Abstract
Introduction
The COVID-19 pandemic resulted in major disruptions in all aspects of human life including a decline of medical services utilized during 2020. An analysis of the impact of COVID-19 pandemic showed an 18.7% reduction in utilization patterns of interventional techniques in managing chronic pain in the Medicare population from 2019 to 2020. However, specific changes in utilization patterns of facet joint interventions have not been studied. Thus, we sought to assess the utilization patterns including an update of facet joint interventions from 2018 to 2020, with analysis of the impact of COVID-19 pandemic in managing chronic spinal pain utilizing facet joint interventions in the fee-for-service Medicare population of the United States.
Methods
The present investigation was designed to assess utilization patterns and variables of facet joint interventions, in managing chronic spinal pain from 2010 to 2020 in the fee-for-service (FFS) Medicare population in the United States (US), and how the COVID-19 pandemic impacted these utilization patterns. Data for the analysis were obtained from the master database from the Centers for Medicare & Medicaid Services (CMS) physician/supplier procedure summary from 2000 to 2020.
Results
Results of this analysis showed significant impact of COVID-19 with overall decrease of 18.5% of all facet joint interventions per 100,000 Medicare population compared to 20.2 and 20.5% decrease for lumbar and cervical facet joint injections, 15 and 13.1% decrease per 100,000 Medicare population of lumbosacral and cervicothoracic facet joint neurolysis procedures. The results are significant in that comparative analysis from 2000 to 2010 and 2010 to 2019 showing an annual increase of 14.4 vs. 2.2%, illustrating a decelerating pattern. There were also significant growth patterns noted with decreases in facet joint injections and nerve blocks compared to facet joint neurolytic procedures.
Conclusions
This analysis shows a significant effect of COVID-19 producing an overall decrease in utilization of facet joint interventions relative to pre-COVID data. Further, the analysis demonstrates continued deceleration of utilization patterns of facet joint interventions compared to the periods of 2000–2010 and 2010–2019.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Facet joint interventions in managing spinal pain experienced explosive growth rates from 2000 to 2009, with a reversal of those growth patterns and in some settings a trend of decline after 2009–2018. |
The COVID-19 pandemic reduced utilization of lumbar/sacral facet joint interventions, showing a decrease of 16.7% from 2019 to 2020, in contrast to overall reduction of utilization of interventional techniques of 18.5% per 100,000 Medicare fee-for-service population. |
The study was undertaken to provide an update of pre-COVID utilization patterns through 2019 in the United States fee-for-service Medicare population, and to assess the impact of COVID-19 from 2019 to 2020. |
The results of this study demonstrated an overall rate of decrease of 18.5% for facet joint interventions. The decrease was more significant for lumbar/sacral facet joint injections compared to radiofrequency neurotomy procedures. |
Introduction
The COVID-19 pandemic resulted in major disruptions to the overall economy and to healthcare [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16]. The economic shutdowns, increased pandemic-related hospitalizations, increased disease surveillance, and social isolation contributed to major changes in healthcare. The situation resulted in a decline of services offered during 2020 and extending through and beyond 2021 [1,2,3,4,5,6,7,8,9,10]. In the United States, national healthcare expenditures increased to $4.1 trillion in 2020. Personal and public healthcare in the U.S. from 1996 to 2016 showed an increase of 53.5% from $86.7 billion in 2013, increasing to $134.5 billion in 2016, the highest outlay for back and neck pain [12, 13]. In addition to numerous changes brought by the COVID-19 pandemic, there have been multiple changes resulting in declining utilization and perceived curtailed access to medically necessary treatments, including interventional techniques [14,15,16,17,18,19,20,21,22,23].
Facet joint interventions are one of the commonly utilized interventional techniques for managing chronic spinal pain. However, with treatment modalities being increasingly scrutinized, facet joint interventions have been criticized for their over-utilization and lack of proven clinical and cost utility. Over the past two decades, multiple modalities in pain management have shown significant escalation in utilization, including opioids, leading to an opioid epidemic and escalating deaths [1,2,3,4,5,6].
A recent analysis of the impact of the COVID-19 pandemic showed an 18.7% reduction in utilization patterns of interventional techniques in managing chronic pain in the Medicare population from 2019 to 2020 [3]. This study also showed a decrease of facet joint interventions and sacroiliac joint blocks of 17.5%, epidural and adhesiolysis procedures of 19%, and disc procedures and other types of nerve blocks of 25.6% per 100,000 Medicare recipients.
The utilization patterns of facet joint interventions have been well studied with overall increases until 2009, but declining utilization since 2009 [14, 16, 21]. Analysis of the utilization of interventional techniques in the FFS population from 2000 to 2018 showed an annual increase of 0.2% with an overall increase of 7.4% from 2009 to 2018 for lumbar facet injections and neurolytics per 100,000 Medicare population from 2009 to 2018 [16, 21]. Similarly, cervical and thoracic facet joint interventions demonstrated increases from 2009 to 2018 at an annual rate of 0.5% compared to cervicothoracic facet joint neurolytic procedures of 8.7% per 100,000 Medicare recipients [16, 21]. These studies also showed a reversal of the ratio of lumbosacral facet joint injections compared with facet joint neurolytic procedures, decreasing from 6.7% in 2009 to 2.2% in 2018 [16, 21]. Similarly, the ratio of cervicothoracic facet joint injections compared with neurolytic procedures decreased from 8.85% in 2000 to 2.8% in 2018 [16, 21]. Overall, based on the available literature, radiofrequency procedures have increased relative to facet joint nerve blocks and intra-articular injections in the Medicare and commercially insured population [16, 21, 24]. There was an increase of 2.5% of lumbar facet joint injection procedures annually from 2007 to 2016, compared to radiofrequency neurotomy procedures from 35 to 53 per 100,000 enrollees in the commercially insured population [24].
