Abstract
Introduction
In the late 1990s multiple physicians and advocacy organizations promoted increased use of opioids for the treatment of acute, chronic and cancer pain. There has been an exponential growth in opioid prescribing in the last 20 years in the United States of America, in Australia, and in other developed Western countries. There are negative consequences associated with the liberal use of opioids. The primary aim of this population-based cohort study is to investigate the opioid-related death rate in New Zealand between 1 January 2008 and 31 December 2012. The secondary aims of this cohort study are: (1) to compare the opioid-related death rate per population in New Zealand in 2001/2002 with that between 2011/2012; (2) to investigate the number of opioid prescriptions in New Zealand between 2001 and 2012; (3) to compare the opioid-related death rate per population in New Zealand between 2001 and 2012 with the number of opioid prescriptions in New Zealand between 2001 and 2012.
Methods
Permission to access records from the Coronial Services Office in Wellington for 2008–2012 was acquired. Permission to access records for prescriptions containing opioids (dose and formulation) was obtained from the Pharmaceutical Collection.
Results
The rate of opioid-related deaths in New Zealand has increased by 33% from 2001 to 2012. More than half of the opioid-related deaths between 2008 and 2012 were unintentional opioid overdoses. Opioid analgesic deaths were most likely due to methadone, morphine and codeine prescribed by healthcare professionals. That 179 of these opioid-related deaths between 2008 and 2012 were unintentional opioid overdoses, and thus could have been avoided, is tragic. This study shows that there was a steady annual increases in opioid prescriptions in New Zealand from 2001 to 2012. This rise in opioid analgesic deaths was associated with the increases in the numbers of opioid prescriptions.
Conclusion
A multifaceted national public health approach is needed to bring together the various stakeholders involved with pain management, opioid dependence, opioid availability and opioid diversion. There needs to be a targeted approach to educate current and future medical practitioners regarding the appropriate use of opioid prescriptions for the management of pain, as well as a strengthening of primary, secondary and tertiary resources to support medical practitioners managing their patients who suffer with pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Opioids are used as primary analgesics to relieve acute, chronic and cancer pain. Historically, opioid analgesics were predominantly prescribed for acute pain and cancer-related pain [1]. In the 1980s international attention started focusing on the undertreatment of chronic pain. In 1986, Dr. Russel Portenoy stated that opioids were a “safe, salutary and more humane” treatment for patients with intractable non-malignant pain [2]. It was further asserted that the rate of addiction in chronic pain patients treated with opioids was low and that it was therefore unethical to restrict access to opioids necessary to relieve suffering due to chronic non-cancer pain [2, 3]. The potential adverse effects of chronic opioid use were played down with an overriding belief that opioids were safe, with no dosing threshold in the legitimate pain sufferer [1, 2]. These assertions, together with the availability of new synthetic opioids (e.g. oxycodone), the intense marketing strategies adopted by manufacturers and increased patient demand, have resulted in an exponential growth in opioid prescribing in the last 20 years [4, 5]. Between 1992 and 2012, opioid-dispensing episodes have increased by 15-fold (500,000 to 7.5 million) in Australia [6].
However, recent evidence-based research brings into question whether opioids are indeed effective against long-term chronic pain [7]. Only some patients with chronic non-cancer pain experience clinically significant pain relief with long-term opioid use and, in general, there is inconclusive evidence that opioid therapy improves quality of life and functioning in these patients [7]. In addition, opioids can create suffering with the risks of tolerance, dependence, abuse and opioid-related mortality and morbidity [1, 8]. No objective standard exists for levels of opioid consumption, and the rates of opioid prescription and use cannot be judged as adequate or excessive as there is no recognized baseline for a particular population [9]. Yet there appears to be higher rates of addiction and misuse with respect to opioid use in chronic pain treatment than previously envisaged [10]. There is a parallel relationship between the availability of prescription opioid analgesics through legitimate pharmacy channels and the diversion and abuse of these drugs and associated adverse outcomes [10]. Nonmedical use of prescription pain relievers in the USA is increasing, and there are comparable rises in hospital admissions for misuse [11].
