Abstract
Zoster-associated pain (ZAP) is a painful condition that significantly impacts a patient’s quality of life, often leading to postherpetic neuralgia (PHN). Over 30% of patients with herpes probably experience PHN. However, the understanding and treatment of ZAP remain inadequate. Common interventional treatments include radiofrequency therapy, nerve blocks, epidural block, and spinal cord electrical stimulation. Among these, radiofrequency therapy is widely used for pain control in ZAP, but the standard pulsed radiofrequency technique can still be improved. Researchers have explored different radiofrequency parameters, modes, targets, and combined treatments to enhance the therapeutic effect. In this paper, we review the latest research findings and incorporate our own departmental investigations. We conclude that high-voltage, long-duration pulsed radiofrequency and radiofrequency thermocoagulation therapy have shown improved therapeutic outcomes, despite some remaining limitations. Emphasis is placed on safety in intercostal nerve and extracranial nerve radiofrequency treatments. Combination therapy is also safe and effective; however, many studies have a low grade of evidence. Further high-quality research and systematic reviews are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Zoster-associated pain (ZAP) is a neuropathic pain syndrome characterized by complex mechanisms that cause severe discomfort and a high incidence of complications, leading to significant physical and psychological distress for patients. |
Current treatment approaches for ZAP involve early administration of antiviral medications, analgesics, and various minimally invasive interventions. |
While radiofrequency therapy has gained popularity as a treatment for ZAP, there remains a lack of standardization regarding its parameters and therapeutic objectives, which necessitates further investigation. This paper aims to review the recent advancements in this field. |
What was learned from the study? |
The application of high-voltage, long-duration pulsed radiofrequency and radiofrequency thermocoagulation therapy has shown improved therapeutic outcomes, but attention should be given to potential intraoperative and postoperative complications. |
Both intercostal nerves at the angulus costae and extracranial targets have demonstrated effectiveness as targets for radiofrequency therapy while maintaining a high level of safety. |
Combined treatments utilizing multiple mechanisms are currently gaining recognition and popularity. |
Introduction
Zoster-associated pain (ZAP) is caused by the reactivation of the varicella-zoster virus (VZV) that had been dormant in the ganglion [1]. It results in severe stabbing, stinging, and burning pain in the skin of the affected area during herpes outbreaks and after the herpes has healed. ZAP is the primary clinical manifestation of herpes zoster (HZ) and is the main reason patients seek medical attention. The incidence rate of HZ ranges from 3 to 5 cases per 1000 person-years. The risk of developing postherpetic neuralgia (PHN) varied from 5% to over 30%. Additionally, over 30% of patients with PHN experienced persistent pain for more than 1 year [2]. It significantly reduces patients’ quality of life and causes physical and mental suffering.
Studies have shown that VZV can be reactivated by various factors, including aging, stress, low immunity, and the use of immunosuppressive drugs [3]. The risk of virus reactivation increases when the body’s immunity decreases to the “herpes zoster threshold” (a lower level of VZV-specific T cell) [4]. When that happens, some patients will experience a period of neuropathic pain, which can be categorized into the acute phase, subacute phase, and PHN phase [5, 6]. The mechanism responsible for the transition from the acute phase of ZAP to the PHN phase is still unclear and requires further study [7].
Not all patients progress to PHN, but when it does occur, it is often challenging to treat and typically requires a multimodal pharmacological and interventional treatment approach to alleviate this debilitating pain and provide symptomatic relief to patients [8]. Early identification and treatment of ZAP remain a primary focus [2, 9]. Pharmacological treatments are widely used, and minimally invasive interventions are thriving. Minimally invasive therapies such as nerve block, radiofrequency, spinal cord electrical stimulation, and ozone injection have been proven effective in treating ZAP [10]. Radiofrequency therapy has recently gained popularity for its efficacy, rapid onset of action, minimal invasiveness, and relative affordability. The availability of CT, X-ray, ultrasound, and sensorimotor testing has greatly improved the accuracy and safety of puncturing the dorsal root ganglion (DRG) and the semilunar node of the trigeminal nerve, which are the most commonly targeted areas for radiofrequency therapy.