Even though positive literature continues to emerge showing the clinical and cost-effectiveness of facet joint interventions, along with other interventional techniques, there are persisting impressions of the lack of clinical efficacy and cost-effectiveness. The positive evidence is presented in guidelines, systematic reviews, randomized controlled trials (RCTs), observational studies, diagnostic accuracy studies, and, finally, cost utility studies [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50]. The majority of the discordance regarding the effectiveness of interventional techniques appears to be due to lack of agreement between proponents and opponents of the methodological evaluation of the literature [24, 50].
Consequently, multiple attempts to control utilization patterns have been initiated, specifically following reports from the Office of Inspector General (OIG) on overutilization and increasing costs of facet joint interventions relative to epidural injections [50,51,52]. Multiple local coverage determinations (LCDs), as well as medical policies have been revised using stricter inclusion criteria with severe restrictions on performing therapeutic facet joint injections unless specific contraindications for radiofrequency neurotomy are documented [53,54,55,56,57,58,59,60,61].
The present investigation was undertaken as a retrospective cohort study of utilization of patterns of facet joint interventions including the impact of COVID-19 from 2019 to 2020, with an update of pre-COVID utilization patterns to 2019, from previous publications regarding the United States FFS Medicare population [16, 21].
Methods
The present retrospective cohort study of utilization patterns of facet joint interventions was undertaken using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria and similar methods have previously been utilized by our team [62]. The non-identifiable data utilized in this evaluation was obtained from the public use files (PUF), which is non-attributable and non-confidential, available through the Centers for Medicare and Medicaid Services (CMS) [63].
Ethics Compliance
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Study Design
This retrospective cohort study was designed to assess utilization patterns and variables for using multiple facet joint interventions in managing chronic spinal pain from 2000 to 2020. This study focused on the impact of the COVID-19 pandemic on utilization in the Medicare FFS population in the United States.
Objectives
The objectives of this assessment were the evaluation of the impact of the COVID-19 pandemic on utilization patterns of facet joint interventions from 2019 to 2020 in the FFS Medicare population.
Setting
The national database of specialty usage data files from CMS in the FFS Medicare population in the United States [63].
Participants
All the participants in the database included all FFS Medicare recipients from 2000 to 2020, whether they were on Medicare due to Social Security disability, Social Security insurance, or retirement.
Variables
Multiple variables were assessed in the utilization patterns of facet joint interventions in the Medicare population from 2019 to 2020 in order to evaluate the impact of the COVID-19 pandemic, including an analysis of the usage patterns from 2010 to 2019 and 2010 to 2020. Additionally, multiple characteristics of the Medicare population and the growth of that population were also studied.
Historically, facet joint interventions have been performed by physicians of various specialties, including interventional pain management (− 09 specialty code), pain medicine (− 72), anesthesiology (− 05), physical medicine and rehabilitation (− 25), neurology (− 13), radiology (− 30, − 94), and psychiatry (− 26). A multitude of other specialties also perform interventional procedures less frequently. Based on Medicare designations, orthopedic surgery (− 20), general surgery (− 17), and neurosurgery (− 14) are combined as a surgical group; diagnostic radiology (− 30), and interventional radiology (− 94) are combined as a radiological group. All other physicians constitute a separate group, and all other providers are considered as “other providers”.
The procedure codes for facet joint interventions in effect during 2000–2020 were as follows:
-
Facet joint interventions (CPT 64451 (from 2020), 64470, 64472, 64475, 64476, 64490, 64491-new, 64492-new, 64493-new, 64494-new, 64495-new, 64622, 64623, 64625 (from 2020), 64626, 64627, 64633-new, 64634-new, 64635-new, 64636-new
-
Multiple interventional procedures CPT codes as utilized in comparative evaluations have been described in a recent manuscript [3].
The data were also assessed based on the place of service—facility (ambulatory surgery center or hospital outpatient department) or non-facility (office).
The data were compared based on Medicare Administrative Contractor jurisdictions. A Medicare Administrative Contractor or MAC is a private health insurer who has been granted certain geographical jurisdictions in the US by CMS to process Medicare Part A and Part B medical claims or durable medical equipment claims for Medicare fee-for-service beneficiaries, based on the Medicare Prescription Drug Improvement and Modernization Act (MMA) of 2003.
Data Sources
All the analyzed data were obtained from the CMS Physician/Supplier Procedure Summary Master Data from 2000 to 2020 [63]. These data included all FFS Medicare participants receiving interventional techniques irrespective of the type of disability.
Measures
The CMS 100% dataset consists of procedure codes (primary procedure, add-on, and bilateral), specialty codes, place of service, total services, and denied services. The usage pattern analysis included all allowed services configured by taking services submitted minus services denied, any services with zero payments, and those with a service code of 8 or F. Allowed services were assessed for each procedure. Rates were calculated based on Medicare beneficiaries for the corresponding year and are reported as procedures per 100,000 Medicare beneficiaries.
Bias
The data was purchased from CMS by the American Society of Interventional Pain Physicians (ASIPP). The study was conducted using the internal resources of the primary author’s practice without external funding or grants, either from industry or elsewhere.
Study Size
The study size is large with the inclusion of all patients under Medicare FFS undergoing facet joint interventions in all settings for all regions in the US for chronic spinal pain from 2000 to 2020.
Data Compilation
The data were compiled using Microsoft Access 2020 and Microsoft Excel 2020 (Microsoft Corporation, Redmond, WA, USA).
Funding
There was no external funding in the preparation of this manuscript.
Results
Participants
Participants in this assessment included all FFS Medicare recipients from 2000, and 2010–2020.
Descriptive Data of Population Characteristics
Table 1 shows various characteristics of Medicare beneficiaries and facet joint interventions from 2000–2010 and 2010–2019, and with special emphasis on 2019 to 2020. From 2000 to 2010, the overall US population increased 9.4% with those older than 65 years of age increasing by 14.8%. The proportion of the elderly population in the US constituted 12.4% in 2000, which increased to 13% in 2010 and 16.9% in 2020. Medicare beneficiaries also showed similar changes during 2010 to 2020, with the number of Medicare beneficiaries increasing 33% in contrast to a change in the total population of 7%, and the population above 65 years of age increasing to 39%. The ratio of Medicare beneficiaries was 14% in 2000, which increased to 18.9% in 2020 with an increase of 24% from 2010 to 2020.
