Abstract
Introduction
Recently the DAVID study demonstrated the better analgesic efficacy of tramadol hydrochloride/dexketoprofen 75/25 mg (TRAM/DKP) over tramadol hydrochloride/paracetamol 75/650 mg (TRAM/paracetamol) in a model of moderate to severe acute pain following surgical removal of an impacted third molar. The aim of this subpopulation analysis was to gain a deeper understanding of the relationship between baseline pain intensity (PI) level and the effectiveness in pain control of the TRAM/DKP combination in comparison with the TRAM/paracetamol combination. This will further improve and facilitate the accurate design of future acute pain studies for the use of the TRAM/DKP combination.
Methods
Patients experiencing at least moderate pain, defined as a PI score ≥ 4 in an 11-point numerical rating scale (NRS) were stratified according to NRS-PI at baseline (NRS ≥ 4, 5, 6, 7, or 8) or aggregated in two groups: (i) moderate pain, NRS-PI ≥ 4 to ≤ 6; (ii) severe pain, NRS-PI > 6. Analgesic efficacy was assessed at pre-specified time points by using pain relief (PAR) on a 5-point verbal rating scale (VRS) and PI on an 11-point NRS. The primary endpoint was total PAR over 6 h post-dose (TOTPAR6); secondary endpoints included, among others, the time course of mean PAR and PI scores over 8 h, TOTPAR over 2, 4, and 8 h post-dose, and the sum of PI difference (SPID) over 2, 4, 6, and 8 h. Safety evaluation was based on the incidence, seriousness, intensity, and causal relationship of treatment-emergent adverse events (TEAEs).
Results
The analgesic efficacy evaluated by TOTPAR6 (primary endpoint) remained steady across increasing baseline PI-NRS cutoff groups with TRAM/DKP, but not with TRAM/paracetamol. The study also demonstrated the superiority of TRAM/DKP combination over TRAM/paracetamol in terms of TOTPAR over 2, 4, and 8 h post-dose and SPID at 2, 4, 6, and 8 h post-dose in both baseline PI groups (moderate or severe); similarly, the time course of PAR and PI indicated better efficacy with TRAM/DKP as soon as 30 min and up to 4–6 h. The incidence of adverse drug reactions was not increased in the severe baseline PI group.
Conclusion
Overall, the results of this subgroup analysis of the DAVID study confirmed the superiority of the analgesic efficacy of TRAM/DKP vs TRAM/paracetamol, irrespective of the baseline PI.
Plain Language Summary
The combination tramadol/dexketoprofen (TRAM/DPK) was recently shown to exert a better analgesic effect than the combination tramadol/paracetamol (TRAM/paracetamol) after surgical removal of impacted lower third molar in a clinical trial enrolling more than 600 patients. A subanalysis of the results of this study was performed to assess if the severity of pain intensity (PI) at baseline might modify the analgesic effect and its duration. The results of the subanalysis showed that the analgesic efficacy of TRAM/DKP was independent of baseline PI and persistent up to 6 h, whereas the effect of TRAM/paracetamol progressively decreased with increasing baseline PI and persisted for a shorter period. The incidence of adverse drug reactions was not increased in patients with severe baseline PI. These results confirmed the better analgesic efficacy of TRAM/DKP vs TRAM/paracetamol, irrespective of the baseline PI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The DAVID study demonstrated the better analgesic efficacy of tramadol hydrochloride/dexketoprofen 75/25mg (TRAM/DKP) over tramadol hydrochloride/paracetamol 75/650mg (TRAM/paracetamol) in a model of moderate to severe acute pain following surgical removal of an impacted third molar. |
The aim of this subpopulation analysis was to gain a deeper understanding of the relationship between baseline pain intensity level and the effectiveness in pain control of the TRAM/DKP combination in comparison with the TRAM/paracetamol combination. |
What was learned from the study? |
The analgesic efficacy evaluated by TOTPAR6 (primary endpoint) remained steady across increasing baseline PI-NRS cutoff groups with TRAM/DKP, but not with TRAM/paracetamol. |
The incidence of adverse drug reactions was not increased in the severe baseline PI group. |
Overall, the results of this subgroup analysis of the DAVID study confirmed the superiority of the analgesic efficacy of TRAM/DKP vs TRAM/paracetamol, irrespective of the baseline PI. |
Digital Features
This article is published with digital features, including a summary slide and plain language summary, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13311959.
Introduction
Acute pain has substantial physiological and psychological consequences and becomes more difficult to manage as severity increases. Even brief intervals of painful stimulation can induce suffering, neuronal remodeling, and chronic pain [1]. Therefore, early intervention with an effective, fast-acting analgesic is key to manage acute pain to reduce complications, including progression to chronic pain states [2].
Attaining adequate pain relief (PAR) with monotherapy is difficult and multimodal analgesia is now accepted as the cornerstone of effective pain treatment [3]. Combining analgesics with diverse mechanisms of action and potential synergistic effects yields good pain relief and minimizes side effects. Compared with monotherapy, multimodal analgesia offers several benefits, including a broader spectrum of action, greater efficacy, better compliance, and a better efficacy/safety ratio. As a result, analgesic combinations are recommended by the World Health Organization (WHO), American Pain Society (APS), American College of Rheumatology (ACR), and European Pain Federation (EFIC) and are commonly used in clinical practice [4].
