Abstract
Introduction
This analysis aimed to evaluate demographics, migraine-related disability, symptoms, diagnosis and healthcare consultation, work productivity, and treatment patterns according to headache frequency in adults with migraine in the OVERCOME (ObserVational survey of the Epidemiology, tReatment and Care Of MigrainE) (Spain) study.
Methods
Data were obtained from an observational, cross-sectional, web-based survey conducted between October 2020–February 2021 in Spain. Eligible participants were adult members of online survey panels living in Spain who were able to read and write Spanish and fulfilled the International Classification of Headache Disorders, third edition (ICHD-3) criteria for migraine or had a self-reported physician diagnosis.
Results
In total, 10,229 patients comprised the Spanish sample. Only 56.2% of respondents had a confirmed healthcare professional (HCP) diagnosis of migraine, despite almost all meeting modified ICHD-3 criteria. Pain severity, migraine-related disability, and interictal burden increased with increasing number of headache days per month. Migraine impacted on respondents’ work productivity, with increases in presenteeism, work productivity loss, and daily activity impairment at higher headache frequencies. Over the past year, 66.2% of all HCP visits were specifically due to migraine, most commonly with a general practitioner or pharmacist. A subgroup of 1277 patients (12.5% of the total survey population) met eligibility criteria for migraine preventive medications, of whom only 36.6% were currently taking a preventive.
Conclusions
Results of the OVERCOME (Spain) survey reveal the substantial burden of migraine, which is directly linked to headache frequency. However, most patients experiencing frequent headaches and eligible for migraine preventives are currently not taking them. Findings highlight the importance of addressing unmet needs for people with migraine in Spain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? | |
Migraine is a chronic and painful condition that is estimated to affect over 10% of Spanish adults; however, prior population-based surveys of migraine have been hampered by limitations. | |
The OVERCOME (Spain) study was intended to address gaps in current understanding and explore unmet needs among people with migraine in Spain. | |
What did the study ask?/What was the hypothesis of the study? | |
The study evaluated demographics, migraine-related disability, symptoms, diagnosis and healthcare consultation, work productivity and treatment patterns according to headache frequency in adults with migraine in Spain. | |
What was learned from the study? | |
The study concluded that migraine in Spain is associated with substantial disability which is directly linked to increasing headache frequency. | |
This study revealed that, despite the burden of migraine in Spain, the majority of patients experiencing frequent headaches and eligible for migraine preventives are not taking them. | |
These findings highlight the importance of addressing unmet needs for patients with migraine in Spain by improving awareness and increasing access to effective treatment options. |
Introduction
Migraine is a chronic and debilitating disease characterized by attacks of headache and other symptoms, which may evolve over time [1]. Both the frequency and the severity of migraine headaches contribute to the burden that this condition imposes on individuals and wider healthcare systems [2, 3].
The overall 1-year prevalence of migraine in Spain is estimated to be 12.6%, according to results of a nationwide, population-based survey published in 2011 [4]. This Spanish survey found that females were more affected by migraine than males (17.2 vs. 8%) and noted some geographic variability in the prevalence rates of migraine across the country [4]. These data are in line with a recent global migraine prevalence estimate of 14.0%, with 15.5% of females and 7.4% of males affected [5]. Other studies have also revealed the substantial impact of migraine in Spain and other countries, and the link between headache frequency and worsening disability [6, 7].
With novel preventive migraine medications now in the market such as the calcitonin gene-related peptide (CGRP) monoclonal antibodies (mAbs), and anticipated approval of new acute treatments, it is important to better understand the local epidemiology and burden of migraine, identify barriers to the initiation of preventive and acute therapies, and recognize how the introduction of new classes of migraine medication influences healthcare delivery and migraine care, as well as to understand perceptions/attitudes of people with migraine. However, previous population-based surveys on migraine have been hampered by limitations such as geographic location, population subset, and/or outdated results [7,8,9,10]. The ObserVational survey of the Epidemiology, tReatment and Care Of MigrainE (OVERCOME) (European Union, EU) study was designed to address these gaps in current understanding and explore the unmet needs that still exist in the migraine space.
