Abstract
Introduction
This study aimed to analyze the risk factors affecting the recurrence of cervical spondylotic radiculopathy after surgery, construct a nomogram predictive model, and validate the model’s predictive performance using a calibration plot.
Methods
In this study, 304 cervical spondylotic radiculopathy patients who underwent computed tomography (CT)-guided radiofrequency ablation (RFA) of cervical intervertebral discs or low-temperature plasma RFA for cervical radiculopathy were enrolled at the Pain Department of Jiaxing College Affiliated Hospital from January 2019 to March 2022. The patients were randomly divided into training (n = 213) and testing (n = 91) groups in a 7:3 ratio. Lasso regression analysis was used to screen for independent predictors of recurrence 1 year after surgery. A nomogram predictive model was established based on the selected factors using multiple logistic regression analysis.
Results
One year after surgery, 250 of the 304 cervical spondylotic radiculopathy patients did not have recurrences, while 54 had recurrences. Lasso regression combined with multiple logistic regression analysis revealed that duration, numbness, and the Numeric Rating Scale (NRS) were significant predictors of recurrence 1 year after surgery (P < 0.05). A nomogram predictive model was established using these variables. The area under the curve (AUC) of the nomogram predictive model for predicting recurrence in the training group was 0.918 [95% confidence interval (CI) 0.866–0.970], and the AUC in the testing group was 0.892 (95% CI 0.806–0.978). The Hosmer–Lemeshow goodness-of-fit test exhibited a good model fit (P > 0.05). Decision curve analysis (DCA) indicated that the nomogram predictive model had a higher net benefit for predicting the risk of postoperative recurrence in cervical radiculopathy patients when the threshold probability was between 0 and 0.603.
Conclusion
This study successfully developed and validated a high-precision nomogram prediction model (predictive variables include duration, numbness, and NRS) for predicting the risk of postoperative recurrence in cervical radiculopathy patients. The model can help improve the early identification of high-risk patients and screening for postoperative recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The study aimed to analyze the risk factors and develop a predictive model for the recurrence of cervical spondylotic radiculopathy after surgery. |
The study enrolled 304 patients who underwent computed tomography (CT)-guided radiofrequency ablation for cervical radiculopathy and divided them into training and testing groups. |
Duration, numbness, and the Numeric Rating Scale (NRS) were identified as significant predictors of recurrence 1 year after surgery. |
A nomogram predictive model based on these variables was developed and showed high accuracy in predicting recurrence in both the training and testing groups. |
Introduction
Cervical radiculopathy is a disabling disease that significantly impairs a person’s mental health, physical function, and social participation. Patients frequently experience significant pain, numbness, or weakness, among other symptoms [1, 2]. When conservative treatment fails, cervical radiculopathy requires surgical intervention. Numerous surgical treatments, such as anterior cervical discectomy and fusion, cervical disc replacement, and posterior cervical foraminotomy, are available, but these are being gradually replaced by less invasive methods, such as computed tomography (CT)-guided RFA of cervical intervertebral discs and low-temperature plasma RFA for cervical radiculopathy [3, 4]. Although minimally invasive RFA is an effective treatment for cervical radiculopathy, a risk of recurrence after surgery exists, and the causes and risk factors for recurrence remain unknown. Therefore, it is important to investigate the risk factors for the postoperative recurrence of cervical radiculopathy, construct predictive models, and improve the effectiveness and prognosis of postoperative treatment for patients. This study aimed to predict the risk of postoperative recurrence of cervical radiculopathy by reviewing the relevant information about cervical radiculopathy patients who have received minimally invasive radiofrequency (RF) treatment, selecting independent predictive factors, and constructing a predictive model. This study may help provide personalized treatment plans for cervical radiculopathy patients, improve their postoperative recovery, and provide new ideas and methods for analyzing cervical spondylosis.