Dexketoprofen (DKP) is an anti-inflammatory and analgesic drug that inhibits cyclooxygenase 1 (COX-1) and COX-2, with proven high analgesic potency in a wide spectrum of acute pain syndromes [5, 6]. It was shown to be as effective as the double dose of the racemic ketoprofen, but with a faster onset of analgesia. The rapid dissolution and absorption (tmax between 15 and 45 min) ensure rapid PAR, which is crucial for the effective management of acute pain [7]. DKP efficacy and rapid onset of analgesic activity are complemented by a safety profile that favors DKP over many other nonsteroidal anti-inflammatory drugs (NSAIDs) [8,9,10].
Tramadol (TRAM) has a dual analgesic mechanism: through its action as a μ-opioid receptor agonist, and as a norepinephrine and serotonin reuptake inhibitor, it is a central acting analgesic with peripheral and local analgesic effects. Its opioid and non-opioid mechanisms are thought to act synergistically on descending inhibitory pathways in the central nervous system [11]. TRAM’s analgesic efficacy is complemented by a long duration of action (half-life approximately 6 h) and by a safety profile that favors TRAM over other opioids [12].
A fixed dose combination (FDC) of DKP trometamol, a fast-acting NSAID, and TRAM hydrochloride, a long-lasting opioid, has been recently developed to generate multimodal analgesia at lower and better tolerated doses than those of the single agents used alone [13,14,15]. TRAM/DKP FDC offers several important advantages including proven efficacy and tolerability with a 25% overall reduction in the opioid dosage, improved compliance, and a convenient mode of administration [3].
The DAVID study compared the combination of TRAM 75 mg and DKP 25 mg (TRAM/DKP) with TRAM 75 mg and paracetamol 650 mg (TRAM/paracetamol) in moderate to severe pain [16]. Results showed that TRAM/DKP is effective and superior to TRAM/paracetamol in relieving moderate to severe acute pain following surgical removal of an impacted lower third molar, with a faster onset of action, greater and durable analgesia, and a favorable safety profile [16].
To further explore if the severity of pain intensity (PI) at baseline impacted on the analgesic efficacy and on the maintenance of analgesic response of the two fixed-dose combinations (TRAM/DKP vs TRAM/paracetamol), the results of the DAVID study were analyzed stratifying patients by baseline PI.
Methods
Trial Design
The DAVID study was a multicenter, randomized, double-blind, double-dummy, parallel-group, placebo and active-controlled, single-dose, phase IIIb trial conducted in 18 centers in five countries (Hungary, Italy, Poland, Spain, and the UK) [16]. The participation of each patient in the study lasted for approximately 3 weeks, encompassing: (i) a screening period (within 2 weeks before randomization), including the outpatient surgical extraction of at least one impacted lower third molar and a 4-h post-surgery qualification period; (ii) randomization and treatment administration (day 1, t0), followed by an 8-h efficacy assessment period; (iii) end of study visit (6 ± 1 days after randomization) [16].
During the qualification period, patients rated their post-surgical PI on an electronic diary using an 11-point numerical rating scale (NRS) ranging from 0 (no pain) to 10 (worst pain). Patients experiencing moderate to severe pain (defined as NRS-PI ≥ 4) were randomized with a 2:2:1 ratio to a single oral dose of three possible treatment arms: TRAM/DKP 75 mg/25 mg, TRAM/paracetamol 75 mg/650 mg, or placebo. The DAVID study was designed in line with the current academic [17] and regulatory [18] recommendations for acute pain trials. Dose selection of TRAM/DKP and TRAM/paracetamol was based on the posology recommended in the current summary of product characteristics (European package insert) of each drug for the initial treatment of moderate to severe acute pain [19, 20].
Ibuprofen 400 mg was available as a rescue medication (RM) during the 8-h post-dose assessment period, up to a maximum of two tablets at a minimum interval of 4 h [16].
The study was conducted in accordance with the principles of Good Clinical Practice and the Declaration of Helsinki. The study was approved by all the concerned competent authorities and ethics committees. Patients provided their written consent to participate in the study.
Blinding
Randomization was performed through Interactive Voice/Web Response System according to a computer-generated randomization sequence. Participants, healthcare providers, medical monitors, other personnel involved in the conduction of the trial, data collectors, and biometricians were unaware of the treatment that participants were receiving. Moreover, double-blind conditions were secured by using a double dummy technique; the study dose consisted of one tablet (containing TRAM/DKP 75 mg/25 mg or placebo) plus two tablets (containing TRAM/paracetamol 37.5 mg/325 mg or placebo).
Patients
Healthy adult patients (over 18 years of age) scheduled to undergo outpatient surgical extraction of at least one fully or partially impacted lower third molar requiring bone manipulation were included in the trial. Criteria for randomization included postoperative pain of moderate to severe intensity (NRS ≥ 4) within the 4-h qualification post-surgery period. Inclusion and exclusion criteria and other study restrictions were based on the reference safety information of both drug combinations [19, 20] and were described in detail in a previous publication [16].
For the purpose of the present subgroup analysis, enrolled patients were stratified according to baseline NRS-PI score ≥ 4, 5, 6, 7, and 8, and aggregated in two groups, according to the presence of moderate (NRS-PI ≥ 4 to ≤ 6) or severe (NRS-PI > 6) baseline PI.