OVERCOME (EU) was conducted in Germany and Spain and is part of an overarching study program that also includes the US and Japan [11, 12]. Adopting an Internet-based survey approach as in OVERCOME (EU) allowed for a large number of study participants, including people with self- or physician-diagnosed migraine, or both, and enabled data on satisfaction and behavior of people with migraine in real life to be collected and analyzed. Importantly, the study facilitated access to a broad population of people with migraine that was representative of all patients—including those who do not appear in clinical trials because they have not been diagnosed with migraine or who have not sought medical care from a healthcare professional (HCP).
This article presents survey data from the OVERCOME (EU) study for people with migraine living in Spain—the OVERCOME (Spain) cohort. The objective of the OVERCOME (Spain) analysis was to evaluate demographics, migraine-related disability, symptom patterns, diagnosis status and healthcare consultation, work productivity, and treatment patterns according to headache frequency in Spanish adults with migraine.
Methods
Study Design
OVERCOME (Spain) was a non-interventional, cross-sectional, population-based, online survey of adults, with and without migraine, conducted between October 2020 and February 2021. This article reports on data for people with migraine only.
Briefly, the survey consisted of three phases. In phase I, a sample population that was demographically representative of the Spanish population was created. Adults who had registered for existing opt-in online survey panels (Kantar Profiles [Lightspeed] global panel and its partners) (Kantar Profiles [Lightspeed]) were invited to participate in the health survey without prior knowledge of the specific health topic. Sample selection was based on pre-specified demographics (age and sex) to ensure representativeness of data, and was refined as quota targets were achieved. A “first come, first served” approach was adopted with categories closed when required quotas were reached. Specific inclusion criteria for participation were: aged ≥ 18 years; resident in Spain and able to read and write Spanish; and online survey panel member, with Internet access and the ability to provide electronic informed consent.
In phase II, respondents with migraine in the demographically representative population were identified. Respondents were asked a series of questions around health and comorbidities, including whether they had experienced at least one headache in the past 12 months not associated with head injury, illness, or hangover. These potentially eligible individuals were then assessed for migraine either by a self-reported physician diagnosis of migraine or by fulfilling the modified International Classification of Headache Disorders, third edition (ICHD-3) criteria based on self-reported symptoms [13].
Phase III involved the establishment of a migraine cohort. The planned sample size of the Spanish migraine cohort was a total of 10,000 participants to facilitate analysis of smaller subgroups and account for potential loss at follow-up surveys. Respondents included in the migraine cohort were required to answer all survey questions assessing the consultation, treatment, and impact of migraine.
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Ethical approval for the study was granted by the the hospital Universitario Marqués de Valdecilla (Spain). All survey respondents provided informed consent and all data were anonymized before analysis.
Survey Instrument and Measurements
The OVERCOME (Spain) survey instrument was approximately 30 min in length and consisted of nine main categories of questions. Full details of these questions have been previously reported [11, 12]. The key assessment and outcome measures evaluated in this analysis are outlined below.
The reported clinical features of migraine were: number of headache days per month (HDs/m); migraine symptoms; duration of most recent migraine/severe headache; and pain severity. For most frequently reported symptoms, values correspond to those respondents who answered with “less than half the time or more” for each symptom from a list provided, with the remainder of respondents having answered “never or rarely”. Pain severity was rated on a scale of 0–10, with 10 being highest.
Migraine burden was assessed in this study using several well-validated self-assessment measures: Migraine Disability Assessment (MIDAS); Work Productivity and Activity Impairment-Migraine (WPAI-M) scale; and Migraine Interictal Burden Scale-4 (MIBS-4).
