Abstract
Introduction
Chronic low back pain (cLBP) is a problem globally, creating a tremendous economic burden. Since conventional treatments often fail, various forms of electrical stimulation have been proposed to improve function and decrease pain. Patient-reported outcome measures (PROMs) have not been adequately reported in the electrical stimulation literature.
Methods
A retrospective independent statistical analysis was conducted on PROMs data for users of H-Wave® device stimulation (HWDS) collected by the device manufacturer over a period of 4 years. Final surveys for 34,192 pain management patients were filtered for pain chronicity limited to 3–24 months and device use of 22–365 days, resulting in 11,503 patients with “all diagnoses”; this number was then reduced to 2711 patients with nonspecific cLBP, sprain, or strain.
Results
Reported pain was reduced by 3.12 points (0–10 pain scale), with significant (≥ 20%) relief in 85.28%. Function/activities of daily living (ADL) improved in 96.36%, while improved work performance was reported in 81.61%. Medication use decreased or stopped in 64.41% and sleep improved in 59.76%. Over 96% reported having expectations met or exceeded, service satisfaction, and confidence in device use, while no adverse events were reported. Subgroup analyses found positive associations with longer duration of device use, home exercise participation, and working, whereas older age and longer pain chronicity resulted in reduced benefit. Similar analysis of the larger all-diagnoses cohort demonstrated near-equivalent positive outcomes.
Conclusion
Treatment outcomes directly reported by cLBP HWDS patients demonstrated profound positive effects on function and ADL, robust improvement in pain perception, and additional benefits like decreased medication use, better sleep, and improved work performance, representing compelling new evidence of treatment efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
Chronic low back pain remains difficult to treat, but responds well to H-Wave® device stimulation (HWDS) for most patients. |
What was learned from the study? |
Over 96% of patients self-reported improvement in function/activities of daily living (ADL). |
Over 85% reported significant (≥ 20%) pain relief, averaging more than 3 points (0–10, visual analogue scale). |
Other demonstrated benefits include decreased medication use, better sleep, and improved work performance. |
Introduction
Musculoskeletal (MSK) disorders, primarily resulting from low-energy injury, with associated inflammation of muscles, tendons, ligaments, joints, and nerves, ultimately impact most adults and pose a significant economic burden on healthcare systems worldwide [1,2,3]. Low back pain (LBP), the most common MSK disorder, is frequently associated with functional deficits including reduced range of motion (ROM), difficulty with activities of daily living (ADL), physical disability, and psychological disorders [1,2,3,4]. Despite significant advances in the prevention and treatment of spinal disorders, chronic LBP (cLBP) persists as one of the most problematic MSK challenges across the globe [5].
Conventional treatments for cLBP have included the use of pharmacological agents like nonsteroidal anti-inflammatory drugs and opioids, as well as non-pharmacological approaches including activity modification, physical therapy, cognitive behavioral therapy, complementary and alternative medicine, and various invasive interventions (e.g., radio-frequency ablation) [6]. Traditional therapies for cLBP have notable deficiencies and unsolicited adverse effects, typically providing only temporary pain relief and failing to target the causal pathology [7].
There has been increasing interest in applying different forms of electrical stimulation (ES) for cLBP, including transcutaneous electrical nerve stimulation (TENS), neuromuscular electrical stimulation (NMES), and H-Wave® device stimulation (HWDS), to improve function and/or decrease pain. While TENS is the most widely used form of ES, most studies have reported either very little or only slight pain improvement over the short term [8]. The majority of TENS studies with adequate sample size were categorized as very low- or low-quality evidence, demonstrating no improvement in physical function, psychological parameters, or overall quality of life (QoL) [8]. In contrast, most HWDS studies, with low- to moderate-quality evidence, have demonstrated significant decreases in pain and medication use, with improvement in physical function and overall QoL [8,9,10,11]. However, there have been no HWDS studies with adequate sample size to evaluate treatment efficacy more specifically in patients experiencing nonspecific cLBP.
