Abstract
Introduction
Chronic pain (CP) negatively impacts the lives of almost 2 billion people worldwide, including approximately 37% of adults in Portugal. As most of these patients are followed by a general practitioner, identifying the prevalence and characterizing the pain of patients who visit primary care units will provide valuable insights into the CP landscape in Portugal.
Methods
To achieve this goal, an observational, cross-sectional study was conducted in 58 primary care units of mainland Portugal between June 2017 and March 2018. Interviews were conducted with 8445 patients, and 578 CP patients were characterized.
Results
We observed that one third of patients suffered from CP, and of these, approximately one third felt that their pain management was insufficient. Most of the population was 55 years old or older, retired, and had more than three comorbidities. However, age and the number and type of comorbidities were not predictors of pain intensity. Additionally, most of the population had pain or discomfort that hindered their mobility and the performance of their everyday activities. This decrease in the quality of life led to feelings of anxiety and depression, which were associated with pain intensity.
Conclusion
Given the high prevalence of CP, strategies to improve the quality of life of these patients and decrease the negative impacts, as well as awareness campaigns to increase the populations’ knowledge of this condition, are essential for the suitable and timely treatment of CP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
In Portugal, there is a paucity of information regarding the characterization of patients with chronic pain who visit primary care units, and no real-world data are available regarding chronic pain epidemiology in this setting. |
This study bridges the existent gap by providing valuable information on the prevalence of chronic pain and its impact on the quality of life of patients who visit primary care units. |
What was learned from the study? |
Chronic pain affects one third of patients who present to primary care units and has a significant impact on the quality of life of patients in all domains, mainly on psychological status, with feelings of anxiety and/or depression. |
Roughly one in three chronic pain patients did not consider that their pain was correctly managed. This observation highlights the need to raise awareness about this multidimensional condition. |
Introduction
Chronic pain (CP) affects approximately 1.9 billion people worldwide [1], including approximately 37% of the Portuguese population [2]. It has been defined as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage” which has persisted after the cause has been healed or for longer than 3 months [3, 4]. Usually considered an outcome of injury or disease, CP has been classified as a distinct clinical entity and not as a consequence of other diseases [1, 5]. This condition impacts many aspects of patients’ lives, affecting home/family responsibilities, work, social life and recreational activities [2, 6]. Accordingly, low back and neck pain, which are symptomatic chronic conditions, are among the main causes of disability [1]. Thus, besides pain relief, treatment of chronic pain also strives to minimize disability, decreasing physical and social limitations, and ultimately improving the quality of life of the patients [7].
In most countries, patients first present to primary care, as it provides accessible, continuous, complete and coordinated care [4]. Therefore, the majority of chronic pain patients are followed by their general practitioner in primary care units (PCU) [4]. In 2006, a survey in 15 European countries (which did not include Portugal and Israel) showed that only 2% of patients with CP were referred to specialized care [8, 9]. Moreover, approximately 50% of patients received inadequate pain management [8]. However, in Portugal, there is a paucity of information regarding the characterization of patients with CP who visit PCU.
This work reports the results of a cross-sectional observational study based on interviews of individuals aged 18 years or older who visited 58 Portuguese PCU within a period of 10 months. Patients with CP were selected, and the prevalence and characteristics of CP diagnosis and management were assessed. The data obtained from this study will help to improve the timely diagnosis, referral, and proper management of CP by general practitioners, the first point of contact for CP patients.
Methods
Geographical Representation and Compliance with Ethical Standards
This was an observational, cross-sectional study, conducted at 58 PCU in mainland Portugal. The study sites were chosen using a population proportional sampling method and are thus representative of the Portuguese population. Patient interviews were conducted between June 2017 and March 2018. Written informed consent was obtained from all participants and the study protocol was approved by local Ethics Committees. This work was conducted according to the tenets of the Declaration of Helsinki in its latest amendment (Brazil, 2013). The leading ethical committee, representative of the largest number of centers, Comissão de Ética para a Saúde da Administração Regional de Saúde do Norte, approved the study protocol and the written informed consent form, with approval reference number 99/2017. The names of all ethics committees and the reference numbers of the approvals are provided in table S1 (Supplementary Material).
Eligibility Criteria
Eligibility criteria were as follows: (1) age 18 years or older and (2) being able and willing to provide written informed consent. A total of 8480 interviews were conducted, but 35 were excluded due to protocol deviations. Of the 8445 participants, 2834 suffered from CP. CP patients were defined as individuals who (1) had pain for more than 3 months, (2) had pain for less than 3 months, but the pain persisted after the cause was healed, or (3) had a previous diagnosis of CP but were asymptomatic due to suitable treatment. Of the 2834 CP patients, 578 were selected for further characterization.