MIDAS data are reported for the migraine cohort stratified by monthly HDs. MIDAS measures headache-related disability based on five disability questions on the number of missed days, in the past 3 months, due to headache in school or paid work, household work, and family, social, or leisure activities as well as the number of additional days with significant limitations to activity in the domains of employment and household work [14].
The Work Productivity and Activity Impairment (WPAI) questionnaire is a patient-reported instrument developed to measure the impact on work productivity and regular activities attributable to a specific health problem [15]; for this study, the questions were specific to migraine. Scores are calculated as impairment percentages, with higher numbers indicating greater impairment and less productivity, namely, worse outcomes. The following WPAI data are reported: WPAI-M scores; mean (standard deviation [SD]); Absenteeism (% work time missed); Presenteeism (% impairment at work); Work productivity loss (%); and total daily activity impairment (%).
MIBS-4 measures the burden related to headache between attacks [16, 17]. The self-administered instrument consists of four items that address disruption at work and school, diminished family and social life, and planning and emotional difficulties. This article reports distribution of MIBS-4 total score, percentage (no, mild, moderate, severe) by HD/m.
In this survey, diagnosis of migraine was based on the modified gold standard ICHD-3 diagnostic criteria for migraine [13]. Data on patients’ healthcare resource utilization, including frequency and type of HCP consultation, were also collected and reported. Finally, the OVERCOME (Spain) survey gathered data on respondents’ current and previous use of medications for migraine. As part of this data analysis, a specific subgroup of survey respondents was identified as eligible for migraine preventive medication. This subgroup was defined by a migraine diagnosis from an HCP, ≥ 4 HDs/m and MIDAS score ≥ 11. When describing patterns of medication use in the survey, the term “oral” preventive medications was used to refer to the following medications: propranolol, atenolol, metoprolol, topiramate, valproic acid, candesartan, flunarizine, amitriptyline, and venlafaxine.
Statistical Analysis
The migraine cohort and specific subgroups (based on different frequencies of monthly HDs) were analyzed using descriptive statistics. Continuous variables are reported as means with SDs, or medians and ranges, as appropriate. Categorical variables are summarized as frequencies and percentages. The software utilized for statistical analyses was SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Demographics and Baseline Characteristics
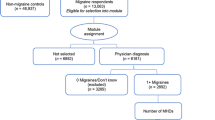
In total, 10,229 respondents fulfilled the modified ICHD-3 criteria for migraine or had a self-reported physician diagnosis, thereby comprising the OVERCOME (Spain) migraine cohort (see Fig. S1 in the electronic supplementary material for details). Table 1 outlines the demographics and baseline clinical characteristics of the migraine cohort overall and by HDs/m subgroup. The mean age of respondents was ~ 40 years and around 60% were female. In general, the proportion of female respondents increased with increasing headache frequency, as did the prevalence of anxiety and depression as comorbidities.
Clinical Features of Migraine
Most respondents (n = 7131, 69.7%) had experienced 0–3 HDs/m, followed by 4–7 HDs/m (n = 1971, 19.3%), 8–14 HDs/m (n = 689, 6.7%), and ≥ 15 HDs/m (n = 438, 4.3%) (see Fig. S1 in the electronic supplementary material for details). Accompanying symptoms of migraine such as head pain, phonophobia, and photophobia were reported by a substantial proportion of individuals (see Fig. S2 in the electronic supplementary material for details). The most frequent migraine symptom across all HDs/m groups was moderate or severe intensity pain (93.5%) (see Fig. S2 in the electronic supplementary material for details). Patients’ mean headache severity, rated on a scale from 1–10, increased with increasing number of HDs/m (see Fig. S3 in the electronic supplementary material for details).
The most reported durations for migraine attacks were 2–3 h (29.1%) or 4–7 h (25.4%). In nearly one-third of cases (31.4%), the duration of the most recent migraine/severe headache was 8 h or more, while only 14.3% of respondents said their attacks lasted less than 2 h.
