Abstract
Introduction
Mindfulness-based stress reduction (MBSR) has demonstrated its effectiveness in reducing pain-related stress in adults with chronic pain. However, the implementation of MBSR needs modifications across cultures. This pilot study reports the findings of a randomized controlled trial that investigated the effects of a culturally adaptive MBSR program on self-report and neuroimaging outcomes for chronic pain adults in China.
Methods
Sixty-seven participants were randomly assigned to the treatment group (n = 40) or the treatment-as-usual group (n = 27) group at a ratio of 1.5:1. Participants completed self-report measures of pain severity, pain interference, depression, perceived stress, pain catastrophizing, mindfulness, and resilience at baseline assessment (T1), post-treatment (T2), and 3-month follow-up (T3) assessments. Functional magnetic resonance imaging (fMRI) scanning was also performed at T1 and T3 assessments.
Results
For the intention-to-treat sample, the results of the mixed-effect model indicated that Group × Time interaction was significant for pain catastrophizing only (F (2, 130) = 3.51, p = 0.033). Compared with the control group, those in the MBSR group reported greater reductions in pain catastrophizing at T2 (d = − 0.60), though this effect was not maintained at T3 (d = − 0.05). Additionally, the results of completer analyses found significant Group × Time interactions for pain interference (F (2, 88) = 4.40, p = 0.015) and perceived stress (F (2, 88) = 3.13, p = 0.048), but not for other measures. Finally, both groups exhibited decreased regional homogeneity (ReHo) in the frontal lobe, while increased ReHo in the cerebellum anterior lobe was unique to the MBSR group.
Conclusions
The present findings suggest that the minor modified MBSR program improves certain pain-related outcomes for Chinese adults with chronic pain. Future studies with larger samples of Chinese chronic pain patients are needed to detect the small-to-moderate benefit of MBSR on fMRI and/or other objective methods.
Similar content being viewed by others
Why carry out this study? |
Chronic pain threatens individuals’ physical and mental health, and it brings economic burdens on individuals and society. Mindfulness-based stress reduction (MBSR) and its modified versions are widely used to reduce emotional distress among chronic pain samples. However, there is little known about the mechanisms of how the MBSR group could help in improving pain-related functioning in the Chinese context. |
We conducted a pilot randomized control trial study to investigate the effects of a culturally adaptive MBSR program on a culturally adaptive MBSR program on pain-related outcomes and their potential mechanistic variables via self-report and neuroimaging measures in Chinese adults with chronic pain. |
What was learned from the study? |
The minor modified MBSR program is more effective in reducing pain catastrophizing, pain interference, and perceived stress compared to the treatment-as-usual for adults with chronic pain in China. |
In addition, the increased regional homogeneity in the cerebellum anterior lobe was unique to the MBSR group, indicating that the minor modified MBSR program promotes brain plasticity in regulating muscular tension, which is a leading cause of pain, stiffness, and limited movement. |
Introduction
Chronic pain patients experience personal consequences, including social withdrawal, financial strain, lifestyle impairment, loss of gray matter, and emotional distress [1]. Furthermore, chronic pain has a huge economic impact on society in countries such as the United States [2], Switzerland [3], and China [4]. Approximately 25–35% of Chinese adults have experienced chronic pain [4, 5], and pain treatment is typically disease-based or symptom-based in clinical practice. Nevertheless, a significant number of chronic pain patients do not respond to medical treatments and face the risk of developing dependence on pain medication and experiencing disability [6]. Therefore, the goals of therapy are tailored towards an improved quality of life rather than meaningful pain reduction for many patients. Exercise and psychological interventions are important alternatives in managing pain, improving functioning, and maintaining a satisfactory quality of life [1].
Mindfulness-based interventions (MBIs), which include body movement and mindfulness meditation practices, have emerged as increasingly popular approaches to treating chronic pain [7]. The empirical foundation of MBIs can be traced back to the 8-week mindfulness-based stress reduction (MBSR) project developed by Jon Kabat-Zinn and colleagues at the University of Massachusetts Medical School in 1979 [8]. MBSR was developed to teach participants to attend to body sensations while decoupling pain sensations from emotional suffering so that they could improve their functioning despite ongoing pain [8].
In a network meta-analysis of 21 randomized controlled trials (RCTs) consisting of 1981 chronic pain patients, Khoo et al. examined the relative efficacy of MBSR, cognitive behavioral therapy (CBT), and control conditions [9]. MBSR and CBT were found to be significantly more effective than no treatment in reducing physical impairment and depressive symptoms, but not in pain severity [9]. Despite such evidence, research from highly populated Eastern nations has been somewhat underrepresented in this literature. For example, limited studies have investigated the effects of MBSR on pain-related dysfunction (e.g., pain severity, pain interference, emotional distress) in Chinese adults with pain conditions [10, 11]. Furthermore, there is a lack of research exploring the potential mechanisms underlying why and how MBSR could improve pain-related functioning in the Chinese context.
The biopsychosocial framework of pain may explain the underlying mechanisms of MBSR on pain-related dysfunction. Pain area theorists categorize individuals who limit activities to avoid painful experiences due to pain-related fear and catastrophizing as “avoiders” and those who recover from pain or function well despite ongoing pain as “confronters” [12, 13]. The confronters could also be characterized by resilience, a construct that has been defined as both a dynamic process and a relatively stable capacity to maintain physical and psychological functioning despite adversity [14]. Evaluations of general resilience and pain resilience among Chinese adults with chronic pain were related to lower pain catastrophizing levels and better pain-related functioning [15, 16].
