Abstract
Background
Extensive research into potential sources of neck pain and referred pain into the upper extremities and head has shown that the cervical facet joints can be a potential pain source confirmed by precision, diagnostic blocks.
Study Design
Systematic review and meta-analysis utilizing the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist, quality assessment of the included studies, conventional and single-arm meta-analysis, and best evidence synthesis.
Objective
The objective of this systematic review and meta-analysis is to evaluate the effectiveness of radiofrequency neurotomy as a therapeutic cervical facet joint intervention in managing chronic neck pain.
Methods
Available literature was included. Methodologic quality assessment of studies was performed from 1996 to September 2021. The level of evidence of effectiveness was determined.
Results
Based on the qualitative and quantitative analysis with single-arm meta-analysis and Grading of Recommendations, Assessment, Development and Evaluations (GRADE) system of appraisal, with inclusion of one randomized controlled trial (RCT) of 12 patients in the treatment group and eight positive observational studies with inclusion of 589 patients showing positive outcomes with moderate to high clinical applicability, the evidence is level II in managing neck pain with cervical radiofrequency neurotomy. The evidence for managing cervicogenic headache was level III to IV with qualitative analysis and single-arm meta-analysis and GRADE system of appraisal, with the inclusion of 15 patients in the treatment group in a positive RCT and 134 patients in observational studies. An overwhelming majority of the studies produced multiple lesions.
Limitations
There was a paucity of literature and heterogeneity among the available studies.
Conclusion
This systematic review and meta-analysis shows level II evidence with radiofrequency neurotomy on a long-term basis in managing chronic neck pain with level III to IV evidence in managing cervicogenic headaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic axial neck pain is one of the major causes of disability and healthcare costs, accounting for nearly half of the US health care burden, with neck pain among the top three causes |
Cervical facet joints have been shown to be potential sources of neck pain and referred pain into upper extremities and head |
The present systematic review identified a total of 5 RCTs and 15 observational studies with 2 RCTs evaluating the role of radiofrequency in managing facet joint pain |
The evidence is level II in managing neck pain with cervical radiofrequency neurotomy and level III to IV in managing cervicogenic headache |
There continues to be significant paucity of literature and heterogeneity among the available studies |
Introduction
Chronic axial neck pain with or without headache or upper extremity pain is one of the major causes of disability and health care costs. The widely published literature shows that morbidity and chronic disability now account for nearly half of the US health care burden, with neck pain ranking as number three among the 30 leading diseases and injuries [1,2,3,4,5,6]. In addition, Dieleman et al. [7, 8] showed an estimated spending of $134.5 billion in 2016, with a 53.5% increase from $87.6 billion spent in 2013, in managing low back and neck pain, accounting for the highest amount of various disease categories.
Bogduk and Marsland [9] described facet joints as a source of idiopathic neck pain in 1988. Since then, numerous diagnostic accuracy studies, systematic reviews, and guidelines have been published [3, 10,11,12,13,14,15,16,17,18,19,20]. Multiple discussions have continued to evolve in reference to the diagnosis of facet joint pain and subsequent therapy with either facet joint nerve blocks or radiofrequency neurotomy [3, 21, 22]. The present evidence shows that the prevalence and false positive rates of diagnosis of facet joint pain with controlled comparative local anesthetic blocks utilizing 80% criterion standard ranges from 29% to 60% and 27% to 63%, respectively, with high variability. The discussion centers around the value and validity based on the acute pain model or chronic pain model. The group headed by Bogduk described that any response longer than 2 h for short-acting local anesthetic and 8 h for long-acting local anesthetic was a discordant response and judged it as false positive [10, 11, 14,15,16, 23]. This theory was tested with lumbar facet joint nerve blocks with 100% pain relief as the criterion standard [23]. The prevalence was shown to be 15% [23]. Manchikanti et al. [10] showed prevalence and false positive rates of 49.3% and 25.6%, respectively, in chronic neck pain using a chronic pain model. They also showed that the duration of relief of at least 80% was 6 days with lidocaine and 12 days with bupivacaine, with a total relief of at least 50% of 31 days and 55 days, respectively. In addition to multiple publications by Manchikanti et al. [10, 18,19,20,21,22, 24], a recent randomized controlled trial (RCT) by van Eerd et al. [25] of the comparative value of local anesthetic blocks with radiofrequency neurotomy in patients with clinically diagnosed cervical facet joint pain showed pain treatment success of 61.1% in both groups, either with local anesthetic alone or with local anesthetic and radiofrequency neurotomy with a single lesion at 3 months, 55.6% in the denervation group and 51.3% in the bupivacaine alone group at 6-month follow-up with no significant difference among the groups, reinforcing long-term relief of local anesthetic injections [24, 26,27,28,29,30,31].
Among the therapeutic interventions, radiofrequency has been considered as the standard treatment to provide long-term improvement; however, there has been only one RCT and three observational studies assessed in the previous evaluations [3]. The first systematic review by Geurts et al. [32] identified only one RCT by Lord et al. [33]. A recent systematic review of the literature by Engel et al. [34] published in 2020 evaluated the effectiveness of cervical medial branch thermal radiofrequency neurotomy stratified by selection criteria. They concluded that higher degrees of relief from cervical medial branch thermal radiofrequency neurotomy are more often achieved, to a statistically significant extent, if patients are selected on the basis of the complete relief of index pain following comparative diagnostic blocks and used a randomized trial [33] and multiple nonrandomized studies [33, 35,36,37,38,39,40,41,42]. They utilized selection criteria as complete relief, with placebo-controlled blocks, complete relief with comparative blocks, 75% relief with comparative blocks, or 50% relief with comparative blocks. Thus, they showed that on the basis of a lesser degree of relief, patients are less likely to obtain complete relief. In another review of best practice guidelines, Lee et al. [43] utilized one RCT [33] and multiple clinical studies [33, 36, 38, 39, 41, 42] like Engel et al. [34]. They concluded that the efficacy of radiofrequency neurotomy was directly related to the rigor of the diagnostic blocks performed, as well as the use of proper technique for both diagnostic and neurotomy procedures. They also opined that utilizing multiple passes and two separate approaches may allow for neurotomy in a larger proportion of the medial branch, resulting in improved pain relief with longer duration. in a systematic review in preparation of guidelines, Manchikanti et al. [3] showed level II evidence for short-term and long-term effectiveness utilizing one RCT [33] and three observational studies [35, 36, 41] and provided level II evidence with moderate strength of recommendation when performed after the diagnosis of cervical facet joint pain with controlled comparative local anesthetic blocks utilizing 80% pain relief of criterion standard. However, there are also other issues related to producing multiple lesions at each nerve and needle sizes may be variable, too. These can alter the responses and also the side effect profile.
In a recent publication, Manchikanti et al.’s [44] comparative effectiveness study of cervical facet radiofrequency and cervical facet joint nerve blocks in a similar group of population showed that a significant proportion of the radiofrequency-treated patients (29%) obtained inadequate relief (less than minimum of 6 months) and 4% of patients also developed side effects related to irritation, swelling, and increased levels of pain, etc. In fact, this study showed that cervical facet joint nerve blocks may be better than radiofrequency neurotomy in reference to the tolerance and providing relief as expected for 3 months and with a cost utility of 1 year of quality-of-life improvement ($4994 vs. $5364).
Additionally, the COVID-19 pandemic and the opioid epidemic have affected chronic pain sufferers substantially with both access to treatment and costs [45,46,47,48,49,50,51,52]. Recent analysis of national health care spending in the USA showed an increase of 9.7% to reach $4.1 trillion in 2020, a much faster rate than the 4.3% increase seen in 2019 [51]. The acceleration in 2020 was due to a 36% increase in federal expenditures for health care that occurred largely in response to the COVID-19 pandemic. These increases were reported despite health care expenditures for health care unrelated to the COVID-19 pandemic. Further, consolidation of providers into an employment model by health systems, which has increased substantially, has been contributing to increasing health care expenses [52]. Multiple effects due to COVID-19 with increased psychological stress and suffering may also have a significant effect on outcomes. The use of interventional techniques for the treatment of spinal pain increased exponentially until 2009, at which point utilization started decreasing [53,54,55,56,57,58]. A recent analysis of utilization patterns and fee-for-service (FFS) Medicare population, including the impact of COVID-19, showed declining interventional techniques with overall decrease of interventional techniques at an annual rate of 0.4% per 100,000 Medicare population from 2010 to 2019, with an annual increase of 2.1% for facet joint interventions and sacroiliac joint injections from 2010 to 2019. However, the decrease from 2019 to 2020 due to the COVID-19 pandemic was 18.7% for all interventions compared to 17.5% for facet joint interventions and sacroiliac joint blocks [59].
Consequently, the debate in reference to effectiveness and efficacy, utilization patterns, and indications and medical necessity of cervical radiofrequency neurotomy procedures continues among patients, clinicians, researchers, and payors [3, 44].
The present systematic review and meta-analysis of RCTs and observational studies of radiofrequency neurotomy in managing chronic neck pain is sought to provide updated evidence.
Methods
A systematic review and meta-analysis were performed on the basis of methodological and reporting quality of systematic reviews as described by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [60, 61]. Methodology from other reviews was also utilized [62, 63].