Information Collected
Data on demographic characteristics, healthcare and pain characteristics, comorbidities, and pharmacological and non-pharmacological pain treatments were collected by the physician during the patients’ regular medical appointments. The information was introduced in an electronic case report form specifically designed for this study, which included a section for the patient information and another for the physician assessment. All information subject to recall bias was collected from the medical records. Pain intensity and the patients’ perception regarding the understanding of pain severity by the physician were assessed using 11-point Likert scales, with 0 corresponding to no pain/understanding and 10 corresponding to maximum pain/understanding. Pain relief was assessed using a five-point Likert scale comprising the categories “significant relief,” “sufficient relief,” “some relief,” “small relief,” and “no relief.” Health-related quality of life was evaluated using the EQ-5D-3L questionnaire [10].
Statistical Analysis
An intent-to-treat (ITT) statistical analysis was performed. According to the original statistical analysis plan (SAP), statistical analysis was performed with available data, and no method of imputation for missing data was used. Quantitative variables were tested for normality using the Shapiro–Wilk test. Since the majority of quantitative variables were not normally distributed, baseline median, interquartile range (IQR), minimum and maximum are presented. For categorical variables, number and percentage of total are presented. Between-group analyses of quantitative variables were performed using the Mann–Whitney or Kruskal–Wallis test as appropriate, and adjusted for multiple comparisons using the Šidák correction when needed. For categorical variables, the χ2 test was used. Two univariate regressions were performed to analyze if age was a predictor of the maximum and average pain intensity. The dependent variables were maximum and average pain intensity, and the independent variable was age, being all these variables analyzed as continuous. A significance level of α = 0.05 (two-sided) was used. The software used was the SPSS version 23.0 statistical package.
Results
Pain Prevalence and Characteristics
We observed that 33.6% of primary care unit patients suffered from CP. The characterized patients were all 25 years or older, and 73% were 55 years or older. The cohort comprised 423 women (73.2%) and 155 men (26.8%). The majority of patients were retired (48.8%), 22.8% were still actively working, 14.4% were on sick leave, 8% were housewives, 5.7% were unemployed, and 0.3% were students. Most of the patients (60.9%) had more than three comorbidities, with those related to cardiometabolic disorders being the most prevalent (74.6%) (Table 1).
The median and IQR of the maximum pain intensity reported during the previous week was 7.0 (3.0) on a scale of 1–10. The median and IQR of average pain intensity reported during the previous week was 5.0 (3.0), also on a scale of 1–10. More than 95% (n = 575) of patients were under pharmacological treatment, and 69% reported feeling some relief, while 31% felt minor or no relief. Most of the patients were diagnosed by a general practitioner (61.4%), and approximately half (51.7%) were diagnosed after experiencing symptoms for less than 1 year. CP had a negative impact on the mobility and usual activities of patients, as most of them reported having at least some problems (66.4% and 66.8%, respectively) in performing these activities. Additionally, 12.1% of patients reported not being able to carry out their personal hygiene routine and/or get dressed by themselves, and 41.3% reported having some problems performing these activities. Accordingly, 91.5% of patients reported feeling pain/discomfort. Regarding anxiety/depression, 14.4% of patients were extremely depressed/anxious, 54.2% were moderately depressed/anxious, and 31.5% did not feel depressed/anxious (Table 2).
Factors Influencing Pain Resolution Expectations
CP patients and their physicians reported the time that they expected would be needed to achieve pain resolution. Physicians anticipated successful resolution in less than 1 year for patients with a lower number of visits to the PCU and for patients who perceived that their physician understood the severity of their pain. Moreover, a higher number of medical tests (performed in the previous 12 months) negatively influenced physicians’ expectations of the time needed for pain resolution.
Age did not have an impact on patients’ expectations regarding time for pain resolution. Moreover, on regression analysis, age was not a predictor of maximum or average pain intensity reported by patients. The number of radiological exams, on the other hand, influenced the time expectation of patients. A higher number of radiological exams was found for the group of patients who predicted that > 1 year would be needed to achieve pain resolution, suggesting that patients who undergo a greater number of radiological exams expect that more time will be needed to achieve pain resolution (Table 3).