The effects of MBSR in reducing pain catastrophizing among samples with chronic pain have been well documented [17, 18]. In contrast, few studies have investigated the effects of MBIs on resilience measures in chronic pain patients from the perspective of “confronters”. For example, an RCT for individuals with multiple sclerosis found that the MBSR group and the educational group did not have significant differences in general resilience improvements at 8 weeks or 12 months [19]. Conversely, a mind–body and activity intervention for chronic pain participants showed that a reduction in depression, but not anxiety, from baseline to post-treatment was explained by the increase in pain resilience [20]. However, this study did not have a control group. Therefore, RCTs are needed to verify whether pain catastrophizing and/or resilience could be potential psychological mechanisms underlying MBSR effects on pain-related dysfunction in the Chinese context.
The Monitor and Acceptance Theory (MAT) explains the mechanism of trait mindfulness and MBIs effects on cognition, affect, stress, and health outcomes. The theory highlights the importance of attention monitoring and acceptance to increase awareness of one’s experience and reduce affective reactivity, respectively [21]. Accordingly, Cillessen et al. investigated the effects of MBIs on psychological and physical health outcomes based on 29 RCTs of 3274 cancer patients and survivors [22]. Compared to control conditions, MBIs were superior in mindfulness skills, self-compassion, rumination, and psychological distress, with small but significant post-treatment effect sizes reported, while the post-treatment effect size for pain was not statistically significant. Preliminary findings also partially supported the utility of MAT among Chinese patients with chronic musculoskeletal pain. The “describing one’s experience” and “acting with awareness” components contributed an additional 5–21% to the prediction of depression, perceived stress, and pain catastrophizing after controlling for demographics and pain experience [23]. Again, it remains unclear whether mindfulness skills could be potential psychological mechanisms underlying MBSR effects on pain-related dysfunction in the Chinese context.
Psychosocial factors are primarily assessed by self-report measures, yet only a few RCT studies have addressed the neural basis of MBSR for patients with chronic pain and the results were inconsistent. For instance, one RCT study investigating enhanced MBSR effects in patients with episodic migraine found that there were no treatment-by-time effects in gray matter volume (GMV), although both groups (MBSR group and stress management control group) showed decreased anterior midcingulate volume at week 20 [24]. A more recent study investigated MBSR effects on GMV in selected breast cancer survivors with chronic neuropathic pain from a larger RCT and found that the MBSR group (n = 13) had greater GMV in the angular gyrus and middle frontal gyrus post-training compared to controls (n = 10). Additionally, the MBSR group had increased GMV in the right parahippocampal gyrus whereas the control group had decreased GMV in the left parahippocampal gyrus, precuneus, middle temporal gyrus, and right cuneus from pre- to post-training [25]. In addition, MBSR effects on resting-state brain activity in chronic pain samples are lacking, although there are preliminary findings immediately at post-treatment in pain-free participants. Specifically, the pain-free MBSR group had a decreased amplitude of low-frequency fluctuations (ALFF) in the cingulate gyrus/cortex, left anterior and posterior insula, and left superior medial frontal gyrus from pre- to post-training [26, 27] and an increased regional homogeneity (ReHo) in the right superior parietal lobule and left postcentral gyrus from pre- to post-training [28]. In summary, it remains unclear whether changes in brain structure and resting-state brain activity caused by MBSR training could be sustained over a longer follow-up duration in chronic pain patients.
To this end, we conducted a pilot RCT that compared MBSR and treatment-as-usual groups among Chinese adults with chronic pain. We aimed to investigate MBSR effects on self-report pain-related dysfunction (i.e., pain intensity, pain interference, depression, perceived stress), pain catastrophizing, resilience (i.e., general resilience, pain resilience), and mindfulness (i.e., describe one’s experience, act with awareness, non-judgment of inner experience) at post-treatment and 3-month follow-up assessments. Additionally, for exploratory purposes, we performed functional magnetic resonance imaging (fMRI) to assess MBSR effects on brain structure (i.e., GMV) and resting-state brain activity (i.e., ReHo, ALFF, fractional ALFF) at the 3-month follow-up.
Methods
Participants
The study protocol was approved by the Research Ethics Committee of Southwest University (No. H21034). The study was carried out in compliance with the most recent iteration of the Helsinki Declaration and adhered to all other stipulations outlined by the local legislation of China. The participants were recruited from local hospitals, the university campus, and communities in Chongqing, China. Based on the results of a recently published pilot RCT examining MBSR effects on migraine [29], a minimal sample size of 60 participants was determined for a pilot RCT study. Written informed consent was obtained from all participants.
Eligibility for the study was assessed using an online screening questionnaire. Inclusion criteria were as follows: (1) willing and able to provide informed consent, (2) aged 18 to 65 years, (3) reported pain duration of at least for 3 months and painful days for at least 60 days within the past 3 months, (4) able to read and write in Chinese, (5) agreeing to complete homework if assigned to the treatment group, (6) meet the criteria for fMRI scanning. Meanwhile, exclusion criteria were: (1) no Internet access, (2) prior participation in any structured mindfulness training, (3) regular meditation practice (more than once per month), (4) unable or unwilling to commit to the prescribed amount of sessions and home practice, (5) concurrent enrollment in another study assessing a pharmacological or psychological treatment for chronic pain, (6) diagnosis of psychiatric disorder, (7) participants with pacemaker, metal implants, dentures, severe claustrophobia.
