Abstract
Patients see their primary care physicians (PCPs) for a variety of medical conditions, chronic pain being one of the most common. An increased use of prescription medications (especially opioids) has led to an increase in adverse drug reactions and has heightened our awareness of the variability in response to medications. Opioids and other pain adjuvants are widely used, and drug–drug interactions involving these analgesics can be problematic and potentially lethal. Pharmacogenetics has improved our understanding of drug efficacy and response, opened doors to individual tailoring of medical management, and created a series of ethical and economic considerations. Since it is a relatively new field, genetic testing has not been fully integrated into the primary care setting. The purpose of this paper is to review the metabolism of commonly prescribed opioids, discuss the economic and ethical issues, and provide PCPs with an understanding of how to incorporate genetic testing into routine use to improve clinical practice and patient management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pain is one of the most common reasons that patients visit physicians in the primary care setting [1]. With a rapidly aging population, primary care physicians (PCPs) are seeing a higher incidence of chronic pain conditions. These patients are often plagued with multiple medical problems, which make their medication management more challenging. Pain medications are some of the most commonly prescribed drugs in the United States, with opioids continuing to be the mainstay of chronic pain management [2, 3]. Adjuvant therapies such as antidepressants, benzodiazepines, anti-inflammatory agents, or anticonvulsants can also be useful in managing pain, and many (if not most) pain patients may be treated with a combination of these medications. Therefore, PCPs must be increasingly aware of the potential risk for drug-to-drug interactions. Fatal adverse drug reactions have been reported to be the fourth leading cause of death in the USA [4]. In addition, the “trial-and-error” approach to prescribing medicine is costly and causes delays in effective care. As personalized medicine becomes more prevalent, these costly approaches to medical care will eventually become obsolete, and streamlined methods guiding therapeutic decisions will prevail.
One of the tools available for implementing a more personalized approach, with greater optimization of patient outcomes, is pharmacogenetic testing. Pharmacogenetics is a type of genetic test that assesses a patient’s risk of an adverse response or likelihood of responding to a given drug, thereby informing drug selection and dosing [5]. As the personalized medicine movement gains momentum, pharmacogenetic testing will be important across all medical specialties, with an emphasis in primary care, since a majority of all prescription drugs are written in this setting [6].
Pharmacogenetics is a relatively new field, and as yet it is only slowly being integrated into the primary care setting. Many PCPs are still not familiar with how to test, interpret, or apply this technology in clinical practice [7]. This paper serves as a primer for PCPs to enhance their understanding of pharmacogenetics, with a focus on opioid pain medications.
The article is based on previously conducted studies, and does not involve any studies of human or animal subjects performed by any of the authors.
Opioid Metabolism
To understand how opiates are metabolized, it is necessary to start with related terminology. Pharmacokinetics is the process by which the body absorbs, distributes, metabolizes, and excretes drugs, while pharmacodynamics describes the drug’s effects on the body at the cellular or receptor level [8].
Genetic polymorphism is the term for variations in the structure of genes, which includes structural changes such as deletion, duplication, and translocation. Each of these gene alterations is called an allele of the original gene (wild-type). Having two copies of the same allele is called a homozygous genotype, while having any combination of two different alleles is called a heterozygous genotype. A single-nucleotide polymorphism (SNP) is the most common altered gene form.
Patients can be classified by their genetic ability to metabolize a medication: a normal metabolizer (NM) responds as expected when given a medication and has two normal or “wild-type” alleles; an intermediate metabolizer (IM) can have partially active alleles or one fully defective allele; a poor metabolizer (PM) has two abnormal alleles with minimal gene activity; a rapid metabolizer (RM) has at least one highly active allele, and an ultra-rapid metabolizer (UM) can have many copies of the normal gene, leading to activity many times the baseline level [9].
These changes in alleles may have a significant effect on pain perception and opioid use. A retrospective chart review analyzed the DNA of female postoperative patients and concluded that smokers and those possessing the PM genotype were more likely to experience severe postoperative pain than other patients (71% vs. 26–28% in all the other groups combined), based on self-reported pain scores and opioid intake [10].