The objective of this systematic review and meta-analysis was to assess the efficacy and effectiveness of radiofrequency thermoneurolysis in managing chronic neck pain of facet joint origin.
Ethics Compliance
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Literature Search
A comprehensive literature search was conducted to include RCTs published from all countries and in all languages. Searches were performed from the following sources without language restrictions:
-
1.
PubMed from 1966 https://pubmed.ncbi.nlm.nih.gov/
-
2.
Cochrane Library https://www.cochranelibrary.com/
-
3.
Google Scholar https://scholar.google.com/
-
4.
US National Guideline Clearinghouse (NGC) https://www.ahrq.gov/gam/index.html
-
5.
Clinical Trials https://www.clinicaltrials.gov/
-
6.
Previous systematic reviews and cross-references
-
7.
All other sources including non-indexed journals and abstracts
The search period was from 1966 through September 2021.
Search Strategy
The search strategy emphasized chronic neck pain treated with cervical facet joint interventions. The search terms included ((((((spinal pain, chronic low back pain) OR chronic back pain) OR facet joint pain) OR cervical surgery syndrome) OR zygapophysial)) AND ((((facet joint) OR zygapophyseal) OR zygapophysial) OR medial branch block OR intraarticular injection OR radiofrequency neurotomy) OR radiofrequency ablation.
Inclusion and Exclusion Criteria
RCTs studying radiofrequency neurotomy with at least 6 months of follow-up were included in this study. The trials with appropriate diagnosis established by diagnostic blocks or clinical diagnosis were included.
All observational studies of radiofrequency neurotomy with at least 6 months of follow-up were also included meeting the criteria.
Studies without an appropriate diagnosis and case reports were excluded.
Methodological Quality Assessment
RCTs were assessed for their quality or risk of bias methodologically utilizing Cochrane review criteria (Table 1 in the supplementary material) [64], Interventional Pain Management techniques–Quality Appraisal of reliability and Risk of Bias Assessment (IPM-QRB) (Table 2 in the supplementary material) [65], and Interventional Pain Management Techniques–Quality Appraisal of Reliability and Risk of Bias Assessment for Nonrandomized Studies (IPM-QRBNR) was utilized for observational studies, as shown in Table 3 in the supplementary material [66].
Risk of Bias of Individual Studies
Trials that met the inclusion criteria and scored at least 9 of 13 using the Cochrane review criteria [64] were considered high quality, while trials scoring 5–8 were considered of moderate quality. Trials that scored less than 5 were considered of low quality and were excluded from the analysis.
Trials meeting the inclusion criteria were also assessed with IPM-QRB criteria [65]. Studies scoring 32–48 were considered of high quality, those scored 16–31 were of moderate quality, and those that scored below 16 were considered of low quality and were excluded from the analysis.
On the basis of IPM-QRBNR criteria [66], studies meeting the inclusion criteria but scoring less than 16 were considered low quality and were excluded, studies scoring from 16 to 31 were considered moderate quality, and studies scoring from 32 to 48 were considered high quality and were included.
Methodological quality of the trials was assessed by two authors, independently in an unblinded manner. If a discrepancy occurred, a third author was involved to resolve the conflict. When an issue of conflict of interest was raised in reviewing the manuscript (regarding authorship), the involved authors were not allowed to review those manuscripts for quality assessment.
Outcome Measures
An outcome is considered clinically significant if a reduction of 2 points on the Visual Analog Scale (VAS) or Numeric Rating Scale (NRS), or at least 50% reduction in pain and improvement in the functional status. A positive study is said to be clinically significant and effective indicating that the primary outcome should be statistically significant at a P value ≤ 0.05.
Analysis of Evidence
The evidence was analyzed utilizing qualitative and quantitative evidence synthesis. Quantitative evidence synthesis was performed utilizing conventional meta-analysis and a single-arm meta-analysis.
The qualitative analysis of the evidence was performed on the basis of best-evidence synthesis, modified, and collated using multiple criteria, including the Cochrane Review criteria and United States Preventive Services Task Force (USPSTF) criteria as illustrated in Table 1 [67]. The analysis was conducted using five levels of evidence ranging from strong to opinion- or consensus-based. The results of best evidence as per grading were utilized and Grading of Recommendations, Assessment, Development and Evaluations (GRADE) system of appraisal for determining the body of evidence [68]. Clinical relevance and pragmatism of all studies were assessed [69]. At least two of the review authors independently, in a standardized manner, analyzed the evidence. Any disagreements between reviewers were resolved by a third author and consensus was attained. If there were any conflicts of interest (e.g., authorship), the reviewers of interest were recused from assessment and analysis.
Results
Literature Search
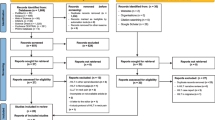
The flow diagram illustrates the search results and the final number of studies that were considered for inclusion (Fig. 1). The search criteria started with a total of 1146 publications, with 28 studies [25, 33, 35,36,37,38,39,40,41,42, 44, 70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88] with different aspects considered for inclusion. The full articles were reviewed for 23 studies [25, 33, 35,36,37,38,39,40,41,42, 44, 70,71,72,73,74,75,76,77,78, 86,87,88]. Among the 23 studies considered for inclusion, two studies were excluded because of lack of availability of the full articles [78, 88]. An additional study [37] was also excluded as it was reporting previously published data. Overall, 20 studies met inclusion criteria [25, 33, 35, 36, 38,39,40,41,42, 44, 70,71,72,73,74,75,76,77, 86, 87], out of which five RCTs [25, 33, 71,72,73] were selected (Fig. 1). Of the five RCTs, only one of them assessed with a sham control [33] and one was an active-control trial [25] studying efficacy for neck pain, two RCTs evaluated the role of radiofrequency in managing cervicogenic headache [72, 73], and one assessed psychological distress [71]. Among the 15 observational studies [35, 36, 38,39,40,41,42, 44, 70, 74,75,76,77, 86, 87], there were eight studies assessing neck pain [35, 36, 38, 39, 41, 70, 74, 77], five studies assessing cervicogenic headache [40, 42, 77, 86, 87], and two studies assessed psychological functioning [75, 76]. Among the RCTs assessing neck pain, only one study [33] utilized diagnostic blocks as the criterion standard for inclusion, whereas the second study was performed on the basis of clinical examination [25]. Among the observational studies, all of them except one study utilized diagnostic blocks prior to the enrollment; however, van Eerd et al. [70], similar to the RCT [25], based the inclusion on clinical criteria. Only four studies in five publications [39, 75,76,77, 86] utilized 50% pain relief with dual blocks, whereas the remaining studies utilized 80% or greater pain relief for the inclusion criteria; six studies [33, 36, 42, 71, 74, 87] included 100% relief as the inclusion criteria. Among the four RCTs, a single lesion was applied in only one study, whereas all others utilized multiple lesions ranging from two to six. Among the observational studies, two studies [44, 70] utilized a single lesion, whereas all others utilized multiple lesions of more than two and up to six. Needle cannula sizes varied from 22 to 18 gauge and the exposed tip varied from 4 to 10 mm. Where data is available, all studies utilized a local anesthetic prior to lesioning, whereas one study reported utilizing bupivacaine injection after lesioning. Procedure time description was provided in only a few studies; these included 90 min for three level radiofrequencies [72], and 3 h for a single lesion [33, 71].
Methodological Quality Assessment
The methodological quality assessment of the RCTs meeting the inclusion criteria was carried out using Cochrane review criteria and IPM-QRB, and observational studies utilizing IMP-QRBNR criteria and the results are illustrated in Tables 2, 3, and 4.
According to the Cochrane quality assessment and the previously established score ranges in the “Methods” section of this study, three trials [25, 33, 71] scored between 9 and 13, thus meeting our criteria of high-quality studies, while two trials [72, 73] scored between 5 and 8, thus said to be studies of moderate quality.
On the basis of the IPM-QRB criteria for randomized trials, five trials [25, 33, 71,72,73] scored between 32 and 48, hence they are of high quality. Thus, only three trials met the criteria for high quality with both instruments [25, 33, 71]. This indicates the importance of IPM specific instruments in methodologic quality assessments.
On the basis of the IPM-QRBNR criteria for observational studies, five studies [35, 36, 41, 75, 76] scored between 32 and 48, hence they are of high quality, while 10 studies [38,39,40, 42, 44, 70, 74, 77, 86, 87] scored between 16 and 31, thus are considered as moderate quality.
Study Characteristics of RCTs and Observational Studies
Among the total of five RCTs available, there were two RCTs in the neck pain category [25, 33], two trials for the treatment of headache [72, 73], whereas one trial [71] evaluated psychological distress from the partial data derived from the neck effectiveness study [33].
Table 5 shows the study characteristics of all the included randomized trials assessing cervical radiofrequency neurotomy in neck pain and headache.
The study characteristics of observational studies meeting inclusion criteria are described in Table 6. There were a total of 15 observational studies included in the analysis [35, 36, 38,39,40,41,42, 44, 70, 74,75,76,77, 86, 87] with eight studies assessing neck pain [35, 36, 38, 39, 41, 70, 74, 77], five studies assessing cervicogenic headache [40, 42, 77, 86, 87], and two studies assessing psychological functioning [75, 76].