Methods
Study Subjects
The cervical radiculopathy patients who received CT-guided cervical disc RF or plasma treatment were collected retrospectively from the Pain Department of Jiaxing University Affiliated Hospital from January 2019 to March 2022. This study was approved by the Ethics Committee of Jiaxing University Affiliated Hospital (2023LY277). This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All patients had received regular medication but had a poor response, so they voluntarily underwent procedural treatment and signed the procedural consent form. Inclusion criteria included a diagnosis of single-segment cervical radiculopathy [5] and procedural success. Exclusion criteria included incomplete data, an inability to contact them, and an unwillingness to cooperate with follow-up.
Procedural Methods
Patients were routinely instructed to fast for 6 h before surgery and to refrain from drinking. Upon admission to the CT operating room, nasal cannula oxygen was administered, venous access was established, and heart rate, blood pressure, and peripheral oxygen saturation were monitored. Patients lay supine on the CT table with a pillow placed under their shoulders to extend the neck at an angle of approximately 20°. After CT scanning to determine the cervical vertebra segment and design the optimal puncture path, the puncture point on the affected side of the neck was disinfected and covered with a surgical drape.
CT-guided RFA of cervical intervertebral discs (RF) [6]. After administering local anesthesia at the puncture point, a 22G radiofrequency puncture needle (Cosman TCN-10, USA) with a 10-mm working end was guided using CT to puncture the protruding intervertebral disc on the affected side. The impedance was measured at 250–500 Ω using a radiofrequency generator (Baylis Medical Company Inc., Toronto, Canada), and sensory and motor testing was performed. Sensory testing was conducted using a high-frequency current (50 Hz, 500 μs), while motor testing was conducted using a low-frequency current (2 Hz, 1000 μs). The needle tip was adjusted until the current reached 3 mA, but neither sensory nor motor responses were elicited to ensure that the radiofrequency ablation was carried out in a safe range away from nerves. The following parameters were set: a temperature of 95 °C and a duration of 300 s. Radiofrequency coagulation was performed. If pain or discomfort occurred during the procedure, the radiofrequency ablation was stopped immediately and the needle tip position was re-adjusted. After completion of the radiofrequency ablation, the patients were observed for 20 min and then returned to the ward if no adverse reactions occurred.
Low-temperature plasma RFA for cervical radiculopathy (plasma) [7]. The puncture process was similar to that of RF. A specially designed 18G puncture sleeve needle with a needle core (ZJFERT AN-T18G, China) was used to puncture the target intervertebral disc. Then, the needle core was replaced with an electrode and connected to a bipolar radiofrequency system (Unitech SD-2000, Beijing, China). An electric field was created to activate the electrolyte and generate a plasma field. The plasma field dissolved a small amount of tissue in the target area at a relatively low temperature (40–70 °C). After 4–5 s of ablation, the electrode was repositioned to another part of the nucleus pulposus based on the protrusion morphology. The total ablation time was approximately 5–10 min. After completing the procedure, the patients were observed for 20 min and returned to the ward if no adverse reactions occurred. All patients were required to stay in bed for 24 h after surgery and wear a cervical collar for 1 month.
Data Collection
The following data were collected using a Haite electronic medical record system 3.0: gender, age (years), body mass index [BMI = weight (kg)/(height (m) × height (m)], < 18.5 as underweight, 18.5–30 as normal, > 30 as overweight), disease duration, complication (including chronic diseases such as hypertension and diabetes that were still being treated), numbness (whether the affected arm had numbness), history (whether the patient had received treatment before, including minimally invasive surgery and nerve block), location (the responsible segment of the lesion, as determined by imaging and clinical manifestations), type (surgical type: RF or plasma), preoperative pain score [Numerical Rating Scale (NRS)], and other indicators. The NRS was collected via a telephone follow-up 1 year after surgery. The outcome indicator was recurrence: (preoperative NRS − postoperative NRS)/preoperative NRS < 50%.