Influence of Medical Specialty on Diagnosis and Pain Management
Patients diagnosed and monitored by medical specialties other than general practitioners reported a higher level of maximum pain intensity (8.0 vs. 7.0, p = 0.006; 7.5 vs. 7.0, p = 0.008, respectively) (Fig. 1), but no significant difference was found in the time needed to diagnose CP. Median (IQR) values, in years, from the time of first symptoms to diagnosis were 0.5 (2.2) and 0.3 (2.0) for patients diagnosed by a general practitioner or by a physician from another medical specialty, respectively.
Association between the medical specialty that diagnosed and/or monitored patients and pain intensity. The groups studied included patients diagnosed (n = 355) and monitored (n = 482) by a general practitioner (GP) and patients diagnosed (n = 100) and monitored (n = 96) by other medical specialties (other). Columns represent median values and error bars represent 95% CIs. Between-group analyses were performed using the Mann–Whitney test. A significance level of α = 0.05 (two-sided) was used
Anxiety and Depression in CP Patients
Patients with higher levels of maximum pain intensity were more likely to report feeling moderately or extremely anxious and/or depressed. Significant differences were found between the groups that reported moderate and extreme states of anxiety/depression when compared with those who reported not feeling anxious/depressed (p < 0.001). No significant differences were observed between patients who reported moderate or extreme levels of anxiety/depression (see Fig. 2).
Association between pain intensity and patients’ mental well-being. Level of maximum pain intensity described by patients who reported not feeling anxious and/or depressed (n = 182) and by patients who reported feeling moderately (n = 313), or extremely (n = 83) anxious and/or depressed. Columns represent mean values, and error bars represent 95% CIs. Between-group analyses were performed using the Kruskal–Wallis test and adjusted for multiple comparisons using the Šidák correction. A significance level of α = 0.05 (two-sided) was used
Discussion
The main goal of this study was to assess and characterize CP in patients who visit Portuguese PCU. The prevalence of CP in this population was 33.6%, which is in line with an epidemiological study from 2012 that estimated CP prevalence in Portugal of 36.7% [2]. Although the study designs were different, since our study focused on individuals who visit the PCU whereas the study by Azevedo et al. was based on computer-assisted telephone interviews to the general population [2], both studies point to approximately one third of the Portuguese population being affected by CP.
Patients 55 years or older comprised 73% of the studied population, and patients 65 years or older, 46.2%. This prevalence of CP in older adults is in accord with the reported high prevalence of CP in individuals 65 years or older [11, 12]. Although age can increase the probability of developing CP, no causality was found between age and pain intensity. Thus, age does not seem to be a predictor of the pain intensity felt by patients. In fact, the cultural context might be more important for the perception of pain intensity than age, since if the individuals believe that a medical consultation will help, they present to the physician regardless of age.
Disability is one of the main consequences of CP, with a direct impact on patients’ lives and on the economy [13]. In the studied population, approximately one in seven (14.4%) CP patients were on sick leave. Although no direct comparisons can be made, Azevedo et al. also reported that 15% of individuals who suffered from CP had a severe disability [2], which could translate into the need for sick leave. Also, in a European study that did not include Portugal, Breivik et al. showed that one in four individuals reported that their pain had impacted their employment status [8], although the percentage of patients on sick leave was not specified.
Gender is thought to influence the risk of developing CP, with women being at higher risk than men [2, 14]. In our cohort, 73.2% of the individuals were female, which supports the higher risk of developing CP among women.
Although more than half (60.9%) of the studied population had more than three comorbidities, no association between the existence of comorbidities and pain intensity, either maximum or average, was observed. Nevertheless, the presence of comorbidities is relevant for the treatment of CP, since pharmacological interactions and effects of the prescribed medication in all pathologies must be considered [11, 12].
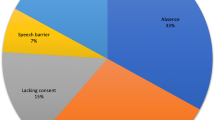
Approximately one third of the studied population did not feel that their pain was managed correctly. First-line treatment of chronic pain usually comprises non-opioid analgesics such as paracetamol and nonsteroidal anti-inflammatory drugs [15]. If these are ineffective, weak and then strong opioids should be prescribed [15]. However, Portugal is ranked as one of the countries with the lowest opioid consumption among western Europe [7, 16]. Physicians reported legal risk and fear of adverse events as the main reason for their reluctance in prescribing opioids [16, 17], which might explain why 31% of the patients felt that their treatment was ineffective. Other possible reasons include lack of support for psychological follow-up and for other non-pharmacological strategies that could improve CP treatment. The introduction of psychological support could help manage CP patients’ expectations and, consequently, increase treatment adherence. Some patients might feel they would receive better care in a hospital or might have misguided expectations regarding the progression of their condition. Similarly, introduction of support for non-pharmacological strategies such as physical rehabilitation could contribute to improved functionality in these patients and overall treatment satisfaction.