Pulsed radiofrequency is widely used for treating ZAP owing to its nondestructive nature. However, researchers have observed that standard pulsed radiofrequency treatment only provides short-term pain relief, making it prone to recurrence. To enhance the therapeutic effect and prolong the duration of analgesia, researchers have been continuously exploring potential solutions.
Selection of Evidence
Papers for this narrative review were collected through a keyword search in several databases including PubMed, Google Scholar, and Web of Science Core Collection using terms “herpes zoster,” “neuralgia,” “radiofrequency therapy,” and “intercostal nerve” without considering publication date limitations; no gray literature was included. The search was last updated in May 2023. The authors determined inclusion on the basis of the papers’ relevance to the topic; 26 papers were finally included. This article is a collection of previous studies and does not involve any new studies with human or animal participants conducted by the authors.
Overview of Radiofrequency Therapy
The principle of radiofrequency therapy involves the emission of an electric current by a device, creating a constantly changing electric field between the working electrode’s tip and the surrounding tissue. This generates a magnetic field and heat through friction and impact, known as the field effect and thermal effect [11]. The mechanism of radiofrequency therapy, whether attributed to the field effect or thermal effect, remains controversial.
Radiofrequency modes can be broadly categorized into pulsed radiofrequency and radiofrequency thermocoagulation. In the standard pulsed radiofrequency mode, the electrode rests for 480 ms for every 20 ms of work, maintaining the tissue temperature around the working electrode at a low 42 °C. This produces field and biological effects without causing thermal damage to the tissue cells. On the other hand, radiofrequency thermocoagulation mode involves continuous work by the electrode, raising the tissue temperature around the working tip to 65 °C or higher.
However, the use of radiofrequency thermocoagulation on spinal nerves with overt motor function involvement, such as those innervating the upper and lower extremities, is avoided because of the risk of motor function damage [12].
Progress in Radiofrequency Therapy in ZAP
This section examines the efficacy and safety of radiofrequency therapy in ZAP, analyzing recent research progress in radiofrequency parameters (Supplementary Table 1), modes (Supplementary Table 2), targets (Supplementary Table 3), and combined treatments. ZAP predominantly affects spinal nerves, with approximately 48.1% of cases occurring in the thoracodorsal nerve region [13]. Treatment often involves targeting the DRG of the spinal nerve, which plays a crucial role in transmitting and processing sensory signals related to neuropathic pain. The distinct tissue and anatomical structure of the DRG make it accessible and susceptible to external physical and chemical influences [10, 14, 15].
Radiofrequency Parameters
Currently, there is no standardized approach to pulsed radiofrequency parameters. Researchers have studied the impact of various radiofrequency voltages and time durations on the efficacy of pulsed radiofrequency treatment. For example, a randomized controlled study compared three groups of patients with PHN who received thoracic DRG pulsed radiofrequency at different voltages (45, 55, and 65 V). The study found that pulsed radiofrequency at 65 V provided better pain relief, improved quality of life, and increased patient satisfaction 12 months post surgery [16]. A similar analysis of various pulsed radiofrequency parameters in acute-phase ZAP showed that the high-voltage group (76.50 ± 5.61 V) had lower pain scores, improved sleep quality, and required less medication compared to the standard-voltage group (47.73 ± 2.45 V) [17].
Disease duration is a known risk factor for treatment outcome. One study retrospectively observed 64 patients with subacute stage ZAP and PHN who underwent high-voltage, long-duration pulsed radiofrequency treatment. The results showed that pain was significantly reduced in all patients after treatment, but those in the subacute group had better pain relief than those in the PHN group at 1, 3, and 6 months postoperatively. The success rate of pulsed radiofrequency in the subacute group was significantly higher than in the PHN group (81.3% vs. 56.3%, P = 0.031) [18]. Another retrospective study with a sample size of 81 individuals indicated that application of high-voltage, long-duration pulsed radiofrequency therapy effectively treated acute ZAP and produces better outcomes when applied repeatedly [19].