Efficacy Evaluation
Evaluation of efficacy was based on data entered by patients in electronic diaries (eDiary). The following measures of analgesia were performed: (i) pain relief (PAR) measured on a 5-point verbal rating scale (VRS) (0 = “no relief”, 1 = “a little (perceptible) relief”, 2 = “some (meaningful) relief”, 3 = “lot of relief”, 4 = “complete relief”) at the predefined post-dose time points (15 min, 30 min, 1 h, 1.5 h, 2 h, 4 h, 6 h, and 8 h); (ii) PI measured on an 11-point NRS at baseline and at the same predefined post-dose time points. The onset of analgesia was documented using the double stopwatch method over a 2-h period post-dose: following treatment, two stopwatches were automatically activated in the eDiary. Patients were instructed to stop the first stopwatch when they felt “first perceptible” PAR (FPPAR, i.e., at the moment they first felt any PAR) and the second when they experienced a “meaningful” PAR (MPAR, i.e., when the relief from pain became meaningful to them). An overall assessment of the study medication was reported through patient global evaluation (PGE) on a 5-point VRS (1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent) at the end of the 8-h assessment period or immediately before the RM intake. The number of patients using RM and the time to first intake of RM were also evaluated [16].
The primary efficacy endpoint was total PAR over 6 h (TOTPAR6) calculated as the weighted sum of the PAR scores. TOTPAR6 was analyzed in patients stratified according to the baseline PI-NRS score, or aggregated into the moderate or severe baseline PI groups.
Secondary efficacy endpoints included the time course of mean PAR and PI scores over 8 h; TOTPAR over 2, 4, and 8 h post-dose; sum of pain intensity difference (SPID) over 2, 4, and 8 h; percentage of responders in terms of PAR or PI reduction, namely patients who achieved at least 50% of max TOTPAR or at least 30% of PI reduction versus baseline at pre-specified time points over 8 h; time to confirmed FPPAR (i.e., time to FPPAR if confirmed by experiencing MPAR); time to MPAR; PGE at 8 h or whenever the patient used RM; time of first intake of RM since study drug intake; and percentage of patients using RM at 2, 4, and 8 h [16].
All secondary endpoints were assessed in the present analysis in patients aggregated into the moderate or severe baseline PI groups.
In addition, the number needed to treat (NNT) for at least 50% pain relief over 6 h and 8 h vs placebo was calculated for the moderate or severe baseline PI groups.
Safety Evauation
Safety evaluation was based on the incidence, seriousness, intensity, and causal relationship of treatment-emergent adverse events (TEAEs). The occurrence of clinically significant changes post-dose versus the baseline in the physical examination, vital signs (VS; blood pressure and heart rate), and laboratory safety tests (hematology, biochemistry, and urinalysis) were also assessed [16]. In the present analysis, safety evaluations were performed in patients aggregated into the moderate or severe baseline PI groups.
Statistical Methods
The sample size was calculated for the original overall non-inferiority analysis between the active treatment groups and the superiority of active groups over placebo for sensitivity purposes [16]. No formal sample size calculation was performed for the analysis of the baseline PI groups. All efficacy variables were descriptively analyzed and tested as follows: NRS-PI, SPID, and TOTPAR (continuous variables) were analyzed by analysis of covariance (ANCOVA) model including terms of treatment and the baseline PI as covariates; PAR and PGE (categorical variables) were analyzed by Wilcoxon rank-sum test; percentage of responders and percentage of patients who required RM were tested using a chi-squared (χ2) test. Time to first use of RM and time to confirmed FPPAR and MPAR were assessed using a log-rank test. All analyses were performed in SAS V.9.3 (SAS) software [16].
The method of “last observation carried forward” was applied among patients who missed more than one consecutive data input; otherwise, the missing value was replaced by the mean of the two non-missing data collected before and after the missing one. This procedure was applied to all efficacy outcomes. After RM intake, PI returned to its baseline level and PAR to zero (“no relief”) for all subsequent time points (i.e., baseline observation carried forward) [16].
Adverse drug reactions (ADRs) were coded using the MedDRA dictionary. The incidence of each ADR was summarized by system organ class (SOC), preferred term (PT), treatment and baseline PI group. Safety variables were analyzed by descriptive statistics [16].
The subgroup analysis was performed on randomized patients stratified according to their baseline PI.
Results
Study Population
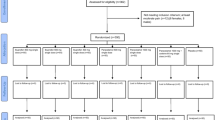
Of a total of 792 patients that were screened, 654 were randomized and received study treatment. One patient was excluded from any analysis for being less than 18 years old. Another patient qualified for the study initially (NRS > 4) but reported a lower value at baseline (NRS-PI = 3) and was therefore not included in this analysis (Fig. 1). The moderate and severe baseline PI groups contained 508 (77.8%) and 144 (22.1%) patients, respectively (Table 1).
Participant flow chart of study analysis of baseline pain intensity (PI) groups. *One patient was excluded from all analyses being aged less than 18 years; another patient was excluded from the analysis of baseline PI groups having reported a baseline (t0) PI-NRS < 4. TRAM/DKP tramadol/dexketoprofen, TRAM/Paracetamol tramadol/paracetamol
Demography and baseline characteristics are summarized in Table 1. Overall, the different treatment groups were comparable: gender distribution by treatment was homogeneous in the moderate baseline PI group (around 60% female across groups) but showed high variability in the severe baseline PI group (percentage of women ranging from 50.8% to 72.4%). Mean (standard deviation; SD) age was similar in both the moderate and severe baseline PI groups (26.8 [7.93] and 27.2 [7.22], respectively). Most patients in all groups were of Caucasian ethnicity (around 90%). The mean (SD) baseline PI was 5.0 (0.74) in the moderate group and 7.7 (0.82) in the severe group.
