Abstract
Introduction
This study evaluated the usefulness of rigid endoscopy placed on the corneal surface to observe the peripheral retina.
Methods
The authors studied 15 eyes in 15 patients (12 men, 3 women; mean age 55.9 years; range 22–74 years) that underwent vitreous surgery at the Department of Ophthalmology at Saga University Hospital. With patients in a supine position, after topical anesthesia, an eye cup was placed between the eyelids and filled with hydroxyethyl cellulose solution and physiologic saline. With a rigid endoscope placed near the corneal surface, the target areas were then observed and recorded. The usefulness of rigid endoscopy to observe the peripheral retina was evaluated based on differences due to lens status and pupil size.
Results
In seven aphakic eyes, irrespective of pupil size, the peripheral retina could be observed up to the entire ora serrata (all quadrants). In eight eyes implanted with an intraocular lens, the observable area changed with pupil size and anterior capsulorrhexis size.
Conclusion
This technique using rigid endoscopy was simple to manipulate and useful for observing and recording the peripheral retina. In particular, in aphakic eyes, irrespective of pupil size, the retina could be observed to the ora serrata.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The basics of ophthalmic evaluation include detailed observation and recording of intraocular findings. Among retinal diseases, marked advances have been made in observing macular lesions, and testing can be performed rapidly and noninvasively [1, 2]. However, to observe the peripheral retina, particularly near the ora serrata, testing depends on the skill of the examiner; for example, by slit-lamp microscopy using a contact lens with a depressor, or binocular indirect ophthalmoscopy using scleral depression [3–5]. Slit-lamp microscopy is difficult in children and patients who have difficulty sitting, and with binocular indirect ophthalmoscopy, differences in diagnostic ability among examiners are substantial, and saving the findings as image recordings is difficult.
Guyomard et al. [6] observed animal eyes and reported topical endoscopy fundus imaging (TEFI) using a rigid endoscope. Using this technique, the iridocorneal angle and peripheral retina in small animals, which have previously been difficult to observe and record, can now be visualized. Hirata and Okinami also reported its usefulness for imaging retinal findings in rabbit eyes and as an observation system during surgery [7]. In the present study, the authors modified this technique and investigated its clinical usefulness for postoperative retinal evaluation in patients with retinal detachment and proliferative retinopathy (proliferative vitreoretinopathy, proliferative diabetic retinopathy), in whom examination of the peripheral retina is necessary.
Methods
Patients
This study included 15 eyes in 15 patients (randomly selected; 12 men, 3 women; mean age 55.9 years; range 22–74 years) that underwent vitreous surgery at the Department of Ophthalmology at Saga University Hospital. The underlying disease requiring surgery was rhegmatogenous retinal detachment (seven eyes), proliferative vitreoretinopathy (six eyes), and proliferative diabetic retinopathy (two eyes). Lens status was aphakia (seven eyes) and intraocular lens (IOL) implantation (eight eyes). The study protocols were approved by the Clinical Research Ethics Committee at Saga University. Patients were given a full written explanation about the usefulness of this technique and potential complications, and each provided written informed consent.
Modified Method of Topical Endoscopic Observation
For observation of the peripheral retina using the rigid endoscope, the authors modified a previously reported method [6, 7]. The rigid endoscope system was similar to that reported previously. For this study, the authors used a 6.0 cm × 4 mm (outer diameter) rigid endoscope for otoscopic use (1215AA; Karl Storz, Tuttlingen, Germany). The tip has a crescent-shaped light and is used by connecting it to a xenon light source (Xenon Nova 175; Karl Storz, Tuttlingen, Germany). The endoscope was connected to a digital camera utilizing a 400,000-pixel charge-coupled device (CCD) image sensor unit (Telecam-C and Telecam DXII; Karl Storz, Tuttlingen, Germany), and was connected to a monitor.
Although the xenon light source used in this study is widely used in clinical settings, this equipment is not adjusted for ophthalmic use. Therefore, the authors determined an acceptable power of light (below the maximum permissible exposure ≅1 mW/cm2) using a xenon light source used in a standard vitrectomy. As a control, the spectral irradiance of the xenon light source (Xenon BrightStar illumination system; DORC, Zuidland, The Netherlands) was measured using a spectroradiometer (USR-30; Ushio Inc., Yokohama, Japan) at a distance of 20 mm from the tip of the 23-gauge light pipe to the surface of the light receiving unit at 50%, 80%, and 100% of maximal strength equipped with a 420 nm cut-off filter (Fig. 1; blue, light blue, and purple, respectively). Then, in order to determine the appropriate condition for this study, the strength of the spectral irradiance of the xenon light source used in this study was adjusted not to exceed the peak of the light strength at 50% of the control xenon light source by turning the setting dial (Fig. 1; green). Moreover, a filter with a 420 nm cut-off filter (Sharp Cut Filter L42; Hoya Candeo Optronics, Toda, Japan) was attached to prevent the potential phototoxicity of the short-wavelength light (Fig. 1; red). The sum total examination time was set to less than 7 min for each examination. In addition, the absence of thermal injury of the cornea due to a temperature increase was confirmed beforehand by preliminary testing [7].