In the USA, there is a rapidly emerging public health epidemic of prescription opioid-related mortality in patients with chronic non-cancer pain; more than 100,000 people have died from an unintentional overdose since policies changed in the late 1990s, and more than 16,000 people are dying from opioid-related causes annually [12, 13]. Opioid prescription drug overdose has surpassed motor vehicle collision as the leading cause of unintentional injury-related death in the USA [12, 14].
Deaths due to accidental poisoning (pharmaceutical opioids and illicit substances combined) in Australia increased from 151 in 2002 to 266 in 2011 [6]. The use of opioids is under increasing scrutiny, and many governmental agencies are focusing on strategies to manage what is seen to be an increasing epidemic of opioid use and abuse [10]. The trends in long-term opioid use and the problem of opioid-related mortality seen in the USA and Australia may not be reflected in New Zealand because of differences in healthcare systems, funding models and prescribing guidelines. In New Zealand, only deaths from opioid poisonings from 1 January 2001 to 31 December 2002 have previously been published, motivating the need for a fresh audit of the data [15].
Methods
Aims
The primary aim of this population-based cohort study was to investigate the opioid-related death rate in New Zealand between 1 January 2008 and 31 December 2012. The secondary aims were: (1) to compare the opioid-related death rate per population in New Zealand in 2001/2002 with that in 2011/2012; (2) to investigate the number of opioid prescriptions in New Zealand between 2001 and 2012; (3) to compare the opioid-related death rate per population in NZ between 2001 and 2012 with the number of opioid prescription in New Zealand between 2001 and 2012.
Data Sources
For this study, permission to access records from the Coronial Services Office in Wellington was acquired. Data from the Coroner (2008–2012 only) was taken from the year of notification of death and filtered for primary contribution. Deaths from opioid poisonings or overdoses in New Zealand from 1 January 2008 to 31 December 2012 were identified. A manual review of the coding of all cases in the dataset was undertaken to confirm that the cases were of relevance. The following incidents were excluded from the data set: cases which involved anaphylaxis; fatalities occurring due to complications during medical treatment, such as the administration of anesthetic during surgery.
A substance was considered to have made a primary contribution to a death where drug toxicity was noted within the cause of death or the primary object field in the National Coronial Information System code set, or where aspiration of gastric contents was noted in the cause of death and drug toxicity was noted anywhere in the cause of death. Additionally, if the death was noted as being contributed to by a combination of multiple coded drugs (such as ‘mixed drug toxicity’ or ‘multiple drug overdose’), the drugs that were part of the ‘multiple drug’ combination were recorded. The determination of the “intent” of the deceased person was subject to the individual determination of the Coroner investigating the fatality. The medical cause of death was based on the Forensic Pathologist’s individual opinion [16].
Statistics
The number of opioid-related deaths were summarized by year, gender, age and type of opioid. Mortality rates per million person-years were calculated by age and gender with 95% Poisson confidence intervals (CI) using, as the denominator, estimates of the New Zealand resident population provided by Statistics New Zealand [17]. Rate ratios with 95% mid-p exact confidence intervals were used to compare differences in mortality rates between females and males. The association between opioid prescriptions (per 100,000) and opioid-related deaths from 2001 to 2012 was estimated using a linear regression model. Analysis was performed using the R statistical package (R Foundation for Statistical Computing, Vienna, Austria).
Permission to access records for prescriptions containing opioids (dose and formulation) was obtained from the Pharmaceutical Collection. The Pharmaceutical Collection contains claim and payment information from pharmacists for subsidized dispensing processed by the Sector Services General Transaction Processing System. It is jointly owned by the Ministry of Health and the Pharmaceutical Management Agency (PHARMAC) in New Zealand [18]. Data were accessed to determine the sum of the opioid prescriptions between 2001 and 2012 only.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors. Ethical approval from the University of Otago’s Human Ethics Committee was obtained (Number HD15/036), and the appropriate statistical analyses were performed.
Results
From 2008 to 2012, a total of 325 deaths were primarily ascribed to opioid use (Table 1). Males had a higher rate of death than females (16.58 vs. 13.43 per 1,000,000 person-years; rate ratio 1.23; 95% Cl 0.99–1.54; p = 0.059). The highest incidence rate per 1,000,000 person years was in the 40–49 year age group as shown in Table 2. During this same period, there were 179 unintentional opioid overdoses, 110 intentional opioid overdoses and 37 opioid deaths from undetermined or other specified intent. The number of opioid deaths per year and type of opioid (2008–2012) is shown in Table 3. The opioids methadone, morphine, codeine were the most frequent causes of death.