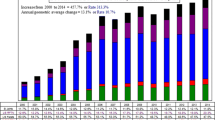
Facet joint interventions from 2000 to 2010 showed a progressive increase in annual services of 16.3% with an average annual change per 100,000 Medicare recipients of 14.4%. However, from 2010 to 2019, there was a deceleration in growth with services increasing at an annual rate of only 5.3%, whereas the average annual change per 100,000 Medicare recipients increased by only 2.2%. From 2019 to 2020, facet joint interventions services decreased 16.6%, with the average annual change per 100,000 Medicare recipients decreasing by 18.5%. Utilizing the number of episodes or patient encounters per region, changes were similar. However, significant negative effects were seen from 2019 to 2020 with services decreasing to 3600 from 4416 per 100,000 Medicare recipients and episodes decreasing from 1774 in 2019 to 1432 in 2020.
Figure 1 shows changes in the Medicare population and utilization of facet joint procedures in Medicare beneficiaries, as well as the rate of facet joint procedures per 100,000 beneficiaries. It also shows the change in the rate of facet joint episodes.
Analysis of the annual growth the utilization rate of facet joint services in the Medicare beneficiaries, and the rate of episodes per 100,000 Medicare beneficiaries (data presented in Table 1)
Utilization Characteristics
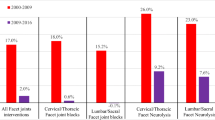
Table 2 shows the frequency of utilization of facet joint interventional services, which also includes add-on codes in the FFS Medicare population from 2000 to 2020. This table shows data of facet joint nerve blocks and radiofrequency neurotomy, both in the cervical/thoracic spine and the lumbar/sacral spine. From 2000 to 2010, services increased 17.4% for cervical facet joint nerve blocks at a rate of 15.5% annually compared to lumbar facet joint nerve blocks, which increased 15.7% at an annual rate of 13.8%. During the same period, radiofrequency neurolytic procedures increased in cervical spine total services by 25.6% at an annual rate of 23.5%, compared to those in the lumbar spine of 21.7 and 19.6%. From 2000 to 2010, all cervical facet joint interventions increased by 18.8%, services per year at an average annual rate of 16.8%, whereas all lumbar facet joint interventions increased by 15% at an average annual rate of 13.8%. There was an increase in all facet joint interventions by 16.3% at an annual rate of 14.4%. From 2010 to 2019, there were substantial changes with an increase in cervical facet joint nerve blocks of 4.9% at an average annual rate of 1.8%, compared to lumbar facet joint nerve blocks with an increase of 3.7% services at an average annual 0.7% rate of change. In contrast, during the same period from 2010 to 2019, cervical facet neurolysis procedures increased 9.7% at an average annual rate of 6.5%, and lumbar facet neurolysis procedures increased 7.8% at an average annual rate of 4.7%. All cervical facet joint interventions increased 6.1% at an average annual rate of 3%, and lumbar facet joint interventions increased 5% and 2%. There was an overall increase of all facet interventions by 5.3%, at an average rate of 2.2% per annum. There was a complete reversal from 2019 to 2020 with cervical facet joint nerve blocks decreasing 18.7% at an average annual rate of decrease of 20.5% compared to lumbar facet joint nerve blocks which decreased 15% at an average annual rate of 16.7%. Radiofrequency neurotomy procedures in the cervical spine decreased 11.1% at an average annual rate of 13.1% compared to the decreases in lumbar facet joint radiofrequency neurotomies of 15% at an average annual rate of 16.7%, with an overall decrease of all services by 16.6% at an average annual rate of 18.5%.
Figure 2 shows the same data in a graphic presentation.
Annual change in frequency of utilization of facet joint interventional services from 2000 to 2020 per 100,000 Medicare recipients. Data derived from Table 2
Table 3 shows the frequency of facet joint interventional episodes utilizing primary codes only without add-on codes. While the total number of episodes compared to services was lower, the rate of change showed similar patterns with increases similar to those presented above with slightly different percentages.
Figure 3 shows the data in a graphic display.
The data also show the number of procedures per episode was 2.6 in 2000 and 2010, with 2.5 procedures per episode in 2019 and 2020.
As shown in Tables 2 and 3, the declines were steeper for lumbar facet joint interventions compared to cervical facet joint interventions. The comparison in decline of services is also based on the number of services provided. Lumbar facet joint services were 777 in the year 2000 per 100,000 Medicare beneficiaries, which increased to 3365 in 2019 and decreased to 2741 in 2020 compared to cervical total rate of services of 69 vs. 777 in 2000 and 414 vs. 3365 in 2019 and 2741 vs. 338 in 2020. Thus, for each cervical procedure, over 8.5 lumbar procedures are performed. Similarly, cervical facet joint episodes also show similar ratios with 22 in 2000 compared to 294 for lumbar facet joint interventions, changing to 322 for cervical facet joint episodes compared to 1360 for lumbar facet joint episodes in 2019, whereas in 2020, the numbers were 280 vs. 1094 for cervical and lumbar, respectively, with a ratio of 3.9 episodes of lumbar interventions compared to one intervention of cervical episode.
Specialty Characteristics
Table 4 and Fig. 4 show the frequency of utilization of facet joint interventions on specialty designation. Interventional pain management specialties gradually increased their share from 71.1% in 2000 to over 94% in 2018, continuing through 2020.
Site of Service Characteristics
Facet joint interventions are performed in multiple settings including hospital outpatient departments, ambulatory surgical centers, and in physician offices with resultant implications for payment. There has been a significant shift over the years in the performance of interventional techniques based on the location of the procedures performed, as shown in Table 5.