With the exception of morphine, oxymorphone, and hydromorphone, opioid metabolism is primarily mediated by the cytochrome P450 enzyme system located in the liver [11]. This enzyme system is extensively involved in the metabolism of drugs as well as other chemicals, foods, or toxins in the body. Although more than 30 CYP450 isoenzymes have been identified, seven of these are clinically important: CYP1A2, 2C8, 2C9, 2C19, 2D6, 2E1, and 3A4, whose presence and activity levels vary based on a variety of factors including race, ethnic background and tobacco abuse [9] as well as interactions with other medication, and other receptors, such as the opioid receptors [12].
Clinicians have always noted a wide variability in patient response to opioid pain medications. In the past, this has been attributed to differences in gender, body mass, or cultural factors influencing pain perception [13, 14]. However, genetics appears to play a larger role in the clinical efficacy of opioid medications than was previously thought, which is related to the high inter-individual variability in the activity level of the CYP system [15, 16]. Further discussion in this article will be limited to the isoenzymes with a significant impact on pain medication metabolism [9, 17].
CYP2D6
CYP2D6 is responsible for the metabolism of most of the commonly prescribed opiate medications, including codeine, tramadol, hydrocodone, and oxycodone. Decreases in CYP2D6 activity may lead to reduced conversion of prodrugs into their more active metabolites, causing inadequate analgesia and the need for increased opioid medication. Conversely, increased CYP2D6 activity can lead to elevated levels of active metabolites in the blood, increasing the risk of adverse outcomes (such as an overdose) [18]. At present, over 80 subtypes of the CYP2D6 allele have been identified, and their prevalence varies by race and ethnicity [9, 18]. Almost 10% of the white population lacks a good copy of this gene [19].
CYP2D6 metabolizes inactive codeine to its active form. morphine; inactive hydrocodone is metabolized into the active hydromorphone; active oxycodone is metabolized into the more active oxymorphone; and less active tramadol is metabolized into the more active o-desmethyltramadol [8]. A common clinical scenario is as follows: Codeine (a prodrug) is given to a patient who is a PM for the CYP2D6 gene. Because of this genetic makeup, the patient is unable to convert enough of the prodrug into its active form to obtain relief, and may be accused of drug-seeking if they complain of inadequate analgesia. If the patient is an RM or UM, they can experience a higher than expected level of sedation, addiction, and other systemic side effects at lower doses than standard metabolizers [18]. In a 2007 study, the area-under-the-curve (AUC) diagram of morphine concentration over time varied at least 30-fold between PM and UM patients taking codeine [18].
Tramadol is a weak mu opioid receptor agonist; however, CYP2D6 metabolizes the M1 metabolite (o-desmethyltramadol), which is many times more potent than the parent compound [20] and may cause adverse side effects in UMs [21]. Hydrocodone is a semi-synthetic codeine derivative, which is metabolized by CYP2D6 into hydromorphone, its active metabolite [19, 22]. Depending on patient classification (PM, UM, RM, etc.) and ratio of parent compound to active metabolite (as measured in urine), a large degree of variability in the clinical efficacy of this medication can be observed [9, 23].
Alternately, CYP2D6 may increase the fraction of inactive drug that is present. For example, oxycodone is active at the mu receptor [9]. Oxycodone is metabolized by CYP3A4 into noroxycodone, which has less than 1% of the activity of the parent compound. However, CYP2D6 subsequently converts that noroxycodone to noroxymorphone and then converts oxycodone to oxymorphone (dual metabolism); therefore, PM patients may note improved analgesia while using this medication [9], and UM or RM patients may paradoxically note reduced analgesic efficacy [15].
Forty-five women who had undergone C-sections were treated postoperatively with codeine, and their genetic CYP2D6 status was evaluated. The two PM patients noted no analgesia, and two of the three UMs noted immediate pain relief from the codeine, but they stopped the medication due to dizziness and constipation [24]. The authors noted that the response to codeine matched their genetic status.