Analysis of Evidence
Table 5 shows the study characteristics of all the studies meeting inclusion criteria for RCTs, whereas Table 6 shows study characteristics of observational studies assessing cervical radiofrequency neurotomy. The analysis of evidence was based on qualitative and quantitative analysis.
Qualitative Analysis
As shown in Tables 7 and 8, qualitative analysis was determined on the basis of multiple factors including the application of diagnostic blocks, number of patients, number of lesions, successful outcomes, clinical utility, and pragmatism. In addition, GRADE criteria were also applied with downgrading or no change or upgrading of the study quality.
Overall, 11 studies were included in the qualitative analysis of treatment of chronic neck pain with radiofrequency neurotomy. Of these, five studies utilized 100% pain relief as the criterion standard for inclusion with inclusion of 201 patients. In all studies [33, 36, 38, 42] except one [74], 4–6 lesions were performed. The results showed complete pain relief variable from 58% to 74% of the patients in three studies [33, 36, 38], whereas 70% was reported in one study with similar 4–6 lesions with at least 50% relief in 70% of the patients with one study with twi lesions [74] reporting in 54% of the patients. Clinical utility of these studies was judged as moderate for four studies [33, 36, 38, 42] and high for one study [74]. There was no change in the GRADE criteria.
Three studies utilized at least 80% pain relief as inclusion criterion [35, 41, 44] with controlled diagnostic blocks with inclusion of 361 patients with three lesions produced in one study [35] reporting 39% complete relief and 79% at least 50% relief at 1 year; a minimum of two lesions were produced in one prospective assessment [41] involving 30 litigant patients and 30 nonlitigant patients with improvement in 46% of the former and in 73% of the latter. The study was judged to be positive in nonlitigant patients. Another clinical study [44] comparing radiofrequency neurotomy with cervical medial branch blocks utilizing one lesion reported at least 50% relief in 69% of the patients at 6-month follow-up and 64% at 1-year follow-up with repeat radiofrequency performed as needed. Clinical utility was moderate in two studies [35, 41] and high in one study [44]. There was no change in GRADE criteria.
There was only one study [39] utilizing 50% pain relief as the criterion standard producing four lesions; it reported 100% pain relief in 42% of the patients at 6-month follow-up and in 68% at least 50% pain relief at 6-month follow-up. This was shown to be a positive study with moderate clinical utility with no change in GRADE criteria.
Two studies [25, 65], which included an RCT [25], studied without diagnostic blocks based on clinical criteria. The RCT utilized 30% improvement as the pain relief criterion. Both studies were shown to be negative with low clinical applicability based on selection criteria with no change in GRADE criteria for the observational study [70] and reduction of GRADE criteria for the RCT [25].
Table 8 shows qualitative analysis for headache. Seven studies met the inclusion criteria [40, 42, 72, 73, 77, 86, 87]. Of these, only two studies [42, 87] utilized complete pain relief as the criterion standard producing multiple lesions with positive results in both studies. In one study [42] utilizing complete pain relief as the criterion standard for diagnosis, nine patients were included with headache producing 4–6 lesions; however, they reported at least 50% pain relief in only 40%. Consequently, this study was shown as negative with absent clinical applicability with reduced grading for headache. The second study [87] evaluated 49 patients with complete pain relief utilizing 4–6 lesions and reported excellent results with 88% of the patients reporting complete pain relief at 6-month follow-up shown to be positive results with moderate clinical applicability due to required 100% pain relief and 4–6 lesions, which is a long duration of procedure. There was no change in the GRADE criteria.
Only one study [40] utilized at least 80% pain relief as the criterion standard and studied 11 patients with a single lesion reporting at least 50% pain relief in 68% at 6 months; this study was shown to be positive with high clinical applicability with no change in scoring based on GRADE criteria.
Two other studies [77, 86] studied 30 patients and 49 patients utilizing 50% pain relief as the criterion standard reporting at least 50% relief in 77% of the patients at 1 year [77] and 70% of the patients at 6 months in the second study [86]. Ironically, the study utilizing a single lesion produced better results [77] compared to 2–3 lesions produced in the second study [86]. Consequently, the study by Lee et al. [77] shows high clinical applicability with no change in GRADE criteria.
Finally, two studies [72, 73] based their treatments on clinical criteria with a small number of patients with 6 plus 15 producing 3–4 lesions in one study [72] and only one lesion in the second study [73]. The study with 3–4 lesions was shown to be negative with absent clinical applicability with reduction in grading criteria. The second study, however, showed with a single lesion at least 50% improvement in 53%of patients, once again with low clinical applicability based on reduced criteria on GRADE. Consequently, it appears from the qualitative analysis that strict inclusion criteria of 100% pain relief with controlled diagnostic blocks and producing multiple lesions are superior to other selection criteria in managing neck pain with moderate to low clinical applicability due to the rigorous criteria, making this approach difficult to apply in the USA, because of the long duration of the procedure, which may not be feasible in the USA.
Among the five studies included with complete pain relief [33, 36, 38, 42, 74], only three of them achieved superior results [33, 36, 38] with complete pain relief, whereas the other two [42, 74], despite 2 or 4–6 lesions, achieved criteria similar to the 80% pain relief groups with 54% and 70% of patients at 1-year follow-up.
Comparatively, there were three studies [35, 41, 44] utilizing 80% pain relief with the controlled diagnostic blocks as the criterion standard utilizing a large proportion of patients. A total of 362 patients utilized either one [44], two [41], or three [35] lesions. However, the pain relief judged by the at least 50% criterion was higher in the three-lesion group with 79%, and two-lesion group, with 73% compared to one-lesion study with 64%. Consequently, clinical utility has been judged as moderate for the first two studies with multiple lesions [35, 41] and high with a single lesion [44], which is the common practice without compromising the outcomes.
There was only one study utilizing at least 50% pain relief as the inclusion criterion with inclusion of 28 patients producing four lesions, and it showed at least 50% relief in 68% of the patients similar to other categories with moderate clinical utility based on four lesions produced.
Thus, overall, on the basis of one RCT [33] with 12 patients in the treatment group and eight positive observational studies [35, 36, 38, 39, 41, 42, 44, 74] with inclusion of 589 patients, the outcomes were positive with moderate to high clinical applicability. Two studies [25, 70] with inclusion of 106 patients showed negative results, one of them being an RCT with low clinical applicability and downgrading as per GRADE criteria. Thus, the evidence is level II with a moderate recommendation for cervical radiofrequency neurotomy in managing neck pain.
The evidence based on qualitative analysis in managing cervicogenic or occipital headache is inferior to managing neck pain with one RCT, with inclusion of six patients in the treatment group, showing negative results [72] and lack of clinical utility; the second RCT [73], with inclusion of 15 patients in the treatment group, showing only borderline outcomes with low clinical utility; and five observational studies [40, 42, 77, 86, 87], with inclusion of 134 patients, showing positive results with moderate to low clinical utility with multiple lesions in every study except one [73], the evidence being level III to IV, yielding a borderline recommendation.
Quantitative Analysis
We sought to perform a quantitative analysis utilizing conventional dual-arm meta-analysis and single-arm meta-analysis. However, there were only two RCTs evaluating radiofrequency in the neck [25, 33] and two evaluating headache [72, 73]. The methodologic quality was highly variable among the two trials [25, 33] performed in the cervical spine. Similarly, methodologic quality and variations were significant in the headache group with a small number of patients included in two RCTs [72, 73] in the headache trials. Consequently, dual-arm analysis was not performed.
A single-arm meta-analysis was performed for all observational studies in managing neck pain and headache separately.
Single-Arm Meta-analysis
Figure 2 shows the results of a single-arm analysis utilizing the radiofrequency ablation groups. Five studies [25, 40, 41, 66, 73] were used to assess pain scores after 6 months using pain scores in patients who underwent radiofrequency neurotomy. As shown in Fig. 2, the pooled mean difference of pain score from baseline to 6 months of follow-up was decreased by 4.157 points (95% CI − 4 .260 to − 4.053, P < 0.001).
Figure 3 shows the results of a single-arm analysis utilizing the control treatment groups. Three studies [25, 66, 73] were used to assess pain scores after 6 months using pain scores in patients who underwent the control treatment. As shown in Fig. 3, the pooled mean difference of pain scores from baseline to 6 months of follow-up was decreased by 4.725 points (95% CI − 4.835 to − 4.616, P < 0.001).
Figure 4 shows the results of a single-arm analysis utilizing the radiofrequency ablation groups. Three studies [41, 66, 73] were used to assess pain score after 12 months using pain scores in patients who underwent radiofrequency neurotomy. As shown in Fig. 4, the pooled mean difference of pain score from baseline to 12 months of follow-up was decreased by 4.762 points (95% CI − 4.897 to − 4.628, P < 0.001).
Figure 5 shows the results of a single-arm analysis utilizing the control treatment groups. Two studies [66, 73] were used to assess pain scores after 12 months using pain scores in patients who underwent the control treatment. As shown in Fig. 5, the pooled mean difference of pain scores from baseline to 12 months of follow-up was decreased by 4.895 points (95% CI − 5.010 to − 4.779, P < 0.001).