Migraine Burden
Overall, 44% of the Spanish migraine cohort reported little or no disability (MIDAS grade I), 18.4% reported mild disability (MIDAS grade II), 18.2% reported moderate disability (MIDAS grade III), and 19.4% reported severe disability (MIDAS grade IV). Migraine-related disability increased markedly with increasing number of HDs/m (see Fig. S4 in the electronic supplementary material for details).
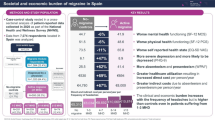
Of respondents in the OVERCOME (Spain) study, 7221 (70.6%) reported being in full-time or part-time employment. Figure 1 highlights the impact of migraine on patients’ work productivity over the past 7 days as measured by the WPAI score and stratified according to HDs/m. Rates of absenteeism (mean percentage of work time missed) and presenteeism (percentage of work time impaired) due to migraine were 16.3% and 41.9%, respectively in the overall population. Presenteeism, work productivity loss, and daily activity impairment (but not absenteeism) all increased with an increasing number of HDs/m.
Work productivity (WPAI-M score) stratified by monthly HDs. a7221 (70.6%) patients reported being in full-time or part-time employment. Work productivity components were measured using the WPAI questionnaire. HDs headache days, HDs/m headache days per month, WPAI Work Productivity and Activity Impairment, WPAI-M Work Productivity and Activity Impairment-Migraine
The overall interictal burden of migraine was considerable, with nearly half (46.8%) of the total Spanish migraine cohort reporting a severe burden (MIBS score of 5 +) (see Fig. S5 in the electronic supplementary material for details). Interictal burden varied according to headache frequency, but the rate of severe burden was highest (57.8%) in the group with ≥ 15 HDs/m.
Diagnosis of Migraine and HCP Consultation
Of all respondents, 75.4% reported having ever sought care for their headache or migraine. The proportion of patients who had ever asked for help was numerically higher in those experiencing the most frequent headaches (85.8% ≥ 15 HDs/m) and numerically lower in the less frequent headache categories (72.2% 0–3 HDs/m; 81.3% 4–7 HDs/m; 85.2% 8–14 HDs/m).
Most of the total for physician visits was comprised of medical appointments related specifically to migraine. Figure 2 illustrates the proportion of the migraine group who had sought care for migraine or severe headache on one or more occasion during the past 12 months. Two-thirds of physician visits (66.2%) over the past year were specifically due to migraine, with the highest rates of consultation for migraine in those experiencing the most frequent headaches.
Figure 3 shows the most common types of HCP consulted for migraine among the Spanish migraine cohort. Most patients had discussed their migraine with a primary care doctor/general practitioner (GP) (44.2%) or pharmacist (27.0%) and only a small percentage (7.1%) had ever consulted a headache specialist. Overall, approximately 30% of survey respondents had hesitated to seek medical attention for migraine. Of the reasons explaining this hesitancy, the most common was: “I did not think it was serious/painful enough,” which was reported by 9.1% of patients overall. Other reasons included: “Medications or other treatments that do not need a physician’s prescription worked well enough” (7.0%); “I wanted to try and take care of/deal with it on my own” (6.9%); and “I felt my migraine or headache would not be taken seriously” (6.6%) (see Table S1 in the electronic supplementary material for details).
Only 56.2% of survey respondents in the Spanish migraine cohort had received a diagnosis of migraine from an HCP; the remaining 43.8% of patients remained formally undiagnosed despite meeting ICHD-3 criteria for migraine (see Fig. S6 in the electronic supplementary material for details).