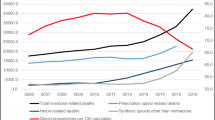
There was an increase in prescriptions issued in New Zealand for each type of opioid between 2001 and 2012 (see Fig. 1). Two types of opioid prescriptions were not included in this Fig. 1 due to the small total number of prescriptions issued between 2001 and 2012. These were buprenorphine hydrochloride (total of 88 prescriptions) and pentazocine (total of 815 prescriptions). Prescriptions for pethidine fell from 21,696 in 2001 to 8442 in 2012, while prescriptions for dextropropoxyphene declined after 2007 to nil in 2012.
The total number of prescription opioids rose from 686,063 in 2001 to 1,673,640 in 2012. Codeine and codeine plus paracetamol prescriptions increased from 225,723 in 2001 to 789,214 in 2012 (an increase of 250%). Tramadol prescriptions increased from 142,059 in 2010 (when first subsidized in New Zealand) to 331,126 in 2012 (an increase of 133% 2 years later). Morphine prescriptions increased from 136,619 in 2001 to 190,816 in 2012 (an increase of 40%). The dispensing of oxycodone prescriptions increased from 2836 in 2005 (when introduced into New Zealand) to 180,830 in 2012 (an increase of 6276% over a 7-year period). The number of methadone prescriptions increased from 49,951 in 2001 to 103,477 in 2012 (an increase of 107%). The number of fentanyl prescriptions increased from 217 in 2004 to 28,623 in 2012 (an increase of 13,090%).
The number of opioid deaths by primary opioid contribution (2001–2012) versus the total number of opioid prescriptions in New Zealand (2001–2012) is shown in Fig. 2. Between 2001 and 2012 there was an approximate linear relationship between the number of opioid prescriptions and the number of deaths by primary opioid contribution, such that an increase of 100,000 opioid prescriptions was associated with an additional 2.4 (95% CI 1.6–3.2, p < 0.001) deaths. Much of the increase in deaths occurred between 2002 and 2008, with only weak evidence of a linear increase by year from 2008 and 2012 (p = 0.07).
Discussion
Opioid-Related Death Rate and Characteristics
In New Zealand, the rate of opioid-related deaths in 2012 was 1.6 per 100,000. This is considerably less than the corresponding rate of 3.6 per 100,000 in Victoria, Australia in 2012 and 7.9 per 100,000 in 2013 in the USA [19, 20]. However, there is no room for complacency. The rate of opioid deaths in New Zealand is increasing at a significant rate. In 2001–2002, the rate of opioid-related deaths was 1.17 per 100,000 [15]; this rose to 1.60 per 100,000 in 2011–2012, reflecting a 33% increase in the 10-year interim period.
The number of deaths in New Zealand ascribed to be primarily due to use during the period 2008–2012 is 325. Of these, 110 deaths (34%) were from intentional opioid overdoses, and 179 (55%) were from unintentional opioid overdoses. The high number of unintentional overdoses is tragic as these are potentially avoidable. These data emphasize the need for educating both prescribers and the public alike. Similar to other countries, the rate of opioid poisoning deaths in New Zealand is marginally higher among men [20, 21]. The highest incidence rate per 1,000,000 person-years was in the 40–49 year age group, possibly due to a cohort effect arising from the aging baby-boomer generation. In addition, age and physical state could affect one’s capacity to metabolize medications.
In New Zealand from 2008 to 2012, opioid-related deaths were most frequently attributed to the opoids methadone, morphine, codeine and oxycodone. Clearly, the availability of drugs has an influence on the level of abuse. New Zealand was successful in the restriction of heroin supply in the 1970s and 1980s, probably as a result of unique factors, such as island isolation, a small market, and effective law enforcement and low corruption rates [22]. Our study shows a relatively high use of methadone and morphine relative to illicit heroin use, similar to results of other studies undertaken in New Zealand [15, 23]. The Pharmaceutical Management Agency (PHARMAC) in New Zealand regulates funding for drugs according to clinical effectiveness and cost-effectiveness, health needs, budget impact, direct cost to users and availability of alternative treatments [24]. The actions of PHARMAC have influenced the number of opioid-related deaths during the period 2008–2012. Slow-release oxycodone (OxyContin) became available in 2005, and since then, dispensing rates have increased significantly.