Thus, quantitative analysis with single-arm meta-analysis showed positive results at 6 months and 12 months both in treatment and control groups. The differences were rather significant from baseline to follow-up at 6 months and 12 months with 4.2 points decrease in the treatment group, and 4.7 points decrease in the control group at 6-month follow-up, and 4.8 and 4.9 points in the treatment and control groups at 12-month follow-up. The results are similar to qualitative analysis with level II evidence with moderate recommendation for cervical radiofrequency neurotomy in managing neck pain and level III to IV, and thus a borderline recommendation of radiofrequency neurotomy in managing headache with only one study meeting eligibility criteria to be included in single-arm analysis.
Discussion
This systematic review of RCTs and observational studies and meta-analysis of observational studies of the effectiveness of cervical radiofrequency neurotomy in managing chronic neck pain showed level II evidence for long-term effectiveness of 6 months or longer. However, the evidence for neck pain and headaches utilizing radiofrequency neurotomy is level III–IV with only a borderline recommendation.
For qualitative analysis in managing neck pain, one RCT [33] with 12 patients in the treatment group and eight positive observational studies [35, 36, 38, 39, 41, 42, 44, 74] with inclusion of 589 patients showed positive outcomes with moderate to high clinical applicability. However, two studies [25, 70] with the inclusion of 106 patients showed negative results, one of them being an RCT with low clinical applicability and the study was downgraded by application of GRADE criteria.
For quantitative analysis, while conventional meta-analysis was not feasible, single-arm analysis showed positive results in all the included studies [25, 40, 41, 66, 73] in the treatment group, as well as control groups with significant decreases in pain patterns from baseline to the follow-up period of 4.2 and 4.8 points at 6- and 12-month follow-up, respectively, in the treatment group, and 4.7 and 4.9 points in the control group at 6 and 12-month follow-up, respectively. These relief patterns were achieved in the majority of the cases with repeat procedures in multiple studies. Overall success rate ranged from 42% to 74% at 6 months and 58% to 76% at 1 year. These results are based on studies utilizing high levels of diagnostic criteria and many studies producing multiple lesions, often with large needles.
For managing cervicogenic headache these results are poor. We included one RCT [72] with only six patients with negative results and the second RCT [73] with inclusion of 15 patients showing only borderline outcomes with low clinical utility. Further, there were five observational studies [40, 42, 77, 86, 87], with the inclusion of 134 patients, that showed positive results with moderate to low clinical utility with multiple lesions in three studies [42, 86, 87] and a single lesion in two studies [40, 77], the evidence level is level III to IV, with borderline recommendation. Of note, none of the studies met criteria for conventional meta-analysis and only one study met inclusion criteria for single-arm analysis [73].
The results of the present analysis are similar in some aspects, but significantly different in other aspects from other previously published systematic reviews and guidelines.
The guidelines for facet joint interventions [3] showed level II evidence with moderate strength of recommendations with inclusion of one RCT with positive results, and two observational studies with long-term improvement in managing neck pain. Engel et al.’s [34] systematic review of the literature with inclusion of RCTs and observational studies showed variable results based on selection criteria, including triple placebo-controlled medial branch blocks, dual comparative medial branch blocks, single medial branch blocks, intraarticular blocks, and physical examination findings or symptoms alone. Further, the data showed a greater degree of pain relief more often in patients selected by triple placebo controlled medial branch blocks or dual comparative medial branch blocks, producing 100% relief of the index pain. However, the degree of pain relief was similar when triple or dual comparative blocks were used. It is also of importance to note that Engel et al. [34] stratified the outcomes, showing in patients with placebo controlled or comparative blocks with 100% pain relief a success rate of 52% in the placebo-controlled blocks group with inclusion of 64 patients (94% CI 40–64) with 100% pain relief. Similarly to the placebo-controlled blocks, comparative dual blocks with inclusion of 125 patients showed a success rate of 61% (95% CI 52–70%). In contrast, with 75% relief with comparative blocks the pooled results with inclusion of 234 patients showed a success rate of 31% (95% CI 25–37%) with complete relief; however, there was a 44% success rate with 80% relief (95% CI 37–51%), and a 59% success rate with greater than 50% relief (95% CI 52–66%). Only one study with only six patients studied comparative blocks with a success rate of 50% with greater than 50% relief, whereas with complete relief it was only 17%. It is of importance to note that Engel et al. [34] showed complete relief at the highest level of 61% and 70% at 95% CI at the upper end. However, they have not provided data on 50% success rate. Further, multiple lesions were performed, many of them with several passes, which essentially takes several hours to treat one patient.
Hurley et al. [31] in consensus practice guidelines on interventions for cervical facet joint pain concluded that cervical medial branch radiofrequency ablation may provide benefit to well-selected individuals, with medial branch blocks being more predictive than intraarticular injections. They also added that the most stringent selection criteria are likely to improve denervation outcomes, but at the expense of false negatives with an overall lower success rate.
Overall, the results show that radiofrequency neurotomy is effective in 54–76% with multiple passes providing multiple lesions taking several hours to perform a single lesion, whereas cervical facet joint nerve blocks with easy performance except that the relief is half that of radiofrequency neurotomy in duration with success rate ranging from 85% to 92% at 12-month follow-up, showing level II evidence with moderate strength of recommendation by the American Society of Interventional Pain Physicians (ASIPP) guidelines utilizing one RCT [30] and three observational studies [89,90,91].
Multiple guidelines and systematic reviews basically considered most of the studies included in the present systematic review and meta-analysis. Consequently, it is crucial to review the clinical characteristics of included randomized and observational studies.
Among the RCTs, van Eerd et al. [25] was the only trial assessing the efficacy and long-term effect of radiofrequency denervation in patients with clinically diagnosed cervical facet joint pain. They compared radiofrequency denervation plus an injection of bupivacaine with the injection of bupivacaine alone, with a sham radiofrequency neurotomy treatment in 76 patients. In this study, a single lesion was produced with a 5 cm needle with a 5 mm active tip. The results were positive in the intervention group showing 55.6% with greater than 30% pain decrease versus 51.3% in the control group with no significant difference. The Neck Disability Index was 15 ± 8.7% in the intervention group compared with 16.5 ± 7.2% in the local anesthetic group. However, the median time to end of the treatment success for patients in the radiofrequency group was 42 months compared to 12 months in the bupivacaine group with significant difference. This study illustrates the importance of local anesthetic alone blockade with significant improvement noted at 3 months, 6 months, and up to 1 year. This was described extensively by Manchikanti et al. [29, 30] in multiple studies with an average relief of 14–16 weeks. However, this study [25] is limited with assessment of 30% pain decrease instead of 50% or higher decrease in pain and improvement in function.
Lord et al. [33] performed the first RCT utilizing a sham control of percutaneous radiofrequency neurotomy producing multiple lesions in patients with chronic zygapophysial joint pain developing after whiplash injury. They studied 12 patients in each group (n = 24) with identification of the source of pain with the use of a double-blind, placebo-controlled, local anesthesia with 100% relief as the criterion standard. The results showed that the median time that elapsed before pain returned to at least 50% of the preoperative level was 263 days in the active treatment group and 8 days in the control group (p = 0.04). They also showed that at 27 weeks, seven patients (58%) in the active treatment group were free of pain. The technical details included use of a 10 cm, 22-gauge electrode with a 4 mm exposed tip introduced in two planes and producing 5–6 lesions to accommodate possible variation in the course of the nerve. The duration of the procedure has been described as 3 h per patient [71]. They also reported that six patients (50%) in the control group and 3 (25%) in the active treatment group had a return of their accustomed pain in the period immediately after the procedure. While major advantages of this trial include meticulous selection of the patients and meticulous technique, at the same time, multiple disadvantages include the small sample, even though justified by sample size calculations, long duration for operation time of 3 h per patient, and 5–6 lesions at each level, which is not a clinically reliable practice.
Stovner et al. [72] assessed radiofrequency denervation of facet joints at C2–C6 in cervicogenic headache in a randomized, double-blind, sham-controlled study, with randomization of six patients into each group. The treatment group received radiofrequency neurotomy with 3–4 lesions with a 50 mm, 22-gauge needle. They injected 1 mL of local anesthetic, then produced 3–4 lesions. Overall, two patients showed greater than 50% improvement in each group at 3 months. Multiple drawbacks in this study include the lack of inclusion criteria for diagnostic blocks, extremely small sample size, and producing 3–4 lesions.
Haspeslagh et al. [73] also evaluated the effectiveness of cervical radiofrequency lesioning in an RCT. The authors included 30 patients with cervicogenic headache according to the Sjaastad diagnostic criteria. They randomized 30 patients into two equal groups receiving either radiofrequency treatments with cervical facet joint denervation followed by cervical dorsal root ganglion lesions when necessary or injection of local anesthetic with steroid of the greater occipital nerve, followed by transcutaneous electrical nerve stimulation (TENS) when necessary. Group 1 with radiofrequency neurotomy and cervical dorsal root ganglion neurotomy preceded by local anesthetic injection showed improvement with reduction of the mean VAS of at least 2 points and/or global perceived effect of + 2 or + 3 with a success rate of 66.7% at 16 weeks, while the success rate was 53.3% in the local anesthetic and TENS group. Utilizing the same criteria, at 1-year follow-up, the authors found the improvement was 53.3% in group 1 and 46.7% in group 2. A large number of patients were withdrawn, or data was not available. Consequently, this was judged to be a negative trial.
