Abstract
Introduction
Opioid use disorder is a global problem. Although opioid analgesics are prescribed less frequently in Japan than in many other countries, the rate of aberrant prescription opioid-taking behaviors in Japan is unknown.
Methods
An internet survey was conducted to estimate the prevalence of and risk factors for prescription opioid misuse, abuse, diversion and doctor shopping in Japanese subjects with chronic pain who had been prescribed opioid analgesics.
Results
The proportion of respondents (n = 387) who reported opioid misuse was 45.5% (95% confidence interval [CI]: 40.4–50.6); rates were: 24.6% (95% CI: 20.3–29.2) for abuse; 15.0% (95% CI: 11.6–19.0) for diversion; and 10.6% (95% CI: 7.7–14.1) for doctor shopping. Aberrant prescription opioid-taking behaviors were higher in participants with chronic post-cancer treatment pain (misuse, 64.2%; abuse, 52.2%) or chronic cancer pain (misuse, 57.4%; abuse, 26.2%) than in those with chronic noncancer pain (misuse, 37.8%; abuse, 17.0%). Younger age, male sex, smoking, habitual drinking, diagnosis of psychiatric disease, use of opioids other than tramadol, and use of opioids for chronic post-cancer treatment pain and chronic cancer pain were identified as risk factors for aberrant prescription opioid-taking behaviors.
Conclusion
Even in Japan, which has not experienced the surge in opioid consumption documented in other countries, aberrant prescription opioid-taking behaviors were observed. When prescribing opioid analgesics, universal precautions should always be taken for both cancer and non-cancer patients.
Trial Registration
UMIN000041788.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
To our knowledge, no studies have investigated the level of aberrant prescription opioid-taking behaviors in Japan. |
Based on our hypothesis that misuse, abuse, diversion, and doctor shopping of prescription opioids also occur in Japan, we conducted an internet survey to investigate the prevalence of and risk factors for these aberrant prescription opioid-taking behaviors. |
The survey involved 387 Japanese subjects who had been prescribed opioid analgesics for chronic cancer pain, chronic post-cancer treatment pain, or chronic noncancer pain. |
Aberrant prescription opioid-taking behaviors were highest in participants with chronic post-cancer treatment pain (misuse, 64.2%; abuse, 52.2%) or chronic cancer pain (misuse, 57.4%; abuse, 26.2%). |
Risk factors for aberrant prescription opioid-taking behaviors were younger age, male sex, smoking, habitual drinking, diagnosis of psychiatric disease, use of opioids other than tramadol, and use of opioids for chronic post-cancer treatment pain and chronic cancer pain. |
To prevent opioid use disorder or opioid overdose in Japan, universal precautions for opioid use should be followed not only for patients with chronic noncancer pain but also for patients with cancer pain or pain related to cancer treatment. |
Introduction
Opioid analgesics are considered essential treatment for moderate to severe cancer pain [1, 2]. However, cancer pain remains undertreated even in developed countries, highlighting the need for early pain assessment and treatment [3]. On the other hand, since the late 1990s, opioid analgesics have been widely prescribed for noncancer pain [4]. As the number of opioid prescriptions increased, misuse and diversion became widespread, leading to an increase in addiction and overdose [4, 5]. Opioid dependence is now a global problem. The “Global Burden of Diseases, Injuries, and Risk Factors Study” estimated that, in 2017, 40.5 million people had opioid dependence and nearly 110,000 people died from opioid overdose [6]. The challenge for healthcare providers is to recognize and prevent problematic use of prescription opioids without restricting access to patients in need (e.g., cancer pain patients) [2, 7, 8].
A systematic review of studies conducted in the US and other western countries involving patients with chronic noncancer pain reported widely varying opioid misuse rates ranging from 2.0 to 56.3%, even when the analysis was limited to high-quality studies. The integrated average misuse rate was estimated to be between 21 and 29% [9]. The misuse rate of oral tramadol in the US, a Schedule IV opioid, as estimated from the National Survey of Drug Use and Health using self-reported questionnaires, was 4–5% of total prescriptions, and that of Schedule II opioids (morphine, oxycodone, and hydrocodone) was 6–9% [10].
In Japan, opioid analgesics are strictly regulated by the ‘Narcotics and Psychotropics Control Act’ [11]. Moreover, because Japanese physicians have lower opioid prescribing practices for both acute and chronic noncancer pain than US physicians [12, 13], Japan has not experienced the dramatic increase in opioid consumption documented in other countries [14]. Many Japanese physicians thus consider misuse or abuse of opioid analgesics in Japan to be rare [15]. However, in view of increasingly prolonged cancer survival which may lead to long-term opioid therapy, surveillance is required. As no investigation of aberrant prescription opioid-taking behaviors has been reported to date in Japan, the current situation remains unknown.