Current Use of Medications for Migraine
The most frequently used acute treatment was nonsteroidal anti-inflammatory drugs (NSAIDs) (85.3%), followed by paracetamol (63.0%), triptans (35.7%), a fixed combination of analgesics (20.9%), and ergotics (13.5%). Respondents’ use of acute and/or preventive medications for migraine, stratified according to their previous use of oral triptans, is shown in Fig. 4. Only 35.7% of the overall migraine cohort were currently taking oral triptans for acute use (Fig. 4). The percentage of patients using triptans was markedly higher in those who had used triptans in the past (54.7–84.9%) compared to those who had never used them before (19.4%) (Fig. 4). For the preventive treatment of migraine, 21.6% of respondents had ever used oral medications, which included beta blockers, topiramate, valproic acid, lisinopril, candesartan, flunarizine, amitriptyline, and venlafaxine (Fig. 4). The proportion of patients who had used oral preventives was highest in the cohorts that had previously tried two or more oral triptans. Use of specific antimigraine preventive medications was universally low: only 4.6% of the overall migraine cohort were currently using a CGRP mAb for the prevention of migraine and just 2.2% were receiving treatment with onabotulinumtoxin A (Botox) (Fig. 4). The use of Botox was expected to be low as it is indicated solely for chronic migraine. Use of CGRP mAbs or onabotulinumtoxin A as preventive medications was highest in the group who had previously received three or more triptans, 35.8% and 19.8%, respectively (Fig. 4).
In the migraine cohort, a subgroup of 1277 patients (12.5% of the total survey population) met eligibility criteria for migraine preventive medications—defined by a migraine diagnosis from an HCP, ≥ 4 HDs/m and MIDAS score ≥ 11 (Fig. 5). Figure 5 depicts the proportion of eligible patients in the migraine cohort currently taking migraine preventive medication. From the subgroup of 1277 survey respondents eligible for migraine preventive medication only 468 patients were currently taking a preventive. As expected, the proportion of patients meeting eligibility criteria for migraine preventive medications, as well as the percentage currently taking preventives, was greatest in the highest frequency headache subgroups. In the 8–14 HDs/m and ≥ 15 HDs/m categories, respectively, 46.2% (n = 318) and 49.5% (n = 271) of patients were eligible for preventives and 16.1% (n = 111) and 19.6% (n = 86) were currently taking them (Fig. 5).
Discussion
Results of the OVERCOME (Spain) survey show that the burden of migraine in Spain is substantial, even in individuals with the lowest headache frequency. Patients with migraine experienced considerable pain, migraine-related disability, interictal burden, and negative impacts on work productivity. The rate of moderate-to-severe disability and almost all other measures of migraine burden increased with increasing headache frequency.
Study results also highlight that migraine remains frequently underdiagnosed in Spain, independently of its severity. Over half of respondents only received a formal diagnosis of migraine from an HCP—despite almost all surveyed patients fulfilling the gold standard ICHD-3 diagnostic criteria for migraine. Underdiagnosis presents a major barrier that prevents patients receiving suitable medical care for their migraine, as well as accessing potentially beneficial medicines.
One possible reason contributing to underdiagnosis in Spain is patients’ reluctance to seek care. In this survey, one in three patients said they had hesitated to seek medical attention for their migraine, with lack of proper medical information and migraine-related stigma, as well as doubts about the possibility of a solution, among the most common reasons. These findings highlight the importance of providing people with migraine with adequate medical information to ensure accurate expectations about treatments and to help combat migraine-related stigma.
Despite problems with hesitancy in some patients, most respondents in the OVERCOME (Spain) study had sought care for their headache or migraine. Two-thirds of physician visits over the past 12 months were due directly to migraine. As would be expected, the highest rates of consultation for migraine were in those patients experiencing the most frequent headaches, with 80% in the ≥ 15 HDs/m subgroup having visited their HCP at least once over the past year. This finding could suggest potential shortcomings in the current management of migraine that is continuing to drive patients to their HCP with persistent symptoms. The most common settings for HCP consultations for migraine were in primary care and pharmacy, with only a small minority of migraine patients having seen a headache specialist.
