Rerkasem K, Rothwell PM. Carotid endarterectomy for symptomatic carotid stenosis. Cochrane Database Syst Rev. 2011. doi:10.1002/14651858.CD001081.pub2.
Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998;351(9113):1379–87.
Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, Rankin RN, Clagett GP, Hachinski VC, Sackett DL, Thorpe KE, Meldrum HE, Spence JD. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339(20):1415–25.
Halliday A, Mansfield A, Marro J, Peto C, Peto R, Potter J, et al. Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet. 2004;363(9420):1491–502.
Russell RW. The source of retinal emboli. Lancet. 1968;2(7572):789–92.
Younge BR. The significance of retinal emboli. J Clin Neuroophthalmol. 1989;9(3):190–4.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Afsara Ahmmed, Peter Carey, David Steel and Teresa Sandinha have nothing to disclose.
Compliance with Ethics Guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhance content for this article go to http://www.medengine.com/Redeem/78D4F060238B7888.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ahmmed, A.A., Carey, P.E., Steel, D.H.W. et al. Assessing Patients with Asymptomatic Retinal Emboli Detected at Retinal Screening. Ophthalmol Ther 5, 175–182 (2016). https://doi.org/10.1007/s40123-016-0055-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-016-0055-5