This internet survey study was conducted to investigate potential problematic opioid use in persons with chronic pain, including cancer-related pain, who had been prescribed opioid analgesics. Our aim was to gain an understanding of the prevalence of misuse, abuse, diversion, and doctor shopping of prescription opioid analgesics in Japan.
Methods
Participants
To begin the recruitment process, an email requesting participation in the survey was sent to persons over the age of 20 years living in Japan who were registered in the Rakuten Insight Disease Panel as disease panel monitors for the following conditions: Crohn’s disease, ulcerative colitis, migraine, trigeminal neuralgia, neuropathic pain, postherpetic neuralgia, diabetic neuropathy, lumbago, herniated disc, osteoporosis, gout, osteoarthritis, osteoarthritis of the knee, fibromyalgia, rheumatoid arthritis, and all types of cancer.
The commercial survey firm, Rakuten Insight (Rakuten Insight Inc., Tokyo, Japan, https://insight.rakuten.co.jp/en/), recruits registrants from across Japan through a variety of sources (e.g., credit cards, insurance, mobile services, online advertising channels, online affiliates, banner ads, e-commerce sites, etc.). Individuals choose to register as a disease panel monitor.
All eligible disease panel monitors who had registered to participate in any type of survey received online informed consent about the study; those who voluntarily provided consent progressed to the screening survey. The screening survey identified subjects who met the following criteria: (1) persistent pain lasting longer than 3 months; (2) regular attendance as an outpatient at a medical institution because of chronic pain; and (3) regularly prescribed an opioid analgesic (oral or patch). Persons who met all of these criteria progressed to the main survey.
Study Outcomes
The primary outcome was the proportion of participants in the analysis population with opioid misuse. Secondary outcomes were the proportion of participants in the analysis population with opioid abuse, diversion, and doctor shopping. For subgroup analysis, participants were divided into three groups: chronic cancer pain, chronic post-cancer treatment pain, and chronic noncancer pain.
Definitions
In this study, the definitions of misuse, abuse, diversion and doctor shopping were those reported in the literature [16,17,18]. Opioid misuse was defined as intentional noncompliance with the dosage regimen instructions or use of the opioid to relieve pain other than for prescribed purposes. Abuse was defined as use of a prescribed opioid for the purpose or motive of achieving a desirable effect (e.g., to induce sleep, to relieve anxiety or depression) other than relieving pain, i.e., use of a prescribed opioid for purposes for which it was not intended. Diversion was defined as having given a prescribed opioid analgesic to another person on at least one occasion. Doctor shopping was defined as receiving prescriptions for opioid analgesics at multiple medical institutions except for the following reasons: application at a different body site, geographical reasons, or accidentally running out of the drug and requiring an emergency prescription. These definitions (and the survey questions used to capture self-determined aberrant behaviors) applied to the prescribed opioid analgesic(s) that survey participants were currently receiving to relieve pain (as identified in the screening survey).
Internet Survey
Based on the abovementioned definitions, and referring to existing opioid misuse surveys (e.g., Addiction Behaviors Checklist [19], Current Opioid Misuse Measure [20]), survey questions were developed by the authors to match the Japanese environment. Questions were developed in the Japanese language and the survey was conducted in Japanese. Prior to distributing the questionnaire to survey participants, an informal pilot test was conducted involving six volunteers within Shionogi.
The screening survey consisted of informed consent and five questions: (1) “Do you have pain lasting more than 3 months?”; (2) “Are you regularly prescribed medicine to treat your pain?”; (3) “What type of analgesics are you prescribed? (Choice, multiple answers)”; (4) “Which analgesics are you prescribed?” (Select from product names including nonopioid analgesics, multiple answers); and (5) “What is the cause of your pain?” (Choose from cancer pain, pain associated with cancer treatment, chronic noncancer pain, unknown). Participants with an unknown pain history did not progress beyond the screening survey.
The main survey consisted of 17 questions that were designed to: identify prescription opioid misuse, abuse, diversion, and doctor shopping; capture background demographic and clinical information about participants (area of pain, causative disease in noncancer pain, history of psychiatric disease diagnosis, duration of opioid analgesia, drinking habits, smoking habits, academic background); determine participants’ behavior with regard to storage and disposal of leftover opioids; and ascertain any medication guidance participants may have received about their prescription opioids.