Additionally, we observed that aspects such as the number of visits to the PCU, the patients’ notion of how well the physician understood the severity of their pain, and number of exams performed influenced the physicians’ expectation of the time needed to identify an effective treatment regimen. A higher number of visits to PCU suggests that the condition is worsening, explaining the negative impact on the physicians’ expectation. Due to the subjective nature of pain, good communication between patients and physicians seems to be essential. The patient needs to understands that, most likely, there will not be a cure for their pain, but rather a good management regimen to ensure the best possible quality of life. Besides pain relief, CP treatment aims at decreasing disability and ameliorating physical and social limitations, with the ultimate goal of improving patients’ quality of life [7]. Thus, effective communication will help patients feel that the physician understands their condition, and will improve physicians’ ability to identify a good treatment regimen to which the patients will successfully adhere. In both these components, no difference was observed between an expectation of greater than 1 year and no immediate resolution (NIR), suggesting that when NIR is predicted, more than 1 year will be needed to achieve acceptable pain management. A higher number of exams negatively impacted physicians’ expectations for pain management. The need for more exams suggests difficulties in diagnosing the cause of pain, which would increase the time needed to identify a good therapeutic regimen. This difficulty might be related to the subjectivity of pain, which is affected by personal bias and by the pain threshold of each individual. The number of radiological exams also had a negative impact on patients’ expectations of pain resolution, as more exams suggest difficulties in reaching a diagnosis. Moreover, patients might perceive that other types of exams, instead of more radiological exams, would be more useful for diagnostic purposes.
Patients diagnosed and monitored by medical specialties other than general practitioners reported higher levels of pain intensity. This might be a result of patient referral, as general practitioners usually refer patients with higher pain intensity to other medical specialties. Moreover, when the patient needs specific resources, the monitoring of CP patients is undertaken by these medical specialties. Although general practitioners might have more limitations in the exams that they can prescribe, no significant difference in the time needed to diagnose CP was observed when comparing general practitioners with other medical specialties. In fact, a significant proportion of the population was diagnosed in less than 6 months, regardless of the specialty of the physician making the diagnosis.
Depression and anxiety are the most prevalent emotional consequences in patients with CP [2]. In our cohort, patients with higher intensity of pain were more likely to feel moderately and extremely depressed and/or anxious. This result reflects the huge impact that CP has on the patients’ quality of life due to pain or discomfort and due to problems with mobility and in performing everyday activities. Interestingly, no significant difference was observed between the levels of pain intensity reported by individuals who felt moderate and extreme levels of anxiety/depression, again highlighting the subjective nature of pain and how the individual pain threshold may cause differences in how patients are emotionally affected by CP. Due to the subjectivity of pain, it is also important to keep in mind that these results should be interpreted taking into account the Portuguese cultural context that will influence patients’ expectations and knowledge of CP.
Strengths and Limitations
This study analyzed the prevalence of CP in the PCU. Due to the high prevalence of this condition, a thorough characterization of the population with CP and the impact on their quality of life is of the utmost importance. Moreover, in addition to patient interviews, the study interviewed general practitioners, who are usually the first contact for these patients. On one hand, to attain a good representation of the Portuguese population, the geographical distribution of the population was considered in the selection of the location and number of included PCU. On the other hand, the study was limited in that it included only mainland Portugal and did not consider the islands of Azores and Madeira. Another limitation, commonly observed in CP studies, is related to pain subjectivity. As pain and health-related quality of life assessment are based on self-reports, there is always the possibility of bias due to the different cultural context of patients and their perception of and tolerance to pain.
Conclusions
Overall, we determined that CP is highly prevalent, affecting one third of patients who present to the PCU. Also, we verified that this condition has a significant impact on the quality of life of patients, causing feelings of anxiety and/or depression. Approximately one in three CP patients did not feel that their pain was correctly managed, which underscores the need for awareness campaigns and information dissemination on CP and its treatment. CP treatment should include both pharmacological treatment for pain relief and non-pharmacological strategies to increase patients’ functional ability and well-being, and to decrease feelings of social isolation, anxiety, and depression.
References
Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019;123(2):e273–83.