Efficacy Results
Primary Endpoint
The mean (SD) TOTPAR6 (primary endpoint) reported by patients in the overall TRAM/DKP group (13 [7.0]) was significantly superior (p < 0.0001) compared to the TRAM/paracetamol and placebo groups (9.2 [7.7] and 1.9 [3.9], respectively) (Table 2), as previously reported [16].
The analgesic efficacy of TRAM/DKP evaluated by TOTPAR6 remained steady across all baseline PI-NRS cutoff groups. In contrast, TRAM/paracetamol analgesic efficacy showed a marked and progressive decrease as baseline PI-NRS cutoffs increased (Fig. 2).
Considering the baseline PI groups, patients treated with TRAM/DKP reported significantly (p < 0.0001) higher TOTPAR6 values in both the moderate (12.9 [7.12]) and severe (13.4 [6.37]) baseline PI groups compared with patients in the TRAM/paracetamol (9.7 [7.67] and 7.0 [7.27)], respectively) and placebo groups (2.1 [4.10)] and 1.5 [3.08], respectively) (Table 2).
Secondary Endpoints
The superiority of TRAM/DKP was achieved in both baseline PI groups in terms of PAR summary measures (TOTPAR 2, 4, 6, and 8 h post-dose). The mean values obtained with TRAM/DKP were significantly higher than those obtained with TRAM/paracetamol at all evaluated time points in either moderate or severe baseline PI groups (p ≤ 0.0003; Supplementary Table 1 and Fig. 3).
Mean (SD) of total pain relief (TOTPAR) over 2, 4, 6, and 8 h post-dose for tramadol/dexketoprofen (TRAM/DKP), tramadol/paracetamol (TRAM/paracetamol), and placebo in baseline PI moderate group (a) and in baseline PI severe group (b). *Statistically significant TRAM/DKP versus TRAM/paracetamol (p < 0.0001). †Statistically significant (p = 0.0003). TOTPAR6 was the primary endpoint of the study
The time course of the mean PAR (Fig. 4) and PI (Fig. 5) showed that TRAM/DKP provided a more rapid onset of action compared with TRAM/paracetamol, with statistically significant differences observed after 30 min post-dose in both baseline PI groups. In the moderate baseline PI group, the statistically significant difference between TRAM/DKP- and TRAM/paracetamol-treated patients was maintained for up to 4 h in terms of PAR (Fig. 4a) and 6 h in terms of PI (Fig. 5a). Among patients with severe baseline PI, the statistically significant difference was observed up to 6 h for PAR (Fig. 4b) and up to 4 h for PI (Fig. 5b).
Time course of mean pain relief (PAR) over 8 h for tramadol/dexketoprofen (TRAM/DKP), tramadol/paracetamol (TRAM/paracetamol), and placebo with PAR measured on a 5-point verbal rating scale (PAR-VRS, ranging from 0 = “no relief” to 4 = “complete relief”) in baseline pain intensity (PI) moderate group (a) and in baseline PI severe group (b). The area under the curve for pain relief at a given time point corresponds to TOTPAR at the same time point. *Statistically significant TRAM/DKP versus TRAM/paracetamol (p < 0.0001); †statistically significant TRAM/DKP versus TRAM/paracetamol (p = 0.0205); ‡Statistically significant TRAM/DKP versus TRAM/paracetamol (p < 0.05)
Time course of mean pain intensity (PI) over 8 h for tramadol/dexketoprofen (TRAM/DKP), tramadol/paracetamol (TRAM/paracetamol), and placebo with PI measured on 11-point numerical rating scale (PI-NRS) ranging from 0 (no pain) to 10 (worst pain) in baseline PI moderate group (a) and in baseline PI severe group (b). *Statistically significant TRAM/DKP versus TRAM/paracetamol (p < 0.0001); †statistically significant TRAM/DKP versus TRAM/paracetamol (p < 0.05); ‡statistically significant TRAM/DKP versus TRAM/paracetamol (p = 0.0147). Dashed lines representing the threshold for “minimal pain relief”, “much improvement”, and “very much improvement”, calculated according to Cepeda et al. [23], are included as a reference
Accordingly, SPID 2, 4, 6, and 8 h post-dose of TRAM/DKP were significantly higher than those obtained in the TRAM/paracetamol group at all evaluated time points in either moderate or severe baseline PI groups (p ≤ 0.0006; Table 3 and Supplementary Fig. 1).
Regarding the percentage of responders in terms of PAR (patients achieving at least 50% of the theoretical maximum TOTPAR), the best results were detected in patients treated with TRAM/DKP, in both the moderate (68.4% were responders at 2 h, 69.4% at 4 h, 59.2% at 6 h, and 49.5% at 8 h) and severe baseline PI groups (81.0% were responders at 2 h, 77.8% at 4 h, 65.1% at 6 h, and 42.9% at 8 h). Conversely, in TRAM/paracetamol-treated patients, the percentages of responders were always lower, in both the moderate (45.7% were responders at 2 h, 45.2% at 4 h, 40.5% at 6 h, and 36.7% at 8 h) and the severe baseline PI groups (38.5% were responders at 2 h, 34.6% at 4 h, and 30.8% at 6 and 8 h). All differences between treatment groups were statistically significant (except for severe baseline PI group at 8 h; Supplementary Table 2 and Fig. 6).