Procedure
Randomization
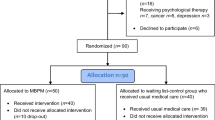
A CONSORT flow diagram is depicted in Fig. 1. Among the 139 patients assessed for eligibility, 89 were eligible and invited for the first assessment visit. Among the eligible participants, 22 declined to participate, leaving 67 eligible participants to be randomized in the study. The participants provided written consent, which outlined the vague purpose of the present study and assessment schedules. Of these, 40 were randomized to the mindfulness group (MBSR) and 27 were assigned to the treatment-as-usual group (TAU), according to a ratio of 1.5:1 between MBSR and TAU. This ratio was employed because the participants in the treatment group were more likely to drop out [30, 31]. Excel software was used to generate the random number, with a range of 0–1. Twenty-seven participants with the lowest sequence scores were assigned to the TAU and the remaining 40 participants were allocated to the MBSR group. Participants were given the chance to one of the three MBSR classes to attend, based on their schedule. Once they decided to attend the class at a particular time, they were not allowed to change the class throughout the treatment period. Finally, a total of three MBSR classes, with 9 to 16 participants per course, were conducted in the laboratory (Class 1, n = 15; Class 2, n = 9; Class 3, n = 16). It should be noted that five participants in the MBSR group did not attend any mindfulness courses but they participated in the online group discussion after classes, were available for mindfulness practice recordings, and completed self-report questionnaires at all three assessments (Fig. 1).
Modified Mindfulness-Based Stress Reduction Program
The modified MBSR training was conducted on the campus of Southwest University. Participants were instructed to continue their stable use of prescribed preventative treatments and continue taking acute abortives as needed. Considering the health conditions of the sample, we reduced the regular class duration from 2.5–3 h to 2–2.5 h. The separate groups for each intervention met for about 2.5 h for weeks 1 and 8 and 2 h weekly for weeks 2–7. One-day retreat practice was not conducted. Therefore, the total MBSR course duration was 17 h. Two instructors, certified as the MBSR teacher or under supervision, guided the MBSR courses in Chinese. In line with a manualized protocol that included participant handouts and materials for home use [8, 32], we also made several modifications based on characteristics of the current sample. For example, the people of Chongqing enjoy spicy foods, an almost painful sensation on the tongue. Savoring spicy foods in daily life could challenge the mindset that painful sensation is terrible and hateful. The outline of the modified MBSR course for Chinese adults with chronic pain is listed in the Electronic Supplementary Material (Table S1). Specifically, we focused on trauma-informed methods, disassociation among painful sensations, ruminative thoughts and sufferings, and emphasized loving kindness to distress and self-compassion.
Mindfulness practice sections in Class 1 were audio-recorded and transferred to written scripts, which were used by the junior instructor to guide Class 2 and Class 3 to increase the treatment fidelity. Of note, the mindfulness expert provided real-time online courses for weeks 5–7 because of health conditions that made it difficult to visit the laboratory during that period. A master-level student majoring in applied psychology assisted with the course and managed the online group community. Missed sessions were made up by sending the mindfulness practice audio that was recorded in class. Research staff conducting the assessments were blind to the study allocation.
Assessment Schedule
Baseline (Time [T]1), post-treatment (T2), and 3-month follow-up (T3) consisted of a battery of self-report questionnaires, which will be described in detail in the following section. The questionnaire took approximately 20–40 min to complete. All participants completed the written questionnaires at the T1 assessment during their visit to our laboratory. Those participants who were unavailable for the T2 and/or T3 visits completed the questionnaires online. In addition, participants attended the fMRI scanning at the T1 and T3 assessments, with 8 min allocated for acquiring resting-state brain activity and 6 min for collecting brain structure imaging. The imaging-acquisition procedure is described in detail in the Electronic Supplementary Material. Participants received minor compensation at each assessment.
Outcome Measures
Self-Report Measures
The Chronic Pain Grade (CPG) evaluates pain severity and pain interference across three items each [33]. Items measuring current pain, average pain, and most severe pain over the previous 3 months rated from 0 (no pain at all) to 10 (most severe pain). The pain interference tests how much the pain has interfered with daily activities, social activities, and work abilities rated from 0 (no interference) to 10 (unable to carry out activities/extreme change over the past 3 months). The subscale average scores were used. Previous investigations have validated CPG in Chinese chronic pain samples [15].
The 20-item Center for Epidemiologic Studies Depression (CES-D) scale was used for measuring depressive symptomatology [34]. Participants rated the frequency of each symptom throughout the previous week from 0 (rarely or never [less than 1 day]) to 3 (most or always [5–7 days]). The CES-D has been shown to be reliable and valid in Chinese adults with chronic pain [23].
Perceived positive and negative stress reactions were measured by the ten-item Perceived Stress Scale (PSS-10) [35] based on the original 14-item PSS [36]. In a sample of Chinese patients, a hierarchical two-factor PSS-10 structure outperformed the 14-item PSS and the four-item PSS in terms of overall psychometric qualities [35].
The 12-item Mindfulness Questionnaire (MQ-12) [37] was adopted from the 39-item FFMQ, which measures five aspects of mindfulness in its original form [38]. The MQ-12 evaluated three aspects of mindfulness: describing one’s experience, acting with awareness, and non-judgment of inner experience. Items are rated from 1 (very seldom true) to 5 (always true). A more proficient level was indicated by higher overall scores for each facet of mindfulness. The MQ-12 was validated in Chinese university students [37] and Chinese chronic pain individuals [23].
The 13-item Pain Catastrophizing Scale (PCS) measures a person’s propensity for pain catastrophizing, which includes feelings of helplessness, magnifying pain, and ruminating about it [39]. Scores for each PCS item range from 0 (not at all) to 4 (always). Previous studies showed that PCS has acceptable psychometrics among Chinese individuals with chronic pain [40].