Additionally, Han et al. found that patients in the 65 V group had significantly more areas of skin numbness on postoperative day 3 compared to the other two groups (both P < 0.05), but this difference was no longer statistically significant on postoperative day 30 [16]. Increasing the voltage to a certain level may cause pain and immediate discomfort, including tachycardia and hypertension [20]. Furthermore, patients with cardiac insufficiency and hypertension are at a higher potential therapeutic risk. Studies often exclude participants with severe cardiorespiratory insufficiency, which may explain the low incidence of reported treatment-related complications. In the clinical setting, when dealing with patients in poor physical condition, treatment regimens should be cautiously selected and risk factors carefully evaluated.
In summary, increasing voltage and duration have been found to effectively manage pain in patients with ZAP, especially when the duration of the disease is shorter [18, 19]. However, higher voltages may increase discomfort and sensory numbness. Adjusting the radiofrequency voltage based on patient feedback during treatment may help balance efficacy and treatment-related discomfort.
Radiofrequency Mode
Radiofrequency thermocoagulation has been proposed as a viable treatment option for patients with PHN [21]. Although spinal nerve radiofrequency thermocoagulation has been controversial because of its potential nerve damage, it may offer a more effective long-term pain management solution for patients with refractory PHN who have not responded well to other interventions [22, 23].
In a retrospective comparison study by Luo et al., radiofrequency thermocoagulation (95 °C, 45 V, 240 s) was compared to standard pulsed radiofrequency for treating ZAP [24]. The results showed that radiofrequency thermocoagulation had a significantly lower short-term recurrence rate (14.93%) within 3 months compared to standard pulsed radiofrequency (37.31%). This indicates that radiofrequency thermocoagulation has the potential to provide superior pain relief. Another study by Zhang et al. followed patients who received radiofrequency thermocoagulation therapy for PHN for up to 10 years [25]. The study concluded that this therapy was safe and effective, with a 1-year recurrence rate of 22.2% and an overall recurrence rate of 47.9% at 10 years. The main complications reported were intraoperative pain sensation (71.9%) and postoperative numbness (89%). Additionally, abdominal distension was observed in 18.4% of cases. However, these postoperative complications decreased over time. The duration of the disease, type of radiofrequency electrode, pain level, and complication status were found to be associated with the recurrence rate.
In a retrospective study by Zhu et al., the effectiveness of bipolar radiofrequency thermocoagulation (95 °C, 45 V, 300 s) of the posterior spinal nerve root in treating PHN was observed [26]. The study found that after 2 years of treatment, 94.7% of patients in the bipolar radiofrequency group achieved pain relief of up to 75%, compared to 53.3% of patients in the monopolar radiofrequency group. The study suggests that bipolar radiofrequency thermocoagulation with 5-mm spacing should be used to achieve a higher success rate and longer-lasting effectiveness. It should be noted that two complications, numbness of skin segments and abdominal distension, were more common in the first 3 months post treatment and decreased to approximately 30% at 2 years in the unipolar radiofrequency thermocoagulation group. However, 68.4% of patients in the bipolar radiofrequency thermocoagulation group still experienced sensory numbness after 2 years, likely due to the higher degree of spinal nerve destruction caused by bipolar radiofrequency thermocoagulation.
In conclusion, spinal nerve radiofrequency thermocoagulation is an effective alternative intervention for patients with prolonged PHN who are willing to accept the potential complications associated with the treatment. Lower temperature radiofrequency thermocoagulation of the semilunar nodes has been shown to provide satisfactory pain relief with fewer and milder postprocedural complications compared to higher temperature radiofrequency thermocoagulation [27]. However, further research is needed to evaluate the relationship between temperature, efficacy, and complications in spinal nerve radiofrequency thermocoagulation for PHN.
Radiofrequency Targets
Intercostal Nerve Radiofrequency
For patients with thoracic ZAP, researchers have studied the effectiveness and safety of using radiofrequency therapy on the intercostal nerves at the angulus costae guided by ultrasound, CT, and X-ray as an additional treatment option alongside DRG. This treatment modulates the entire intercostal nerve axis, covering the affected dermatomes in the paravertebral and anterior thoracic regions. The nerves at the angulus costae extend to the lower edge of the rib cage, while the vascular system is found in the intercostal groove. During radiofrequency treatment, the vasculature in the angulus costae is not compromised unless there are anatomical variations. Compared to the DRG, the nerve at the angulus costae is more superficial, making the puncture path shorter and enabling identification through ultrasound guidance, resulting in a safer and simpler procedure.