Percentage of responders in terms of pain relief (patients who achieved at least 50% of theoretical maximum total pain relief [TOTPAR]) over 2, 4, 6, and 8 h post-dose for tramadol/dexketoprofen (TRAM/DKP), tramadol/paracetamol (TRAM/paracetamol), and placebo in baseline pain intensity (PI) moderate group (a) and in baseline PI severe group (b). *Statistically significant TRAM/DKP versus TRAM/paracetamol (p < 0.0001). †Statistically significant (p = 0.0002); ‡statistically significant (p = 0.0091)
Similarly, considering the percentage of responders in terms of PI reduction (patients achieving at least 30% of PI reduction vs baseline), the best results were detected in patients treated with TRAM/DKP, with a statistically significant difference in the moderate baseline PI group up to 6 h and in the severe baseline PI group up to 4 h (Table 4 and Supplementary Fig. 2).
In terms of PGE, a higher percentage of patients rating the study drug as “good”, “very good”, or “excellent” was observed in the TRAM/DKP in both moderate (80.1%) and severe (84.1%) baseline PI groups, with a statistically significant difference compared with patients treated with TRAM/paracetamol (59.5% and 44.2% in the moderate and severe baseline PI groups, respectively; Supplementary Table 3 and Fig. 7). The distribution of PGE categories by baseline PI group and treatment is shown in Fig. 8.
Percentage of responders in terms of patient global evaluation (PGE, patients who rated the study drug as “good”, “very good”, or “excellent” at the end of the assessment period or whenever the patient used rescue medication) for tramadol/dexketoprofen (TRAM/DKP), tramadol/paracetamol (TRAM/paracetamol), and placebo by baseline pain intensity (PI) group *Statistically significant TRAM/DKP versus TRAM/paracetamol (p < 0.0001)
Percentage of patients who rated the treatment as “poor”, “fair”, “good”, “very good”, or “excellent” on patients’ global evaluation (PGE) at the end of the assessment period or whenever they used rescue medication for tramadol/dexketoprofen (TRAM/DKP), tramadol/paracetamol (TRAM/paracetamol), and placebo in baseline pain intensity (PI) moderate group (a) and in baseline PI severe group (b)
When the onset of analgesia was evaluated with the double stopwatch method, it was significantly faster in the TRAM/DKP group than in the TRAM/paracetamol group in both baseline PI groups. In the moderate baseline PI group, the median (95% confidence interval [CI]) times to confirmed FPPAR and MPAR after single dose of TRAM/DKP were 22 (18, 25) and 43 (35, 49) min, respectively, compared to the TRAM/paracetamol group with 27 (23, 27) and 52 (47, 57) min, respectively. Log-rank test showed a statistically significant difference (p = 0.0034 and p = 0.0018, respectively). In the severe baseline PI group, the median (95% CI) times to confirmed FPPAR and MPAR after a single dose of TRAM/DKP were 18 (13, 25) and 33 (28, 44) min, respectively, compared with 27 (15, 49) and 57 (49, 87) min, respectively, in the TRAM/paracetamol group. Log-rank test showed a statistically significant difference (p = 0.0010 and p < 0.0001, respectively) (Supplementary Table 4).
Fewer patients treated with TRAM/DKP vs TRAM/paracetamol used RM in both the moderate (6.6% vs 17.1% within 2 h, 13.8% vs 32.4% within 4 h, 30.6% vs 42.4% within 6 h, and 48.0% vs 52.4% within 8 h) and severe baseline PI groups (7.9% vs 34.6% within 2 h, 14.3% vs 51.9% within 4 h, 41.3% vs 59.6% within 6 h, and 58.7% vs 65.4% within 8 h). The differences were statistically significant up to 6 h in the moderate baseline PI group and up to 4 h in severe baseline PI group (Table 5).
The median (95% CI) time to first use of RM in the severe baseline PI group was 417 (328, not achieved [NA]) min with TRAM/DKP and 233 (124, 414) min with TRAM/paracetamol; in the moderate baseline PI group the median time was NA with TRAM/DKP and it was 459 (369, NA) with TRAM/paracetamol. Log-rank tests were not statistically significant (Supplementary Table 5).
Finally, the NNT (95% CI) for at least 50% max TOTPAR at 6 h in the overall study population was 1.8 (1.6, 2.0) for TRAM/DKP and 2.9 (2.4, 3.5) for TRAM/paracetamol. The NNT (95% CI) at 8 h were 2.4 (2.0, 2.8) for TRAM/DKP and 3.3 (2.7, 4.3) for TRAM/paracetamol. In the moderate baseline PI group, the NNT at 6 h was 1.8 (1.6, 2.2) for TRAM/DKP and 2.8 (2.3, 3.6) for TRAM/paracetamol. The NNT at 8 h were 2.3 (1.9, 2.8) for TRAM/DKP and 3.3 (2.6, 4.3) for TRAM/paracetamol. In addition, in the severe baseline PI group, the NNT at 6 h was 1.5 (1.3, 1.9) for TRAM/DKP and 3.3 (2.3, 5.4) for TRAM/paracetamol. The NNT at 8 h were 2.5 (1.9, 3.8) for TRAM/DKP and 3.7 (2.4, 7.8) for TRAM/paracetamol (Supplementary Fig. 3).
Safety Results
Overall, 46 (9.1%) patients in the moderate baseline PI group experienced one or more adverse drug reactions (ADRs; 79 in total). In the severe baseline PI group, 7 (4.9%) patients experienced a total of 18 ADR. No serious ADR was recorded.