Wallis et al. [71] evaluated the role of pain relief and radiofrequency neurotomy in the resolution of psychological distress of patients with whiplash, 3 months after the procedure. The study sample was derived from Lord et al.’s [33] radiofrequency study. Of the 24 patients in that study, they used 17 patients with a single painful cervical zygapophysial joint. All patients with complete pain relief exhibited resolution of their preoperative psychological distress, whereas all but one of the patients without pain relief remained unrelieved and continued to suffer from psychological distress.
Among the observational studies meeting inclusion criteria, Speldewinde [35] evaluated 151 patients undergoing cervical radiofrequency neurotomy. This is a single-author, single-practice data collection. The selection criterion was at least 80% pain relief following the controlled, comparative local anesthetic blocks. Outcome assessment was appropriate. Speldewinde assigned patients from 2001 to 2007 as cohort A and 2007 to 2009 as cohort B. There were 104 patients in cohort A and 47 in cohort B, with a total of 151 patients. The basis for the cohort was that a 22-gauge, 10 cm active tip was used during the earlier periods and that was then changed to an 18-gauge cannula. The conventional radiofrequency neurotomy was provided at 80 °C for 90 s in the early cohort with 18-gauge cannula at 80 °C for 60 s in the second cohort. Speldewinde also produced a minimum of three contiguous burns to each target nerve. Overall, Speldewinde reported significant improvement of greater than 50% in 76% of the patients with 79% of patients in cohort A and 85% of the patients in cohort B with the large needle and shortened radiofrequency neurotomy time. Successful patients were reported to have relief for more than 18 months, with an average duration of 27.5 months and a range of 18–68 months. The author also assessed psychological and functional status improvement which was significantly improved in patients with successful pain relief.
MacVicar et al. [36] studied a total of 104 patients selected from two separate practices. Inclusion criteria were based on complete relief of pain following controlled diagnostic medial branch blocks. They included strict outcome measures with successful outcome defined as complete pain relief of pain or at least 80% relief for at least 6 months, with complete restoration of activities of daily living, with no need for any further health care and return to work. They utilized a 16-gauge cannula with 10 cm active tip and produced at least three lesions at 80 °C and 85 °C for 90 s with the time to complete the operation of 2 h for a single facet joint and 1.5 h to complete the treatment of the third occipital nerve. Sixty-six percent of subjects met the treatment objective at 6 months. The authors have not reported any complications.
Sapir and Gorup [41] evaluated radiofrequency medial branch neurotomy in litigant and nonlitigant patients with cervical whiplash. The inclusion criteria were based on at least 80% pain relief following diagnostic medial branch blocks. Overall, 50 patients met the inclusion criteria, and 46 patients completed the study. A total of 32 litigants and 18 nonlitigants were included. The overall reductions in cervical whiplash symptoms and VAS pain scores were significant, both immediately after the treatment and after 1-year follow-up. The improvement was better after 1 year post treatment with NRS scores with nonlitigants vs. litigants of 2.5 vs. 3.6. The authors postulated that the difference between litigants and nonlitigants in the degree of symptomatology is response to treatment; however, it did not reach significance. Thirteen of the 32 litigant patients settled their case after the treatments. However, they also had pain recur 1 year after the treatment. Overall, 21 patients reported recurrence of pain within 1 year. Time to recurrence defined as 50% return of pain was 8 ± 2 months.
Among other observational studies, Shin et al. [39] studied 28 patients with conventional radiofrequency neurotomy reporting improvement in 68% of patients. Barnsley [38] assessed the role of percutaneous radiofrequency neurotomy for chronic neck pain with evaluation of outcomes in a series of consecutive patients. The results showed 36 of 45 assessable procedures (80%) achieved significant pain relief with 36 weeks of mean relief; 74% of the patients achieved 100% pain relief. Only one serious adverse event with local infection was reported.
In a recent comparative effectiveness study [44] clinical outcomes and cost utility of therapeutic medial branch blocks with radiofrequency neurotomy in managing chronic neck pain of facet joint origin were published. In this study with the main outcome being NRS, significant improvement was defined as at least 50% improvement in pain relief. In this study, 132 patients receiving cervical medial branch blocks and 163 patients with cervical radiofrequency neurotomy were included. One hundred and seven patients in the cervical medial branch group and 105 patients in the radiofrequency group completed 1-year follow-up.
The maximum number of procedures in the medial branch blocks was four per year, whereas that in the radiofrequency neurotomy group was two per year administered at 3 or 6 months, if medically needed with adequate relief of 3 or 6 months with each procedure. The results showed significant improvement reported in100%, 94%, and 81% of the patients in the medial branch blocks group compared to 100%, 69%, and 64% in the radiofrequency neurotomy group at 3, 6, and 12-month follow-up, respectively, with significant differences noted at 6 and 12 months. They also performed cost utility analysis showing an average cost per quality-adjusted life-year (QALY) of $4994 for cervical medial branch blocks compared to $5364 for cervical radiofrequency neurotomy. Interestingly, in this study, 6 of 132 patients (or 5%) in the cervical medial branch group and 53 of 163 (or 33%) of the patients in the cervical radiofrequency neurotomy group were converted to other treatments, either because of side effects (6 patients or 4%) or inadequate relief (47 patients or 29%).
Among the remaining studies meeting the inclusion criteria, four of them studied headache [40, 77, 86, 87] whereas one study included patients with headache as well as neck pain [42]. Two studies from the same group of authors involving the same data focused on modulation of facet joint nociception and reduction of psychological features in individuals with chronic whiplash syndrome in a prospective assessment [75, 76].
Facet joint interventions showed an overall 2.9% annual increase from 2010 to 2019 compared to annual increases of 14.2% from 2000 to 2010, with 19.3% COVID-19 pandemic-related decline from 2019 to 2020. In addition, the analysis of expenditures for facet joint interventions in the Medicare population [58] also showed an increase in expenditures of 79% from 2009 to 2018 in the form of total cost for facet joint interventions. Inflation-adjusted costs with 2018 US dollars, however, showed an overall increase of 53% instead of 79% with an annual increase of 4.9%. Further, cervical facet joint injection procedures increased by 2% annually from 2010 to 2019, whereas cervical radiofrequency neurotomy procedures increased by 8.9%. In comparison, lumbosacral facet joint blocks increased at an annual rate of 0.8% from 2010 to 2019, whereas radiofrequency neurotomy procedures during the same period increased 7.4%. During the COVID-19 pandemic overall facet joint interventions decreased 19.3%, with cervical/thoracic facet joint blocks decreasing 20.2%, lumbar/sacral facet joint blocks decreasing 20.7%, with cervical/thoracic facet neurolysis decreasing 14.1%, and lumbosacral facet neurolysis procedures decreasing 7.3% [59]. In contrast, epidural procedures showed an overall decrease of inflation-adjusted costs of 2%, whereas prior to inflation adjustment, total expenditures increased by 14.6%, an annual increase of 1.5% [54]. Spinal cord stimulation procedures also increased in utilization and costs; however, utilization of percutaneous adhesiolysis procedures and vertebral augmentation procedures have declined significantly [55, 57]. In addition, recent evaluations assessing the impact of the COVID-19 pandemic showed a 18.7% reduction in overall interventional techniques from 2019 to 2020 [59].
With changes in policies in the USA and emerging guidelines, it is conceivable that radiofrequency neurotomy will increase much faster while intraarticular injections and medial branch blocks will continue to decline [92, 93]. As with very few systematic reviews available on this cervical radiofrequency neurotomy procedure and multiple other systematic reviews and meta-analysis, the value and validity of this publication is only as reliable as the validity of the primary studies included. As described earlier, the majority of the studies in this systematic review and meta-analysis are observational studies with a single high-quality RCT [33] with a small number of patients (12 in sham, 12 in intervention), the remaining were observational studies. Consequently, numerous issues have been highlighted in reference to systematic reviews in interventional pain management. These have been discussed in guidelines and multiple other systematic reviews extensively [3, 5, 26,27,28, 31, 32, 34, 94,95,96,97,98,99,100,101,102,103]. Significant discussions continue with descriptions of placebo and inappropriately converted placebo analysis of active control trials. Manchikanti et al. [98] have shown sodium chloride solution injected into the epidural space is not a placebo. Similarly, it has been widely publicized that epidural injection of local anesthetic is an active agent with only short-term differences in improvement with local anesthetic alone compared to local anesthetic with steroids [26,27,28]. Ironically, in contrast to numerous descriptions, the manuscripts included in this analysis showed similar improvement with local anesthetic injection compared to radiofrequency neurotomy, however, requiring early repeat injections similar to a short-acting compared to a long-acting drug or any other technique. It is also crucial that real-world evidence be applied in analysis of the evidence with higher clinical relevancy. The majority of the trials and studies included in this analysis showed only moderate clinical relevance due to extensive lesioning and time-consuming techniques. Dal-Ré et al. [69] discussed the issues related to real-world evidence focusing on pragmatic RCTs in contrast to explanatory RCTs, which are used to test hypotheses on whether the intervention causes an outcome of interest in ideal circumstances; pragmatic RCTs aim to provide information on the relative merits of real-world clinical alternatives in routine care. A critical aim of an explanatory RCT is to ensure internal validity (prevention of bias), in contrast to a pragmatic RCT which focuses on maximizing external validity (generalizability of the results to many real-world settings), preserving internal validity as much as possible. Dal-Ré et al. also noted that a genuinely pragmatic RCT should fulfill at least two fundamental features, including conduct of the study resembling usual clinical practice and the results being applicable clinically to multiple other settings.