In randomized controlled trials with follow-up periods ranging from 6 to 12 months, Ma et al. [28] and Makharita et al. [29] investigated the effectiveness and safety of using the intercostal nerve at the angulus costae as a puncture site for treating thoracic PHN. Their studies demonstrated that pulsed radiofrequency treatment of the intercostal nerves at the angulus costae significantly relieved pain and improved the quality of life in patients with PHN compared to the sham-operated group. There were no apparent signs of pneumothorax, bleeding, infection, or other serious side effects.
A retrospective study by Huang et al. compared the effectiveness of thoracic DRG with intercostal nerve pulsed radiofrequency for PHN in elderly patients [30]. The results showed significantly lower pain scores and improved quality of life in both groups during a 12-week follow-up period. However, patients receiving thoracic DRG pulsed radiofrequency treatment had lower pain scores compared to those receiving intercostal nerve pulsed radiofrequency treatment from 2 weeks post treatment until week 12. The SF-36 scores, which assess emotional, psychological, and social aspects, were also higher in the DRG pulsed radiofrequency group compared to the intercostal nerve pulsed radiofrequency group.
In summary, existing studies show that the intercostal nerve at the thoracic level is an effective target for radiofrequency therapy in patients with thoracic PHN. It offers a high puncture success rate and safety when performed under ultrasound guidance. However, in terms of efficacy for pain relief, the short-term and long-term efficacy of pulsed radiofrequency in the intercostal nerve at the angulus costae is not as good as that in the DRG. The choice between the two therapeutic targets should consider the patient’s general condition, pain location, treatment conditions, and the practitioner’s familiarity with the procedure.
Extracranial Nerve Radiofrequency
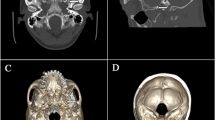
Around 13.6% of patients with HZ experience cranial nerve involvement [13]. The Gasserian ganglion, located in Meckel’s cavity at the base of the middle cranial fossa, gives rise to the ophthalmic, maxillary, and mandibular branches that exit the skull through the supraorbital fissure, foramen rotundum, and foramen ovale, respectively. However, treating the Gasserian ganglion with radiofrequency carries the risk of complications such as ptosis, corneal ulceration, ocular damage, vision loss, intracranial hemorrhage, and infection [31, 32]. To investigate the effectiveness of ZAP treatment with lower risk, researchers have explored safer extracranial nerve radiofrequency targets guided by CT, and ultrasound.
Previous studies suggest that extracranial pulsed radiofrequency treatment of the supraorbital, infraorbital, and chin nerves is slightly less effective than Gasserian ganglion treatment for trigeminal postherpetic neuralgia (TPHN), with overall efficacy rates of 68.9% and 86.7%, respectively, at 1 year [33]. In a study by Li et al., high-voltage, long-duration (65 V, 900 s, T < 50 °C) supraorbital nerve pulsed radiofrequency was evaluated for ophthalmic herpetic neuralgia (OHN) with a 6-month follow-up [34]. The effective rate of high-voltage pulsed radiofrequency for the supraorbital nerve was 84.62%, compared to 53.84% for standard pulsed radiofrequency (45 V, 900 s, 42 °C). No serious complications were reported. Some researchers have also applied radiofrequency thermocoagulation to the supraorbital nerve in patients with OHN, resulting in a significant decrease in pain levels within 1 year [31]. However, some patients experienced temporary numbness in the supraorbital innervation area, which resolved over time. These findings are consistent with the efficacy of high-voltage, long-duration pulsed radiofrequency and radiofrequency thermocoagulation in spinal nerves, suggesting that extracranial high-voltage, long-duration pulsed radiofrequency and radiofrequency thermocoagulation may be safe and effective treatments for TPHN. However, the occurrence and impact of post-treatment numbness should be further explored.