HWDS, a unique form of transcutaneous ES, emits a proprietary, biphasic, exponentially decaying waveform [8,9,10,11]. An H-Wave® device delivers 0–35 mA current and 0–35 V voltage at a load of 1000 Ω, with an ultra-long pulse duration of 5000 µs [8,9,10,11]. It consists of two treatment components, low-frequency (2 Hz) and high-frequency (60 Hz), with two dual modes allowing either two low- or two high-frequency or combined low- and high-frequency treatments [8,9,10,11]. The preclinical studies for HWDS, summarized in a thorough review [9], underlined several mechanisms of action. The low-frequency component results in additive physiologic effects including (1) stimulation of voluntary contraction of small, slow-twitch skeletal red muscle fibers leading to non-fatiguing low-tension contractions; (2) increased blood flow through nitric oxide mediated vasodilation; (3) angiogenesis; (4) and increased rhythmic drainage of lymphatic vessels by stimulation of voluntary contraction of smooth muscles fibers leading to removal of protein and fluid waste from areas of inflammation, thereby restoring tissue homeostasis [9]. The high-frequency component has been shown to result in significant analgesia via additive suppressive effects on nerve action potentials through deactivation of the sodium channel pump, a physiological effect which persists after treatment cessation [9].
Patient-reported outcome measures (PROMs) have gained widespread interest as healthcare continues to transition from volume to value, particularly as a key indicator of treatment quality from the patient’s perspective [12]. The American Academy of Orthopaedic Surgeons, like other specialty organizations, has developed position statements regarding principles for MSK PROMs development and implementation [12]. PROMs measure subjective elements of patients’ conditions, including QoL, pain intensity, activity limitations, participation restrictions, and satisfaction or adherence to treatment [12]. While initially applied in pharmacological research, over the past two decades PROMs data have been increasingly used to assess the effects of various treatments and quality of care from a health economics and policy perspective, being recognized as important by the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) [13]. PROMs data have been minimally reported for various forms of ES, where no consensus regarding the effectiveness of TENS (as an example) for chronic MSK disorders or LBP has been established. One TENS study using a standardized PROMs tool, the World Health Organization International Classification of Functioning, Disability and Health (ICF), found a disappointing mismatch between measured outcomes and other perceived benefits noted by experienced device users, suggesting a need to use more proprietary, condition-specific PROMs [14].
The goal of this large retrospective PROMs survey study is to evaluate the efficacy and safety of HWDS in a cohort of nonspecific cLBP patients. Primary outcome measures include the impact of HWDS on pain, function/ADL, medication use, and sleep. Secondary outcomes include the effects of HWDS on work performance and preference for HWDS over prior treatments, as well as expectations, service satisfaction, and confidence with device usage. Based on previous study outcomes, it is hypothesized that HWDS for cLBP is safe and results in clinically significant and robust pain reduction, with concomitant improvements in function/ADL and sleep quality, as well as reduction in pain medication usage.
Methods
Data Source and Study Design
This is a retrospective analysis of HWDS PROMs survey data routinely collected by Electronic Waveform Lab, Inc. (Huntington Beach, CA, USA) involving a cohort of 34,192 pain management patients. Only final patient surveys were analyzed, to avoid reporting duplications. The 4-year data were consecutively collected between January 1, 2019, and December 31, 2022. No protected health information was collected, and the study was approved by the South Texas Orthopaedic Research Institute Institutional Review Board (number: STORI09192023-1, dated September 19, 2023). This PROMs study focuses primarily on patients prescribed an H-Wave® device for nonspecific cLBP, with reported symptom chronicity from date of injury until initiation of HWDS between 3 and 24 months (90–730 days), duration of HWDS treatment between 22 and 365 days, and having a diagnosis of low back pain, sprain or strain [sprain of ligaments of lumbar spine—initial and subsequent encounters; strain of muscles, fascia and tendons of lower back—initial and subsequent encounter]. Patients were excluded with primary diagnoses of radiculopathy in the lumbar region, lumbosacral neuritis, lumbar/lumbosacral disc degeneration, lumbar disc displacement, other intervertebral disc displacement lumbar, other intervertebral disc degeneration lumbar, and sciatica. Patients with incomplete survey forms were excluded from individual measures analysis. All participants were offered formal instructions on how to properly apply and operate an H-Wave® device.