It is crucial in interventional pain management to identify real-world trials with high clinical applicability. This is the first systematic review comparing cervical radiofrequency in assessing cervical radiofrequency neurotomy utilizing a single-arm meta-analysis. Single-arm meta-analysis essentially showed significant improvement with conventional radiofrequency neurotomy. Even though not well appreciated, single-arm analysis should be made a crucial part of meta-analysis in elucidating the effectiveness of both groups and real-world RCTs.
Conclusion
This systematic review provided level II evidence for the short-term and long-term effectiveness of radiofrequency neurotomy in managing neck pain with a diagnosis of facet joint pain with dual control diagnostic blocks with at least 80% criterion standard for diagnosis. However, the evidence is level III–IV for radiofrequency neurotomy in managing headaches. Further, the literature is extremely scant in assessing efficacy or effectiveness of radiofrequency neurotomy in the cervical spine with extremely small sample sizes.
References
U.S. Burden of Disease Collaborators. The state of US health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. https://doi.org/10.1001/jama.2013.13805.
Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol. 2010;24(6):783–92. https://doi.org/10.1016/j.berh.2011.01.019.
Manchikanti L, Kaye AD, Soin A, et al. Comprehensive evidence-based guidelines for facet joint interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2020;23(3S):S1-127.
Navani A, Manchikanti L, Albers SL, et al. Responsible, safe, and effective use of biologics in the management of low back pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2019;22(1S):S1-74.
Manchikanti L, Knezevic NN, Navani A, et al. Epidural interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) comprehensive evidence-based guidelines. Pain Physician. 2021;24(S1):S27–208.
Manchikanti L, Centeno CJ, Atluri S, et al. Bone marrow concentrate (BMC) therapy in musculoskeletal disorders: evidence-based policy position statement of American Society of Interventional Pain Physicians (ASIPP). Pain Physician. 2020;23(2):E85-131.
Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996–2013. JAMA. 2016;316(24):2627–46. https://doi.org/10.1001/jama.2016.16885.PMID:28027366.
Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863–84. https://doi.org/10.1001/jama.2020.0734.PMID:32125402.
Bogduk N, Marsland A. The cervical zygapophysial joints as a source of neck pain. Spine (Phila Pa 1976). 1988;13(6):610–17.
Manchikanti L, Kosanovic R, Cash KA, et al. Assessment of prevalence of cervical facet joint pain with diagnostic cervical medial branch blocks: analysis based on chronic pain model. Pain Physician. 2020;23(6):531–40.
Barnsley L, Lord S, Bogduk N. Comparative local anaesthetic blocks in the diagnosis of cervical zygapophysial joint pain. Pain. 1993;55(1):99–106. https://doi.org/10.1016/0304-3959(93)90189-V.
Yin W, Bogduk N. The nature of neck pain in a private pain clinic in the United States. Pain Med. 2008;9(2):196–203. https://doi.org/10.1111/j.1526-4637.2007.00369.x.
Speldewinde G, Bashford G, Davidson I. Diagnostic cervical zygapophyseal joint blocks for chronic cervical pain. Med J Aust. 2001;174(4):174–6. https://doi.org/10.5694/j.1326-5377.2001.tb143210.x.
Barnsley L, Lord SM, Wallis BJ, Bogduk N. The prevalence of chronic cervical zygapophyseal joint pain after whiplash. Spine (Phila Pa 1976). 1995;20(1):20–6. https://doi.org/10.1097/00007632-199501000-00004.
Lord SM, Barnsley L, Wallis BJ, Bogduk N. Chronic cervical zygapophysial joint pain with whiplash: a placebo-controlled prevalence study. Spine (Phila Pa 1976). 1996;21(15):1737–44. https://doi.org/10.1097/00007632-199608010-00005.
Barnsley L, Lord S, Wallis B, Bogduk N. False-positive rates of cervical zygapophysial joint blocks. Clin J Pain. 1993;9(2):124–30. https://doi.org/10.1097/00002508-199306000-00007.
Persson M, Sörensen J, Gerdle B. Chronic Whiplash Associated Disorders (WAD): responses to nerve blocks of cervical zygapophyseal joints. Pain Med. 2016;17(12):2162–75. https://doi.org/10.1093/pm/pnw036.
Manchukonda R, Manchikanti KN, Cash KA, Pampati V, Manchikanti L. Facet joint pain in chronic spinal pain: an evaluation of prevalence and false positive rate of diagnostic blocks. J Spinal Disord Tech. 2007;20(7):539–45. https://doi.org/10.1097/BSD.0b013e3180577812.
Manchikanti L, Singh V, Rivera J, Pampati V. Prevalence of cervical facet joint pain in chronic neck pain. Pain Physician. 2002;5(3):243–9.
Manchikanti L, Boswell MV, Singh V, Pampati V, Damron KS, Beyer CD. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic, and lumbar regions. BMC Musculoskelet Disord. 2004;5:15. https://doi.org/10.1186/1471-2474-5-15.
Manchikanti L, Kaye AD, Boswell MV, et al. A systematic review and best evidence synthesis of the effectiveness of therapeutic facet joint interventions in managing chronic spinal pain. Pain Physician. 2015;18(4):E535–82.
Manchikanti L, Hirsch JA, Kaye AD, Boswell MV. Cervical zygapophysial (facet) joint pain: effectiveness of interventional management strategies. Postgrad Med. 2016;128(1):54–68. https://doi.org/10.1080/00325481.2016.1105092.
MacVicar J, MacVicar AM, Bogduk N. The prevalence of “pure” lumbar zygapophysial joint pain in patients with chronic low back pain. Pain Med. 2021;22(1):41–4. https://doi.org/10.1093/pm/pnaa383.
Manchikanti L, Kosanovic R, Pampati V, et al. Low back pain and diagnostic lumbar facet joint nerve blocks: assessment of prevalence, false-positive rates, and a philosophical paradigm shift from an acute to a chronic pain model. Pain Physician. 2020;23(5):519–30.
van Eerd M, de Meij N, Kessels A. Efficacy and long-term effect of radiofrequency denervation in patients with clinically diagnosed cervical facet joint pain: a double-blind randomized controlled trial. Spine (Phila Pa 1976). 2021;46(5):285–93. https://doi.org/10.1097/BRS.0000000000003799.
Knezevic NN, Manchikanti L, Urits I, et al. Lack of superiority of epidural injections with lidocaine with steroids compared to without steroids in spinal pain: a systematic review and meta-analysis. Pain Physician. 2020;23(4S):S239–70.
Manchikanti L, Kosanovic R, Vanaparthy R, et al. Steroid distancing in interventional pain management during COVID-19 and beyond: safe, effective and practical approach. Pain Physician. 2020;23(4S):S319–50.
Shanthanna H, Busse J, Wang L, et al. Addition of corticosteroids to local anaesthetics for chronic non-cancer pain injections: a systematic review and meta-analysis of randomised controlled trials. Br J Anaesth. 2020;125(5):779–801. https://doi.org/10.1016/j.bja.2020.06.062.
Manchikanti L, Singh V, Falco FJE, Cash KA, Fellows B. Cervical medial branch blocks for chronic cervical facet joint pain: a randomized double-blind, controlled trial with one-year follow-up. Spine (Phila Pa 1976). 2008;33(17):1813–20. https://doi.org/10.1097/BRS.0b013e31817b8f88.
Manchikanti L, Singh V, Falco FJE, Cash KA, Fellows B. Comparative outcomes of a 2-year follow-up of cervical medial branch blocks in management of chronic neck pain: a randomized, double-blind controlled trial. Pain Physician. 2010;13(5):437–50.
Hurley RW, Adams MCB, Barad M, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Reg Anesth Pain Med. 2022;47(1):3–59. https://doi.org/10.1136/rapm-2021-103031.
Geurts JW, van Wijk RM, Stolker RJ, Groen GJ. Efficacy of radiofrequency procedures for the treatment of spinal pain: a systematic review of randomized clinical trials. Reg Anesth Pain Med. 2001;26(5):394–400. https://doi.org/10.1053/rapm.2001.23673.
Lord S, Barnsley L, Wallis B, McDonald G, Bogduk N. Percutaneous radiofrequency neurotomy for chronic cervical zygapophyseal-joint pain. N Engl J Med. 1996;335(23):1721–6. https://doi.org/10.1056/NEJM199612053352302.
Engel A, King W, Schneider BJ, Duszynski B, Bogduk N. The effectiveness of cervical medial branch thermal radiofrequency neurotomy stratified by selection criteria: a systematic review of the literature. Pain Med. 2020;21(11):2726–37. https://doi.org/10.1093/pm/pnaa219.