The original 14-item Pain Resilience Scale (PRS) was used to assess a person’s capacity to successfully manage or adapt to pain [41]. Items are rated between 0 (never) and 4 (all the time), with higher total scores indicating more pain resilience. The 12-item PRS was optimal for Chinese adults with chronic musculoskeletal pain [16].
The six-item Brief Resilience Scale (BRS) was employed to assess one’s general capacity to bounce back from adversities [42]. In an initial validation study with four independent samples, the BRS was shown to have a unitary factor structure and strong convergent and discriminant validity [42]. Moreover, the BRS had good reliability in Chinese young adults [43].
Brain Structure
Gray matter volume (GMV) is an index of gray matter density defined as the product of cortical thickness and cortical surface area [44]. GMV changes could be as a function of genetics, aging, and pathology as well as in response to particular training [45]. The voxel-based morphometry (VBM) was employed to investigate focal differences in GMV [46].
Resting-State Brain Activity
The amplitude of low-frequency fluctuation (ALFF), the fractional amplitude of low-frequency fluctuation (fALFF), and regional homogeneity (ReHo) were used to assess resting-state brain activity measured by functional magnetic resonance imaging (fMRI). ALFF refers to the averaged square root of power spectra within a low-frequency oscillation range (e.g., 0.01–0.1 Hz) from fast Fourier transformations [47]. The fALFF measures the ratio of fluctuations within the low-frequency band to the entire frequency range, providing information on relative amplitudes in low frequencies [48].
Demographic Information
We collected information on participants’ age, gender, body mass index (BMI), the highest education level (1 [primary school or lower], 2 [middle school completion or partial completion], 3 [high school completion or partial completion], 4 [post-secondary education]), ethnicity, pain duration (months), primary pain site, prescribed analgesic usage, and presence or absence of pain every day in the past week.
Data Analyses
Self-Report Measures
All statistical analyses were conducted in RStudio (version 1.2.5033; RStudio Team, 2019) based on the R programming environment (Version 3.6.3; R Core Team, 2019). Initially, independent samples t tests and chi-square tests were conducted to analyze baseline differences in patient characteristics between intervention groups. Mean scores at baseline (T1), post-treatment (T2), and 3-month follow-up (T3) were derived from linear mixed-effects models, which account for the within-subject correlation of responses over time and enable the use of all available data across all time points to increase statistical efficiency [49]. The intervention group and time point were treated as fixed effects. Group × Time interaction was assessed to determine whether participants randomized to MBSR differ from those randomized to TAU for change from T1 to T2, and from T1 to T3 on outcomes; the significance level is reported for the Group × Time interaction. Moreover, we reported the between-group effect sizes of change from T1 to T2, and from T1 to T3, as Cohen’s d (0.20 small; 0.50 medium; 0.80 large). We conducted intent-to-treat (ITT) analyses involving the entire randomized participants and “completer” analyses limiting the MBSR group who attended at least four sessions [50].
Imaging Outcomes
Imaging preprocessing is described in the Supplementary Materials. We included the sample of individuals who completed both T1 and T3 fMRI scanning with adequate data quality and participants in the MBSR group attended at least four treatment sessions. Initially, full factorial analysis was conducted on GMV via SPM. Then, the paired t test was performed on each group if the Group × Time interaction was significant. Age, gender, and total intracranial volume (TIV) were included as covariates for all GMV analyses per conventions of VBM [51]. Voxels with GMV values under 0.2 were excluded using absolute threshold masking. A threshold of p < 0.05 with a false discovery rate (FDR) correction at the voxel level and a cluster size over 40 voxels were used to identify peak clusters on which subgroups differed [52].
As for resting-state brain activity, mixed-effects models of Group × Time with covariates (age, gender, head motion) were conducted using the Data Processing & Analysis for Brain Imaging toolbox (DPABI 4.0, http:/rfmri.org/dpabi). Again, the paired t test with head motion as the covariate was applied for each group if the Group × Time interaction was significant. Gaussian random field (GRF) correction (voxel level p < 0.05, cluster level, p < 0.05, two-tailed) was conducted for each analysis.
Results
Baseline Characteristics
The intervention groups did not differ significantly in demographics (age, gender, education, BMI, ethnicity, work status) and pain information (pain duration, primary pain site, analgesic use, pain every day) (see Table 1 for details).
The “completer” was defined as attendance in at least four MBSR classes; 19 of 40 chronic pain patients (47.5%) randomized to MBSR condition were considered treatment completers. The mean number of MBSR class sessions attended was 3.78 (SD 2.78 sessions; range, 0–8 sessions). The research compliance rate was 100%, with all the participants completing the post-test questionnaire assessment and the 3-month follow-up assessment. Notably, all participants visited our laboratory for the baseline questionnaire assessment. Twenty-seven participants (40.3%) and 14 participants (10.9%) at post-treatment and 3-month follow-up were unable to come to the laboratory, so their self-report data were provided online via the link from the Questionnaire Platform Wenjuanxing. Items of the online version are the same as those in the printed scales.
Self-Report Outcomes
Intention-to-Treat Analyses
Mean and standard deviation scores for outcome measures over time based on the intention-to-treat sample are presented in the Supplementary Material (Table S2). Figure 2 depicts a significant Group × Time interaction for pain catastrophizing (F (2, 130) = 3.51, p = 0.033, partial η2 = 0.05). Compared with chronic pain patients randomized to the TAU group, those in the MBSR group reported greater reductions in pain catastrophizing at post-treatment with a medium effect size (t (130) = − 2.39, p = 0.018, d = − 0.60), but this effect did not persist at 3-month follow-up (t (130) = − 0.21, p = 0.836, d = − 0.05). No significant differences were observed between Group × Time interactions in pain (i.e., pain severity, pain-related interference, emotional distress (i.e., depression, perceived stress), mindfulness skills (i.e., describe one’s experience, act with awareness, non-judgment of inner experience), and resilience levels (i.e., general resilience, pain resilience).