The most common ADRs in the moderate baseline PI active treatment groups (TRAM/DKP and TRAM/paracetamol) were vomiting (5.1% and 5.2%, respectively), nausea (4.6% and 3.8%, respectively), dizziness (3.1% and 3.8%, respectively), and somnolence (3.6% and 1.9%, respectively; Table 6). The most common ADRs in the severe baseline PI active treatment groups (TRAM/DKP and TRAM/paracetamol) were nausea (1.6% and 7.7%, respectively), vomiting (1.6% and 5.8%, respectively), somnolence (1.6% and 1.9%, respectively), and dizziness (0% and 9.6%, respectively). The incidence of ADRs was not increased in the severe baseline PI group (Table 7).
No clinically relevant change vs baseline was observed in the treatment groups in terms of VS or physical examination. No deaths occurred during the study.
Discussion
The results of the present subgroup analysis confirmed the superiority of TRAM/DKP combination over TRAM/paracetamol in terms of TOTPAR6 (primary endpoint) in patients with moderate and severe PI at baseline. TRAM/DKP (75/25 mg) proved to be equally effective in relieving pain in patients with moderate or severe pain, while TRAM/paracetamol analgesia decreased in patients with severe pain at baseline. The superiority of TRAM/DKP combination over TRAM/paracetamol was also confirmed in terms of all secondary endpoints evaluated in either patients with moderate or severe PI at baseline. In particular, the time course of PAR and PI indicated better efficacy with TRAM/DKP in terms of rapidity of onset and duration of the analgesic action. The percentage of responders, defined as at least 50% max TOTPAR at 2, 4, 6, and 8 h, was also significantly higher with TRAM/DKP vs TRAM/paracetamol in both moderate and severe PI groups at baseline (with the only exception of the baseline severe PI group at 8 h). Similarly, the percentage of responders defined as at least 30% PI reduction was significantly higher with TRAM/DKP at 2, 4, and 6 h in the moderate baseline PI group and at 2 and 4 h in the severe baseline PI. Accordingly, the overall PGE was higher in both baseline PI groups with TRAM/DKP vs TRAM/paracetamol. Time to confirmed FPPAR and MPAR was significantly shorter with TRAM/DKP in both baseline PI groups. The percentage of patients using RM was significantly lower with TRAM/DKP in the moderate baseline PI group within 2, 4, and 6 h and in the severe baseline PI group within 2 and 4 h. A very low clinical response for patients receiving placebo was identified in terms of TOTPAR (Fig. 3) and PI reduction (Supplementary Fig. 2), for both moderate and severe baseline PI subgroups. Accordingly, the overall PGE showed that most patients treated with placebo rated the study drug received as poor (Fig. 7) in both baseline PI subgroups. These results confirmed the superiority of TRAM/DKP combination over TRAM/paracetamol in terms of intensity, rapidity of onset, and duration of analgesia in patients with either moderate or severe PI at baseline.
A decrease in NRS-PI around 1 point (1.3 mm in a visual analog scale) has been usually considered the minimum clinically relevant in acute moderate to severe pain trials [21, 22]. However, according to Cepeda et al. [23], when baseline pain intensity is severe, larger changes in the NRS appear necessary to obtain a similar degree of pain relief. In their study, different thresholds for “minimal improvement”, “much improvement”, and “very much improvement” according to moderate or severe baseline PI were identified [23].
The threshold for “minimal improvement” was a 1.3-point decrease in PI for patients with moderate baseline PI [23]. The mean PI differences in our study were at least 1.3 points from 30 min time point up to 8 h with TRAM/DKP, and from 1 to 8 h with TRAM/paracetamol.
The threshold for “minimal improvement” was a 1.8-point decrease in PI for patients with severe baseline PI [23]. The mean PI differences in our study were at least 1.8 points from 30 min time point up to 8 h with TRAM/DKP, and from 1 to 6 h with TRAM/paracetamol.
In moderate baseline PI patients, a difference of 2.4 points corresponded to “much improvement” [23]: in our study, the mean PI differences were at least 2.4 points with TRAM/DKP from 1 to 4 h; and with TRAM/paracetamol from 1.5 to 2 h. A difference of 3.5 points corresponded to “very much improvement” [23]: in our study, the mean PI differences were at least 3.5 points with TRAM/DKP from 1.5 to 2 h; and with TRAM/paracetamol this PI difference value was not reached at any time point.
In severe baseline PI, a difference of 4.0 points corresponded to “much improvement” [23]: in our study, the mean PI differences were at least 4.0 points with TRAM/DKP from 1 to 4 h; and with TRAM/paracetamol this PI difference value was not reached at any time point. A difference of 5.2 points corresponded to “very much improvement” [23]: in our study, the mean PI differences were at least 5.2 points with TRAM/DKP from 1.5 to 2 h (Supplementary Table 6).
Accordingly, the percentage of patients using RM was significantly lower with TRAM/DKP than with TRAM/paracetamol. Although the differences between treatment groups were not statistically significant in terms of time to RM, it is noteworthy that in patients with moderate PI at baseline treated with TRAM/DKP the median time to RM was not achieved (vs about 7 h with TRAM/paracetamol) and was about 7 h (vs 4 h with TRAM/paracetamol) in patients with severe PI at baseline.