There were a significant number of deaths due to dextropropoxyphene in 2001–2002. Dextropropoxyphene was discontinued in New Zealand in December 2009; this resulted in limited access to this drug and a decrease in the number of deaths associated with its use. Access and use of opioids is established not only by physical availability and practical accessibility, but also by affordability [25]. Tramadol use in New Zealand increased rapidly after it became fully funded by PHARMAC in June 2010 [26].
The results of this study show that from 2001 to 2012 there appears to be a linear relationship between the number of deaths due to opioid use and the prescription rates. A similar trend of increasing opioid consumption accompanied by increasing rates of misuse and overdose have been observed in Australia and the USA [21, 27].
Opioid Prescription Rates and Characteristics
In New Zealand from 2011 to 2012 (2-year period) there were 3,233,946 prescriptions dispensed for opioid medicines, representing 36,583 prescriptions per 100,000 people. In comparison, there were 13,905,258 prescriptions dispensed for opioid medicines in Australia in the period 2013–2014 (2 years), representing 55,126 prescriptions per 100,000 people [28]. In the international framework, opioid consumption in New Zealand is less than that in Canada, the USA, Australia and the UK, respectively [29].
This study shows an exponential increase in total opioid prescriptions in New Zealand from 2001 to 2012 (686,063 in 2001 to 1,673,640 in 2012), driven mainly by an increase in codeine prescriptions. In other countries, opioid use has doubled over a similar period, particularly in high-income countries, such as those of North America, western and central Europe and Oceania [25]. A recent study has shown this trend is continuing beyond 2012, with an average of 16.4/1000 people in New Zealand receiving a strong opioid in 2015, a marginal increase from 2011 (14.3/1000) [30]. The dispensing rates of both strong and weak opioids in New Zealand have been shown to be higher for people of Caucasian origin (as compared to Māori, Pacific or Asian ethnicities) and higher for women and people aged ≥ 80 years [30]. Nearly half of all New Zealanders who received a strong opioid in 2015 had recently attended a public hospital as an inpatient or outpatient, suggesting many of these prescriptions are generated in the hospital setting [30].
The mortality rate per prescription for methadone, morphine and codeine has not changed markedly (Table 4). However, the number of prescriptions has increased, and so have the number of deaths. These data highlight the increase in deaths according to increased prescription of existing drugs and introduction of new drugs (Table 4).
Findings for Specific Drugs
Methadone
Methadone accounts for the highest number of opioid-related deaths in New Zealand. Methadone has been used as part of opioid substitution treatment (OST) for opioid dependence in New Zealand since the 1970s [31]. The increasing total number of methadone prescriptions is likely to be related to the steadily increasing number of OST patients in New Zealand since 1995 [31]. There were more than 5000 OST patients in 2012, and an increasing proportion of these patients were being managed in primary care [31]. Methadone constitutes a significant proportion of street opioid supply in New Zealand, and since methadone is primarily prescribed for OST, this may suggest insufficient dispensing controls [23]. Methadone prescription has been found to significantly decrease intravenous heroin use, which could contribute to the low rate of heroin overdoses in New Zealand [31]. Buprenorphine became subsidized by PHARMAC in July 2012 and has provided an alternative OST medication to methadone [31]. This is a positive step as buprenorphine has a reduced potential risk of overdose compared to methadone [32, 33]. It has been suggested that buprenorphine should be considered as the drug of first choice by clinicians treating patients with opioid dependence, especially polydrug users [19].
Codeine
Codeine-related deaths in New Zealand rose markedly from 1.5 per million people in 2001/2002 to 4.0 per million in 2012. In Australia, codeine-related deaths increased from 3.5 per million in 2000 to 8.7 per million in 2009, and deaths from accidental overdoses were found to be more common (48.8%) than intentional deaths (34.7%) [34]. Severe harmful events have been described with codeine use, especially from the consumption of high doses of combination products, such as codeine/paracetamol and codeine/ibuprofen [35]. About 5% of the white population are ultra-rapid metabolizers, meaning that there is a higher conversion to morphine with an increased risk of adverse events, such as respiratory depression and fatal overdose [36, 37]. Codeine has been implicated in the postoperative deaths of children [36]. Research in Australia and overseas has shown that those individuals who misuse codeine tend to be better educated and more often employed and tend not to use illicit drugs [38]. In Australia from 1 February 2018 onwards, analgesics containing codeine will be available only on prescription [39].