Completer Analyses
Chronic pain patients randomized to the MBSR group who attended at least four classes (completers) were compared with those randomized to the TAU group (see Supplementary Material Table S3). Significant Group × Time interactions were observed in pain interference (F (2, 88) = 4.40, p = 0.015, partial η2 = 0.09) and perceived stress (F (2, 88) = 3.13, p = 0.048, partial η2 = 0.07). Corresponding figures are depicted in Fig. 3a and b. Compared with those in the TAU group, chronic pain patients in the MBSR group reported greater reductions in pain interference at post-treatment with a large effect size (t (88) = − 2.93, p = 0.004, d = -0.91) and marginally significant effect at 3-month follow-up (t (88) = − 1.86, p = 0.066, d = − 0.56). The MBSR group did not report greater reductions in perceived stress at immediate post-intervention assessment (t (88) = − 0.69, p = 0.484, d = − 0.21) but reported greater reductions at 3 months with a medium-to-large effect size (t (88) = − 2.43, p = 0.017, d = − 0.74). Finally, the differences between Group × Time interactions were not significant in pain severity, depression, mindfulness skills, pain catastrophizing, and resilience levels.
Imaging Outcomes
Sixty-seven and 53 participants completed the T1 and T3 fMRI scanning, respectively. Sixteen participants in the MBSR group who completed scanning but attended fewer than four sessions were excluded from analyses. Furthermore, three participants in the TAU group who had head motion larger than 3.0 mm and 3.0 degrees were also excluded from resting-state fMRI analyses. Final samples comprised 37 (MBSR = 16, TAU = 21) participants for GMV and 34 (MBSR = 16, TAU = 18) participants for resting-state fMRI outcomes (i.e., ALFF, fALFF, ReHo).
Group Differences in Resting-State Brain Activity
Age, gender, and head motion were included as covariates conventionally. Figure 4 illustrates the overall brain resting-state ReHo results for the Group × Time interaction of the mixed-effects model. The peak MNI coordinate was found to be − 54 − 63 − 39 and the peak MNI coordinate region was identified as the cerebellum posterior lobe with 950 voxels. The peak intensity was 5.25. Paired t tests were conducted within each group to detect T3-T1 changes. Both groups showed decreased ReHo in the frontal lobe while the increased ReHo in the cerebellum anterior lobe was unique to the MBSR group (Fig. 5). Compared with the baseline assessment, the MBSR group had increased ReHo in the cerebellum anterior lobe [peak MNI coordinate: 9 − 42 − 27, 109 voxels, peak intensity: 3.35] and decreased ReHo in the frontal lobe [peak MNI coordinate: − 6 63 − 12, 71 voxels, peak intensity: - 2.94] at 3-month follow-up. The TAU group also showed decreased ReHo in the frontal lobe [peak MNI coordinate: 39 48 15, 182 voxels, peak intensity: − 4.33]. Finally, no significant Group × Time interaction was observed in ALFF and fALFF measures.
Whole-brain resting-state regional homogeneity (ReHo) results for the interaction of mixed-effects model. a depictes the interaction at three-dimension. b shows the peak MNI Z-coordinate. Blue crosshairs are localized at the default position. The peak MNI coordinate is − 54 − 63 − 39. The peak MNI coordinate region is the cerebellum posterior lobe with 950 voxels. The peak intensity is 5.25. The color guide represents F values with Gaussian random field (GRF) correction
Whole-brain resting-state ReHo results for each group (T3 > T1). a The mindfulness-based stress reduction group had increased ReHo in the cerebellum anterior lobe and decreased ReHo in the frontal lobe at the 3-month follow-up compared to baseline. b The treatment-as-usual group had decreased ReHo in the frontal lobe at 3-month follow-up compared to baseline. The color guide represents t values with GRF correction
Group Differences in Brain Structure
In the GMV analyses, age, gender, and TIV were included as the conventional covariates. The MBSR and TAU groups did not differ significantly in total mean GMV [MBSR group: M = 603.19 ml, SD = 73.84 ml; TAU group: M = 623.91 ml, SD = 71.81 ml, t = − 0.86, p = 0.399]. Finally, no significant Group × Time interaction was detected for GMV.
Discussion
This study was designed to evaluate the efficacy of the 8-week mindfulness-based stress reduction (MBSR) (versus treatment as usual, TAU) among Chinese adults with chronic pain via evaluating self-report pain- and mindfulness-related measures at post-treatment (compared with baseline) and at 3-month follow-up (compared with baseline). In addition, we examined the effects of MBSR on brain structure and resting-state brain activity at baseline and 3-month follow-up assessments. This pilot randomized controlled trial (RCT) shows that the 8-week MBSR program can serve as a promising intervention for Chinese adults with chronic pain.
Intention-to-treat (ITT) analyses of all randomized samples for self-report measures found significant Group × Time interaction in pain catastrophizing, but not in other pain- or mindfulness-related measures. Compared to the control group, the MBSR group had a greater reduction in pain catastrophizing (e.g., worry about the recurrent pain and ruminate the consequences of pain in the future) at post-treatment assessment, which was consistent with past RCT studies on mindfulness effects for clinical pain samples [17, 53]. The immediate reduction in pain catastrophic beliefs in the MBSR group, regardless of the number of attended sessions, suggests that the mindfulness attitudes towards pain (e.g., present-moment awareness and acceptance of body sensations/unpleasantness) embodied throughout the training confronted the pain catastrophizing, which is the predominately vulnerable factor of pain-related dysfunction in the fear-avoidance model [13].