Speldewinde GC. Outcomes of percutaneous zygapophysial and sacroiliac joint neurotomy in a community setting. Pain Med. 2011;12(2):209–18. https://doi.org/10.1111/j.1526-4637.2010.01022.x.
MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Cervical medial branch radiofrequency neurotomy in New Zealand. Pain Med. 2012;13(5):647–54. https://doi.org/10.1111/j.1526-4637.2012.01351.x.
McDonald GJ, Lord SM, Bogduk N. Long-term follow-up of patients treated with cervical radiofrequency neurotomy for chronic neck pain. Neurosurgery. 1999;45(1):61–7. https://doi.org/10.1097/00006123-199907000-00015.
Barnsley L. Percutaneous radiofrequency neurotomy for chronic neck pain: outcomes in a series of consecutive patients. Pain Med. 2005;6(4):282–6. https://doi.org/10.1111/j.1526-4637.2005.00047.x.
Shin WR, Kim HI, Shin DG, Shin DA. Radiofrequency neurotomy of cervical medial branches for chronic cervicobrachialgia. J Korean Med Sci. 2006;21(1):119–25. https://doi.org/10.3346/jkms.2006.21.1.119.
Park SW, Park YS, Nam TK, Cho TG. The effect of radiofrequency neurotomy of lower cervical medial branches on cervicogenic headache. J Korean Neurosurg Soc. 2011;50(6):507–11. https://doi.org/10.3340/jkns.2011.50.6.507.
Sapir DA, Gorup JM. Radiofrequency medial branch neurotomy in litigant and non-litigant patients with cervical whiplash. Spine (Phila Pa 1976). 2001;26(12):E268–73. https://doi.org/10.1097/00007632-200106150-00016.
Lord SM, Barnsley L, Bogduk N. Percutaneous radiofrequency neurotomy in the treatment of cervical zygapophysial joint pain: a caution. Neurosurgery. 1995;36(4):732–9. https://doi.org/10.1227/00006123-199504000-00014.
Lee DW, Pritzlaff S, Jung MJ, et al. Latest evidence-based application for radiofrequency neurotomy (LEARN): best practice guidelines from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2021;14:2807–31. https://doi.org/10.2147/JPR.S325665.
Manchikanti L, Pampati V, Sanapati MR, et al. Outcomes of cervical therapeutic medial branch blocks and radiofrequency neurotomy: clinical outcomes and cost utility are equivalent. Pain Physician. 2022;25(1):35–47.
Manchikanti L, Vanaparthy R, Atluri S, Sachdeva H, Kaye AD, Hirsch JA. COVID-19 and the opioid epidemic: two public health emergencies that intersect with chronic pain. Pain Ther. 2021;10(1):269–86. https://doi.org/10.1007/s40122-021-00243-2.
Manchikanti L, Singh V, Kaye AD, Hirsch JA. Lessons for better pain management in the future: learning from the past. Pain Ther. 2020;9(2):373–91. https://doi.org/10.1007/s40122-020-00170-8.
Shah S, Diwan S, Soin A, et al. Evidence-based risk mitigation and stratification during COVID-19 for return to interventional pain practice: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2020;23(4S):S161–82.
Gharibo C, Sharma A, Soin A, et al. Triaging interventional pain procedures during COVID-19 or related elective surgery restrictions: evidence-informed guidance from the American Society of Interventional Pain Physicians (ASIPP). Pain Physician. 2020;23(4S):S183-204.
Stone S, Malanga GA, Capella T. Corticosteroids: review of the history, the effectiveness, and adverse effects in the treatment of joint pain. Pain Physician. 2021;24(S1):S233–46.
Manchikanti L, Singh VM, Staats PS, et al. Fourth wave of opioid (illicit drug) overdose deaths and diminishing access to prescription opioids and interventional techniques: cause and effect. Pain Physician. 2022;25(2):97–124.
Hartman M, Martin AB, Washington B, Catlin A, The National Health Expenditure Accounts Team. National Health Care Spending In 2020: growth driven by federal spending in response to the COVID-19 pandemic. Health Aff (Millwood). 2022;41(1):13–25. https://doi.org/10.1377/hlthaff.2021.01763.
Furukawa MF, Kimmey L, Jones DJ, Machta RM, Guo J, Rich EC. Consolidation of providers into health systems increased substantially, 2016–18. Health Aff (Millwood). 2020;39(8):1321–1325.
Manchikanti L, Sanapati MR, Pampati V, et al. Update of utilization patterns of facet joint interventions in managing spinal pain from 2000 to 2018 in the US fee-for-service Medicare population. Pain Physician. 2020;23(2):E133–49.
Manchikanti L, Pampati V, Soin A, Sanapati MR, Kaye AD, Hirsch JA. Declining utilization and inflation-adjusted expenditures for epidural procedures in chronic spinal pain in the Medicare population. Pain Physician. 2021;24:1–15.
Manchikanti L, Pampati V, Vangala BP, et al. Spinal cord stimulation trends of utilization and expenditures in fee-for-service (FFS) Medicare population from 2009 to 2018. Pain Physician. 2021;24(1):293–308.
Manchikanti L, Manchikanti MV, Vanaparthy R, Kosanovic R, Pampati V. Utilization patterns of sacroiliac joint injections from 2000 to 2018 in fee-for-service Medicare population. Pain Physician. 2020;23(5):439–50.
Manchikanti L, Kosanovic R, Pampati V, Kaye AD. Declining utilization patterns of percutaneous adhesiolysis procedures in the fee-for-service (FFS) Medicare population. Pain Physician. 2021;24(1):17–29.
Manchikanti L, Pampati V, Soin A, et al. Trends of expenditures and utilization of facet joint interventions in fee-for-service (FFS) Medicare population from 2009–2018. Pain Physician. 2020;23(3S):S129–47.
Manchikanti L, Pampati V, Sanapati MR, et al. COVID-19 pandemic reduced utilization of interventional techniques 18.7% in managing chronic pain in the Medicare population in 2020: analysis of utilization data from 2000 to 2020. Pain Physician. 2022;25(3):223–238.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; Mar 29;372:n71. https://doi.org/10.1136/bmj.n71.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65-94. https://doi.org/10.7326/0003-4819-151-4-200908180-00136.
Manchikanti L, Atluri S, Boswell MV, et al. Methodology for evidence synthesis and development of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Pain Physician. 2021;24(S1):S1–26.
Janapala RN, Manchikanti L, Sanapati MR, et al. Efficacy of radiofrequency neurotomy in chronic low back pain: a systematic review and meta-analysis. J Pain Res. 2021;14:2589–91. https://doi.org/10.2147/JPR.S323362.
Furlan AD, Malmivaara A, Chou R, et al. 2015 updated method guideline for systematic reviews in the Cochrane back and neck group. Spine (Phila Pa 1976). 2015;40(21):1660–73. https://doi.org/10.1097/BRS.0000000000001061.
Manchikanti L, Hirsch JA, Cohen SP, et al. Assessment of methodologic quality of randomized trials of interventional techniques: development of an interventional pain management specific instrument. Pain Physician. 2014;17(3):E263–90.
Manchikanti L, Hirsch JA, Heavner JE, et al. Development of an interventional pain management specific instrument for methodologic quality assessment of non-randomized studies of interventional techniques. Pain Physician. 2014;17(3):E291-317.
Manchikanti L, Falco FJE, Benyamin RM, Kaye AD, Boswell MV, Hirsch JA. A modified approach to grading of evidence. Pain Physician. 2014;17(3):E319–25.
Ryan R, Hill S. How to GRADE the quality of the evidence. Version 3.0. 2016. http://cccrg.cochrane.org/author-resources. Accessed 12 Feb 2021.
Dal-Ré R, Janiaud P, Ioannidis JPA. Real-world evidence: How pragmatic are randomized controlled trials labeled as pragmatic? BMC Med. 2018;16(1):49. https://doi.org/10.1186/s12916-018-1038-2.
van Eerd M, de Meij N, Dortangs E, et al. Long-term follow-up of cervical facet medial branch radiofrequency treatment with the single posterior-lateral approach: an exploratory study. Pain Pract. 2014(1);14:8–15. https://doi.org/10.1111/papr.12043.
Wallis BJ, Lord SM, Bogduk N. Resolution of psychological distress of whiplash patients following treatment by radiofrequency neurotomy: a randomised, double-blind, placebo-controlled trial. Pain. 1997;73(1):15–22. https://doi.org/10.1016/s0304-3959(97)00060-2.
Stovner LJ, Kolstad F, Helde G. Radiofrequency denervation of facet joints C2–C6 in cervicogenic headache: a randomized, double-blind, sham-controlled study. Cephalalgia. 2004;24(10):821–30. https://doi.org/10.1111/j.1468-2982.2004.00773.x.
Haspeslagh SR, Van Suijlekom HA, Lamé IE, Kessels AG, van Kleef M, Weber WE. Randomised controlled trial of cervical radiofrequency lesions as a treatment for cervicogenic headache [ISRCTN07444684]. BMC Anesthesiol. 2006;6:1. https://doi.org/10.1186/1471-2253-6-1.PMID:16483374.