Misuse of prescribed opioids was identified by an affirmative response to at least one of two survey items: (1) When using an opioid painkiller, I took action at my own discretion to relieve pain. Some possible answers were: “I took (applied) a larger dose than prescribed”; “I took (applied) the medicine more often than prescribed”; “I took (applied) the medicine earlier than scheduled” (i.e., shortened the administration interval); “I chewed the tablet/capsule before swallowing”; “I opened the capsule or crushed the tablet to take the medicine”; “I warmed up the patch”; “I applied the patch in the mouth”; “I snorted the drug”; “I injected the drug”; and (2) “I used an opioid analgesic to relieve pain other than for its prescribed purpose (yes/no)”.
Abuse of prescribed opioids was identified by an affirmative response to one survey item: “I used an opioid analgesic for a purpose or motive other than to relieve pain”. Some response options were: to sleep better; to relieve anxiety; to relieve an irritable mood; to uplift myself; to feel better; to relax; to get high.
Diversion of prescribed opioids was identified by the act of the survey participant transferring their prescribed opioid analgesic(s) to another person.
Doctor shopping of prescribed opioids was identified by the act of receiving opioid analgesics from multiple institutions for reasons other than reasonable necessity (pain in a different area, geographical inconvenience, accidently running out of drug).
Sample Size
Since there are no data regarding the frequency of misuse of opioid analgesics in Japanese patients with chronic pain, the analysis was conducted with reference to a report on tramadol misuse in the US from 2002 to 2017 [10]. Assuming a frequency of 8%, the required number of subjects per group was 177 with a confidence level for detection of 95% and a margin of error of ± 4%. To account for potential dropouts, it was planned to include 200 participants in each pain group.
Statistics
Descriptive statistics were used. Quantitative data are summarized by mean and standard deviation (SD) and qualitative data by number (n) and frequency (%). 95% confidence intervals (95% CI) for proportions of subjects in the analysis target population reporting misuse, abuse, diversion, or doctor shopping were calculated using the Clopper–Pearson method.
A post hoc multivariate logistic regression analysis was performed to identify risk factors for aberrant prescription opioid-taking behavior using candidate risk factors selected from previous studies [21,22,23,24] as explanatory variables, and misuse, abuse, diversion, and doctor shopping as outcome variables. Explanatory variables (reference category) were age, sex (male/female), diagnosis of psychiatric disorder (with/without), pain site (head/non-head), causes of pain (chronic cancer pain/chronic pain unrelated to cancer; chronic pain associated with cancer treatment/chronic cancer pain unrelated to cancer), opioid analgesic use (with/without tramadol), alcohol use (habitual drinker/non-drinker; opportunistic drinker/non-drinker), smoking status (current smoker/non-smoker; history of smoking/non-smoker), and academic background (university or higher graduate/school graduate). Odds ratios and 95% CIs were calculated according to:
where p is the probablity of ‘yes’ for outcome (misuse, abuse, etc.); β0 the intercept; βi the partial regression coefficient; and χi an explanatory variable (age, continuous variable; others, categorical variables).
Statistical analysis was performed using BellCurve for Excel v.3.21 (Social Survey Research Information).
Ethical Considerations
The study was approved by the institutional Research Ethics Committee of Dokkyo Medical University Hospital(R-37-18) and was registered through the University Hospital Medical Information Network (UMIN000041788). All respondents provided voluntary consent to participate in the survey.
Results
Patient Characteristics
Screening Survey
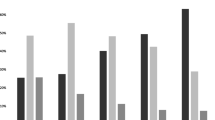
The survey began on September 1, 2020, with an invitation email delivered to 61,996 disease panel monitors with the prespecified pain conditions. The participant flow diagram is presented in Fig. 1. A total of 37,893 potential participants from across Japan (Supplementary Material) received the screening survey and 36,045 provided research consent, of whom 39.7% (n = 14,316) reported experiencing chronic pain (lasting > 3 months). More than half this chronic pain group had been prescribed analgesics (n = 7953, 55.6%), including 1043 subjects (13.1%) with a prescription for opioid analgesics. Because the number of potential participants with a primary prescription of opioid analgesics for chronic noncancer pain exceeded the 200 case target on the first day, inclusion into the main survey was halted for this group. On September 16, recruitment forecasting indicated that additional registration of participants with cancer-related pain could not be expected. The survey was thus conducted with the inclusion of 259 participants (66.9%) with chronic noncancer pain, 61 participants (15.8%) with cancer pain, and 67 participants (17.3%) with cancer treatment-associated pain.