For both acute and preventive treatment, the use of specific antimigraine drugs in Spain was low. Only one-third of patients were currently taking a triptan for acute treatment, despite these drugs being a guidelines-recommended first-line therapy [18]. Similarly, regarding preventive treatment, only 36% of all respondents who met eligibility criteria for migraine prevention were currently taking a preventive medication. This means that most migraine patients in Spain who are eligible for preventives are still not receiving them. The use of novel, targeted agents such as CGRP mAbs as preventive therapy for migraine was low. A possible reason for this may be that these mAbs are new therapies and therefore access to them can be limited. CGRP mAbs are reimbursed in Spain for patients with eight or more migraine days/month (high-frequency episodic migraine and in patients with chronic migraine) and three or more failures of previous treatments used at sufficient doses for at least 3 months, one of these treatments being botulinum toxin in the case of chronic migraine [19]. However, even in the broader preventive setting, only 21.6% of the Spanish migraine population was currently taking oral migraine preventives. This finding is in line with wider European data, which show that most people in Europe do not take traditional migraine preventive medications despite being eligible [20]. Collectively, these results highlight the need to improve both acute and preventive treatment of migraine in Spain to help reduce patients’ headache frequency and mitigate the disabling impact of this condition. A consensus has recently been published on the definitions of triptan response and triptan failure that may help clinicians in determining the most appropriate acute migraine medication for individual patients [21].
Reducing headache frequency and severity also has the potential to lessen the broader impacts of migraine on patients’ daily lives, including quality of life, mental health, and the ability to work, study, and socialize [22, 23]. Accordingly, a recent study has called for improved consistency in the definitions of terms regarding migraine-related burden, impact, disability, and quality of life [22]. This should also help in the appropriate use of current quantifying instruments, along with the development of new outcome measures to inform health policy [22, 24].
As GPs and pharmacists appear to be the front line of migraine care provision in Spain, it is important to ensure these HCPs are kept up to date with the latest clinical data and information on new treatment options for people with migraine. This is particularly important in chronic migraine where there was a low percentage of preventive medication use, even though this is a group where 100% of patients should be on preventives.
Overall, the OVERCOME (Spain) study has provided important real-world evidence highlighting the considerable burden and impact of migraine in Spain and identifying potential barriers to care. Results are in line with findings from other OVERCOME cohorts in the US and Japan, which have also highlighted key areas of unmet need for people with migraine [11, 12]. In the US, only 16.8% of patients were currently taking a migraine preventive and similarly, in Japan, 89.8% of patients had never used preventive medication [11, 12]. At a national level, improvements in both the diagnosis and treatment of migraine in Spain may help to decrease migraine overall burden for patients. Despite the clear link that exists between headache frequency and disability, only a minority of those patients eligible for migraine preventives in Spain are currently receiving them. This discrepancy highlights the importance of improving awareness of, and access to, effective migraine preventive medications, which can help to reduce the number of disabling headache attacks patients experience each month.
Study Strengths and Limitations
Study strengths include the use of a general population-based assessment, not limited to specific clinical settings or niche migraine population. Migraine cases were identified robustly using recognized international criteria (ICHD-3) or via self-report of a confirmed medical diagnosis. A very high number of subjects were included in the study and participants did not know in advance that the questionnaire in this case was due to migraine.
Limitations of the study include the fact that survey questions were answered by respondents and hence were potentially subject to recall or selection bias.
Conclusions
Migraine imposes a substantial burden in Spain and migraine-related disability increases with the frequency of monthly attacks. Despite this, migraine in Spain remains underdiagnosed and undertreated. There is a clear need for improved awareness of migraine in Spain, including appropriate uptake of traditional treatments and up-to-date information for patients and clinicians on newly available therapies. This is particularly important as we enter a new era of targeted therapeutic options for migraine prevention.
References
Riesco N, García-Cabo C, Pascual J. Migraña. Med Clin. 2016;146(1):35–9. https://doi.org/10.1016/j.medcli.2015.07.003.