Azevedo LF, Costa-Pereira A, Mendonca L, Dias CC, Castro-Lopes JM. Epidemiology of chronic pain: a population-based nationwide study on its prevalence, characteristics and associated disability in Portugal. J Pain. 2012;13(8):773–83.
International Association for the Study of Pain. IASP Announces Revised Definition of Pain. Washington: International Association for the Study of Pain (2020). https://www.iasp-pain.org/PublicationsNews/NewsDetail.aspx?ItemNumber=10475&navItemNumber=643. Accessed Mar 2021.
Mills S, Torrance N, Smith BH. Identification and management of chronic pain in primary care: a review. Curr Psychiatry Rep. 2016;18(2):22.
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19–27.
Cáceres-Matos R, Gil-García E, Barrientos-Trigo S, Porcel-Gálvez AM, Cabrera-León A. Consequences of chronic non-cancer pain in adulthood. Scoping review. Rev Saude Publica. 2020;54:39.
Azevedo LF, Costa-Pereira A, Mendonca L, Dias CC, Castro-Lopes JM. A population-based study on chronic pain and the use of opioids in Portugal. Pain. 2013;154(12):2844–52.
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333.
World Health Organization. Primary health care, main terminology (2018). https://www.eurowhoint/en/health-topics/Health-systems/primary-health-care/main-terminology Accessed 1 Mar 2021.
Ferreira LN, Ferreira PL, Pereira LN, Oppe M. EQ-5D Portuguese population norms. Qual Life Res. 2014;23(2):425–30.
Domenichiello AF, Ramsden CE. The silent epidemic of chronic pain in older adults. Prog Neuropsychopharmacol Biol Psychiatry. 2019;93:284–90.
Schwan J, Sclafani J, Tawfik VL. Chronic pain management in the elderly. Anesthesiol Clin. 2019;37(3):547–60.
Azevedo LF, Costa-Pereira A, Mendonca L, Dias CC, Castro-Lopes JM. The economic impact of chronic pain: a nationwide population-based cost-of-illness study in Portugal. Eur J Health Econ. 2016;17(1):87–98.
Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, et al. Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(36):1001–6.
Hylands-White N, Duarte RV, Raphael JH. An overview of treatment approaches for chronic pain management. Rheumatol Int. 2017;37(1):29–42.
Reis-Pina P, Lawlor PG, Barbosa A. Moderate to severe cancer pain: are we taking serious action? The opioid prescribing scenario in Portugal. Acta Med Port. 2018;31(9):451–3.
Verloo H, Mpinga EK, Ferreira M, Rapin CH, Chastonay P. Morphinofobia: the situation among the general population and health care professionals in North-Eastern Portugal. BMC Palliat Care. 2010;9:15.
Acknowledgements
The authors would like to thank the personnel involved in data collection, the general practitioners, and the patients, who were essential for this study.
Funding
Sponsorship for this study and for the journal’s Rapid Service Fee was provided by Grünenthal Portugal.
Editorial Assistance
Editorial assistance was provided by Constança Coelho, PhD, and Inês Torcato, PhD, from X2 Science Solutions. Financial support for this assistance was provided by Grünenthal Portugal.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
Study conception and design: FA, RT. Material preparation, data collection and data analyses: all authors. All authors read and approved the final manuscript.
Prior Presentation
Part of the data presented in this manuscript were presented in poster format at the 11th Congress of the European Pain Federation EFIC, Valencia, Spain, Sep. 4–8, 2019.
Disclosures
Filipe Antunes has received fees from Angelini, Bene, Menarini, Grünenthal, and Pfizer. Raul Marques Pereira has received fees from Menarini, Pfizer, Mylan and Grünenthal. Vera Afonso has received fees from Grünenthal. Rita Tinoco is an employee of Grünenthal Portugal.
Compliance with Ethics Guidelines
This study was conducted according to the tenets of the Declaration of Helsinki in its latest amendment (Brazil, 2013) and was approved by the ethics committee of all participating centers. The leading ethical committee, representative of the largest number of centers, Comissão de Ética para a Saúde da Administração Regional de Saúde do Norte, approved the study protocol and the written informed consent form, with approval reference number 99/2017. The names of all ethics committees and the reference numbers of the approvals are provided in Table S1 (Supplementary Material).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Antunes, F., Pereira, R.M., Afonso, V. et al. Prevalence and Characteristics of Chronic Pain Among Patients in Portuguese Primary Care Units. Pain Ther 10, 1427–1437 (2021). https://doi.org/10.1007/s40122-021-00308-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-021-00308-2