Data Collection
All survey participants were asked an extensive predefined set of questions (Fig. 1) regarding their HWDS experiences, including effects on pain, function/ADL, medication usage, sleep, prior treatments and preference for HWDS, work status and performance, expectations, satisfaction with service, and confidence with device use. Patient characteristics including gender, age when injured, and age when treated with HWDS, as well as pain chronicity length and HWDS usage duration were documented and entered into the database. The patient survey completed by each study participant was necessarily proprietary for HWDS, but contained components of validated measures, including the visual analogue scale (VAS, 1–10) for pain and Oswestry Disability Index (ODI) for function/ADL. Of the 34,192 patients who completed a final survey, some had returned several surveys (usually two), and in one instance up to seven. For consistency and to avoid duplication, only the single final survey completed was analyzed for the purposes of this study. The 34,192 patients were reduced to 33,478 after removal of some surveys with spurious data values. After applying clinical filters for pain chronicity and usage duration, 11,503 remained. Of these, 2711 patients met the diagnostic criteria for nonspecific cLBP.
Statistical Analysis
A statistical analysis of 4-year PROMs survey data was conducted, involving 34,192 pain management patients. If a patient completed more than one survey, only the most recent survey response was used. Any erroneous survey responses were omitted before conducting the analyses. Certain inclusion and exclusion criteria, primarily diagnosis- and timeframe-related, were strictly enforced to produce a more focused and clinically relevant subset of the initial data set. Reporting consisted of demographics, followed by primary and secondary outcomes, with further subgroup analyses, particularly related to length of device use. In addition to the contingency table analyses, multiple logistic and linear regression techniques were applied with all patient covariates collected to assess the efficacy of HWDS treatment. The stepwise model selection technique was employed to produce a parsimonious and highly statistically significant model (p < 0.0001).
Results
Cohort and Exclusion
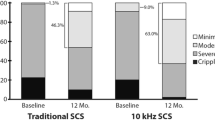
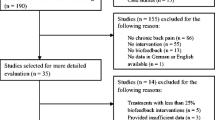
Of 34,192 total survey respondents, 2711 patients met the inclusion/exclusion criteria and were included in this cLBP study (Fig. 2).
The gender distribution was uniform with 52.55% male and 47.45% female. The average age ± standard deviation (SD) at injury and when treated with HWDS were 44.97 ± 12.60 years and 45.76 ± 12.65 years, respectively. The average reported pain chronicity was 287.60 ± 171.75 days and the average duration of HWDS usage was 94.89 ± 63.89 days. These data are summarized in Table 1.
Device Usage
On average, 2636 patients treated themselves almost twice daily (1.91 ± 0.91) over 5.5 days (5.50 ± 1.69) each week. Almost half (49.98%) applied the device for sessions lasting 30–45 min.
Insurance Mix
This cohort consisted almost entirely of workers’ compensation (n = 1722, 63.5%), personal injury (n = 778, 28.7%), and auto injury (n = 207, 7.6%) claimants.
Concomitant Home Exercise Program
Over two-thirds (1784 patients, 68.5%) reported active participation in a prescribed home exercise program, while the rest of the cohort did not.
Safety
No adverse or severe adverse events related to HWDS use were reported by any survey participants in this study.