Discussion
The present analysis of utilization patterns of facet joint interventions in managing spinal pain through 2020 provides an update from previous publications up to 2018 [16, 18], and assesses the impact of the COVID-19 pandemic in the Medicare FFS population. Overall results showed a continued increase, albeit at a slower rate, of facet joint interventional services of 5.3% at an average annual rate of 2.2% from 2010 to 2019, compared to the data from 2000 to 2010, which demonstrated a significant progressive increase in annual services of 16.3% with an average annual change per 100,000 Medicare recipients of 14.4%. The reduction in growth and decline of some procedures with an increase of others has been observed from 2010 onwards as in previous evaluations [16]. In addition, from 2000 to 2010, lumbar facet joint injections sessions or episodes grew by 14% at an average annual rate of 12.1%, but declined from 2010 to 2019 to a growth rate of 3.7% with an average annual rate of 0.7%. From 2000 to 2010, cervical/thoracic facet joint injection episodes increased by 17.4% at an average annual rate of 15.5%. Although those procedures increased during 2010 to 2019, they did so at a slower pace of 4.9% at an average annual rate of 1.8%. Cervical/thoracic facet neurolysis procedures grew during 2000–2010 by 25.6% at an annual rate of 23.5%. Those procedures had a slower increase during 2010 to 2019 of 9.7% at an average annual rate of 6.5%.
The greatest decline in growth rates during 2010 to 2019 occurred with lumbar/sacral facet joint injections, decreasing to 3.7% at an average annual rate of 0.7%. Comparatively, growth in lumbar/sacral facet neurolysis declined to 7.8% at an average annual rate of 4.7%, while cervical/thoracic neurolysis declined to 9.7% with an average annual rate of 6.5%.
One of the important findings of this analysis is the substantial drop in all services due to the COVID-19 pandemic that led to facility closures and lack of access to interventions. Comparing data from 2019 to 2020 for all cervical/thoracic and lumbar/sacral interventions there was a pronounced absolute decline of 16.6% in services at an average annual rate of − 18.5%. The declines were based on only 9 months of data in 2020; had the entire data from 2020 been available, the declines would have likely been more severe. Another important finding was the significant isolated decline in lumbar/sacral facet joint injections from 2010 to 2019, and an even greater drop in both services and rate during 2019–2020 of − 18.7% and − 20.6%, respectively. In addition, the data show that the 2.2% growth of facet joint interventions was less than the 3% growth of the Medicare beneficiary population from 2010 to 2019. There was also a decrease in episodes from 2019 to 2020 of 19.3% compared to the Medicare population growth of 2.3%, which was less than the prior years because of the significant number of COVID-19 deaths.
Analysis of various expenditures in 2020 shows both Medicare and Medicaid expenditures for physicians and clinical services slowed in 2020 [11]. Even then, Medicare spending increased 0.5%, which is down from the 8.9% increase in 2019, with the deceleration driven by a decline in all interventional techniques from 2019 to 2020. In particular, there was a decrease in epidural interventions and percutaneous adhesiolysis procedures when compared to earlier years [3, 17, 19, 20, 22].
There was a reversal of growth and decline of facet joint interventions from 2010 to 2019, These declines after 2010 may be attributed to multiple health care regulations initiated by the Affordable Care Act (ACA) [64,65,66,67,68,69,70], enactment of multiple LCDs [53,54,55,56,57,58], advocacy in the favor of radiofrequency neurotomy procedures [71], and reduced reimbursement rates [66, 72, 73]. In addition, disagreements as to the lack of indications and medical necessity may also have significant influence on reduced services, which extends beyond the Medicare FFS population to managed care organizations and includes those of Medicaid, all of Medicare, and services provided by commercial payers.
Overall decline in utilization patterns is often described as a positive sign; however, this can also imply impaired access. Further, this may also indicate denial of procedures which do not meet controversial criteria and “evidence” in the diagnosis and treatment of facet joint pain [43, 47, 74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90]. The focus should be to develop evidence-based data founded on pragmatic trials with real-world evidence [83, 84].
Similar to any epidemiological or analytic study, this analysis incorporates some limitations including lack of availability of data from approximately 40% of the participants enrolled in the Medicare Advantage Plans. Another limitation is the lack of monthly data for 2020, which might have demonstrated greater declines in the utilization of facet joint interventions.
Conclusions
No one can fully understand the extent of the detrimental effects of COVID-19 on patient care. The COVID-19 pandemic significantly impacted the utilization patterns of facet joint interventions producing an overall decline of 18.5%. Facet joint interventions grew at a slow rate from 2010 to 2019 with an overall annual increase of only 2.2% per 100,000 Medicare recipients. The decreasing number of facet joint interventions and other interventional procedures in conjunction with the reduced number of prescriptions and dosages of opioids is most certainly creating access issues for chronic pain patients [4]. A change in the regulatory and practice atmosphere is required to improve access to care for patients with chronic spinal pain.
References
Jha S, Shah S, Calderon MD, Soin A, Manchikanti L. The effect of COVID-19 on interventional pain management practices: a physician burnout survey. Pain Physician. 2020;23(4S):S271–82 (PMID: 32942787).
Manchikanti L, Pampati V, Jha SS, et al. The impact of COVID-19 on interventional pain management practices is significant and long-lasting: an interventional pain management physician survey. Pain Physician. 2022;25(2):131–44 (PMID: 35322967).
Manchikanti L, Pampati V, Sanapati MR, et al. COVID-19 pandemic reduced utilization of interventional techniques 18.7% in Managing chronic pain in the Medicare population in 2020: Analysis of utilization data from 2000 to 2020. Pain Physician. 2022;25(3):223–38 (PMID: 35652763).
Manchikanti L, Singh VM, Staats PS, et al. Fourth wave of opioid (illicit drug) overdose deaths and diminishing access to prescription opioids and interventional techniques: cause and effect. Pain Physician. 2022;25(2):97–124 (PMID: 35322965).
Manchikanti L, Vanaparthy R, Atluri S, Sachdeva H, Kaye AD, Hirsch JA. COVID-19 and the opioid epidemic: two public health emergencies that intersect with chronic pain. Pain Ther. 2021;10(1):269–86. https://doi.org/10.1007/s40122-021-00243-2. (Epub 2021 Mar 14. PMID: 33718982; PMCID: PMC7955940).