Main Survey
The 387 participants who progressed to the main survey constituted the study analysis population (Table 1). Participants had a mean (SD) age of 55.4 (12.2) years, and 73.9% were male. More than three-quarters of participants (n = 300; 77.5%) had been prescribed opioids for ≥ 6 months. The most frequently prescribed opioid analgesic was a tramadol/acetaminophen combination (n = 201; 51.9%) followed by tramadol immediate release (n = 72; 18.6%), then transdermal formulations of fentanyl (n = 45; 11.6%) and oxycodone immediate release (n = 40; 10.3%). Psychiatric diseases diagnosed or treated were mainly insomnia (23.0%) and depression (21.7%); most participants (60.5%) had never been diagnosed with a mental health condition. Most participants were either current (31.3%) or previous (43.2%) smokers and were regular (31.3%) or occasional (28.9%) drinkers.
Outcomes
Outcomes according to chronic pain type are summarized in Table 2. The proportion of participants reporting opioid misuse (primary outcome) was 45.5% (95% CI: 40.4–50.6). With regard to secondary outcomes, 24.5% (95% CI: 20.3–29.2) of participants reported opioid abuse, 15.0% (95% CI: 11.6–19.0) reported diversion, and 10.6% (95% CI: 7.7–14.1) reported doctor shopping. Misuse was more common in participants with chronic post-cancer treatment pain (64.2%) or chronic cancer pain (57.4%) than in those with chronic noncancer pain (37.8%). Abuse was more than twice as common in participants with chronic post-cancer treatment pain (52.2%) than in those with chronic cancer pain (26.2%) or chronic noncancer pain (17.0%). Participants with chronic post-cancer treatment pain also reported higher rates of diversion (37.3%) and doctor shopping (32.8%) than those with chronic cancer pain (21.3% and 16.4%, respectively) or chronic noncancer pain (7.7% and 3.5%, respectively).
In participants who reported misuse of prescribed opioids (n = 176; 45.5%), common methods were intentionally changing the dose (18.4%) or dosing frequency (22.5%) for oral opioids and changing the number of patches (30.0%) or dosing frequency (24.0%) for transdermal opioids. Nearly a quarter of participants (23.0%) reported using oral/transdermal opioids for pain relief other than the prescribing physician’s intended purpose (Table 3). In participants who reported behaviors consistent with abuse of prescribed opioids (n = 95; 24.5%), the most common motives to use prescribed opioids for reasons other than pain relief were to relieve anxiety (12.7%) or to enable a better night’s sleep (11.1%) (Table 4).
More than a third of participants reported keeping their leftover opioids (n = 147; 38.0%), most commonly for possible future use (71.4%) (Table 5).
Most participants were aware of the need to adhere to the dose and dosing frequency of their opioid medications (61.2%), but less than one-third were aware of or able to recall being advised not to drive (31.8%) or not to give the drug to other persons including friends or family (29.7%). More than one in five participants (22.0%) could not recall receiving guidance or could not remember any of the guidance received about their opioid medication. About 16–17% of participants (one in six) could recall having received guidance about returning unused portions of the drug to the hospital/pharmacy, about not using multiple medical institutions to acquire the drug, and about keeping the drug out of the reach of children (Table 6).
A subgroup analysis of misuse, abuse, diversion, and doctor shopping outcomes was performed according to psychiatric disease diagnosis, cigarette smoking history, alcohol drinking history, leftover medication storage, and duration of opioid therapy (Table 7). Misuse was common in participants with psychiatric disease diagnoses, especially adjustment disorder (85.0%) and alcoholism (100.0%), and was more prevalent among current smokers (63.6%), those who kept leftover medication (61.9%), and those with opioid exposure of 3–6 months (63.4%) or 6 months to 1 year (63.8%). Abuse was associated most strongly with a diagnosis of adjustment disorder (75.0%) or alcoholism (84.2%), current smoking (40.5%), and leftover medication storage (40.8%). Diversion was associated most strongly with a diagnosis of adjustment disorder (65.0%) or alcoholism (73.7%). The strongest associations with doctor shopping were a diagnosis of adjustment disorder (50.0%) and alcoholism (52.6%).
A comparison of the rates of aberrant prescription opioid-taking behaviors is shown in Table 8 by opioid. Comparatively lower rates of misuse (ranging from 35.5 to 41.7%) and abuse (14.4% to 32.3%) were reported with tramadol formulations. Higher rates of misuse and abuse were reported with fentanyl (misuse: 75.0–80.0%; abuse: 40.0–59.1%); morphine extended-release (misuse: 90.0%; abuse: 70.0%); methadone (misuse: 87.5%; abuse: 87.5%); hydromorphone extended-release (misuse: 75.0%; abuse: 58.3%); and oxycodone (misuse: 62.5–69.0%; abuse: 37.5–44.8%) formulations. For commonly prescribed opioids (prescribed to ≥ 10 survey participants), misuse rates were higher than abuse rates which, in turn, were higher than diversion and doctor shopping rates. For example, misuse of fentanyl transdermal formulations was reported by 75.0% of respondents compared with 59.1% for abuse, 50.0% for diversion and 36.4% for doctor shopping.