Primary Outcome Measures
Pain Reduction
The pre-treatment visual analogue scale (VAS, 0–10) score reported for 2684 patients was 7.56 ± 1.80 (95% interval: 7.49, 7.63), while the post-treatment score for 2672 patients was 4.43 ± 2.14 (95% interval: 4.35, 4.51). The difference between pre- and post-treatment scores (2672 patients) was 3.12 ± 1.96 (95% interval: 3.05, 3.19), which was statistically significant (p = 0.0008) (Fig. 3, Table 2). Of note, 1527 patients (56.89%) reported their pre-treatment pain to be 8 or higher, while 759/1527 (49.71%) reported post-treatment reduction in pain level to 5 or below.
Using a minimum of 20% pain reduction as a liberal estimate—in particular compared to weaker TENS data—of clinically meaningful significance, among 2711 LBP patients, 2312 patients (85.28%) reported pain relief of at least 20% from baseline (before H-Wave treatment) (Fig. 4).
Function/ADL Improvement
Of 2586 patients [after exclusion of 125 surveys missing data], 2492 patients (96.36%) reported statistically significant improvement (p < 0.0001) in function/ADL post-treatment with HWDS (Fig. 5, Table 2).
Medication Usage Reduction
Of 2102 patients [after exclusion of 609 surveys missing data], 1354 patients (64.41%) reported statistically significant (p < 0.0001) reduction or elimination of use of pain medications. Specifically, 1123 (53.42%) decreased and 231 (11.00%) completely stopped medication use (Fig. 6, Table 2).
Sleep Improvement
Of 2711 patients, 1620 patients (59.76%) reported statistically significant (p < 0.0001) improvement in their quality of sleep (Fig. 7, Table 2).
Secondary Outcome Measures
Work Status and Performance
Of 2444 patients [after exclusion of 267 surveys missing data], 1369 (56.0%) were not working when starting HWDS, while 573 (23.5%) were doing modified work and 502 (20.5%) were fully working. Of the 1369 not working, 853 specifically indicated that they had not been working due to their injury, with 281 (32.9%) of those reporting that HWDS had subsequently helped them return to work.
Of the 1017 patients on full or modified duty [after exclusion of 58 surveys missing data], 830 (81.61%) reported statistically significant (p < 0.0001) improvement in their work performance post-treatment with HWDS (Fig. 8, Table 2).
Subgroup analysis indicated that improved work performance was more likely for those on full duty than on modified duty (odds ratio [OR] = 1.758; 95% confidence interval [1.171, 2.639]).
Prior Treatment and Preference for HWDS
Almost all of 2711 patients, 2680 (98.86%), reported the use of various other forms of treatment prior to starting HWDS (p < 0.0001). Of 2615 patients [after exclusion of 96 surveys missing data], 1658 (63.40%) reported that HWDS helped them more than prior treatments, being statistically significant (p < 0.0001); while 905 (34.60%) reported similar effectiveness and only 52 (2.00%) inferior benefits (Table 2).
Patient Expectations
Of 2582 patients [after exclusion of 129 surveys missing data], 2467 patients (95.55%) reported that HWDS use exceeded or met their expectations. Specifically, 863 (33.43%) reported exceeded and 1604 (62.12%) reported met expectations, with these levels of expectation being statistically significant (p < 0.0001) (Fig. 9, Table 2).
Patient Satisfaction with Service
Of 2625 patients [after exclusion of 86 surveys missing data], 2613 (99.54%) reported that the level of service provided by H-Wave® representatives was excellent or satisfactory (p < 0.0001). Specifically, 2208 (84.11%) reported excellent and 405 (15.43%) satisfactory service, which was statistically significant (p < 0.0001) (Fig. 10, Table 2).
Patient Confidence in Device Use
Of 2619 patients [after exclusion of 92 surveys missing data], 2601 (99.31%) reported their level of confidence in device usage to be excellent or satisfactory. Specifically, 1980 (75.60%) reported excellent and 621 (23.71%) satisfactory confidence, which was statistically significant (p < 0.0001) (Fig. 11, Table 2).