The NNT for at least 50% max TOTPAR over placebo at 6 and 8 h were consistently lower with TRAM/DKP than with TRAM/paracetamol and all differences were at least 1 point (except in the severe baseline PI group at 8 h = 0.9). Despite the limited number of patients, the NNTs presented remarkably narrow 95% CIs (Supplementary Fig. 3). Moreover, the NNTs in the overall group for TRAM/paracetamol were similar to those previously reported by Edwards et al. [24]. The lower NNT (and much narrow 95% CI) of TRAM/DKP vs TRAM/paracetamol makes it a superior oral treatment that is able to achieve optimal and consistent analgesia in moderate to severe acute pain.
In terms of safety, both treatments were well tolerated, and their safety profiles were fully in line with the previously reported studies. No increase in the incidence of ADRs was observed in the severe baseline PI group in comparison with the moderate baseline PI group.
Limitations
As the subgroup analysis was not originally included in the study protocol, no formal sample size estimation was performed, and no measures were implemented to guarantee a minimum percentage of patients with baseline severe PI. The overall severe baseline PI group encompassed 144 (22.1%) patients vs 508 (77.8%) patients in the moderate baseline PI group.
A recent clinical trial in dental impaction pain model performed similar subpopulation analyses with a severe baseline PI group of 102 patients [25]. In this study sample size was determined according to clinical, not statistical, criteria.
Acute pain trials in severe PI are rare and are usually performed at emergency departments. For example, one study examining the analgesic efficacy of four oral analgesic combinations in severe acute extremity pain included about 100 patients per group [26]. Another study in acute severe pain that examined the analgesic efficacy of an add-on single dose of intranasally administered sufentanil to the usual intravenous multimodal analgesia included 72 patients per group [27].
Moreover, safety data collected in a single-dose study are not sufficient to adequately characterize the safety profile of the study drugs.
Generalization
The dental impaction pain model is one of several recognized acute pain models and, as such, does not reflect the full scale of all acute pain models. Furthermore, the medications used are not the standard of care for treating acute dental pain in clinical practice. Nevertheless, owing to its sensitivity and reproducibility, dental impaction pain is the most studied and the reference model for assessing analgesia in proof-of-concept, dose-ranging, and relative efficacy studies [28]. Efficacy in the dental model is highly predictive of efficacy in later-stage models. The efficacy and the tolerability profile of the drugs used in this study were previously demonstrated in other models of pain using both the active comparator (TRAM/paracetamol) [29] and study drug (TRAM/DKP) [13, 14, 30].
Conclusion
The results of this subgroup analysis consistently confirmed the superior analgesic efficacy of TRAM/DKP over TRAM/paracetamol, in both primary and all secondary endpoints, irrespective of the baseline PI. Moreover, it showed that TRAM/DKP’s effective analgesia, unlike that of TRAM/paracetamol, was not decreased in patients with severe baseline PI. Analgesia with TRAM/DKP was faster and durable with a good safety profile.
References
National Pharmaceutical Council (NPC). Pain: current understanding of assessment, management, and treatments. Reston, VA: NPC, Joint Commission on Accreditation of Health Care Organization; 2001. https://www.npcnow.org/system/files/research/download/Pain-Current-Understanding-of-Assessment-Management-and-Treatments.pdf. Accessed 15 July 2019.
Viscusi ER, Skobieranda F, Soergel DG, et al. APOLLO-1: a randomized placebo and active-controlled phase III study investigating oliceridine (TRV130), a G protein-biased ligand at the µ-opioid receptor, for management of moderate-to-severe acute pain following bunionectomy. J Pain Res. 2019;12:927–43.
Varrassi G, Hanna M, Macheras G, et al. Multimodal analgesia in moderate-to-severe pain: a role for a new fixed combination of dexketoprofen and tramadol. Curr Med Res Opin. 2017;33:1165–73.
International Association for the Study of Pain. Management of postsurgical pain in adults. IASP. 2017. https://www.europeanpainfederation.eu/wp-content/uploads/2017/01/05.-Management-of-Postsurgical-Pain-Management.pdf. Accessed 15 July 2019
Gay C, Planas E, Donado M, et al. Analgesic efficacy of low doses of dexketoprofen in the dental pain model: a randomised, double-blind, placebo-controlled study. Clin Drug Invest. 1996;11:320–30.
McGurk M, Robinson P, Rajayogeswaran V, et al. Clinical comparison of dexketoprofen trometamol, ketoprofen, and placebo in postoperative dental pain. J Clin Pharmacol. 1998;38:46S-54S.
Walczak JS. Analgesic properties of dexketoprofen trometamol. Pain Manag. 2011;1:409–16.
Hanna H, Moon JY. A review of dexketoprofen trometamol in acute pain. Curr Med Res Opin. 2019;35:189–202.
Arfie A, Scotti L, Varas-Lorenzo C. Nonsteroidal anti-inflammatory drugs and risk of heart failure in four European countries: nested case–control study. BMJ. 2016;354:i4857.
Carne X, Rios J, Torres F. Postmarketing cohort study to assess the safety profile of oral dexketoprofen trometamol for mild to moderate acute pain treatment in primary care. Methods Find Exp Clin Pharmacol. 2009;31:533–40.
Vazzana M, Andreani T, Fangueiro J, et al. Tramadol hydrochloride: pharmacokinetics, pharmacodynamics, adverse side effects, co-administration of drugs and new drug delivery systems. Biomed Pharmacother. 2015;70:234–8.
Scott LJ, Perry CM. Tramadol a review of its use in perioperative pain. Drugs. 2000;60:139–76.