Spectral irradiance of the xenon lamp used in this study and that used for a standard vitrectomy as a control. Purple spectral irradiance of the control xenon light source (Xenon BrightStar illumination system; DORC, Zuidland, The Netherlands) at maximal strength equipped with a 420 nm cut-off filter. Light blue 80% of maximal strength of the control light source. Blue 50% of maximal strength of the control light source. Green spectral irradiance of the xenon light source used in this study (Xenon Nova 175; Karl Storz, Tuttlingen, Germany). The strength of the light was adjusted not to exceed the peak of that at 50% of the control xenon light source. Red spectral irradiance of the xenon light source used in this study at the same setting as the green and with a 420 nm cut-off filter
Patients were placed in the supine position on a bed, and topical anesthetic was instilled into the eye to be examined. In the eye to be examined, an eye cup for use with ultrasound biomicroscopy was placed between the eyelids and, to protect the corneal surface and to create an interface that would improve the quality of the image, the eye cup was filled with hydroxyethyl cellulose solution (Scopisol solution; Senju Pharmaceutical Co., Ltd., Osaka, Japan) and 1–2 mL of physiologic saline. The endoscope was placed in proximate contact with the cornea, and was directed such that the entire peripheral retina could be observed. In addition, while observing with a monitor, the image was recorded (Fig. 2).
Schematic diagram of the examination set-up. An eye cup is placed on the eye to be examined, and the cup is filled with hydroxyethyl cellulose solution and physiologic saline. The rigid endoscope is placed near the eye for observation. The image is displayed on a monitor and saved as a video. CCD charge-coupled device image sensor unit
The recorded data was downloaded to a computer, the necessary scenes were captured, and still images were prepared. Based on the acquired data, differences in the observable area of the peripheral retina were evaluated according to lens status and pupil size. Possible adverse events, such as damage of the corneal epithelium or discomfort during examination, were also recorded.
Results
A total of 15 eyes in 15 patients were examined for observation of the peripheral retina in this study. No complications due to examination occurred in any patients. Due to observation of the peripheral retina alone, complaints of mild photophobia were seen in only two patients, and there were no patients in whom examination could not be performed.
In aphakic eyes (seven eyes), irrespective of pupil size, the entire ora serrata (all quadrants) could be observed (Table 1). By manipulating the endoscope, observation of the peripheral retina to the entire ora serrata was possible (Fig. 3). The observable area was unrelated to pupil size; thus, examination of the postoperative course, for example, of rhegmatogenous retinal detachment from a tear in the ora serrata, was simple (Fig. 4).
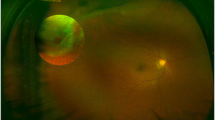
Rigid endoscopic image of proliferative diabetic retinopathy in Case 2. a Observation in only one direction: the ora serrata and peripheral retina are clearly visualized. This demonstrates that retinal photocoagulation in the periphery has been performed. b Composite photograph of endoscopic findings in entire periphery. Observation of the entire ora serrata is possible
Anterior eye findings and rigid endoscopic image of retinal detachment due to giant retinal tear in Case 7. a Anterior eye findings: dilated pupil size of 4.5 mm. With examination of the retina by indirect ophthalmoscopy, the most peripheral regions of the retina cannot be observed, and retinal photography is difficult. b Endoscopic findings: observation to the ora serrata is possible. Posttreatment findings of the causative tear can clearly be seen
On the other hand, among IOL-implanted eyes (eight eyes), the entire ora serrata could be confirmed in only two eyes. The observable areas changed based on pupil size, IOL diameter, anterior capsulorrhexis size, and lens capsule opacification. In particular, because an opacified lens capsule greatly affected visibility, with larger capsulorrhexis size, observation to the periphery was possible (Fig. 5). However, in all cases, at a distance of 2–3 disk diameters from the equator, the periphery could be observed (Table 1). Observation of causative tears and photocoagulation sites was possible in all cases. In addition, even in cases with corneal opacification, by viewing from a site without opacification, retinal observation was possible (Fig. 6).
Rigid endoscopic images of retinal detachment in Cases 9 and 10. a Endoscopic image in Case 9: from the edge of the intraocular lens (7 mm three-piece acrylic), visualization to the ora serrata is difficult, but the sites of treatment of the causative tear and subretinal fluid drainage can be observed in detail. b Endoscopic image in Case 10: lateral to the edge of the intraocular lens (6 mm one-piece acylic), the ora serrata can be seen. The retina below the lens capsule opacification is difficult to visualize, but by changing the direction of the endoscope, it can be observed
Anterior eye findings and rigid endoscopic image of proliferative diabetic retinopathy in Case 15. a Anterior eye findings: dilated pupil size of 4.5 mm. Because of corneal opacification, with examination of the retina by indirect ophthalmoscopy, detailed visualization is not possible, and retinal photography is difficult. b Endoscopic findings: with endoscopic observation of the retina through an area of transparent cornea, the peripheral retina, including photocoagulation spots, is observed
Discussion
This study investigated the usefulness of rigid endoscopy for examination of the peripheral retina. Due to the fact that the rigid endoscope permits wide-angle observation and a wide depth of field, manipulation is simple, and much information can be obtained. Compared with the existing procedures including slit-lamp microscopy using a contact lens with a depressor, or binocular indirect ophthalmoscopy using scleral depression, advantages of the examination procedure using rigid endoscopy include: (1) no need for slit-lamp microscopy; (2) no complex technique is required; (3) examination in patients unable to remain sitting is possible; (4) images can be recorded, and any images can be extracted; and (5) the apparatus is inexpensive [6–8].