Outcomes Based on Treatment Length Periods
For further analysis, survey patients were stratified into three subgroups based on number of days they had used H-Wave, with a “trial period” ranging from 22 to 35 days (3–5 weeks), an “early treatment period” from 36 to 98 days (5–14 weeks), and a “late treatment period” from 99 to 365 days (14–52 weeks). The number of patients in the trial period, early treatment period, and late treatment period are 737 (27.18%), 647 (23.87%), and 1327 (48.95%), respectively.
Subgroup comparison analysis results were generally consistent without any major deviation, although using the device for longer periods resulted in better outcomes of pain relief, medication elimination, sleep improvement, and work performance (Table 3).
These observations were confirmed with statistical significance by further multiple regression analyses, where duration of device usage, participation in a home exercise program, and full or modified work are all important positive variables to consider when assessing the efficacy of HWDS. Negative variables to consider include longer pain chronicity and older patient age when injured. Specific statistically significant (p < 0.0001) inferences of interest include the following:
-
Longer device use results in greater pain relief.
-
Pain reduction is higher for those working than not working.
-
A higher pain level before treatment is associated with more substantial pain relief.
-
Longer pain chronicity results in less pain reduction.
-
Active home exercise program participation is associated with more functional improvement.
Outcomes Based on Analysis of All Diagnoses
While not the primary purpose of this study, the investigators were interested in how outcomes of HWDS for nonspecific chronic LBP might compare with the much larger cohort with “all diagnoses” treated, especially since prior H-Wave® studies have included many other conditions. For this analysis, diagnostic inclusion/exclusion criteria included all patient conditions, with duration of pain chronicity from the date of injury until the start of H-Wave® treatment remaining 90–730 days, and duration of device usage from 22 to 365 days. Of the same 34,192 patients, all-diagnoses cohort totaled 11,503 patients, which included the 2711 primary LBP study patients (23.6%). Survey results were surprisingly similar for the larger cohort, despite being heavily skewed away from nonspecific chronic LBP.
The following outcomes were nearly equivalent for all diagnoses compared to nonspecific cLBP: male gender 52.09% (0.46% less), age when injured 46.50 (1.53 years more), age when treated 47.33 (1.57 years more), duration of device usage 94.51 days (0.38 days less), pain improvement 3.00 (VAS, 1–10; 0.12 less), significant pain relief (≥ 20%) 85.60% (0.32% more), function/ADL improvement 96.07% (0.29% less), not working before treatment 57.61% (1.61% more), improved work performance 82.62% (1.01% more), expectations met 95.75% (0.20% more), service satisfaction 99.67% (0.13% more), confidence with device 99.54% (0.23% more), and device usage 1.90/day and 5.65 days/week (0.01/day less, 0.15 days/week more).
The following outcomes were slightly different: pain chronicity 305.13 (17.53 days more), medication reduction 67.28% (2.87% more), sleep improvement 57.53% (2.23% less), and helped more than prior treatments 66.38% (2.98% more).
Discussion
PROMs involve information directly acquired from the patient rather than the specialist’s records, where such data collectively represent the numerator of the value equation, defined as the outcomes directly benefiting patients relative to the costs of delivering those outcomes [15]. PROMs assign objective measures to patients’ subjective experiences of health, pain, disability, function, and QoL, something useful for providers in shared decision-making, outcome assessment, and relative indications for spinal care treatments [16]. Acceptance of health-related QoL and patient satisfaction PROMs data and advances in measurement are at an all-time high, resulting in ever-increasing publications of such. Insurers, healthcare providers, and patients often ask manufacturers, including device makers, to objectively share their outcomes data [17].
The large amount of patient-derived data for this retrospective PROMs cohort study were collected prospectively and purposively by the device maker, without subsequent tampering, primarily for internal quality control purposes. The extensive core primary database was exported, and statistical analyses were performed by an independent statistician regarding the statistical significance of identified primary and secondary outcomes.