In the ITT sample, MBSR effects were not sustained at 3-month follow-up for either pain catastrophizing or other self-report measures. It is reasonable that the intervention effect will fade away gradually in the long term. Another possible reason for the null intervention effect in the long term is that participants who failed to master the essential mindfulness skills as required are less likely to keep practicing and to ensure the benefit from mindfulness training [50]. The ITT sample included all participants, among whom, several might not have fully gained mindfulness meditation skills. Furthermore, we also conducted completer analyses, which included participants in the MBSR group who had completed at least four sessions.
The completer analyses found significant Group × Time interactions for pain interference and perceived stress. Compared with the control group, the MBSR group had a greater reduction in pain interference at post-treatment and reduction in perceived stress at 3-month follow-up. The results are in line with the recommendation that goals of pain management should be tailored towards improving functioning and maintaining a satisfactory quality of life [1]. However, we did not find the intervention effect in mindfulness-related measures for ITT and completer analyses. This might be due to these measures testing general and dispositional mindfulness rather than pain-specific and state mindfulness, though we selected valid mindfulness measures for Chinese adults with chronic pain [23]. Future studies can focus on developing valid mindfulness measures more sensitive to pain conditions.
Regarding MBSR effects on brain structure and resting-state brain activity at 3-month follow-up compared to baseline assessment, we only found a significant Group × Time interaction on regional homogeneity (ReHo) of the anterior cerebellum lobe. Previous research has shown that higher ReHo of the cerebellum lobe is linked to better functioning in patients with major depression disorder and in male patients with severe obstructive sleep apnea [54, 55]. The unique improvement of ReHo in the cerebellum posterior lobe for the MBSR group revealed the objective evidence supporting the effectiveness of MBSR for Chinese adults with chronic pain. We also found a reduction in ReHo in the frontal lobe for both groups, while we observed no MBSR effects on gray matter volume, resting-state brain activity of amplitude of low-frequency fluctuation (ALFF), or functional ALFF values. These findings are in line with previous fMRI studies on MBSR effects among samples with clinical pain conditions, which showed mixed results [24, 56]. Thus, more RCTs with rigorous design employing similar measured outcomes and whole-brain analyses are warranted to verify the reliability of brain changes and to help understand neural mechanisms underlying mindfulness training for chronic pain patients [7].
Key strengths of the present study included the employment of a methodologically rigorous RCT design with both subjective and objective pain-related outcomes, the involvement of a qualified MBSR facilitator under the discipline of internationally authorized mindfulness training, and the benefit of Chinese local residents from the MBSR program. In addition, we examined both vulnerable factors (e.g., pain catastrophizing) and protective factors (e.g., pain resilience) underlying the effects of MBSR on pain-related dysfunction, although group difference at post-treatment was only marginally significant for pain resilience. Our study is noteworthy for comparing MBSR training vs. treatment-as-usual in a chronic pain sample in the Chinese context, as existing fMRI studies reported mindfulness effects in chronic pain samples mainly from Western cultures [24, 56].
Despite its strength, this study also had several limitations. First, given its pilot nature, small-to-medium effect sizes of MBSR effects (e.g., pain resilience) were not statistically significant. Despite the growing publication of MBI effects in populations with clinical pain, plenty of RCTs were underpowered and deemed exploratory in nature [9, 22]. Therefore, more studies with adequate power are needed to detect the small-to-moderate benefit of MBSR on fMRI and/or other objective measures in the future. Second, the rate of completers in this chronic pain sample was below 50%, though consistent with previous findings that patients with headache pain reported a low percentage of completers in past pilot RCT studies [30]. Participants with chronic pain may not find mindfulness meditation “useful” (i.e., alleviate pain immediately) during the first class, which may cause a loss of interest in mindfulness. Conducting the mindfulness training in a university setting rather than in a hospital could also make patients feel less convenient and less convinced, even though our mindfulness expert is a senior physician with MBSR teacher certification. Third, the likely selection bias limited the generalizability of the study due to the strenuous participation requirements, such as willingness, competency, and time commitment to complete in-person courses and repeated assessments in Chongqing, China.
Conclusions
Results from self-report measures and resting-state brain activity suggested the preliminary effectiveness of the minor modified MBSR program for chronic pain patients in southwest China. This is the first study with neuroimaging evidence supporting the brain plasticity of MBSR in regulating muscular tension for Chinese adults with chronic pain. Future studies with larger samples of Chinese chronic pain patients are needed to detect the small-to-moderate benefit of MBSR on fMRI and/or other objective methods. Future studies targeting chronic pain samples may consider conducting mindfulness training in clinical settings to reduce the time burden for participation, which will be convenient for patients who need to meet physicians regularly. Furthermore, the mindfulness treatment protocol for chronic pain samples may need to be appropriately reorganized in a more specific category (e.g., middle-aged and elderly Chinese people with headaches and menopausal women with chronic low back pain).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021;397(10289):2082–97.
Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–24.
Scholz-Odermatt SM, Luthi F, Wertli MM, Brunner F. Direct health care cost and work incapacity related to complex regional pain syndrome in Switzerland: a retrospective analysis from 2008 to 2015. Pain Med. 2019;20(8):1559–69.
Qiu Y, Li H, Yang Z, et al. The prevalence and economic burden of pain on middle-aged and elderly Chinese people: results from the China Health and Retirement Longitudinal Study. BMC Health Serv Res. 2020;20(1):1–10.