CYP3A4 and CYP2B6
The CYP3A4 system regulates the excretion of fentanyl, methadone, and buprenorphine. PM patients or those who are taking oral CYP3A4 inhibitors (e.g. grapefruit juice, verapamil, diltiazem, clarithromycin) [25] have a higher risk of elevated blood levels and subsequent toxicity [9].
Methadone is a synthetic opioid with n-methyl-d-aspartate (NMDA) inhibitor, serotonin reuptake, and norepinephrine reuptake inhibitor properties [22]. It exists as R- and S-enantiomers, but most of its mu opioid activity is due to the R-enantiomer [22]. In the past, methadone was believed to be metabolized primarily by the CYP3A4 system [26], but more recent studies suggest that its major metabolism may instead be via CYP2B6 [27]. Interestingly, polymorphisms in the CYP 2B6 gene have been associated with differences in methadone treatment dose requirements in individuals managed for opioid addiction [28]. Polymorphisms at the CYP2B6 enzyme may also account for the variability in bupropion metabolism, [29, 30] and may be an important factor in the effectiveness of the reverse transcriptase inhibitor efavirenz [31], as well as ritonavir and nelfinavir [32].
CYP1A2
CYP1A2 partially biotransforms antipsychotic medications, such as clozapine and olanzapine [28], to their inactive form, so patients who are PM for the CYP1A2 appear to be at increased risk for toxic blood levels and increased incidence of tardive dyskinesia [33]. This is also the enzyme that metabolizes caffeine [34]. Both tobacco and marijuana smoking induce CYP1A2 activity, and their combined use is additive [35]. Therefore, when patients stop smoking, the increased metabolism of caffeine will decrease, leading to increased caffeine levels and therefore potentially increased agitation (which might be attributed to the smoking withdrawal) [36].
CYP2C9
CYP2C9 metabolism primarily involves NSAIDs and aspirin, though it is also the system that metabolizes phenytoin and warfarin. A recent study noted that the genetic screening of patients for defective variants of UGT1A6 (see below) and CYP2C9 helped identify those patients at risk for gastritis from aspirin use [37]. Up to 31 defective variants of the CYP2C9 have been found to cause reduced clearance of diclofenac [38], potentially increasing the risk of GI and renal adverse events. Poor metabolizers make up about 8–12% of white populations [39, 40], but it is rare in Ethiopian (4%) and extremely rare in African-American (1%) and Asian populations [40] (0% of Koreans in one study) [41].
CYP2C19
CYP2C19 primarily affects the metabolism of diazepam and carisoprodol, as well as clopidogrel, proton pump inhibitors, and several antidepressants. CYP219 metabolizes amitriptyline, clomipramine, doxepin, imipramine, and trimipramine, and PMs of CYP2C19 need about 60% of the standard dose of these medications, while UMs need about 110% of the standard dose [29]. Cannabinoids are probably significant CYP2C19 inhibitors [34] (which may raise diazepam blood levels). Proton pump inhibitors such as omeprazole and esomeprazole are also CYP2C19 inhibitors [42]. There are at least 27 variant alleles that have been identified [43]. Poor metabolizers of CYP2C19 are seen more commonly in Asian, Swedish, and Ethiopian populations (12–23%) compared to whites (2–5%), while 18% of Swedes and Ethiopians and 4% of Chinese are UMs of CYP2C19 [43].
UDP-Glucuronosyltransferase
One of the most common non-CYP enzymes associated with pain medications is UDP-glucuronosyltransferase (UGT) [44]. UGT is the main metabolizer of morphine, creating morphine-6-glucuronide (M3G), which contributes to pain relief, and morphine-3-glucuronide (M3G), which is hyperalgesic (causing increased pain). An increased concentration of M3G is believed to contribute to the phenomenon of opioid hyperalgesia.