Additionally, initial research has been conducted on the use of the stellate ganglion (SG) as a target for radiofrequency therapy in the treatment of PHN affecting the face and upper extremities. A study by Ding et al. evaluated the effectiveness of pulsed radiofrequency on the SG in patients with facial or upper extremity PHN, showing better pain relief, improved quality of life, and a lower incidence of complications and side effects (Horner’s syndrome) compared to SG block [35].
For patients with persistent cephalofacial PHN involving the great auricular nerve, pulsed radiofrequency treatment has been reported to provide over 50% pain relief with no severe complications [36, 37].
Combined Treatment
Combining treatments with diverse targeting mechanisms is believed to result in a more effective therapeutic response for ZAP. For example, combinations such as DRG pulsed radiofrequency with steroids, ozone, local anesthetics or recombinant human interferon-α2b, as well as pulsed radiofrequency combined with continuous radiofrequency or heat acupuncture are applied for ZAP [38,39,40,41,42,43,44,45,46]. Numerous clinical studies have focused on the combination of pulsed radiofrequency and ozone, consistently demonstrating the safety and effectiveness of this treatment modality [40,41,42,43]. It provides both short-term and long-term analgesia without significant complications. Moreover, it is effective for all stages of ZAP, with better efficacy observed when applied early. However, combination therapy takes various forms, and the safety, efficacy, economy, and convenience of these combined treatment programs still require testing in clinical practice.
Discussion
ZAP is a challenging condition because of its painful nature and the high incidence of PHN, which significantly impacts quality of life. Radiofrequency therapy has emerged as an effective method for pain control in ZAP, but further exploration is needed.
The primary objective of this review is to enhance readers’ understanding of the advancements in radiofrequency treatment for ZAP and facilitate their effective and safe utilization of radiofrequency technology in ZAP treatment.
Our analysis suggests that increasing voltage and duration can enhance pain alleviation and prolong the efficacy of pulsed radiofrequency treatment. Additionally, the use of radiofrequency therapy in combination with multiple targeting mechanisms is gaining momentum, supported by previous studies demonstrating effectiveness. Since pulsed radiofrequency treatments are nondestructive, they can be applied regardless of the affected position or severity of the disease.
Several risk factors have been reported to affect the prognosis of ZAP, including older age, immunosuppression, greater acute pain intensity, affected position, greater extent of rash, and longer duration of prodromal pain [47,48,49]. They can be used to assess patients and identify those at high risk of poor prognosis.
Most patients in the acute/subacute phase typically experience satisfactory outcomes with standard pulsed radiofrequency therapy. However, for patients who are identified as having a higher risk of poor prognosis and show inadequate response to standard treatment, alternative options such as high-voltage, long-duration pulsed radiofrequency or combined therapy may be considered more favorable. The aim is to alleviate ZAP, expedite recovery, reduce the incidence of PHN, and ultimately enhance the patients’ quality of life.
When refractory PHN develops and is unresponsive to nondestructive interventions, radiofrequency thermocoagulation provides better pain control. However, the occurrence of post-treatment numbness continues to be a challenge, and measures to decrease its frequency and intensity are necessary. The safety concerns stemming from pain and discomfort during surgery can be mitigated through real-time monitoring and symptomatic management. Nevertheless, additional research is required to establish a more suitable intraoperative analgesic regimen. On the basis of current research evidence, we believe that the advantages of employing higher temperature radiofrequency thermocoagulation in elderly patients with refractory PHN outweigh the disadvantages. This approach effectively alleviates pain symptoms and disrupts the vicious circle of pain and debilitation. On the other hand, lower temperature radiofrequency thermocoagulation may offer the benefit of reduced postprocedural complications and may be prioritized for patients with PHN who prioritize quality of life. Additionally, it should be noted that radiofrequency thermocoagulation is not suitable for patients with PHN whose nerves have obvious motor function involvement.
Compared to the DRG and the trigeminal semilunar node, targeting the intercostal nerve at the angulus costae and utilizing extracranial nerve radiofrequency therapy offer advantages in terms of safety and efficacy. This approach may be particularly beneficial for patients with ZAP who are at a higher risk of difficult puncture paths, compromised systemic conditions, or lack visual guidance through CT or X-ray.