Multivariate Regression Analysis
Multivariate regression analysis of candidate risk factors for misuse, abuse, diversion, and doctor shopping outcomes is shown in Table 9. Younger age and a diagnosis of psychiatric disease were significantly associated with all categories of aberrant prescription opioid-taking behaviors. ORs (95% CI) for misuse, abuse, diversion and doctor shopping were 0.96 (0.94–0.98), 0.94 (0.91–0.97), 0.93 (0.89–0.96) and 0.93 (0.89–0.97), respectively, for increasing age; and were 1.72 (1.04–2.84), 2.50 (1.34–4.67), 5.15 (2.09–12.69) and 4.29 (1.29–14.26), respectively, for the presence of a psychiatric disease. Male sex was significantly associated with misuse (OR = 1.81, 95% CI: 1.02–3.20) and doctor shopping (OR = 4.20, 95% CI: 1.05–16.81). Chronic pain related to cancer treatment was significantly associated with abuse (OR = 2.53, 95% CI: 1.16–5.51), diversion (OR = 2.55, 95% CI: 1.01–6.46) and doctor shopping (OR = 5.47, 95% CI: 1.73–17.32). Use of tramadol was significantly inversely associated with misuse (OR = 0.38, 95% CI: 0.20–0.72), abuse (OR = 0.28, 95% CI: 0.14–0.58), and doctor shopping (OR = 0.26, 95% CI: 0.09–0.77). Habitual alcohol drinking was significantly associated with abuse (OR = 3.44, 95% CI: 1.61–7.38) and diversion (OR = 10.01, 95% CI: 3.21–31.23). Current smoking was significantly associated with misuse (OR = 2.90, 95% CI: 1.52–5.56). Academic background and pain site were not significantly associated with any categories of aberrant prescription opioid-taking behaviors. Chronic post-cancer treatment pain was a higher risk than chronic noncancer pain in abuse, diversion, and doctor shopping models.
Discussion
This study was conducted in Japan, where opioid consumption is lower than in Western countries, there has not been any flood of illicitly manufactured opioids in our society for medical or nonmedical use, and where opioids are not favored as a drug of abuse. Nevertheless, the possibility of risky behaviors with regard to prescription opioids was unknown. To our knowledge, this is the first survey to investigate aberrant prescription opioid-taking behaviors in Japan. In an initial screening survey, 7953 of 14,316 potential participants with chronic pain reported receiving regular analgesic prescriptions, of whom 13.1% (n = 1043) were prescribed opioid analgesics, most commonly tramadol. This is consistent with current opioid prescribing patterns in Japan [25]. In the main survey, misuse was identified in 45.5%, abuse in 24.5%, diversion in 15.0%, and doctor shopping in 10.6% of survey respondents. These findings are specific to Japan and of considerable interest given the general perception by Japanese physicians that aberrant prescription opioid-taking behavior is rare [15].
In Japan, strong opioid analgesics are prescribed mainly to cancer patients [26]. The Japan Society of Pain Clinicians guidelines also state that several opioid analgesics can be used to treat chronic noncancer pain (with the exception of psychogenic pain), although not as first-line therapy [26]. Low opioid consumption in Japan is attributable to regulations, cultural barriers, and negative perceptions that discourage patients from consuming opioids and physicians from prescribing them [27]. In addition, illegal drug use is not as widespread in Japan as in other countries, according to a 2015 nationwide survey which found that only 0.1% of general population respondents had reported use of an illegal drug in the previous 12 months [28].
Worldwide, opioid use disorder (OUD) is associated with a high disease burden. The Global Burden of Disease Study 2017 estimated that, in North America, OUD accounts for more than 4 million healthy years of life lost due to disability and premature death [29]. Although Japan has largely avoided the dramatic surge in opioid consumption and related adverse outcomes witnessed in other countries [30], the relatively high prevalence of misuse and abuse reported by survey participants, at 45.5% and 24.5%, respectively, suggests a need for greater awareness among medical professionals to detect inappropriate opioid use early and prevent OUD. In contrast to other countries which have established harm reduction strategies for OUD, treatment of OUD has not been approved in Japan, making it difficult to provide opioid maintenance treatment, and detoxification is available only at some psychiatric institutions. As such, prevention of OUD is a priority.