Raggi A, Giovannetti AM, Quintas R, D’Amico D, Cieza A, Sabariego C, et al. A systematic review of the psychosocial difficulties relevant to patients with migraine. J Headache Pain. 2012;13(8):595–606. https://doi.org/10.1007/s10194-012-0482-1.
Diener HC, Solbach K, Holle D, Gaul C. Integrated care for chronic migraine patients: epidemiology, burden, diagnosis and treatment options. Clin Med (Lond). 2015;15(4):344–50. https://doi.org/10.7861/clinmedicine.15-4-344.
Matias-Guiu J, Porta-Etessam J, Mateos V, Diaz-Insa S, Lopez-Gil A, Fernandez C, et al. One-year prevalence of migraine in Spain: a nationwide population-based survey. Cephalagia. 2011;31(4):463–70. https://doi.org/10.1177/0333102410382794.
Stovner LJ, Hagen K, Linde M, Steiner TJ. The global prevalence of headache: an update with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23(1):34. https://doi.org/10.1186/s10194-022-01402-2.
Doane MJ, Gupta S, Vo P, Laflamme AK, Fang J. Associations between headache-free days and patient-reported outcomes among migraine patients: a cross-sectional analysis of survey data in Europe. Pain Ther. 2019;8(2):203–16. https://doi.org/10.1007/s40122-019-0133-1.
Irimia P, Garrido-Cumbrera M, Santos-Lasaosa S, Brace O, Colomina I, Blanch C, et al. Estimating the savings associated with a migraine-free life: results from the Spanish Atlas. Eur J Neurol. 2020;27(12):2616–24. https://doi.org/10.1111/ene.14431.
Buse DC, Manack A, Fanning K, Serrano D, Reed ML, Turkel C, et al. Chronic migraine prevalence, disability, and sociodemographic factors: results from the American Migraine Prevalence and Prevention Study. Headache. 2012;52(10):1456–70. https://doi.org/10.1111/j.1526-4610.2012.02223.x.
Manack Adams A, Serrano D, Buse D, Reed ML, Marske V, Fanning K, et al. The impact of chronic migraine: the Chronic Migraine Epidemiology and Outcomes (CaMEO) study methods and baseline results. Cephalalgia. 2015;35(7):563–78. https://doi.org/10.1177/0333102414552532.
Andrée C, Stovner LJ, Steiner T, Barre J, Katsarava Z, Lainez JM, et al. The Eurolight project: the impact of primary headache disorders in Europe. Description of methods. J Headache Pain. 2011;12(5):541–9. https://doi.org/10.1007/s10194-011-0356-y.
Lipton R, Nicholson R, Reed M, Araujo A, Jaffe D, Faries D, et al. Diagnosis, consultation, treatment, and impact of migraine in the US: results of the OVERCOME (US) study. Headache. 2022;62:122–4. https://doi.org/10.1111/head.14259.
Matsumori Y, Ueda K, Komori M, Zagar A, Kim Y, Jaffe DH, et al. Burden of migraine in Japan: results of the ObserVational survey of the Epidemiology, tReatment, and Care Of MigrainE (OVERCOME [Japan]) study. Neurol Ther. 2022;11:205–22. https://doi.org/10.1007/s40120-021-00305-9.
Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalagia. 2018;38(1):1–211. https://doi.org/10.1177/0333102417738202
Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl 1):S20–8. https://doi.org/10.1212/WNL.56.suppl_1.S20.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–65. https://doi.org/10.2165/00019053-199304050-00006.
Buse DC, Rupnow MFT, Lipton RB. Assessing and managing all aspects of migraine: migraine attacks, migraine-related functional impairment, common comorbidities, and quality of life. Mayo Clin Proc. 2009;84(5):422–35. https://doi.org/10.4065/84.5.422.
Buse DC, Bigal MB, Rupnow M, Reed ML, Serrano D, Lipton R. Development and validation of the Migraine Interictal Burden Scale (MIBS): a self-administered instrument for measuring the burden of migraine between attacks. Neurology. 2007;68:A89.