Statistical Analysis
Statistical analysis was performed using R 4.1.3 software. The Kolmogorov–Smirnov test was used to determine whether continuous variables had a normal distribution. Normally distributed data were expressed as mean ± standard deviation and compared between groups using t tests. Non-normally distributed data were expressed as median (interquartile range) and compared using the Mann–Whitney U test. Categorical variables were evaluated using the chi-square test. After strict data filtering and preprocessing, eligible patients (n = 304) were randomly allocated to the training (n = 213) and the testing (n = 91) groups at a 7:3 ratio. The least absolute shrinkage and selection operator (Lasso) method was used to screen for independent predictors of recurrence 1 year after surgery in the training group as the outcome variable [8, 9]. On this basis, multiple logistic regression analysis was used to explore and establish a nomogram prediction model. The testing group data were used to validate the constructed prediction model. The area under the receiver operating characteristic (ROC) curve was used to evaluate the efficacy of the prediction model and to verify the prediction effect of the model, while the Hosmer–Lemeshow goodness-of-fit test was used to evaluate the degree of fit of the model [10]. Calibration curves were also plotted. Decision curve analysis (DCA) was used to predict the risk of recurrence 1 year after surgery in the cervical spondylotic radiculopathy patients [11]. A P value of < 0.05 was considered statistically significant.
Results
General Information
Among the 304 cervical spondylotic radiculopathy patients, 250 did not experience a recurrence, while 54 did within 1 year after surgery. Gender, age, BMI, complication, history, location, and type did not differ significantly between the non-recurrence and the recurrence groups (P > 0.05). However, duration, numbness, and NRS differed significantly between the two groups (P < 0.05; Table 1). The study randomly divided 304 patients into training (n = 213) and testing (n = 91) groups at a 7:3 ratio. The baseline characteristics did not differ significantly between the two groups (all P > 0.05; Table 2).
Risk Factors for Recurrence
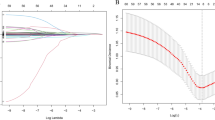
Lasso regression analysis was conducted in the training group using the recurrence of neural root cervical spondylosis in patients 1 year after surgery (coded as “0” for no recurrence and “1” for recurrence) as the dependent variable and gender (coded as “0” for female and “1” for male), age (years), BMI (coded as “0” for < 18.5, “1” for 18.5–30, and “2” for > 30), duration (coded as “0” for < 1 year and “1” for ≥ 1 year), complication (coded as “0” for no and “1” for yes), numbness (coded as “0” for no and “1” for yes), history (coded as “0” for no and “1” for yes), location (coded as “4” for C4/5, “5” for C5/6, and “6” for C6/7), type (coded as “0” for RF and “1” for plasma), and NRS (coded as “0” for < 7 and “1” for ≥ 7) as independent variables (Fig. 1). As the penalty coefficient lambda increased, the number of variables included in the model gradually decreased, and the optimal value of the model was determined to be λ + 1, where λ was the value at the minimum tenfold cross-validation error (1SE of the minimum lambda was 0.067) (Fig. 2). The predictive variables selected at this point were duration, numbness, and NRS. Then, multiple logistic regression analysis was conducted with these predictive variables. The results showed that duration, numbness, and NRS were the factors influencing the recurrence of neural root cervical spondylosis in patients 1 year after surgery (Table 3).
Texture feature selection in the Lasso model, showing the different superparameters (lambda values) corresponding to the diagnostic biases of the different models. The vertical dotted line on the left represents the minimum deviation of log(lambda) at the optimal lambda value, and the vertical dotted line on the right represents the optimal logarithmic value of lambda. The number at the top of the figure is the feature number
Nomogram Prediction Model Construction
We included the variables selected from the aforementioned multiple logistic regression analysis in the nomogram prediction model. The outcome indicator is whether patients with nerve-root-type cervical spondylosis may have a recurrence 1 year after surgery. We created the nomogram (Fig. 3) and used the ruler above each risk factor on the nomogram to obtain the individual score for that factor. We added the scores for all risk factors to obtain the total score that can be used to estimate the probability of pain recurrence in the corresponding patient 1 year after surgery. A higher total score implies a greater likelihood of recurrence of cervical radiculopathy in patients after 1 year of surgery.