We found that more potent opioids, such as oxycodone, fentanyl, hydromorphone, and morphine, were misused and abused more commonly than tramadol. We also found that aberrant opioid use behaviors were more common in participants with chronic post-cancer treatment pain and chronic cancer pain than in those with chronic noncancer pain. As previous studies have shown that at least one in five cancer patients may be at risk of OUD [31], the American Society of Clinical Oncology recommends multi-step universal precautions for cancer survivors, including risk stratification, prescription decisions, risk minimization, monitoring, and response to aberrant behaviors to minimize abuse, addiction, and opioid-related deaths [32]. This is especially true in the early palliative care setting where longer survival may increase the potential for risky behaviors associated with chronic opioid exposure [33]. Physicians should work to reduce misuse and abuse when prescribing opioid analgesics in any patient population, including cancer patients, and stay vigilant for any signs of aberrant opioid-taking behaviors.
This survey revealed that about one in five participants did not remember the medication guidance received about their prescription opioids or were unable to recall having received such guidance. More than a third of respondents (38.0%) admitted to having kept their leftover opioids, mainly for possible future use. Leftover medication storage behavior was associated with increased misuse (61.9% vs. 35.4%) and abuse (40.8% vs. 14.6%) compared with appropriate disposal of leftover drugs. These insights highlight that pharmacists play an important role in providing medication guidance and in confirming that patients understand the advice.
The post hoc multivariate logistic regression analysis identified younger age, a diagnosis of psychiatric disease, male sex, cancer treatment-related pain, opioids other than tramadol, habitual drinking, and current smoking as risk factors for one or more categories of aberrant prescription opioid-taking behaviors. In particular, younger age and a diagnosis of psychiatric disease were significantly associated with all categories of inappropriate use. Mood and anxiety disorders are also known to have a positive risk association with opioid abuse and dependence [21]. In general agreement with our results, a systematic review and meta-analysis of 43 studies (> 30 million subjects) reported that younger age (< 40 years), male sex, a mental health diagnosis, and current or previous substance use were risk factors associated with the development of opioid misuse [22]. In our study, current smoking was a significant risk factor for opioid misuse, consistent with a study which found that a higher proportion of people with versus without opioid misuse behavior were current smokers (64.6% vs. 25.7%) [23]. Although no significant association was found between academic background and aberrant prescription opioid-taking behaviors in our survey population, college attendance was identified as a negative risk factor for prescription opioid misuse in an analysis of National Survey on Drug Use and Health data in the US [24].
This survey study has several limitations. Since individuals self-select to register with Rakuten Insight and to participate in surveys, a degree of bias cannot be ruled out. Survey methodology tends to result in a higher proportion of participants in relatively good health, who may not be truly representative of the target population. The requirement for internet access to register with Rakuten Insight and to complete online surveys may have precluded the participation of older persons with chronic pain, although the mean age of the cohort was around 55 years. Self-reporting by disease panel monitors of a doctor’s diagnosis and the inherent heterogeneity of pain types are recognized as further limitations of the Rakuten Insight ‘patient’ database. Moreover, the numbers of disease panel monitors with a specific pain condition was not proportionate to the prevalence of the pain condition in Japan, also introducing bias. Due to slow recruitment of participants with cancer pain or cancer treatment-related pain, group sizes failed to reach the calculated quota, impacting on the strength of subgroup analyses according to pain type. Other limitations relate to the survey itself. Since definitions of aberrant prescription opioid-taking behaviors are not universal, and environments can differ markedly between countries, our results apply specifically to Japan and within the context of the definitions provided for misuse, abuse, diversion, and doctor shopping outcomes. Although survey questions were developed to the pattern of validated questionnaires, there was no formal evaluation of validity and reliability and only minimal pilot testing; as such, it is possible that participants may have misunderstood certain questions or failed to consider their responses carefully. This is the first survey of inappropriate use of opioid analgesics in Japan and, while results were similar to those from other countries, it cannot be said to have sufficient criterion validity. Due to the online nature of the survey, participants’ responses could not be verified while maintaining anonymity. With regard to the results, we acknowledge that the subgroup analysis of misuse, abuse, diversion, and doctor shopping outcomes according to baseline characteristics was weakened by the lack of control for confounders; nevertheless, the apparent association between aberrant prescription opioid-taking behaviors and the presence of adjustment disorder or alcoholism merits future investigation. Cancer-related pain has a concern in terms of reliability, since the target number of cases was not achieved. Also, in the regression analysis, the lack of multiple adjustment may have led to alpha errors.