Jackson T, Chen H, Iezzi T, Yee M, Chen F. Prevalence and correlates of chronic pain in a random population study of adults in Chongqing. China Clin J Pain. 2014;30(4):346–52.
Fishbain DA, Cole B, Lewis J, Rosomoff HL, Rosomoff RS. What percentage of chronic nonmalignant pain patients exposed to chronic opioid analgesic therapy. Pain Med. 2008;9(4):444–59.
Wielgosz J, Goldberg SB, Kral TRA, Dunne JD, Davidson RJ. Mindfulness meditation and psychopathology. Annu Rev Clin Psycho. 2019;15:285–316.
Kabat-Zinn J. Full catastrophe living: using the wisdom books of your body and mind to face stress, pain, and illness. New York: Delacorte; 1990.
Khoo EL, Small R, Cheng W, et al. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network meta-analysis. Evid-Based Ment Heal. 2019;22(1):26–35.
Wong SYS, Chan FWK, Wong RLP, et al. Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain: a randomized comparative trial. Clin J Pain. 2011;27(8):724–34.
Zhu X, Hu P, Fan Z, et al. Effects of mindfulness-based stress reduction on depression, anxiety, and pain in patients with postherpetic neuralgia. J Nerv Ment Dis. 2019;207(6):482–6.
Crombez G, Vervaet L, Lysens R, Baeyens F, Eelen P. Avoidance and confrontation of painful, back-straining movements in chronic back pain patients. Behav Modif. 1998;22(1):62–77.
Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–32.
Sturgeon JA, Zautra AJ, Arewasikporn A. A multilevel structural equation modeling analysis of vulnerabilities and resilience resources influencing affective adaptation to chronic pain. Pain. 2014;155(2):292–8.
Chen S, Jackson T. Pain beliefs mediate relations between general resilience and dysfunction from chronic back pain. Rehabil Psychol. 2018;63(4):604–11.
You B, Jackson T. Factor structure and construct validity of the pain resilience scale within Chinese adult chronic musculoskeletal pain samples. J Pers Assess. 2021;103(5):685–94.
Turner JA, Anderson ML, Balderson BH, Cook AJ, Sherman KJ, Cherkin DC. Mindfulness-based stress reduction and cognitive-behavioral therapy for chronic low back pain: similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain. 2016;157(11):2434–44.
Wells RE, O’Connell N, Pierce CR, et al. Effectiveness of mindfulness meditation vs headache education for adults with migraine: a randomized clinical trial. JAMA Intern Med. 2021;181(3):317–28.
Senders A, Hanes D, Bourdette D, Carson K, Marshall LM, Shinto L. Impact of mindfulness-based stress reduction for people with multiple sclerosis at 8 weeks and 12 months: a randomized clinical trial. Mult Scler J. 2019;25(8):1178–88.
Grunberg VA, Mace RA, Bannon SM, Greenberg J, Bakhshaie J, Vranceanu AM. Mechanisms of change in depression and anxiety within a mind–body activity intervention for chronic pain. J Affect Disorders. 2021;292:534–41.
Lindsay EK, Creswell JD. Mechanisms of mindfulness training: monitor and acceptance theory (MAT). Clin Psychol Rev. 2017;51:48–59.
Cillessen L, Johannsen M, Speckens AE, Zachariae R. Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: a systematic review and meta-analysis of randomized controlled trials. Psychooncology. 2019;28(12):2257–69.
Chen S, You B, Jackson T. Facets of mindfulness as predictors of emotional distress among Chinese adults with chronic musculoskeletal pain. Mindfulness. 2021;12(3):775–83.
Seminowicz DA, Burrowes SAB, Kearson A, et al. Enhanced mindfulness-based stress reduction in episodic migraine: a randomized clinical trial with magnetic resonance imaging outcomes. Pain. 2020;161(8):1837–46.
Hatchard T, Penta S, Mioduszewski O, et al. Increased gray matter following mindfulness-based stress reduction in breast cancer survivors with chronic neuropathic pain: preliminary evidence using voxel-based morphometry. Acta Neurol Belg. 2022;122:735–43.
Gan Q, Ding N, Bi G, et al. Enhanced resting-state functional connectivity of low-frequency fluctuations of the salience network in mindfulness novices. Front Hum Neurosci. 2022;16: 838123.
Yang CC, Barros LA, Li M, et al. Alterations in brain structure and amplitude of low-frequency after 8 weeks of mindfulness meditation training in meditation-naive subjects. Sci Rep. 2019;9(1):10977.
Xiao Q, Zhao X, Bi G, et al. Alterations of regional homogeneity and functional connectivity following short-term mindfulness meditation in healthy volunteers. Front Hum Neurosci. 2019;13:376.
Simshäuser K, Lüking M, Kaube H, Schultz C, Schmidt S. Is mindfulness-based stress reduction a promising and feasible intervention for patients suffering from migraine? A randomized controlled pilot trial. Complement Med Res. 2020;27(1):19–30.
Day MA, Thorn BE, Ward LC, et al. Mindfulness-based cognitive therapy for the treatment of headache pain: a pilot study. Clin J Pain. 2014;30(2):152–61.
Dowd H, Hogan MJ, McGuire BE, et al. Comparison of an online mindfulness-based cognitive therapy intervention with online pain management psychoeducation. Clin J Pain. 2015;31(6):517–27.