Predictive Value for the Occurrence of Postoperative Recurrence in the Training and Testing Groups
A ROC curve was plotted to assess the predictive accuracy of the nomogram. The ROC curve of the nomogram had an area under the curve (AUC) of 0.918 (95% CI 0.866–0.970) for the training set. The predictive performance of the nomogram was validated further using an independent testing set. The AUC of the ROC curve was 0.892 (95% CI 0.806–0.978; Fig. 4), indicating that the predictive model had good discrimination ability in the training and testing populations.
Calibration Curves for Postoperative Recurrence of Cervical Radiculopathy in the Training and Testing Groups
In the training dataset, the calibration curve of the nomogram presented good agreement between the predicted and observed outcomes. The Hosmer–Lemeshow goodness-of-fit test revealed that the model was insignificant (P > 0.05), indicating good agreement between the model and observed data (Fig. 5). The validation based on the testing dataset also displayed good agreement between predicted and observed outcomes, and the Hosmer–Lemeshow goodness-of-fit test again demonstrated that the model is insignificant (P > 0.05), indicating good agreement between the model and observed data (Fig. 6).
DCA for Postoperative Recurrence in the Training and Validation Groups
Based on the nomogram predictive model, the variables selected were used to conduct DCA for 1-year-postoperative recurrence (Fig. 7). The results showed that when the threshold probability of the patient was 0–0.603, using the nomogram to predict the risk of recurrence in patients with cervical radiculopathy after surgery resulted in a higher net benefit. Therefore, a wide range of alternative threshold probabilities indicated that this model is a good evaluation tool.
Discussion
The present study aimed to analyze the risk factors associated with postoperative recurrence in cervical radiculopathy patients and to construct and validate a nomogram prediction model. We adopted a retrospective study design. We enrolled 304 cervical radiculopathy patients who underwent percutaneous cervical disc RFA or low-temperature plasma RFA (plasma) treatment in the Pain Department of the Affiliated Hospital of Jiaxing University from January 2019 to March 2022. The patients were randomly divided into training and testing groups at a ratio of 7:3. Lasso regression and multiple logistic regression analyses were performed to screen the independent predictive factors for postoperative recurrence at 1 year, while a nomogram prediction model was established. Finally, the prediction model’s discriminative ability, accuracy, and clinical utility were evaluated using the AUC of the ROC curve, calibration curve, and DCA, respectively. The results showed that duration, numbness, and NRS were independent predictive factors for postoperative recurrence in cervical radiculopathy patients. Patients with a disease duration of less than 1 year, no limb numbness, and a preoperative pain score of less than seven had a lower recurrence rate 1 year after surgery.
The longer the disease course, the longer the nerve compression by the intervertebral disc protrusion and the more severe the corresponding nerve damage. Biomarkers of glial cells, axonal damage, inflammation, and synaptic changes in cerebrospinal fluid are altered in patients with chronic cervical spondylosis, suggesting that these patients have axonal damage, astrocyte activation, and abnormal Aβ metabolism [12]. Although the human body has a certain self-healing tendency towards intervertebral disc protrusion, which may be related to the body’s immune system, not everyone can achieve self-healing through conservative treatment [13]. Frequently, patients with a disease course of more than 1 year could not obtain relief from the nerve compression caused by the intervertebral disc protrusion through conservative waiting, resulting in irreversible nerve damage [14].
Limb numbness as a clinical manifestation also proves that the cervical disc herniation compresses and damages the nerves, leading to a sensory deficit besides pain [15]. Numbness frequently occurs in severe nerve injuries [16]. Several studies discovered that cervical radiculopathy patients have distal nerve axonal hyperpolarization. This hyperpolarization pattern may be due to excessive Na+–K+ ATPase activation caused by proximal ischemia, or it may reflect re-myelination [17]. Distal sensory nerve axonal hyperpolarization suggests that nerve excitability testing may be more sensitive to clinical symptoms than nerve conduction testing in cases without no nerve conduction examination changes. Numbness is a unique clinical manifestation of nerve-root-type cervical spondylosis. Treatment may require additional methods besides RFA of the herniated disc, which cannot solve all the problems [18, 19].