Conclusions
Despite its limitations, our study has value since its provides first evidence of the existence of aberrant prescription opioid-taking behaviors in Japan. A clear message to emerge from the study findings is that universal precautions should always be taken when prescribing opioid analgesics, not only for patients with chronic noncancer pain but also for patients with cancer pain or pain related to cancer treatment.
References
[No authors listed]. WHO guidelines for the pharmacological and radiotherapeutic management of cancer pain in adults and adolescents. Geneva: World Health Organization; 2018.
International Association for the Study of Pain. IASP Statement on Opioids. 2018. https://www.iasp-pain.org/Advocacy/Content.aspx?ItemNumber=7194. Accessed 19 Sep 2021.
Bennett M, Paice JA, Wallace M. Pain and opioids in cancer care: benefits, risks, and alternatives. Am Soc Clin Oncol Educ Book. 2017;37:705–13.
Jones MR, Viswanath O, Peck J, Kaye AD, Gill JS, Simopoulos TT. A brief history of the opioid epidemic and strategies for pain medicine. Pain Ther. 2018;7(1):13–21.
Volkow ND, Jones EB, Einstein EB, Wargo EM. Prevention and treatment of opioid misuse and addiction: a review. JAMA Psychiat. 2019;76(2):208–16.
Degenhardt L, Grebely J, Stone J, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet. 2019;394(10208):1560–79.
Centers for Disease Control and Prevention. Evidence-Based Strategies for Preventing Opioid Overdose: What’s Working in the United States. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, US Department of Health and Human Services. 2018. http://www.cdc.gov/drugoverdose/pdf/pubs/2018-evidence-based-strategies.pdf. Accessed 15 Feb 2022.
American Society for Clinical Oncology. ASCO Policy Statement on Opioid Therapy: Protecting Access to Treatment for Cancer-Related Pain. 2016. https://www.asco.org/sites/new-www.asco.org/files/content-files/advocacy-and-policy/documents/2016-ASCO-Policy-Statement-Opioid-Therapy.pdf. Accessed 15 Feb 2022.
Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156:569–76.
Reines SA, Goldmann B, Harnett M, Lu L. Misuse of tramadol in the United States: an analysis of the national survey of drug use and health 2002–2017. Subst Abuse. 2020;14:1178221820930006.
Ministry of Justice. Narcotics and Psychotropics Control Act, Act No. 14 of March 17, 1953. Amendment of Act No. 50 of 2015. 2021. http://www.japaneselawtranslation.go.jp/law/detail/?id=2849&vm=04re=02. Accessed 19 Sep 2021.
Onishi E, Kobayashi T, Dexter E, Marino M, Maeno T, Deyo RA. Comparison of opioid prescribing patterns in the United States and Japan: primary care physicians’ attitudes and perceptions. J Am Board Fam Med. 2017;30(2):248–54.
Tannoury C, Kleweno C, Kamath AF, Gary J. Comparison of opioid use and prescribing patterns in orthopedic surgery in Japan and the United States: a JOA-AOA Traveling Fellowship Investigation. J Orthop Sci. 2020;25(3):520–4.
OECD. Health at a Glance 2019: OECD Indicators, OECD Publishing, Paris; 2019. https://doi.org/10.1787/4dd50c09-en. Accessed 15 Feb 2022.
Miyachi T, Ozaki A, Saito H, Sawano T, Tanimoto T, Crump A. Opioids: a “crisis” of too much or not enough—or simply how rich you are and where you live? Eur J Pain. 2021;25(6):1181–94.
Smith SM, Dart RC, Katz NP, et al. Classification and definition of misuse, abuse, and related events in clinical trials: ACTTION systematic review and recommendations. Pain. 2013;154(11):2287–96.
Cheatle MD. Prescription opioid misuse, abuse, morbidity, and mortality: balancing effective pain management and safety. Pain Med. 2015;16(Suppl 1):S3-8.
Sansone RA, Sansone LA. Doctor shopping: a phenomenon of many themes. Innov Clin Neurosci. 2012;9(11–12):42–6.
Wu SM, Compton P, Bolus R, et al. The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J Pain Symptom Manage. 2006;32(4):342–51.
Butler SF, Budman SH, Fernandez KC, et al. Development and validation of the Current Opioid Misuse Measure. Pain. 2007;130(1–2):144−56. [Erratum in: Pain. 2009;142(1–2):169].
Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(2):247–57.
Cragg A, Hau JP, Woo SA, et al. Risk factors for misuse of prescribed opioids: a systematic review and meta-analysis. Ann Emerg Med. 2019;74(5):634–46.
Parker MA, Weinberger AH, Villanti AC. Quit ratios for cigarette smoking among individuals with opioid misuse and opioid use disorder in the United States. Drug Alcohol Depend. 2020;214: 108164.