Santorelli SF, Kabat-Zinn J, Blacker M, Meleo-Meyer F, Koerbel L. Mindfulness-based stress reduction (MBSR) authorized curriculum guide. Center for Mindfulness in Medicine, Health Care, and Society (CFM). University of Massachusetts Medical School; 2017.
Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50(2):133–49.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1(3):385–401.
Leung DY, Lam T, Chan SS. Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health. 2010;10(1):1–7.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Duan W, Li J. Distinguishing dispositional and cultivated forms of mindfulness: item-level factor analysis of five-facet mindfulness questionnaire and construction of short inventory of mindfulness capability. Front Psychol. 2016;2016(7):1348.
Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45.
Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524–32.
Yap JC, Lau J, Chen PP, et al. Validation of the Chinese Pain Catastrophizing Scale (HK-PCS) in patients with chronic pain. Pain Med. 2008;9(2):186–95.
Slepian PM, Ankawi B, Himawan LK, France CR. Development and initial validation of the pain resilience scale. J Pain. 2016;17(4):462–72.
Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200.
Fung SF. Validity of the brief resilience scale and brief resilient coping scale in a Chinese sample. Int J Environ Res Public Health. 2020;17(4):1265.
Rais M, Van Haren NE, Cahn W, et al. Cannabis use and progressive cortical thickness loss in areas rich in CB1 receptors during the first five years of schizophrenia. Eur Neuropsychopharm. 2010;20(12):855–65.
Draganski B, Gaser C, Busch V, Schuierer G, Bogdahn U, May A. Changes in grey matter induced by training. Nature. 2004;427(6972):311–2.
Ashburner J, Friston KJ. Voxel-based morphometry—the methods. Neuroimage. 2000;11(6):805–21.
Yan C, Cheung B, Kelly C, et al. A comprehensive assessment of regional variation in the impact of head micromovements on functional connectomics. Neuroimage. 2013;76:183–201.
Zou Q, Zhu C, Yang Y, et al. An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: fractional ALFF. J Neurosci Meth. 2008;172(1):137–41.
Demidenko E. Mixed models: theory and applications. Hoboken: Wiley; 2004.
Kearney DJ, Simpson TL, Malte CA, Felleman B, Martinez ME, Hunt SC. Mindfulness-based stress reduction in addition to usual care is associated with improvements in pain, fatigue, and cognitive failures among veterans with Gulf War illness. Am J Med. 2016;129(2):204–14.
Malone IB, Leung KK, Clegg S, et al. Accurate automatic estimation of total intracranial volume: a nuisance variable with less nuisance. Neuroimage. 2015;104:366–72.
Genovese CR, Lazar NA, Nichols T. Thresholding of statistical maps in functional neuroimaging using the false discovery rate. Neuroimage. 2002;15(4):870–8.
Johannsen M, O’Connor M, O’Toole MS, Jensen AB, Zachariae R. Mindfulness-based cognitive therapy and persistent pain in women treated for primary breast cancer. Clin J Pain. 2018;34(1):59–67.
Liu Z, Xu C, Xu Y, et al. Decreased regional homogeneity in insula and cerebellum: a resting-state fMRI study in patients with major depression and subjects at high risk for major depression. Psychiat Res. 2010;182(3):211–5.
Peng DC, Dai XJ, Gong HH, Li HJ, Nie X, Zhang W. Altered intrinsic regional brain activity in male patients with severe obstructive sleep apnea: a resting-state functional magnetic resonance imaging study. Neuropsych Dis Treat. 2014;10:1819–26.
Mioduszewski O, Hatchard T, Fang Z, et al. Breast cancer survivors living with chronic neuropathic pain show improved brain health following mindfulness-based stress reduction: a preliminary diffusion tensor imaging study. J Cancer Surviv. 2020;14(6):915–22.
Acknowledgements
We thank all participants for their involvement in the study. We also acknowledge and thank Chongqing Ninth People's Hospital, Beibei University for the Elderly, and Southwest University Hospital for helping with recruiting participants.
Funding
This study and the Rapid Service Fee were supported by grants from the China National Natural Sciences Foundation (31871141) to Todd Jackson in Chongqing, China; Army Medical University (cx2019js211) to Ying He in Chongqing, China; and Chongqing Xinqiao Hospital, Second Affiliated Hospital of Army Medical University (2022YQB100) to Shuanghong Chen in Chongqing, China.
Author information
Authors and Affiliations
Contributions
Todd Jackson and Shuanghong Chen contributed to the study conception and design. Material preparation and MBSR course delivery were performed by Shuanghong Chen and Xubin Gao. Study coordination was performed by Ting Shi. Data collection was performed by Xibo Zuo, Chengjin Hong, and Yaoyao Zhang. Data analysis was performed by Beibei You and Fenghua Li. Funding was secured from Todd Jackson, Ying He, and Shuanghong Chen. The first draft of the manuscript was written by Shuanghong Chen and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Shuanghong Chen, Xubin Gao, Ting Shi, Xibo Zuo, Chengjin Hong, Yaoyao Zhang, Beibei You, Fenghua Li, Todd Jackson, and Ying He declare that they have no conflicts of interest.
Ethical approval
The study received institutional review board approval from Southwest University in China (H21034). The study was conducted in accordance with the current version of Helsinki Declaration and following all other requirements of local laws of China. Written informed consent was obtained from all participants.
Supplementary Information
Below is the link to the Electronic Supplementary Material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chen, S., Gao, X., Shi, T. et al. Promising Subjective and Objective Benefits of Modified Mindfulness-Based Stress Reduction Training for Chinese Adults with Chronic Pain: A Pilot Randomized Control Study. Pain Ther 12, 1397–1414 (2023). https://doi.org/10.1007/s40122-023-00551-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00551-9