Patients with high preoperative pain scores may experience psychological and physiological impacts [20]. Severe pain can cause central or peripheral sensitization, making the disease more complex and difficult to treat [21]. Psychological problems, such as anxiety and depression caused by severe pain, require multidisciplinary collaborative treatment [22]. Severe pain stimulation occurring in areas responsible for perceiving and integrating sensory information, regulating movement, and pain modulation can even change the brain’s functional connectivity [23].
This study’s clinical significance lies in establishing a highly accurate predictive model for postoperative recurrence in cervical radiculopathy. The model was developed based on three easily measurable variables: duration of symptoms, numbness, and Numeric Rating Scale score. The model was validated in an independent testing group, demonstrating excellent discriminative ability, accuracy, and clinical utility. This model's practical applicability is extensive. Clinicians can use it to identify high-risk patients for postoperative recurrence and then provide more aggressive treatment and close monitoring of those patients. This may lead to earlier detection and intervention, potentially improving patient outcomes and reducing healthcare costs.
However, the study’s limitations include its single-center design and lack of external validation. The use of pain scores as the sole outcome measure may be insufficient to predict the prognosis of cervical radiculopathy accurately. Future prospective, double-blind, randomized, controlled, and multi-center studies must be designed to validate the model.
To summarize, cervical radiculopathy patients with a disease duration of over 1 year, limb numbness, and severe preoperative pain are more likely to experience a recurrence within 1 year after surgery. Therefore, when selecting treatment plans, the patient's condition must be thoroughly considered, and personalized treatment plans must be carefully chosen.
Conclusion
This study explored the risk of postoperative recurrence in cervical radiculopathy patients. We identified key factors, such as duration, numbness, and NRS score, that affect postoperative recurrence in cervical radiculopathy patients by establishing and validating a predictive model. We successfully developed a high-precision nomogram prediction model, providing a tool for identifying and selecting high-risk patients early in clinical practice. This model has high predictive accuracy and clinical utility and is a promising clinical application prospect.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bono CM, Ghiselli G, Gilbert TJ, et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 2011;11:64–72.
Ng E, Johnston V, Wibault J, et al. Factors associated with work ability in patients undergoing surgery for cervical radiculopathy. Spine. 2015;40:1270–6.
Iyer S, Kim HJ. Cervical radiculopathy. Curr Rev Musculoskelet Med. 2016;9:272–80.
Wong JJ, Côté P, Quesnele JJ, et al. The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: a systematic review of the literature. Spine J. 2014;14:1781–9.
Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38:1–211.
Hu JQ, Zhang J, Ru B, et al. Computed tomography-guided radiofrequency ablation of cervical intervertebral discs for the treatment of refractory cervicogenic headache: a retrospective chart review. Headache. 2022;62:839–47.
Lan X, Wang Z, Huang Y, et al. Clinical and radiological comparisons of percutaneous low-power laser discectomy and low-temperature plasma radiofrequency ablation for cervical radiculopathy: a prospective, multicenter, cohort study. Front Surg. 2021;8: 779480.
Mueller-Using S, Feldt T, Sarfo FS, et al. Factors associated with performing tuberculosis screening of HIV-positive patients in Ghana: LASSO-based predictor selection in a large public health data set. BMC Public Health. 2016;16:563.
Kidd AC, McGettrick M, Tsim S, et al. Survival prediction in mesothelioma using a scalable Lasso regression model: instructions for use and initial performance using clinical predictors. BMJ Open Respir Res. 2018;5: e000240.
de Carvalho GMC, Leite TT, Libório AB. Prediction of 60-day case fatality in critically Ill patients receiving renal replacement therapy: external validation of a prediction model. Shock (Augusta, GA). 2018;50:156–61.