Gharaei H, Diwan S. COVID-19 pandemic: Implications on interventional pain practice-a narrative review. Pain Physician. 2020;23(4S):S311–8 (PMID: 32942791).
Shah S, Diwan S, Soin A, et al. Evidence-based risk mitigation and stratification during COVID-19 for return to interventional pain practice: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician. 2020;23(4S):S161–82 (PMID: 32942784).
Gharibo C, Sharma A, Soin A, et al. Triaging interventional pain procedures during COVID-19 or related elective surgery restrictions: Evidence-informed guidance from the American Society of Interventional Pain Physicians (ASIPP). Pain Physician. 2020;23(4S):S183-204 (PMID: 32942785).
Puntillo F, Giglio M, Brienza N, et al. Impact of COVID-19 pandemic on chronic pain management: looking for the best way to deliver care. Best Pract Res Clin Anaesthesiol. 2020;34(3):529–37. https://doi.org/10.1016/j.bpa.2020.07.001. (Epub 2020 Jul 17. PMID: 33004164; PMCID: PMC7366114).
Eccleston C, Blyth FM, Dear BF, et al. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain. 2020;161(5):889–93. https://doi.org/10.1097/j.pain.0000000000001885. (PMID:32251203; PMCID:PMC7172975).
Hartman M, Martin AB, Washington B, Catlin A, The National Health Expenditure Accounts Team. National health care spending in 2020: Growth driven by federal spending in response to the COVID-19 pandemic. Health Aff (Millwood). 2022;41(1):13–25. https://doi.org/10.1377/hlthaff.2021.01763. (Epub 2021 Dec 15. PMID: 34910596).
Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996–2013. JAMA. 2016;316(24):2627–46. https://doi.org/10.1001/jama.2016.16885. (PMID: 28027366; PMCID: PMC5551483).
Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863–84. https://doi.org/10.1001/jama.2020.0734. (PMID: 32125402; PMCID: PMC7054840).
Manchikanti L, Sanapati MR, Pampati V, Boswell MV, Kaye AD, Hirsch JA. Update on reversal and decline of growth of utilization of interventional techniques in managing chronic pain in the Medicare population from 2000 to 2018. Pain Physician. 2019;22(6):521–36 (PMID: 31775397).
Manchikanti L, Sanapati MR, Soin A, et al. An updated analysis of utilization of epidural procedures in managing chronic pain in the Medicare population from 2000 to 2018. Pain Physician. 2020;12(2):111–26 (PMID: 32214288).
Manchikanti L, Sanapati MR, Pampati V, et al. Update of utilization patterns of facet joint interventions in managing spinal pain from 2000 to 2018 in the US fee-for-service Medicare population. Pain Physician. 2020;23(2):E133–49 (PMID: 32214289).
Manchikanti L, Manchikanti MV, Vanaparthy R, Kosanovic R, Pampati V. Utilization patterns of sacroiliac joint injections from 2000 to 2018 in fee-for-service Medicare population. Pain Physician. 2020;23(5):439–50 (PMID: 32967386).
Manchikanti L, Simopoulos TT, Pampati V, et al. Impact of COVID-19 pandemic and updated utilization patterns of sacroiliac joint injections from 2000 to 2020 in the fee-for-service (FFS) Medicare population. Pain Physician. 2022;25(3):239–50 (PMID: 35652764).
Manchikanti L, Kosanovic R, Pampati V, Kaye AD. Declining utilization patterns of percutaneous adhesiolysis procedures in the fee-for-service (FFS) Medicare population. Pain Physician. 2021;24(1):17–29 (PMID: 33400425).
Manchikanti L, Pampati V, Soin A, Sanapati MR, Kaye AD, Hirsch JA. Declining utilization and inflation-adjusted expenditures for epidural procedures in chronic spinal pain in the Medicare population. Pain Physician. 2021;24(1):1–15 (PMID: 33400424).
Manchikanti L, Pampati V, Soin A, et al. Trends of expenditures and utilization of facet joint interventions in fee-for-service (FFS) Medicare population from 2009–2018. Pain Physician. 2020;23(3S):S129–47 (PMID: 32503360).
Manchikanti L, Senapathi SHV, Milburn JM, et al. Utilization and expenditures of vertebral augmentation continue to decline: an analysis in fee-for-service (FFS) recipients from 2009 to 2018. Pain Physician. 2021;24(6):401–15 (PMID: 34554681).
Manchikanti L, Pampati V, Vangala BP, et al. Spinal cord stimulation trends of utilization and expenditures in fee-for-service (FFS) Medicare population from 2009 to 2018. Pain Physician. 2021;24(5):293–308 (PMID: 34323431).
Starr JB, Gold L, McCormick Z, Suri P, Friedly J. Trends in lumbar radiofrequency ablation utilization from 2007 to 2016. Spine J. 2019;19(6):1019–28. https://doi.org/10.1016/j.spinee.2019.01.001. (Epub 2019 Jan 10. PMID: 30639589; PMCID: PMC6534485).
Cho JH, Lee JH, Song KS, et al. Treatment outcomes for patients with failed back surgery. Pain Physician. 2017;20(1):E29-43 (PMID: 28072795).
Manchikanti L, Knezevic E, Knezevic NN, et al. Epidural injections for lumbar radiculopathy or sciatica: a comparative systematic review and meta-analysis of Cochrane review. Pain Physician. 2021;24(5):E539–54 (PMID: 34323441).
Manchikanti L, Kosanovic R, Vanaparthy R, et al. Steroid distancing in interventional pain management during COVID-19 and beyond: Safe, effective and practical approach. Pain Physician. 2020;23(4S):S319–52 (PMID: 32942792).
Manchikanti L, Soin A, Boswell MV, Kaye AD, Sanapati M, Hirsch JA. Effectiveness of percutaneous adhesiolysis in post lumbar surgery syndrome: a systematic analysis of findings of systematic reviews. Pain Physician. 2019;22(4):307–22 (PMID: 31337160).