There continues to be a generalized reluctance among the payer community to embrace coverage for most forms of ES, based partly on the fact that so many have only low-quality supportive evidence, as well as less stringent FDA requirements for marketing approval for class II medical devices [8]. However, several forms of ES, including HWDS, have moderate-quality evidence supporting their use for specifically defined indications [8]. The addition of these encouraging PROMs data, having more than adequate sample size, specifically for the treatment of nonspecific cLBP, represents an additional improvement in overall HWDS literature quality.
Difficult lessons have been learned in pain management, where there is general agreement that if the perception of pain can be mitigated to some degree and the patient can get moving again, then real life-changing progress has the opportunity to begin. Psychological benefits quickly accrue with progressive reduction of anxiety, depression, sleep loss, narcotic dependence, claim dependence, and unemployment [18]. HWDS PROMs result in pain reduction of over 3 (3.12) on a scale of 10, an important finding given that higher-quality TENS published data indicate less than 1 on a scale of 10 (0.884) for cLBP (generally considered of clinical significance), with relief being maintained only while the device is turned on [19]. As such, HWDS appears to have approximately 3.5 times more reported pain reduction than TENS. While it would be desirable for an ES device to have an even greater pain-relieving effect, these new HWDS data demonstrating that over 85% of such patients have more significant (≥ 20%) relief should be welcome.
As observed in previous HWDS publications [9,10,11], improvements in function and ADL in over 96% of this cLBP cohort is probably a more important finding than reported subjective pain outcomes. Work performance improvement in over 81% of those working is consistent with such function and ADL gains. Over 64% either decreased or stopped the use of pain medications, something of particular interest given the ongoing opioid crisis. Sleep improvement was reported in 60%, likely reflective of psychological health effects. Overall HWDS patient satisfaction is quite high, in the upper 90th percentile, as reported for meeting expectations, service satisfaction, and device confidence.
These PROMs outcomes, both primary and secondary, compare favorably to previous peer-reviewed HWDS publications [8,9,10,11]. A systematic review of clinical studies noted some of these older reported outcomes: (1) several studies on HWDS for treatment of diabetic peripheral neuropathy resulted in at least partial pain relief in over 77% of patients; (2) a large observational study of 6591 nonspecific neuropathic pain patients reported > 25% pain relief in 78% of the cohort; (3) patient-reported function improved in 79% of 6530 soft-tissue injury and neuropathic pain patients; and (4) pain medication reduction or elimination occurred in 65% of 5329 neuropathic pain patients [9]. A more recent 2-year HWDS observational study of 157 end-stage workers’ compensation chronic pain (avg. 7.8 years) claimants reported a mean pain scale reduction of 35%, 89% with functional improvement, and 49% reducing or stopping (42%) pain medications. Of patients reporting pain relief, 82% noted “moderate” improvement, while 24% and 31% improvement was measured in depression and anxiety scores, respectively [11]. Another recent survey study of first responders given access to HWDS at their workplace reported improved ROM in 93%, pain reduction in 82%, and better job performance in 50%, with further additional sleep and mental health benefits [10].
HWDS appears to be similarly effective across diverse patient populations, something from earlier reports that is now better confirmed [9]. Positive outcomes occur not only with healthier and more active first responders, but also for hard-to-treat extremely chronic pain management claimants [10, 11]. These PROMs outcomes show minimal variance between cLBP patients and “all diagnoses” device users, which included significant numbers of chronic pain patients with diagnoses related to other lumbar conditions, as well as other body regions, suggesting additional PROMs studies in the future. A prospective randomized controlled trial, using similar inclusion and exclusion criteria for cLBP, should also be considered, given these robust findings.
Study weaknesses include not being fully prospective, lack of a control group, narrow patient selection (claimants), and moderate risk of selection bias. Other study weaknesses include the practical necessity of using an unvalidated proprietary survey instrument and not being able to longitudinally assess multiple individual survey outcomes over time, an issue partially addressed with subgroup analysis of several survey completion time periods.