Nevertheless, further high-quality research and clinical practice are necessary to confirm these findings. It is essential to explore more efficient treatment protocols, examine the influence of various radiofrequency parameters on therapeutic outcomes and complications, and devise strategies to mitigate radiofrequency treatment-related complications.
Conclusion
ZAP is a challenging neuropathic pain condition. The application of radiofrequency therapy in ZAP has expanded treatment options thanks to ongoing research on radiofrequency parameters, modes, targets, and combination therapies, resulting in improved efficacy. Our focus is on enhancing treatment effectiveness, ensuring safety, and reducing complications. Selecting appropriate radiofrequency modes, parameters, and targets based on patient condition is crucial. Knowledge of potential complications and their management is important. The studies cited here are primarily single-center studies with limited sample sizes, highlighting the need for more high-quality research and systematic reviews in the future.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Bricout H, Haugh M, Olatunde O, et al. Herpes zoster-associated mortality in Europe: a systematic review. BMC Public Health. 2015;15(1):1–14.
Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4(6):e004833.
Meng Y, Zhuang L, Jiang W, et al. Segmental zoster paresis: a literature review. Pain Physician. 2021;24(3):253–61.
Johnson RW. Herpes zoster and postherpetic neuralgia. Expert Rev Vaccines. 2010;9(3 Suppl):21–6.
Johnson RW, Alvarez-Pasquin MJ, Bijl M, et al. Herpes zoster epidemiology, management, and disease and economic burden in Europe: a multidisciplinary perspective. Ther Adv Vaccines. 2015;3(4):109–20.
Johnson RW. Zoster-associated pain: what is known, who is at risk and how can it be managed? Herpes. 2007;14(Suppl 2):30–4.
Warner BE, Goins WF, Kramer PR, et al. A guide to preclinical models of zoster-associated pain and postherpetic neuralgia. Curr Top Microbiol Immunol. 2023:438:189–221.
Lang PO, Ferahta N. Recommendations for treatment and prevention of herpes zoster and associated pain in aged adults. Rev Med Interne. 2016;37(1):35–42.
Esposito S, Principi N. Herpes zoster prevention: a difficult problem to solve. Vaccine. 2018;36(36):5442–8.
Sapunar D, Kostic S, Banozic A, et al. Dorsal root ganglion—a potential new therapeutic target for neuropathic pain. J Pain Res. 2012;5:31–8.
Chang IA, Nguyen UD. Thermal modeling of lesion growth with radiofrequency ablation devices. Biomed Eng Online. 2004;3(1):27.
Huang B, Lin HD. Is radiofrequency ablation of spinal nerve root available for the patients with intractable postherpetic neuralgia? Zhonghua Yi Xue Za Zhi. 2021;17(2):133–5.
Shiraki K, Toyama N, Shiraki A, et al. Age-dependent trigeminal and female-specific lumbosacral increase in herpes zoster distribution in the elderly. J Dermatol Sci. 2018;90(2):166–71.
Hasegawa T, An HS, Haughton VM. Imaging anatomy of the lateral lumbar spinal canal. Semin Ultrasound CT MR. 1993;14(6):404–13.
Pope JE, Deer TR, Kramer J. A systematic review: current and future directions of dorsal root ganglion therapeutics to treat chronic pain. Pain Med. 2013;14(10):1477–96.
Han ZK, Hong T, Ding YY, et al. CT-guided pulsed radiofrequency at different voltages in the treatment of postherpetic neuralgia. Front Neurosci. 2020;14:9.
Wang B, Du Z, Xia J, et al. Efficacy of high-voltage pulsed radiofrequency for the treatment of elderly patients with acute herpes zoster neuralgia. Rev Assoc Med Bras (1992). 2021;67(4):585–9.
Sun CL, Li XL, Li CW, et al. High-voltage, long-duration pulsed radiofrequency to the dorsal root ganglion provides improved pain relief for herpes zoster neuralgia in the subacute stage. Pain Physician. 2023;26(3):E155-e162.