Manchikanti L, Knezevic NN, Sanapati MR, Boswell MV, Kaye AD, Hirsch JA. Effectiveness of percutaneous adhesiolysis in managing chronic central lumbar spinal stenosis: a systematic review and meta-analysis. Pain Physician. 2019;22(6):E523–50 (PMID: 31775400).
Manchikanti L, Knezevic NN, Sanapati SP, Sanapati MR, Kaye AD, Hirsch JA. Is percutaneous adhesiolysis effective in managing chronic low back and lower extremity pain in post-surgery syndrome: a systematic review and meta-analysis. Curr Pain Headache Rep. 2020;24(6):30. https://doi.org/10.1007/s11916-020-00862-y. (PMID: 32468418).
Knezevic N, Manchikanti L, Urits I, et al. Lack of superiority of epidural injections with lidocaine with steroids compared to without steroids in spinal pain: a systematic review and meta-analysis. Pain Physician. 2020;23(4S):S239–70 (PMID: 32942786).
Janapala RN, Manchikanti L, Sanapati MR, et al. Efficacy of radiofrequency neurotomy in chronic low back pain: a systematic review and meta-analysis. J Pain Res. 2021;14:2859–91. https://doi.org/10.2147/JPR.S323362. (PMID: 34531682; PMCID: PMC8439627).
Engel A, King W, Schneider BJ, Duszynski B, Bogduk N. The effectiveness of cervical medial branch thermal radiofrequency neurotomy stratified by selection criteria: a systematic review of the literature. Pain Med. 2020;21(11):2726–37. https://doi.org/10.1093/pm/pnaa219. (PMID: 32935126).
Manchikanti L, Pampati V, Sanapati MR, Hirsch JA. Outcomes of cervical therapeutic medial branch blocks and radiofrequency neurotomy: clinical outcomes and cost utility are equivalent. Pain Physician. 2022;25(1):35–47 (PMID: 35051143).
Manchikanti L, Kosanovic R, Pampati V, et al. Equivalent outcomes of lumbar therapeutic facet joint nerve blocks and radiofrequency neurotomy: Comparative evaluation of clinical outcomes and cost utility. Pain Physician. 2022;25(2):179–92 (PMID: 35322977).
Hambraeus J, Pulkki-Brannstrom AM, Lindholm L. Cost-effectiveness of radiofrequency denervation for zygapophyseal joint pain. Pain Physician. 2021;24:E1205–18 (PMID: 34793647).
Manchikanti L, Kaye AD, Soin A, et al. Comprehensive evidence-based guidelines for facet joint interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2020;23(3S):S1-127 (PMID: 32503359).
Manchikanti L, Knezevic NN, Navani A, et al. Epidural interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) comprehensive evidence-based guidelines. Pain Physician. 2021;24(S1):S27-208 (PMID: 33492918).
Manchikanti L, Kosanovic R, Cash KA, et al. Assessment of prevalence of cervical facet joint pain with diagnostic cervical medial branch blocks: analysis based on chronic pain model. Pain Physician. 2020;23(6):531–40 (PMID: 33185369).
Manchikanti L, Kosanovic R, Pampati V, et al. Low back pain and diagnostic lumbar facet joint nerve blocks: assessment of prevalence, false-positive rates, and a philosophical paradigm shift from an acute to a chronic pain model. Pain Physician. 2020;23(5):519–30 (PMID: 32967394).
Manchikanti L, Pampati V, Benyamin RM, Hirsch JA. Cost utility analysis of lumbar interlaminar epidural injections in the treatment of lumbar disc herniation, central spinal stenosis, and axial or discogenic low back pain. Pain Physician. 2017;20(4):219–28 (PMID: 28535546).
Manchikanti L, Helm S 2nd, Pampati V, Racz GB. Cost utility analysis of percutaneous adhesiolysis in managing pain of post-lumbar surgery syndrome and lumbar central spinal stenosis. Pain Pract. 2015;15(5):414–22. https://doi.org/10.1111/papr.12195. (Epub 2014 Mar 26 PMID: 24666747).
Manchikanti L, Pampati V, Kaye AD, Hirsch JA. Cost utility analysis of cervical therapeutic medial branch blocks in managing chronic neck pain. Int J Med Sci. 2017;14(13):1307–16. https://doi.org/10.7150/ijms.20755.PMID:29200944;PMCID:PMC5707747.
Manchikanti L, Pampati V, Parr A III, et al. Cervical interlaminar epidural injections in the treatment of cervical disc herniation, post surgery syndrome, or discogenic pain: Cost utility analysis from randomized trials. Pain Physician. 2019;22(5):421–31 (PMID: 31561644).
Manchikanti L, Falco FJE, Pampati V, Cash KA, Benyamin RM, Hirsch JA. Cost utility analysis of caudal epidural injections in the treatment of lumbar disc herniation, axial or discogenic low back pain, central spinal stenosis, and post lumbar surgery syndrome. Pain Physician. 2013;16(3):E129–43 (PMID: 23703415).
Mohamed OS, Omar SM, Gaber AF, Hassanien MM, Mohamed AM. Three needles approach-a new technique of genicular nerves radiofrequency ablation for pain relief in advanced chronic knee osteoarthritis: a randomized trial. Pain Physician. 2021;24(7):E1067–74 (PMID: 34704716).
Manchikanti L, Pampati V, Kaye AD, Hirsch JA. Therapeutic lumbar facet joint nerve blocks in the treatment of chronic low back pain: cost utility analysis based on a randomized controlled trial. Korean J Pain. 2018;31(1):27–38. https://doi.org/10.3344/kjp.2018.31.1.27. (Epub 2018 Jan 2. PMID: 29372023; PMCID: PMC5780212).
Taylor RS, Ryan J, O’Donnell R, Eldabe S, Kumar K, North RB. The cost-effectiveness of spinal cord stimulation in the treatment of failed back surgery syndrome. Clin J Pain. 2010;26(6):463–9. https://doi.org/10.1097/AJP.0b013e3181daccec. (PMID: 20551721).
Manchikanti L, Knezevic NN, Boswell MV, Kaye AD, Hirsch JA. Epidural injections for lumbar radiculopathy and spinal stenosis: a comparative systematic review and meta-analysis. Pain Physician. 2016;19(3):E365-410 (PMID: 27008296).