Conclusions
Treatment outcomes recorded directly from patients, without coercion, carry considerable clinical weight and are not to be ignored in understanding the impact of any treatment effectiveness currently offered in healthcare. HWDS PROMs for nonspecific cLBP offer hope and encouragement, especially given current trends towards online reviews and ratings of virtually everything. Statistical analyses of these raw patient-reported data, systematically collected by the device maker over a particularly tumultuous 4-year period (e.g., COVID-19), have proven positive outcomes consistent with previous peer-reviewed HWDS published studies. Both primary and secondary outcomes were remarkably similar for “all diagnoses” when compared to those for cLBP, suggesting treatment effectiveness for other body regions.
Significant pain relief, defined as 20% or more, was reported in over 85% of nonspecific cLBP patients, with a greater than three-point reduction in pain on a scale of 0–10. Function and ADLs increased in over 96%, while work performance improved in over 81% of working survey participants. Pain medication use decreased or stopped in two out of three, while sleep improved in almost 60% of HWDS patients (Fig. 12). Almost all of those surveyed reported confidence in device use (99.31%) and service satisfaction (99.54%), as well as having expectations met or exceeded (95.55%).
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
McPhail SM, Schippers M, Marshall AL. Age, physical inactivity, obesity, health conditions, and health-related quality of life among patients receiving conservative management for musculoskeletal disorders. Clin Interv Aging. 2014;9:1069. https://doi.org/10.2147/CIA.S61732.
Thinkhamrop W, Sawaengdee K, Tangcharoensathien V, Theerawit T, Laohasiriwong W, Saengsuwan J, Hurst CP. Burden of musculoskeletal disorders among registered nurses: evidence from the Thai nurse cohort study. BMC Nurs. 2017;16(1):1–9. https://doi.org/10.1186/s12912-017-0263-x.
Van Eerd D, Munhall C, Irvin E, Rempel D, Brewer S, Van Der Beek A, Dennerlein J, Tullar J, Skivington K, Pinion C. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: an update of the evidence. Occup Environ Med. 2016;73(1):62–70. https://doi.org/10.1136/oemed-2015-102992.
Wong JJ, Côté P, Tricco AC, Rosella LC. Examining the effects of low back pain and mental health symptoms on healthcare utilisation and costs: a protocol for a population-based cohort study. BMJ Open. 2019;9: e031749. https://doi.org/10.1136/bmjopen-2019-031749.
Gupta G, Tarique A. Prevalence of musculoskeletal disorders in farmers of Kanpur-rural. India J Commun Med Health Educ. 2013;3(7):249–53. https://doi.org/10.4172/2161-0711.1000249.
Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332:1430–4. https://doi.org/10.1136/bmj.332.7555.1430.
Jalalvandi F, Ghasemi R, Mirzaei M, Shamsi MB. Effects of back exercises versus transcutaneous electric nerve stimulation on relief of pain and disability in operating room nurses with chronic non-specific LBP: a randomized clinical trial. BMC Musculoskelet Disord. 2022;23(1):291. https://doi.org/10.1186/s12891-022-05227-7.
Allen CB, Williamson TK, Norwood SM, et al. Do electrical stimulation devices reduce pain and improve function?—A comparative review. Pain Ther. 2023. https://doi.org/10.1007/s40122-023-00554-6.
Williamson TK, Rodriguez HC, Gonzaba A, Poddar N, Norwood SM, Gupta A. H-Wave® device stimulation: a critical review. J Pers Med. 2021;11(11):1134. https://doi.org/10.3390/jpm11111134.
Williamson TK, Rodriguez HC, Han D, Norwood SM, Gupta A. Job-related performance and quality of life benefits in first responders given access to H-Wave® device stimulation: a retrospective cohort study. J Pers Med. 2022;12(10):1674. https://doi.org/10.3390/jpm12101674.