Zhang E, Fei Y, Xu L, et al. Effect of repeated high-voltage long-duration pulsed radiofrequency on herpetic neuralgia. Pain Physician. 2022;25(7):E1047-E1055.
Wan C-F, Liu Y, Dong D-S, et al. Bipolar high-voltage, long-duration pulsed radiofrequency improves pain relief in postherpetic neuralgia. Pain Physician. 2016;19(5):E721–8.
Zhang WN, Shi LY, Zhao Y, et al. Influences of pulse radiofrequency with different temperatures on the pain, depression and anxiety in the patients with postherpetic neuralgia. Chin J Painol. 2021. https://doi.org/10.3760/cma.j.cn101658-20200827-00150.
Luo C, Yang B, Yang LQ, et al. Computed tomography-guided percutaneous coblation of the thoracic nerve root for treatment of postherpetic neuralgia. Pain Physician. 2020;23(5):E487–95.
Lin HD, Cao G, Yang ZD, et al. Computed tomography-guided radiofrequency ablation of the cervical dorsal root ganglia in 27 patients with cervical and occipital postherpetic neuralgia. Med Sci Monitor. 2021;27:e932612.
Luo G, Zhang Z, Zhu J, et al. Association between the risk of relapse and the type of surgical procedure for herpes zoster-related pain. Pain Physician. 2021;24(8):E1227-1236.
Zhang Z, Xia Z, Luo G, et al. Analysis of efficacy and factors associated with reccurence after radiofrequency thermocoagulation in patients with postherpetic neuralgia: a long-term retrospective and clinical follow-up study. Pain Ther. 2022;11(3):971–85.
Zhu JJ, Luo G, He QL, et al. Evaluation of the efficacy of unipolar and bipolar spinal dorsal root ganglion radiofrequency thermocoagulation in the treatment of postherpetic neuralgia. Korean J Pain. 2022;35(1):114–23.
Yao P, Deng YY, Hong T, et al. Radiofrequency thermocoagulation for V2/V3 idiopathic trigeminal neuralgia: effect of treatment temperatures on long-term clinical outcomes: a cohort study. Medicine (Baltimore). 2016;95(26):e4019.
Ma K, Fan YH, Jin Y, et al. Efficacy of pulsed radiofrequency in the treatment of thoracic postherpetic neuralgia from the angulus costae: a randomized, double-blinded, controlled trial. Pain Physician. 2013;16(1):15–25.
Makharita MY, El Bendary HM, Sonbul ZM, et al. Ultrasound-guided pulsed radiofrequency in the management of thoracic postherpetic neuralgia a randomized, double-blinded, controlled trial. Clin J Pain. 2018;34(11):1017–24.
Huang XH, Ma YF, Wang WM, et al. Efficacy and safety of pulsed radiofrequency modulation of thoracic dorsal root ganglion or intercostal nerve on postherpetic neuralgia in aged patients: a retrospective study. BMC Neurol. 2021;21(1):8.
Zhang H, Ni H, Liu S, et al. Supraorbital nerve radiofrequency for severe neuralgia caused by herpes zoster ophthalmicus. Pain Res Manage. 2020;2020:1–7.
Chen YJ, Liu XL, Xu SS, et al. Anatomy of the trigeminal nerve and its clinical significance via fusion of computed tomography and magnetic resonance imagery. Pain Physician. 2022;25(2):E293–8.
Ding Y, Hong T, Li H, et al. Efficacy of CT guided pulsed radiofrequency treatment for trigeminal postherpetic neuralgia. Front Neurosci. 2019;13:708.
Li HX, Ding YY, Zhu YQ, et al. Effective treatment of postherpetic neuralgia at the first branch of the trigeminal nerve by high-voltage pulsed radiofrequency. Front Neurol. 2021;12:8.
Ding YY, Yao P, Li HX, et al. CT-guided stellate ganglion pulsed radiofrequency stimulation for facial and upper limb postherpetic neuralgia. Front Neurosci. 2019;13:8.
Kim YS, Son JS, Lee H, et al. A case report of refractory otalgia after Ramsay Hunt syndrome successfully treated by applying pulsed radiofrequency to the great auricular nerve. A CARE-compliant article. Medicine. 2021;100(39):4.