Burnham T, Conger A, Salazar F, et al. The effectiveness of cervical medial branch radiofrequency ablation for chronic facet joint syndrome in patients selected by a practical medial branch block paradigm. Pain Med. 2020;21(10):2071–6. https://doi.org/10.1093/pm/pnz358.
Smith AD, Jull G, Schneider GM, Frizzell B, Hooper RA, Sterling M. Modulation of cervical facet joint nociception and pain attenuates physical and psychological features of chronic whiplash: a prospective study. PM R. 2015;7(9):913–21. https://doi.org/10.1016/j.pmrj.2015.03.014.
Smith AD, Jull G, Schneider G, et al. Cervical radiofrequency neurotomy reduces psychological features in individuals with chronic whiplash symptoms. Pain Physician. 2014;17(3):265–74.
Lee JB, Park JY, Park J, Lim DJ, Kim SD, Chung HS. Clinical efficacy of radiofrequency cervical zygapophyseal neurotomy in patients with chronic cervicogenic headache. J Korean Med Sci. 2007;22(2):326–9. https://doi.org/10.3346/jkms.2007.22.2.326.PMID:17449944.
van Suijlekom HA, van Kleef M, Barendse GA, Sluijter ME, Sjaastad O, Weber WE. Radiofrequency cervical zygapophyseal joint neurotomy for cervicogenic headache: a prospective study of 15 patients. Funct Neurol. 1998;13(4):297–303.
Palea O, Andar HM, Lugo R, Granville M, Jacobson RE. Direct posterior bipolar cervical facet radiofrequency rhizotomy: a simpler and safer approach to denervate the facet capsule. Cureus. 2018;10(3):e2322. https://doi.org/10.7759/cureus.2322.
Khan M, Meleka S. CT guided cervical medial branch block and radiofrequency ablation. J Clin Neurosci. 2020;78:393–6. https://doi.org/10.1016/j.jocn.2020.05.009.
LaGrew J, Balduyeu P, Vasilopoulos T, Kumar S. Incidence of cervicogenic headache following lower cervical radiofrequency neurotomy. Pain Physician. 2019;22:E127–32.
Hanna R, Abd-Elsayed A. Review of the safety of bipolar radiofrequency ablation in patients with chronic pain with implantable cardiac rhythm management devices. Pain Physician. 2021;24(2):E169–76.
Ellwood S, Shupper P, Kaufman A. A retrospective review of spinal radiofrequency neurotomy procedures in patients with metallic posterior spinal instrumentation—is it safe? Pain Physician. 2018;21(5):E477–82.
Van de Perck F, Soetens F, Lebrun C, Lataster A, Verhamme A, Van Zundert J. Phrenic nerve injury after radiofrequency denervation of the cervical medial branches. Pain Pract. 2016;16(2):E42–5. https://doi.org/10.1111/papr.12398.
Miller A, Griepp D, Rahme R. Beware the wandering needle: inadvertent intramedullary injection during an attempted cervical medial branch block. World Neurosurg. 2021;149:169–70. https://doi.org/10.1016/j.wneu.2021.02.107.
Hamer JF, Purath TA. Response of cervicogenic headaches and occipital neuralgia to radiofrequency ablation of the C2 dorsal root ganglion and/or third occipital nerve. Headache. 2014;54(3):500–10. https://doi.org/10.1111/head.12295.
Govind J, King W, Bailey B, Bogduk N. Radiofrequency neurotomy for the treatment of third occipital headache. J Neurol Neurosurg Psychiatry. 2003;74(1):88–93. https://doi.org/10.1136/jnnp.74.1.88.
Lang JK, Buchfelder M. Radiofrequency neurotomy for headache stemming from the zygapophysial joints C2/3 and C3/4. Cent Eur Neurosurg. 2010;71(2):75–9. https://doi.org/10.1055/s-0029-1224159.
Manchikanti L, Manchikanti K, Damron K, Pampati V. Effectiveness of cervical medial branch blocks in chronic neck pain: a prospective outcome study. Pain Physician. 2004;7(2):195–201.
Hahn T, Halatsch ME, Wirtz C, Klessinger S. Response to cervical medial branch blocks in patients with cervicogenic vertigo. Pain Physician. 2018;21(3):285–94.
Lee DW, Huston C. Fluoroscopically guided cervical zygapophyseal therapeutic joint injections may reduce the need for radiofrequency. Pain Physician. 2018;21(6):E661–5.
CGS Administrators, LLC. 2021. Local coverage determination (LCD). Facet joint interventions for pain management (L38773). Original effective date May 2,2021.
Noridian Healthcare Solutions, LLC. 2021. Local coverage determination (LCD). Facet joint interventions for pain management (L38801). Original effective date April 25, 2021.
Chou R, Hashimoto R, Friedly JL, et al. Epidural corticosteroid injections for radiculopathy and spinal stenosis: a systematic review and meta-analysis. Ann Intern Med. 2015;163(5):373–81. https://doi.org/10.7326/M15-0934.
Manchikanti L, Knezevic NN, Boswell MV, Kaye AD, Hirsch JA. Epidural injections for lumbar radiculopathy and spinal stenosis: a comparative systematic review and meta-analysis. Pain Physician. 2016;19(3):E365-410.
Manchikanti L, Knezevic E, Knezevic NN, et al. Epidural injections for lumbar radiculopathy or sciatica: a comparative systematic review and meta-analysis of Cochrane review. Pain Physician. 2021;24(5):E539–54.
Manchikanti L, Knezevic E, Knezevic NN, et al. A comparative systematic review and meta-analysis of 3 routes of administration of epidural injections in lumbar disc herniation. Pain Physician. 2021;24(6):425–40.
Manchikanti L, Knezevic NN, Sanapati J, Kaye AD, Sanapati MR, Hirsch JA. Is epidural injection of sodium chloride solution a true placebo or an active control agent? A systematic review and meta-analysis. Pain Physician. 2021;24(1):41–59.
Manchikanti L, Knezevic NN, Parr A, Kaye AD, Sanapati M, Hirsch JA. Does epidural bupivacaine with or without steroids provide long-term relief? A systematic review and meta-analysis. Curr Pain Headache Rep. 2020;24(6):26. https://doi.org/10.1007/s11916-020-00859-7.
Cho PG, Ji GY, Yoon YS, Shin DA. Clinical effectiveness of percutaneous epidural neuroplasty according to the type of single-level lumbar disc herniation: a 12-month follow-up study. J Korean Neurosurg Soc. 2019;62(6):681–90. https://doi.org/10.3340/jkns.2019.0070.
Manchikanti L, Knezevic NN, Sanapati SP, Sanapati MR, Kaye AD, Hirsch JA. Is percutaneous adhesiolysis effective in managing chronic low back and lower extremity pain in post-surgery syndrome: a systematic review and meta-analysis. Curr Pain Headache Rep. 2020;24(6):30. https://doi.org/10.1007/s11916-020-00862-y.
Manchikanti L, Knezevic NN, Sanapati MR, Boswell MV, Kaye AD, Hirsch JA. Effectiveness of percutaneous adhesiolysis in managing chronic central lumbar spinal stenosis: a systematic review and meta-analysis. Pain Physician. 2019;22(6):E523–50.
Manchikanti L, Soin A, Boswell MV, Kaye AD, Sanapati M, Hirsch JA. Effectiveness of percutaneous adhesiolysis in post lumbar surgery syndrome: a systematic analysis of findings of systematic reviews. Pain Physician. 2019;22(4):307–22.
Acknowledgements
The authors wish to thank Bert Fellows, MA, Director Emeritus of Psychological Services at Pain Management Centers of America, for manuscript review, and Tonie M. Hatton and Diane E. Neihoff, transcriptionists, for their assistance in preparation of this manuscript.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Laxmaiah Manchikanti, MD, Nebojsa Nick Knezevic, MD, PhD, Mahendra R. Sanapati, MD, and Emilija Knezevic. The first draft of the manuscript was written by Laxmaiah Manchikanti, MD, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Amol Soin is the founder and CEO of Soin Neuroscience, which is developing a spinal cord stimulator to treat spinal pain and has a patent for Soin Neuroscience, Jan One, and Avanos and a patent pending for Soin Therapeutics. Annu Navani is a consultant for Cornerloc, Scilex Pharmaceuticals and founder and CEO of WorCflo. Thomas Simopoulos is a consultant for Nevro, Boston Scientific and Spectra Medical. Alaa Abd-Elsayed is a consultant of Medtronic, Avanos, Abott, Sprint, and Averitas. Joshua Hirsch is a consultant for Medtronic and Senior Affiliate Research Fellow at the Neiman Policy Institute. Laxmaiah Manchikanti, Nebojsa Nick Knezevic, Emilija Knezevic, Salahadin Abdi, Mahendra R. Sanapati, Bradley W. Wargo, Sairam Atluri, Christopher G. Gharibo Radomir Kosanovic, and Alan D. Kaye have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Manchikanti, L., Knezevic, N.N., Knezevic, E. et al. A Systematic Review and Meta-analysis of the Effectiveness of Radiofrequency Neurotomy in Managing Chronic Neck Pain. Pain Ther 12, 19–66 (2023). https://doi.org/10.1007/s40122-022-00455-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00455-0