Chou R, Hashimoto R, Friedly J, et al. Epidural corticosteroid injections for radiculopathy and spinal stenosis: a systematic review and meta-analysis. Ann Intern Med. 2015;163(5):373–81. https://doi.org/10.7326/M15-0934. (PMID: 26302454).
US Department of Health and Human Services. Office of Inspector General (OIG). Medicare Improperly Paid Physicians for Spinal Facet-Joint Denervation Session. December 2021. https://www.oig.hhs.gov/oas/reports/region9/92103002.pdf. Accessed 6 Jul 2022.
US Department of Health and Human Services. Office of Inspector General (OIG). Medicare Improperly Paid Physicians More than Five Spinal Facet-Joint Injections Sessions During a Rolling 12-Month Period. October 2020. https://oig.hhs.gov/oas/reports/region9/92003003.pdf. Accessed 6 Jul 2022.
CGS Administrators, LLC. Local Coverage Determination (LCD). Epidural Steroid Injections for Pain Management (L39015). Original Effective Date: 12/05/2021.
CGS Administrators, LLC. Billing and Coding: Epidural Steroid Injections for Pain Management (A58731). Original Effective Date: 12/05/2021.
CGS Administrators, LLC. Response to Comments: Epidural Steroid Procedures Injections for Pain Management (A58899). Original Effective Date: 10/21/2021.
CGS Administrators, LLC. Local Coverage Determination (LCD). Facet Joint Interventions for Pain Management (L38773). Original Effective Date 5/02/2021.
CGS Administrators, LLC. Billing and Coding: Facet Joint Interventions for Pain Management (A58364). Original Effective Date 5/02/2021.
CGS Administrators, LLC. Response to Comments: Facet Joint Interventions for Pain Management (A58613). Original Effective Date 5/02/2021.
AIM Specialty Health. Appropriate Use Criteria: Interventional Pain Management (MSK01–1121.3). Effective November 7, 2021. https://aimguidelines.wpengine.com/interventional-pain-management-11-07-21/?highlight=epidural+steroid. Accessed 28 Nov 2021.
United Healthcare Commercial Medical Policy. Epidural steroid injections for spinal pain. Policy Number: 2021T0616C. Effective Date: November 1, 2021. https://www.uhcprovider.com/content/dam/provider/docs/public/policies/comm-medical-drug/epidural-steroid-injections-spinal-pain.pdf. Accessed 28 Nov 2021.
eviCORE Clinical Guidelines. CMM-200: Epidural steroid injections (ESI). Effective July 1, 2021. https://www.evicore.com/-/media/files/evicore/clinical-guidelines/solution/msk--advance/2021/cmm-200-epidural-steroid-injections_eff070121_pub030521.pdf. Accessed 28 Nov 2021.
Manchikanti L, Pampati V, Sanapati MR, Kosanovic T, Beall DP, Atluri S, et al. COVID-19 pandemic reduced utilization of interventional techniques 18.7% in managing chronic pain in the Medicare population in 2020” analysis of utilization data from 2000 to 2020. Pain Physician. 2000;2022(25):223–38.
Centers for Medicare and Medicaid Services. https://www.cms.gov/. Accessed 01 Jul 2022.
Sisko AM, Truffer CJ, Keehan SP, Poisal JA, Clemens MK, Madison AJ. National health spending projections: the estimated impact of reform through 2019. Health Aff (Millwood). 2010;29(10):1933–41. https://doi.org/10.1377/hlthaff.2010.0788. (Epub 2010 Sep 9. Erratum in: Health Aff (Millwood). 2010 Nov;29(11):2128. PMID: 20829295).
Manchikanti L, Helm S 2nd, Benyamin RM, Hirsch JA. A critical analysis of Obamacare: affordable care or insurance for many and coverage for few? Pain Physician. 2017;20(3):111–38 (PMID: 28339427).
Manchikanti L, Singh V, Benyamin RM, Kaye AD, Pampati V, Hirsch JA. Reframing Medicare physician payment policy for 2019: a look at proposed policy. Pain Physician. 2018;21(5):415–32 (PMID: 30282387).
Hirsch JA. The pincer movement of cost and quality in neurointerventional care: resource management as an imperative. J Neurointerv Surg. 2019;11(4):323–5. https://doi.org/10.1136/neurintsurg-2019-014871. (PMID: 30890616).
Hirsch JA, Leslie-Mazwi T, Nicola GN, et al. Storm rising! The Obamacare exchanges will catalyze change: why physicians need to pay attention to the weather. J Neurointerv Surg. 2019;11(2):101–6. https://doi.org/10.1136/neurintsurg-2018-014412. (Epub 2018 Oct 29 PMID: 30373811).
Spilberg G, Nicola GN, Rosenkrantz AB, et al. Understanding the impact of ‘cost’ under MACRA: a neurointerventional imperative! J Neurointerv Surg. 2018;10(10):1005–11. https://doi.org/10.1136/neurintsurg-2018-013972. (Epub 2018 Jul 23 PMID: 30038063).
Golding LP, Nicola GN, Ansari SA, et al. MACRA 2.5: the legislation moves forward. J Neurointerv Surg. 2018;10(12):1224–8. https://doi.org/10.1136/neurintsurg-2018-013910. (Epub 2018 Jul 4. PMID: 29973387).
Manchikanti L, Falco FJE, Benyamin RM, Gharibo CG, Candido KD, Hirsch JA. Epidural steroid injections safety recommendations by the MultiSociety Pain Workgroup (MPW): More regulations without evidence or clarification. Pain Physician. 2014;17(5):E575–88 (PMID: 25247907).
Manchikanti L, Helm S 2nd, Singh V, et al. Accountable interventional pain management: A collaboration among practitioners, patients, payers, and government. Pain Physician. 2013;16(6):E635–70 (PMID: 24284849).
Manchikanti L, Singh V, Hirsch JA. Facility payments for interventional pain management procedures: impact of proposed rules. Pain Physician. 2016;19(7):E957–84 (PMID: 27676688).