Ford JA, Pomykacz C, Ortiz K, McCabe SE, Schepis TS. Educational attainment and prescription drug misuse: The importance of push and pull factors for dropping out. J Crim Justice. 2020;66: 101636.
Akazawa M, Mimura W, Togo K, et al. Patterns of drug treatment in patients with osteoarthritis and chronic low back pain in Japan: a retrospective database study. J Pain Res. 2019;12:1631–48.
The Committee for the Guidelines for Prescribing Opioid Analgesics for Non-cancer Chronic Pain of JSPC. Guidelines for Prescribing Opioid Analgesics for Chronic Non-cancer Pain Second Edition (pp. 150–160). 2017; Shinko Trading Co. Ltd., Tokyo.
Uba RO, Ankoma-Darko K, Park SK. International comparison of mitigation strategies for addressing opioid misuse: a systematic review. J Am Pharm Assoc (2003). 2020;60(1):195–204.
National Center of Neurology and Psychiatry. 2015 nationwide general population survey on drug use in Japan. 2017. https://www.ncnp.go.jp/nimh/yakubutsu/report/pdf/2017_0522_2015EN_shimane2_k.pdf. Accessed 19 Sep 2021.
United Nations Office on Drugs and Crime. World Drug Report 2019. 3. Depressants. 2019; United Nations publication: Sales No. E.19.XI.8. 2022. https://wdr.unodc.org/wdr2019/prelaunch/WDR19_Booklet_3_DEPRESSANTS.pdf. Accessed 15 Feb 2022.
Suga Y, Uchida M, Suzuki S, et al. Current status of adverse events related with opioid analgesics in Japan: assessment based on Japanese Adverse Drug Event Report Database. Biol Pharm Bull. 2019;42(5):801–6.
Carmichael AN, Morgan L, Del Fabbro E. Identifying and assessing the risk of opioid abuse in patients with cancer: an integrative review. Subst Abuse Rehabil. 2016;7:71–9.
Paice JA, Portenoy R, Lacchetti C, et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2016;34(27):3325–45.
Gaertner J, Boehlke C, Simone CB 2nd, Hui D. Early palliative care and the opioid crisis: ten pragmatic steps towards a more rational use of opioids. Ann Palliat Med. 2019;8(4):490–7.
Acknowledgements
The authors sincerely thank the disease panel monitors who participated in the study.
Funding
Sponsorship for the survey and Rapid Service Fee were funded by Shionogi & Co., Ltd. (Osaka, Japan).
Medical Writing, Editorial, and Other Assistance
Medical writing and editorial assistance were provided by Robert Furlong and Kerry Dechant, ISMPP CMPP™ on behalf of Content Ed Net with funding from Shionogi & Co., Ltd. (Osaka, Japan). Editorial support and review of the manuscript were provided by Yasuhide Morioka and Noriyuki Naya, Medical Affairs, Shionogi & Co., Ltd. Data collection and data analysis were carried out by Takashi Usui and Nanako Kafuku, Rakuten Insight Inc. (Tokyo, Japan), with funding from Shionogi & Co., Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Toshifumi Takasusuki, Shinji Hayashi, Yuichi Koretaka, and Shigeki Yamaguchi contributed to the study conception and design, material preparation, data collection and analysis of the results and to the writing of the manuscript.
Prior Presentation
These findings were presented at the 26th Congress of the Japanese Society for Palliative Medicine (Yokohama, Japan; June 18–19, 2021).
Disclosures
Toshifumi Takasusuki has no conflict of interest to disclose. Shinji Hayashi and Yuichi Koretaka are employees of Shionogi & Co., Ltd. Shigeki Yamaguchi has received lecture and manuscript writing fees from Daiichi Sankyo Co., Ltd, Hisamitsu Pharmaceutical Co., Inc., and Shionogi & Co., Ltd. In Japan, Shionogi & Co., Ltd manufactures and distributes opioid analgesics including oxycodone (OxyContin®) and morphine (MSContin®), and distributes methadone (Methapain®).
Compliance with Ethics Guidelines
The study was approved by the institutional Research Ethics Committee of Dokkyo Medical University Hospital (R-37-18) and was registered through the University Hospital Medical Information Network (UMIN000041788). All respondents provided voluntary consent to participate in the survey.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Takasusuki, T., Hayashi, S., Koretaka, Y. et al. Prevalence of and Risk Factors for Prescription Opioid Misuse, Abuse, Diversion and Doctor Shopping in Japan: A Survey Study. Pain Ther 11, 987–1009 (2022). https://doi.org/10.1007/s40122-022-00409-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00409-6