Codeine use in New Zealand is difficult to quantify, as it is relatively inexpensive and low-dose codeine can be obtained in combination with paracetamol over-the-counter (OTC) without a prescription. New Zealand would need to consider its own figures in light of the Australian data and act accordingly.
Oxycodone
Oxycodone made its appearance in New Zealand in 2005 and was promoted as an alternative to morphine. It was preceded and supported by a driven and costly advertising campaign that resulted in the rapid annual rise in oxycodone prescriptions [30]. It was marketed as having a low potential for misuse, which was subsequently shown to be incorrect [40]. The exponential increase in the number of prescriptions of slow-release oxycodone since its introduction has been matched by an increase in oxycodone-related deaths. The overall number of oxycodone-related deaths in New Zealand and Australia is currently relatively low. The proportion of frequent injecting-drug users in New Zealand who had used oxycodone at any time increased from 21% in 2008 to 54% in 2012 [41].
Tramadol
Tramadol is a multimodal analgesic, with only a weak mu opioid effect from its metabolites. It has only been fully funded in New Zealand since June 2010. When used appropriately, tramadol provides important medical benefits. Evidence appears to indicate that tramadol is associated with a low potential for misuse, abuse and dependency [42]. However, it can have serious health consequences when taken without medical supervision, in larger amounts than prescribed or in combination with illicit drugs, alcohol, or other prescription or OTC medications [43].
Fentanyl
From February 2011 fentanyl patches became fully funded in New Zealand without special authorization [44]. Rates of fentanyl use are currently low, but are increasing. Fentanyl use increased from 217 prescriptions in 2004 to 28,623 in 2012, which reflects a 132-fold increase. This increase is probably due to an increasing supply of synthetic opioids and the use of fentanyl patches in residential homes to treat chronic non-malignant pain (CNMP). The risk of fatality with fentanyl patches arises when they are given to opioid-naïve patients [45]. In New Zealand there were only three deaths from fentanyl in 2011–2012.
Preventative Measures to Limit Overprescribing and Mitigate Risk
Mitigation of risk is important to encourage safer prescribing of opioids and to prevent opioid abuse, dependence and death. Appropriate evaluation, documentation, screening and risk stratification are indicated, starting from the initiation of the opioid therapy and continuing through to its discontinuation [5]. There are a wide range of social, psychological, and physical treatment options available for patients with CNMP. Combinations of non-opioid analgesics and non-pharmacological treatments are the mainstay of treatment for CNMP. Opioids should be titrated slowly, with frequent dispensing and close monitoring for signs of misuse [46]. If opioid therapy is deemed to be necessary, patients should be prescribed weaker opioids, such as tramadol, before being started on the stronger ones. Codeine should not be prescribed to breastfeeding mothers due to the risks of toxicity in rapid metabolizers [47]. Fentanyl should only be prescribed to opioid-tolerant patients [48]. Methadone has a long and variable half-life and should not be used for acute pain or breakthrough pain [48]. The opioid should be tapered if the patient’s pain remains severe despite an adequate trial of opioid therapy [46].
General practitioners need to be made aware of the predictors of opioid overdose, which include a mean daily oral morphine-equivalent dose of >100 mg per day, mental health disorders, concomitant use of benzodiazepines and antidepressants and substance use disorders (alcohol) [46, 48]. Care needs to be taken when prescribing opioids for adolescents, who are at high risk of opioid overdose, misuse and addiction [46]. In the elderly, overdose can be minimized through lower initial doses, slower titration, benzodiazepine tapering and careful patient education [46].
Other key prevention strategies include educating the general population on the use of tamper-resistant formulations and the danger of combining opioids (such as oxycodone and buprenorphine) with low-dose naloxone, expanding availability and community access to naloxone and carrying out prescription monitoring programmes [20, 49]. Current evidence on extended-release naltrexone is more encouraging as this drug is not subject to misuse or diversion [50]. Nation-wide prescription monitoring programmes should be implemented to facilitate early detection. In New Zealand more use needs to be made of the information on prescribing collected by the Pharmaceutical Collection. Public health agencies, medical examiners and coroners and law enforcement agencies should work collaboratively to improve the detection of and response to drug overdoses related to illicit opioids [20].