Santos Lasaosa S, Pozo Rosich P (Eds.). Manual de Práctica Clínica en Cefaleas. Recomendaciones diagnóstico-terapéuticas de la Sociedad Española de Neurología 2020. Madrid: Sociedad Española de Neurología; 2020:1–476. Available at: https://www.sen.es/pdf/2020/ManualCefaleas2020.pdf. Accessed 30 March 2022.
Agencia Espanola de Medicamentos y Productos Sanitarios. Therapeutic positioning report of galcanezumab (Emgality) in migraine prophylaxis; 2022. Available at: Therapeutic Positioning Report of galcanezumab (Emgality®) in migraine prophylaxis - Spanish Agency for Medicines and Health Products (aemps.gob.es). Accessed 24th September 2022.
Pascual J, Panni T, Dell Agnello G, Novick D, Evers S. Traditional preventive medication and treatment satisfaction in migraine: results from the OVERCOME (EU) study. In: Poster presented at the 8th European Academy of Neurology (EAN) meeting. June 25–28, 2022 in Vienna, Austria.
Sacco S, Lampl C, Amin FM, Braschinsky M, Deligianni C, Uluduz D, et al. European Headache Federation (EHF) consensus on the definition of effective treatment of a migraine attack and of triptan failure. J Headache Pain. 2022;23(1):133. https://doi.org/10.1186/s10194-022-01502-z.
Steiner TJ, Terwindt G, Katsarava Z, Pozo-Rosich P, Gantenbein AR, Roche SL, et al. Migraine-attributed burden impact and disability and migraine-impacted quality of life: expert consensus on definitions from a Delphi process. Cephalalgia. 2022;42(13):1387–96. https://doi.org/10.1177/03331024221110102.
Bentivegna E, Onan D, Martelletti P. Unmet needs in preventive treatment of migraine. Neurol Ther. 2023;12(2):337–42. https://doi.org/10.1007/s40120-023-00438-z.
Steiner TJ, Linde M, Schnell-Inderst P. A universal outcome measure for headache treatments care-delivery systems and economic analysis. J Headache Pain. 2021;22(1):63. https://doi.org/10.1186/s10194-021-01269-9.
Acknowledgements
The authors would like to thank the participants of this study for their contributions.
Funding
This work was supported by Eli Lilly and Company. The Rapid Service Fee was funded by the sponsor.
Medical Writing, Editorial, and Other Assistance
We would like to thank Helen Boreham and Duncan Marriott (Rx Communications, Mold, UK) for medical writing assistance with the preparation of this manuscript, funded by Eli Lilly and Company.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Material preparation, data collection and analysis were performed by Mercedes Núñez, Tomaso Panni, and Antonio Ciudad. Julio Pascual and Silvia Diaz were involved in interpretation of the work and Diego Novick contributed to the study conception and design. The first draft of the manuscript was written by Helen Boreham (Rx Communications Ltd) and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Prior Presentation
Some of the data contained in this manuscript have been presented previously as poster presentations at the Spanish Society of Neurology (SEN) annual meeting in 2021 and 2022.
Disclosures
Mercedes Núñez, Tommaso Panni, Silvia Díaz-Cerezo, Diego Novick, and Antonio Ciudad are employees of Eli Lilly and Company. Julio Pascual Gomez has participated in Symposia and Advisory Boards of Allergan, Amgen-Novartis, Biohaven, Teva, and Lilly.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Ethical approval for the study was granted by the hospital Universitario Marqués de Valdecilla (Spain). All survey respondents provided informed consent and all data were anonymized before analysis.
Data Availability
The data sets generated during and/or analyzed during the current study are not publicly available due to the need for patient data protection.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pascual, J., Núñez, M., Panni, T. et al. Burden and Unmet Needs in Migraine Patients: Results from the OVERCOME (Spain) Study. Pain Ther 12, 1209–1220 (2023). https://doi.org/10.1007/s40122-023-00538-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00538-6