McQuay HJ, Moore RA, Berta A, et al. Randomized clinical trial of dexketoprofen/tramadol 25 mg/75 mg in moderate-to-severe pain after total hip arthroplasty. Br J Anaesth. 2016;116:269–76.
Moore RA, McQuay HJ, Tomaszewski J, et al. Dexketoprofen/tramadol 25 mg/75 mg: randomised double-blind trial in moderate-to-severe acute pain after abdominal hysterectomy. BMC Anesthesiol. 2016;16:9.
Moore RA, Gay-Escoda C, Figueiredo R, et al. Dexketoprofen/tramadol: randomised double-blind trial and confirmation of empirical theory of combination analgesics in acute pain. J Headache Pain. 2015;16:541.
Gay-Escoda C, Hanna M, Montero A, et al. Tramadol/dexketoprofen (TRAM/DKP) compared with tramadol/paracetamol in moderate to severe acute pain: results of a randomised, double-blind, placebo and active-controlled, parallel group trial in the impacted third molar extraction pain model (DAVID study). BMJ Open. 2019;9:e023715.
Cooper SA, Desjardins PJ, Turk DC, et al. Research design considerations for single-dose analgesic clinical trials in acute pain: IMMPACT recommendations. Pain. 2016;15:288–301.
Committee for Medicinal Products for Human Use (CHMP). Guideline on the clinical development of medicinal products intended for the treatment of pain. EMA/CHMP/970057/2011. 15 December 2016. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-development-medicinal-products-intended-treatment-pain-first-version_en.pdf. Accessed 15 July 2019.
Tramacet® (tramadol hydrochloride/paracetamol 37.5 mg/325 mg) UK SmPC. https://www.medicines.org.uk/emc/product/6630/smpc. Accessed 15 July 2019
Skudexa® (tramadol hydrochloride/dexketoprofen 75 mg/25 mg) UK SmPC. https://www.medicines.org.uk/emc/product/8849. Accessed 15 July 2019
Todd KH, Funk KG, Funk JP, et al. Clinical significance of reported changes in pain severity. Ann Emerg Med. 1996;27:485–9.
Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001;38:633–8.
Cepeda MS, Africano JM, Polo R, et al. What decline in pain intensity is meaningful to patients with acute pain? Pain. 2003;105(1–2):151–7.
Edwards JE, McQuay HJ, Moore RA. Combination analgesic efficacy: individual patient data meta-analysis of single-dose oral tramadol plus acetaminophen in acute postoperative pain. J Pain Symptom Manag. 2002;23:121–30.
López-Cedrún J, Videla S, Burgueño M, et al. Co-crystal of tramadol-celecoxib in patients with moderate to severe acute post-surgical oral pain: a dose-finding, randomised, double-blind, placebo- and active-controlled, multicentre, phase II trial. Drugs R D. 2018;18:137–48.
Chang AK, Bijur PE, Esses D, et al. Effect of a single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: a randomized clinical trial. JAMA. 2017;318:1661–7.
Lemoel F, Contenti J, Cibiera C, et al. Intranasal sufentanil given in the emergency department triage zone for severe acute traumatic pain: a randomized double-blind controlled trial. Intern Emerg Med. 2019;14:571–9.
Singla NK, Desjardins PJ, Chang PD. A comparison of the clinical and experimental characteristics of four acute surgical pain models: dental extraction, bunionectomy, joint replacement, and soft tissue surgery. Pain. 2014;155:441–56.
Sawaddiruk P. Tramadol hydrochloride/acetaminophen combination for the relief of acute pain. Drugs Today (Barc). 2011;47:763–72.
Montero Matamala A, Bertolotti M, Contini MP, et al. Tramadol hydrochloride 75 mg/dexketoprofen 25 mg oral fixed-dose combination in moderate-to-severe acute pain: sustained analgesic effect over a 56-h period in the postoperative setting. Drugs Today (Barc). 2017;53:339–47.
Acknowledgments
Funding
The study sponsor (Menarini Group) contributed to the study design, data analysis and manuscript preparation. The present analysis was funded by Menarini Group as well. Magdi Hanna confirms that he had full access to all the data in the study and had final responsibility for the decision to submit for publication. The journal’s Rapid Service Fee was funded by Content Ed Net.
Medical Writing Assistance
Editorial Assistance for manuscript preparation and submission was provided by Content Ed Net thanks to an unconditioned grant of the Menarini Group.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Magdi Hanna is a member of the scientific board of Menarini and has appeared in several educational symposiums for Menarini International, where he has received an honorarium. Giustino Varrassi is a member of the scientific Board of Menarini and has appeared in several educational symposiums for Menarini International, where he has received an honorarium. Moreover, he is member of the journal’s editorial board. Antonio Montero and Serge Perrot have nothing to disclose.
Compliance with Ethics Guidelines
The study was conducted in accordance with the principles of Good Clinical Practice and the Declaration of Helsinki. The study was approved by all the concerned competent authorities and ethics committees. Patients provided their written consent to participate in the study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hanna, M., Montero, A., Perrot, S. et al. Tramadol/Dexketoprofen Analgesic Efficacy Compared with Tramadol/Paracetamol in Moderate to Severe Postoperative Acute Pain: Subgroup Analysis of a Randomized, Double-Blind, Parallel Group Trial—DAVID Study. Pain Ther 10, 485–503 (2021). https://doi.org/10.1007/s40122-020-00228-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-020-00228-7