Limitations of the Study
The dataset from the Coroner does not claim to be representative of all relevant cases within the time period specified. This may have been due to missing data and occasional processing and coding errors. The Query Design Search Screen was used to identify cases of relevance. There were some limitations as coded fields were not completed until closure of the case and the extent of the information contained in the text reports varied. The determination of the “intent” of the deceased person was subject to the individual determination of the Coroner investigating the fatality. The medical cause of death was based on the Forensic Pathologist’s individual opinion. Another limitation of this and most studies is the lack of distinction between death due to prescription-related opioids and that due to illicit opioids.
Conclusion
Dr. Portenay, who originally promoted the liberal use of opioids in the 1980s, has subsequently stated that in the light of further research it would appear “that the benefits of opioids had been overstated and the risks glossed over” [51]. There is ample evidence of an emerging public health problem in New Zealand, related to inappropriate opioid prescribing patterns.
From 2008 to 2012, a total of 325 deaths were primarily ascribed to opioid use, with a higher rate of death among males than among females: 16.58 vs. 13.43 per 1,000,000 person-years (rate ratio 1.23; 95% Cl 0.99–1.54; p = 0.059). One of the predictors of opioid overdose is the male sex [20, 21]. In 2001–2002, the rate of opioid-related deaths was 1.17 per 100,000 [15]. This has risen to 1.60 per 100,000 in 2012, reflecting a 33% increase in the 10-year interim period. This is in line with the situation in other First World countries.
The first exposure of most opioid abusers to the opioid began with a legitimate prescription for pain [52]. A sharp increase in the prescription of opioids has been associated with increases in opioid overdose [53]. The results of the present study confirm this trend. There have been incremental annual increases in opioid prescriptions in New Zealand from 2001 to 2012, with a more than doubling of the total number of prescriptions issued from 2001 to 2012. This rising trend in opioid prescription rate is associated with a corresponding rise in deaths from opioid analgesics. The fact that more than half (179) of the opioid-related deaths between 2008 and 2012 were unintentional opioid overdoses and could have been avoided is tragic. Opioid analgesic deaths were most likely due to methadone, morphine and codeine prescribed by healthcare professionals. The significant rise in prescriptions of oxycodone, codeine and fentanyl-related products are of growing concern. This concern can be addressed by ensuring that providers perform risk assessments, are perceptive of medication risks, avoid excessive dependence on opioids and adequately educate and monitor patients [54].
A multifaceted national public health approach is needed to bring together the various stakeholders involved with pain management, opioid dependence, opioid availability and opioid diversion. There needs to be a targeted approach to educate current and future medical practitioners in the appropriate use of opioid prescriptions for the management of pain, as well as a strengthening of primary, secondary and tertiary resources to support medical practitioners managing their patients suffering with pain.
References
Cheatle MD. Prescription opioid misuse, abuse, morbidity, and mortality: balancing effective pain management and safety. Pain Med. 2015;16[Suppl 1]:S3–8.
Portenoy RK, Foley KM. Chronic use of opioid analgesics in non-malignant pain: report of 38 cases. Pain. 1986;25(2):171–86.
Porter J, Jick H. Addiction rare in patients treated with narcotics. N Engl J Med. 1980;302(2):123.
Kanouse AB, Compton P. The epidemic of prescription opioid abuse, the subsequent rising prevalence of heroin use, and the federal response. J Pain Palliat Care Pharmacother. 2015;29(2):102–14.
Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: part I—evidence assessment. Pain Phys. 2012;15[3 Suppl]:S1–65.
Blanch B, Pearson SA, Haber PS. An overview of the patterns of prescription opioid use, costs and related harms in Australia. Br J Clin Pharmacol. 2014;78(5):1159–66.
Noble M, Treadwell JR, Tregear SJ, Coates VH, Wiffen PJ, Akafomo C, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;1:Cd006605.
Stein C. Opioid receptors. Annu Rev Med. 2016;67:433–51.
Seya MJ, Gelders SF, Achara OU, Milani B, Scholten WK. A first comparison between the consumption of and the need for opioid analgesics at country, regional, and global levels. J Pain Palliat Care Pharmacother. 2011;25(1):6–18.