Boswell MV, Manchikanti L, Kaye AD, et al. A best-evidence systematic appraisal of the diagnostic accuracy and utility of facet (zygapophysial) joint injections in chronic spinal pain. Pain Physician. 2015;18(4):E497-533 (PMID: 26218947).
Manchikanti L, Kaye AD, Boswell MV, et al. A systematic review and best evidence synthesis of the effectiveness of therapeutic facet joint interventions in managing chronic spinal pain. Pain Physician. 2015;18(4):E535–82 (PMID: 26218948).
Manchikanti L, Abdi S, Atluri S, et al. An update of comprehensive evidence-based guidelines for interventional techniques of chronic spinal pain: Part II: guidance and recommendations. Pain Physician. 2013;16(2 Suppl):S49-283 (PMID: 23615883).
Manchikanti L, Hirsch JA, Kaye AD, Boswell MV. Cervical zygapophysial (facet) joint pain: effectiveness of interventional management strategies. Postgrad Med. 2016;128(1):54–68. https://doi.org/10.1080/00325481.2016.1105092. (Epub 2015 Dec 10 PMID: 26653406).
Manchikanti L, Hirsch JA, Falco FJE, Boswell MF. Management of lumbar zygapophysial (facet) joint pain. World J Orthop. 2016;7(5):315–37. https://doi.org/10.5312/wjo.v7.i5.315. (PMID: 27190760; PMCID: PMC4865722).
Song K, Li Z, Shuang F, et al. Comparison of the effectiveness of radiofrequency neurotomy and endoscopic neurotomy of lumbar medial branch for facetogenic chronic low back pain: a randomized controlled trial. World Neurosurg. 2019;126:e109–15. https://doi.org/10.1016/j.wneu.2019.01.251. (Epub 2019 Feb 18 PMID: 30790724).
Starr JB, Gold LS, McCormick Z, Suri P, Friedly J. Repeat procedures and prescription opioid use after lumbar medial branch nerve radiofrequency ablation in commercially insured patients. Spine J. 2019;20(3):344–51. https://doi.org/10.1016/j.spinee.2019.10.005. (Epub 2019 Oct 22. PMID: 31654808; PMCID: PMC7060813).
Juch JNS, Maas ET, Ostelo RWJG, et al. Effect of radiofrequency denervation on pain intensity among patients with chronic low back pain: the Mint randomized clinical trials. JAMA. 2017;318(1):68–81. https://doi.org/10.1001/jama.2017.7918. (Erratum in: JAMA. 2017 Sep 26;318(12 ):1188. PMID: 28672319; PMCID: PMC5541325).
Snidvongs S, Taylor RS, Ahmad A, et al. Facet-joint injections for non-specific low back pain: a feasibility RCT. Health Technol Assess. 2017;21(74):1–130. https://doi.org/10.3310/hta21740. (PMID: 29231159; PMCID: PMC5742455).
Jarow JP, LaVange L, Woodcock J. Multidimensional evidence generation and FDA regulatory decision making: defining and using “real-world” data. JAMA. 2017;318(8):703–4. https://doi.org/10.1001/jama.2017.9991. (PMID: 28715550).
Sherman RE, Anderson SA, Dal Pan GJ, et al. Real-world evidence—what is it and what can it tell us? N Engl J Med. 2016;375:2293–7. https://doi.org/10.1056/NEJMsb1609216. (PMID: 27959688).
Manchikanti L, Boswell MV, Kaye AD, et al. Therapeutic role of placebo: Evolution of a new paradigm in understanding research and clinical practice. Pain Physician. 2017;20(5):363–86 (PMID: 28727700).
Cappola AR, FitzGerald GA. Confluence, not conflict of interest: Name change necessary. JAMA. 2015;314(17):1791–2. https://doi.org/10.1001/jama.2015.12020. (PMID: 26402846).
Manchikanti L, Knezevic NN, Sanapati J, et al. Is epidural injection of sodium chloride solution a true placebo or an active control agent? A systematic review and meta-analysis. Pain Physician. 2021;24(1):41–59 (PMID: 33400427).
Manchikanti L, Knezevic NN, Parr A III, et al. Does epidural bupivacaine with or without steroids provide long-term relief? A systematic review and metaanalysis. Curr Pain Headache Rep. 2020;24(6):26. https://doi.org/10.1007/s11916-020-00859-7. (PMID: 32335757).
Lee JH, Shin KS, Park SJ, et al. Comparison of clinical efficacy between transforaminal and interlaminar epidural injections in lumbosacral disc herniation: a systematic review and meta-analysis. Pain Physician. 2018;21(5):433–48 (PMID: 30282389).
Lee JH, Kim DH, Kim DH, et al. Comparison of clinical efficacy of epidural injection with or without steroid in lumbosacral disc herniation: a systematic review and meta-analysis. Pain Physician. 2018;21(5):449–68 (PMID: 30282390).
Acknowledgements
The authors wish to thank Bert Fellows, MA, Director Emeritus of Psychological Services at Pain Management Centers of America, for manuscript review, and transcriptionists Tonie M. Hatton and Diane E. Neihoff, transcriptionists, for their assistance in the preparation of this manuscript.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Laxmaiah Manchikanti, MD, Vidyasagar Pampati, MSc, Alan Kaye, MD, and Joshua Hirsch, MD. The first draft of the manuscript was written by Laxmaiah Manchikanti, MD, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Joshua Hirsch is a consultant for Medtronic and Senior Affiliate Research Fellow at the Neiman Policy Institute. Laxmaiah Manchikanti, Alan Kaye, Richard Latchaw, Mahendra Sanapati, and Vidyasagar Pampati have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Manchikanti, L., Kaye, A.D., Latchaw, R.E. et al. Impact of the COVID-19 Pandemic on Utilization Patterns of Facet Joint Interventions in Managing Spinal Pain in a Medicare Population. Pain Ther 12, 505–527 (2023). https://doi.org/10.1007/s40122-023-00476-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00476-3