Fitzgerald M, Saville BR, Lewis RJ. Decision curve analysis. JAMA. 2015;313:409–10.
Tsitsopoulos PP, Holmström U, Blennow K, et al. Cerebrospinal fluid biomarkers of glial and axonal injury in cervical spondylotic myelopathy. J Neurosurg Spine. 2021;34:632–41.
Grodzinski B, Durham R, Mowforth O, et al. The effect of ageing on presentation, management and outcomes in degenerative cervical myelopathy: a systematic review. Age Ageing. 2021;50:705–15.
Borrella-Andrés S, Marqués-García I, Lucha-López MO, et al. Manual therapy as a management of cervical radiculopathy: a systematic review. Biomed Res Int. 2021;2021:9936981.
Li GS, Wang XX, Tan RB, et al. Ultrastructural destruction of neurovascular unit in experimental cervical spondylotic myelopathy. Front Neurosci. 2022;16:1031180.
Plener J, Csiernik B, To D, et al. Conservative management of cervical radiculopathy: a systematic review. Clin J Pain. 2023. https://doi.org/10.1097/AJP.0000000000001092.
Sung JY, Tani J, Hung KS, et al. Sensory axonal dysfunction in cervical radiculopathy. J Neurol Neurosurg Psychiatry. 2015;86:640–5.
Zhang YM, Han XJ, Wang YC, et al. Yunmen (LU 2) combined with neck-seven-acupoint acupuncture for arm numbness caused by cervical spondylotic radiculopathy: a case report. Medicine (Baltimore). 2021;100: e26151.
Jitin B. Cervical spondylosis and atypical symptoms. Neurol India. 2021;69:602–3.
Lee Y, Kim DH, Park J, et al. Stellate ganglion block versus cervical epidural steroid injection for cervical radiculopathy: a comparative-effectiveness study. Reg Anesth Pain Med. 2022;47:501–3.
Adam F, Jouet P, Sabaté JM, et al. The thermal grill illusion of pain in chronic pain patients: a clinical marker of central sensitization? Pain. 2022. https://doi.org/10.1097/j.pain.0000000000002749.
Moghaddamjou A, Wilson JRF, Martin AR, et al. Multidisciplinary approach to degenerative cervical myelopathy. Expert Rev Neurother. 2020;20:1037–46.
Wang C, Holly LT, Oughourlian T, et al. Detection of cerebral reorganization associated with degenerative cervical myelopathy using diffusion spectral imaging (DSI). J Clin Neurosci. 2021;86:164–73.
Acknowledgements
We thank the participants of the study.
Medical Writing/Editorial Assistance
The authors thank MedSci (Shanghai, China) for English editing. The funding for this assistance was provided by the Affiliated Hospital of Jiaxing University.
Funding
This study was supported by the National Natural Science Foundation of China (81901124), Natural Science Foundation of Zhejiang Province of China (LY20H090020), Science and Technology Project of Jiaxing City (2021AD30164), Key Discipline Established by Zhejiang Province and Jiaxing City Joint-Pain Medicine (2019-ss-ttyx), Key Discipline of Anesthesiology of Jiaxing City (2019-zc-06) and Jiaxing Key Laboratory of Neurology and Pain Medicine. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Conception/design: Keyue Xie; data acquisition: Zi Wang; data analysis: Keyue Xie; data interpretation: Zi Wang and Keyue Xie; drafting or revising: Zi Wang and Keyue Xie; final approval: Keyue Xie. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved by all authors.
Corresponding author
Ethics declarations
Conflict of Interest
Zi Wang and Keyue Xie declare that they have no competing interests.
Ethical Approval
This study was approved by the Ethics Committee of Jiaxing University Affiliated Hospital (2023LY277). This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xie, K., Wang, Z. A Predictive Model for the Risk of Recurrence of Cervical Spondylotic Radiculopathy After Surgery. Pain Ther 12, 1385–1396 (2023). https://doi.org/10.1007/s40122-023-00548-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00548-4