Dart RC, Severtson SG, Bucher-Bartelson B. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(16):1573–4.
Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363(21):1981–5.
Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers and other drugs among women—United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(26):537–42.
Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309(7):657–9.
Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011;81:1–8.
Reith D, Fountain J, Tilyard M. Opioid poisoning deaths in New Zealand (2001–2002). N Z Med J. 2005;118(1209):U1293.
National Coronial Information System (NCIS). CR15-19. 2007–2015. Southbank, Australia: NCIS
Statistics New Zealand. Population statistics. http://www.stats.govt.nz/browse_for_stats/population.aspx. Accessed 18 Mar 2017.
Ministry of Health. http://www.health.govt.nz/nz-health-statistics/national-collections-and-surveys/collections/pharmaceutical-collection. Accessed 2 Apr 2017.
Monheit B, Pietrzak D, Hocking S. Prescription drug abuse—a timely update. Aust Fam Physician. 2016;45(12):862–6.
Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50–51):1378–82.
Berecki-Gisolf J, Hassani-Mahmooei B, Clapperton A, McClure R. Prescription opioid dispensing and prescription opioid poisoning: population data from Victoria, Australia 2006 to 2013. Aust N Z J Public Health. 2017;41(1):85–91.
McMinn J. Opioid dependence, a life-threatening condition, is preventable. N Z Med J. 2014;127(1397):5.
Robinson G, Judson G, Loan R, Bevin T, O’Connor P. Patterns of prescription drug misuse presenting to provincial drug clinics. N Z Med J (Online). 2011;124(1336):62–7.
PHARMAC. About PHARMAC. https://www.pharmac.govt.nz/about/. Accessed 12 Apr 2017.
Berterame S, Erthal J, Thomas J, Fellner S, Vosse B, Clare P, et al. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet. 2016;387(10028):1644–56.
Best Practice Journal. Snippets: Safer prescribing of tramadol 2010. http://www.bpac.org.nz/BPJ/2010/June/snippets.aspx. Accessed 12 Apr 2017.
Weisberg DF, Becker WC, Fiellin DA, Stannard C. Prescription opioid misuse in the United States and the United Kingdom: cautionary lessons. Int J Drug Policy. 2014;25(6):1124–30.
Australian Commission on Safety and Quality in Health Care. Australian atlas of healthcare variation. chapter 5.1: Opioid medicines dispensing. https://www.safetyandquality.gov.au/wp-content/uploads/2015/11/SAQ201_06_Chapter5_v12_FILM_tagged_merged_5-1.pdf. Accessed 2 Apr 2017.
University of Wisconsin-Madison Pain & Policy Studies Group. Opioid consumption data. http://www.painpolicy.wisc.edu/opioid-consumption-data. Accessed 2 Apr 2017.
Davis A, Davis K, Gerard C, Goyal S, Jackson G, James C, et al. Opioid rain: opioid prescribing is growing and practice is diverging. N Z Med J. 2016;129(1440):11–7.
Deering D, Sellman JD, Adamson S. Opioid substitution treatment in New Zealand: a 40 year perspective. N Z Med J. 2014;127(1397):57–66.
Pirnay S, Borron SW, Giudicelli CP, Tourneau J, Baud FJ, Ricordel I. A critical review of the causes of death among post-mortem toxicological investigations: analysis of 34 buprenorphine-associated and 35 methadone-associated deaths. Addiction. 2004;99(8):978–88.
Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;2:Cd002207.
Roxburgh A, Hall WD, Burns L, Pilgrim J, Saar E, Nielsen S, et al. Trends and characteristics of accidental and intentional codeine overdose deaths in Australia. Med J Aust. 2015;203(7):299.
Nielsen S, Bruno R, Murnion B, Dunlop A, Degenhardt L, Demirkol A, et al. Treating codeine dependence with buprenorphine: dose requirements and induction outcomes from a retrospective case series in New South Wales, Australia. Drug Alcohol Rev. 2015;35:70–75.
Chidambaran V, Sadhasivam S, Mahmoud M. Codeine and opioid metabolism: implications and alternatives for pediatric pain management. Curr Opin Anaesthesiol. 2017;30(3):349–56.