Trinh A, Williamson TK, Han D, Hazlewood JE, Norwood SM, Gupta A. Clinical and quality of life benefits for end-stage workers’ compensation chronic pain claimants following H-Wave® device stimulation: a retrospective observational study with mean 2-year follow-up. J Clin Med. 2023;12(3):1148. https://doi.org/10.3390/jcm12031148.
Lowry KJ, Brox WT, Naas PL, Tubb CC, Muschler GF, Dunn W. Musculoskeletal-based patient-reported outcome performance measures, where have we been-where are we going. J Am Acad Orthop Surg. 2019;27(13):e589–95. https://doi.org/10.5435/JAAOS-D-18-00429.
Kluzek S, Dean B, Wartolowska KA. Patient-reported outcome measures (PROMs) as proof of treatment efficacy. BMJ Evid Based Med. 2022;27(3):153–5. https://doi.org/10.1136/bmjebm-2020-111573.
Gladwell PW, Cramp F, Palmer S. Matching the perceived benefits of Transcutaneous Electrical Nerve Stimulation (TENS) for chronic musculoskeletal pain against Patient Reported Outcome Measures using the International Classification of Functioning, Disability and Health (ICF). Physiotherapy. 2020;106:128–35. https://doi.org/10.1016/j.physio.2019.01.017.
Jayakumar P, Bozic K. Journal of the American Academy of Orthopaedic Surgeons patient-reported outcome measurements (PROMs) special issue: the value of PROMs in orthopaedic surgery. J Am Acad Orthop Surg. 2023;31(20):1048–56. https://doi.org/10.5435/JAAOS-D-23-00500.
Lee Y, Issa TZ, Vaccaro AR. State-of-the-art applications of patient-reported outcome measures in spinal care. J Am Acad Orthop Surg. 2023;31(20):e890–7. https://doi.org/10.5435/JAAOS-D-22-01009.
Ware Jr. JE. Foreword to Journal of the American Academy of Orthopaedic Surgeons PROMs special issue: why use PROMs in orthopaedic surgery? J Am Acad Orthop Surg. 2023;31(20):1047. https://doi.org/10.5435/JAAOS-D-23-00570.
Borisovskaya A, Chmelik E, Karnik A. Exercise and chronic pain. Adv Exp Med Biol. 2020;1228:233–53. https://doi.org/10.1007/978-981-15-1792-1_16.
Jauregui JJ, Cherian JJ, Gwam CU, Chughtai M, Mistry JB, Elmallah RK, Harwin SF, Bhave A, Mont MA. A meta-analysis of transcutaneous electrical nerve stimulation for chronic low back pain. Surg Technol Int. 2016;28:296–302.
Acknowledgements
We thank the participants of the study.
Authorship.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
No funding or sponsorship was received for this study or publication of this article. The journal’s rapid service fee was funded by Electronic Waveform Lab, Inc. (Huntington Beach, CA, USA).
Author information
Authors and Affiliations
Contributions
Stephen M. Norwood and Ashim Gupta conceptualized the study. Statistical analysis was performed by David Han. The first draft of the manuscript was written by Stephen M. Norwood and Ashim Gupta. Stephen M. Norwood, David Han and Ashim Gupta commented on the previous versions of the manuscript. Ashim Gupta supervised and administered the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Stephen M. Norwood and Ashim Gupta are consultants for Electronic Waveform Lab, Inc. David Han has nothing to disclose.
Ethical Approval
This study was approved by the South Texas Orthopaedic Research Institute Institutional Review Board (number: STORI09192023-1, dated September 19, 2023). Electronic Waveform Lab, Inc. gave permission for these data to be accessed. The data were de-identified. The participants provided their informed consent for the collected data to be analyzed for publication in a scholarly journal.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Norwood, S.M., Han, D. & Gupta, A. H-Wave® Device Stimulation for Chronic Low Back Pain: A Patient-Reported Outcome Measures (PROMs) Study. Pain Ther 13, 113–126 (2024). https://doi.org/10.1007/s40122-023-00570-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00570-6