Zhou HS, Li TT, Pi Y, et al. Ultrasound-guided selective pulsed radiofrequency treatment of great auricular nerve for post-herpetic neuralgia of the head and neck: a case report. J Pain Res. 2021;14:3301–7.
Sun Z, Liu L, Liu H, et al. Effect of CT-guided gasserian ganglion block with local anesthetics and steroids on acute/subacute zoster-related trigeminal neuralgia: a multicenter retrospective study. J Pain Res. 2022;15:2303–13.
Li M, Hu H, Tong SX, et al. The therapeutic efficacy of pulsed radiofrequency alone versus a dexamethasone and pulsed radiofrequency combination in patients with trigeminal postherpetic neuralgia: a double-blind, randomized controlled trial. Pain Physician. 2022;25(4):E543–9.
Ma L, Yao M. Safety and efficacy of CT-guided pulsed radiofrequency combined with steroid and ozone injection-treated cervical 3–8 herpes zoster neuralgia using a posterior and upper quarter of the cervical foramina puncture approach. J Pain Res. 2022;15:23–32.
Li LM, Zhang ZL, Zheng BS, et al. Effective treatment of high-voltage pulsed radiofrequency combined with oxygen-ozone injection in acute zoster neuralgia. Clin Neurol Neurosurg. 2022;223:107496.
Wang RX, Ni HD, Xie KY, et al. Analysis of the efficacy and safety of CT-guided dorsal root ganglion pulsed radiofrequency combined with ozone injection in the treatment of acute herpes zoster neuralgia in the neck and upper extremities. Zhonghua Yi Xue Za Zhi. 2023;103(7):500–5.
Wang X, Yu J, Han CF, et al. The effect of CT-guided pulsed radiofrequency combined with ozone injection on zoster-associated pain: a retrospective study. J Pain Res. 2023;16:1321–32.
Li D, Sun GH, Sun HZ, et al. Combined therapy of pulsed radiofrequency and nerve block in postherpetic neuralgia patients: a randomized clinical trial. PeerJ. 2018;6:10.
Fei Y, Huang B, Deng JJ, et al. Efficacy of dorsal root ganglion pulsed radiofrequency combined with paravertebral injection of recombinant human interferon-alpha 2b in herpetic neuralgia. J Pain Res. 2021;14:711–9.
Fei Y, Yao M, Huang B, et al. Efficacy of internal heat acupuncture combined with high-voltage long-duration pulsed radiofrequency on subacute postherpetic neuralgia: a retrospective study. Pain Res Manag. 2022;2022:2180214.
Yamada K, Mori Y, Cui RZ, et al. Predictors of herpes zoster severity and immune responses according to pain trajectories: a community-based prospective cohort study. J Dermatol. 2023;50(8):1020–33.
Volpi A, Gatti A, Pica F, et al. Clinical and psychosocial correlates of post-herpetic neuralgia. J Med Virol. 2008;80(9):1646–52.
Wang XX, Zhang Y, Fan BF. Predicting postherpetic neuralgia in patients with herpes zoster by machine learning: a retrospective study. Pain Ther. 2020;9(2):627–35.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
This study was supported by the National Natural Science Foundation of China (82171216), China Postdoctoral Science Foundation (2022M712310), Zhejiang Provincial Traditional Chinese Medical Innovation Team (No. 2022-19), Key Discipline Established by Zhejiang Province and Jiaxing City Jointly—Pain Medicine (2019-ss-ttyx), and Jiaxing Key Laboratory of Neurology and Pain Medicine. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Min Rui, Longsheng Xu, and Ming Yao contributed to the study conception. Min Rui searched the literature and wrote the first draft of the manuscript. Longsheng Xu, and Ming Yao commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
Min Rui, Huadong Ni, Keyue Xie, Longsheng Xu, and Ming Yao have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rui, M., Ni, H., Xie, K. et al. Progress in Radiofrequency Therapy for Zoster-Associated Pain About Parameters, Modes, Targets, and Combined Therapy: A Narrative Review. Pain Ther 13, 23–32 (2024). https://doi.org/10.1007/s40122-023-00561-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00561-7