Tverdohleb T, Dinc B, Knezevic I, Candido KD, Knezevic NN. The role of cytochrome P450 pharmacogenomics in chronic non-cancer pain patients. Expert Opin Drug Metab Toxicol. 2016;12(11)1303–11.
Nielsen S, Murnion B, Dunlop A, Degenhardt L, Demirkol A, Muhleisen P, et al. Comparing treatment-seeking codeine users and strong opioid users: findings from a novel case series. Drug Alcohol Rev. 2015;34(3):304–11.
Therapeutic Goods Administration. Codeine-containing medicines: Department of Health, Australian Government. http://www.tga.gov.au/. Accessed 12 Apr 2017.
Dyer O. Kentucky seeks $1bn from Purdue Pharma for misrepresenting addictive potential of oxycodone. BMJ. 2014;349:g6605.
Wilkins C, Jawalkar P, Parker K. Recent trends in illegal drug use in New Zealand, 2006-2012: findings from the 2006, 2007, 2008, 2009, 2010, 2011 and 2012 Illicit Drug Monitoring System (IDMS) 2013. http://www.whariki.ac.nz/massey/learning/departments/centres-research/shore/projects/illicit-drug-monitoring-system.cfm. Accessed 2 Apr 2017.
Radbruch L, Glaeske G, Grond S, Münchberg F, Scherbaum N, Storz E, et al. Topical review on the abuse and misuse potential of tramadol and tilidine in Germany. Subst Abuse. 2013;34(3):313–20.
Bush DM. Emergency department visits for drug misuse or abuse involving the pain medication tramadol. The CBHSQ report. Rockville: Substance Abuse and Mental Health Services Administration (US); 2013.
Best Practice Advocacy Centre Inc (BPAC). Snippets: fentanyl patches. Best Practice Journal 2010. http://www.bpac.org.nz/BPJ/2010/December/snippets.aspx. Accessed 12 Apr 2017.
Taghogho Agarin M, Andrea Trescot M, Aniefiok Agarin M. Reducing opioid analgesic deaths in America: what health providers can do. Pain Phys. 2015;18:E307–22.
Kahan M, Wilson L, Mailis-Gagnon A, Srivastava A. Canadian guideline for safe and effective use of opioids for chronic noncancer pain: clinical summary for family physicians. Part 2: special populations. Can Fam Physician. 2011;57(11):1269–76, e419–28.
Al-Adhami N, Whitfield K, North A. Changing prescribing culture—a focus on codeine postpartum. Arch Dis Child. 2016;101(9):e2.
Warner EA. Opioids for the treatment of chronic noncancer pain. Am J Med. 2012;125(12):1155–61.
Faculty of Pain Medicine Australian and New Zealand College of Anaesthetists. Recommendations regarding the use of opioid analgesics in patients with chronic non-cancer pain—position statement. http://www.fpm.anzca.edu.au/. 2015.
Connery HS. Medication-assisted treatment of opioid use disorder: review of the evidence and future directions. Harvard Rev Psychiatry. 2015;23(2):63–75.
Catan T, Perez E. A pain-drug champion has second thoughts. Wall Street J. 2012; December 17. http://www.wsj.com/articles/SB10001424127887324478304578173342657044604. Accessed 12 Apr 2017.
Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265–9.
Frenk SM, Porter KS, Paulozzi LJ. Prescription opioid analgesic use among adults: united States, 1999-2012. NCHS Data Brief. 2015;189:1–8.
Lamvu G, Feranec J, Blanton E. Perioperative pain management: an update for obstetrician-gynecologists. Am J Obstetr Gynecol. 2017. doi: 10.1016/j.ajog.2017.06.021
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Elspeth E. Shipton, Ashleigh J. Shipton, Jonathan A. Williman and Edward A. Shipton have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors. Ethical approval from the University of Otago’s Human Ethics Committee was obtained (Number HD15/036), and the appropriate statistical analyses were performed.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/52FBF06057E63193.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shipton, E.E., Shipton, A.J., Williman, J.A. et al. Deaths from Opioid Overdosing: Implications of Coroners’ Inquest Reports 2008–2012 and Annual Rise in Opioid Prescription Rates: A Population-Based Cohort Study. Pain Ther 6, 203–215 (2017). https://doi.org/10.1007/s40122-017-0080-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-017-0080-7