In this study, with examination using a rigid endoscope, manipulation was simple, and the peripheral retina could be observed and recorded. In particular, in aphakic eyes, irrespective of pupil size, observation up to the entire ora serrata (all quadrants) was possible. For postoperative evaluation of retinal detachment patients, adequate observation is essential; not only of the causative tear, but also to assess any new breaks, or new break formation associated with traction of the retina due to residual vitreous. In diseases where more vitreoretinal traction is involved, including proliferative vitreoretinopathy and proliferative diabetic retinopathy; the recording of retinal changes over time is useful in judging the need for additional treatment and can lead to early detection of complications.
However, this method does have some limitations. Although not fully evaluated in the present study, in phakic eyes of elderly patients retinal translucency can decrease due to light scattering from the examination light. Therefore, preoperative evaluation of the peripheral retina and causative tears in elderly and cataractous eyes seems difficult. Moreover, the possibility of phototoxicity and risk of corneal injury due to long-term observation may require further investigation.
Conclusion
Advances in endoscopes have led to improved resolution, less invasiveness, and greater functionality. To date, in the field of ophthalmology, endoscopy has been limited to fiber optic endoscopes used for insertion into the eye through scleral incisions during surgery [9], or used in lacrimal duct evaluation or treatment [10, 11]. This observation technique is a novel method in terms of looking into the eye from the corneal surface. In the future, with improved illumination systems, stereoscopic-vision rigid endoscopes, and image processing methods, the possibilities will greatly expand [12–14].
References
Hee MR, Izatt JA, Swanson EA, et al. Optical coherence tomography of the human retina. Arch Ophthalmol. 1995;113:325–32.
Zhang Y, Rha J, Jonnal R, Miller D. Adaptive optics parallel spectral domain optical coherence tomography for imaging the living retina. Opt Express. 2005;13:4792–811.
Havener WH. Schepens’ binocular indirect ophthalmoscope. Am J Ophthalmol. 1958;45:915–8.
Hovland KR, Elzeneiny IH, Schepens CL. Clinical evaluation of the small-pupil binocular indirect ophthalmoscope. Arch Ophthalmol. 1969;82:466–74.
Schepens CL, Bahn GC. Examination of the ora serrata: its importance in retinal detachment. Arch Ophthalmol. 1950;44:677–90.
Guyomard JL, Rosolen SG, Paques M, et al. A low-cost and simple imaging technique of the anterior and posterior segments: eye fundus, ciliary bodies, iridocorneal angle. Invest Ophthalmol Vis Sci. 2008;49:5168–74.
Hirata A, Okinami S. Viability of topical endoscopic imaging system for vitreous surgery in rabbit eyes. Ophthal-Mic Surg Lasers Imaging. 2012;43:e64–7.
Paques M, Guyomard JL, Simonutti M, et al. Panretinal, high-resolution color photography of the mouse fundus. Invest Ophthalmol Vis Sci. 2007;48:2769–74.
Norris JL, Cleasby GW, Nakanishi AS, Martin LJ. Intraocular endoscopic surgery. Am J Ophthalmol. 1981;91:603–6.
Gonnering RS, Lyon DB, Fisher JC. Endoscopic laser-assisted lacrimal surgery. Am J Ophthalmol. 1991;111:152–7.
Metson R. Endoscopic surgery for lacrimal obstruction. Otolaryngol Head Neck Surg. 1991;104:473–9.
Kim K, Kubota M, Ohkawa Y, et al. A novel ultralow-illumination endoscope system. Surg Endosc. 2011;25:2029–33.
Zobel J. Basics of three-dimensional endoscopic vision. Endosc Surg Allied Technol. 1993;1:36–9.
Eguchi S, Kohzuka T, Araie M. Stereoscopic ophthalmic microendoscope system. Arch Ophthalmol. 1997;115:1336–8.
Acknowledgments
This study was supported by “Japan Society for the Promotion of Science Grant-in-Aid for Scientific Research (C)”. Dr. Hirata is the guarantor for this article, and takes responsibility for the integrity of the work as a whole.
Conflict of interest
The authors have no conflicts of interest to disclose.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hirata, A., Ishikawa, S. & Okinami, S. Observation of Peripheral Retina by Topical Endoscopic Imaging Method—A Preliminary Study. Ophthalmol Ther 2, 11–18 (2013). https://doi.org/10.1007/s40123-012-0008-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-012-0008-6