Other Receptors and Enzymes Associated with Opioids and Analgesics
Polymorphisms in the mu opioid receptor itself may cause reduced potency of opioid medications. For example, the mu receptor subtype OPRM1 is the primary site of action of most opioid medications as well as endogenous endorphins. This receptor also controls the rewarding effects of nicotine and alcohol [45]. Whether the patient possesses the wild-type (two normal copies), heterozygous (one normal, one altered) or homozygous (two altered copies) alleles of this gene has been shown to influence postoperative opioid requirement after abdominal surgery [9]. One of the best-studied OPRM1 SNPs is 118A/G, with the G variant seen in 10–48% of tested patients, depending on the study [12]. Reynolds et al. found that patients carrying the GG genotype required much higher opioid doses to achieve pain relief [12].
Other receptors such as catechol-o-methyl transferase (COMT) have known variants (i.e. Val/Val, Met/Met) that are associated with increased opioid requirements, fibromyalgia, and a higher risk of addictive behaviors such as gambling and drinking [46]. In a study evaluating the role of genetics in predicting how well morphine would control cancer pain, Reyes-Gibby et al. found that the morphine dose needed by carriers of the OPRM1 GG genotype was 93% higher than that for carriers of the AA allele, and the lowest dose requirement was observed among carriers of the OPRM1 AA and COMT Met/Met genotype [13].
The P-glycoprotein 1 (permeability glycoprotein, abbreviated as P-gp or Pgp), also known as multidrug-resistant protein 1 (MDR1), is a glycoprotein that in humans is encoded by the ABCB1 gene. The ABCB1/MDR1 transporter gene is a major determinant of morphine bioavailability, and, as stated above, the OPRM1 gene encodes for the mu opioid receptor, the primary site of morphine activity. Mutations in either of these two genes can affect the efficacy of morphine [47]. Campa et al. genotyped 145 patients for the SNP C3435T of the ABCB1/MDR1 gene and the A80G SNP of the OPRM1 gene (a different SNP than the A118G discussed above) and observed statistically significant variability in pain relief (P < 0.00001), allowing for the detection of three groups of patients—strong responders, intermediate responders, and non-responders—with close to 100% sensitivity and 70% specificity [48].
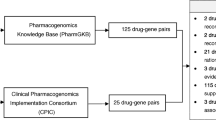
Drug–Gene Interactions
Many of the common medicines used in pain management are metabolized by the CYP450 system, i.e. they are substrates of this system (see Table 1). Some of the adjuvant medications used to treat pain, such as antidepressants, can significantly inhibit the activity of the CYP450 system, and therefore influence the effect of other medications such as opioids. For example, paroxetine [49] and duloxetine [50] are CYP2D6 inhibitors (but not citalopram or escitalopram), and would be expected to reduce the analgesia of opioids requiring CYP2D6 activity for activation (see Table 2). This can convert a genetically normal CYP2D6 metabolizer into a phenotypically poor CYP2D6 metabolizer.
Other medications can induce these CYP450 enzymes, increasing the effect of prodrug medications, causing patients to phenotypically become ultrametabolizers (see Table 3).
Thus there are several types of interactions between medications and genes: drug–drug interactions (DDIs), drug–gene interactions (DGIs), and drug–drug–gene interactions (DDGIs). Verbeurgt et al. looked at a sample of 1143 patients, genotyped them for CYP2C9, CYP2C19, and CYP2D6, and then looked at drug–gene and drug–drug–gene interactions [51]. The total number of medications that these patients were prescribed ranged from 1 to 44, with a mean of 8.4 and a median of 7 medications. The authors found that 31% of the patients had a DDI, 12% had a DGI, and 12% had a DDGI.
The Ins and Outs of Genetic Testing
Why Test Patients?
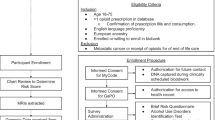
Effective pain management can be challenging, especially in settings where potent analgesics are used to treat patients with a high level of pain, and the patients do not respond to therapy or experience side effects. In addition, comorbidities requiring polypharmacy complicate decisions regarding which medications can be prescribed [51]. Genetic testing may be most useful in these types of settings and may provide data to determine the most efficacious drugs to prescribe at the safest dosing. Other scenarios in which genetic testing may be useful include patients who have shown a poor response to medications in the past, those with a family history of drug sensitivity, and selected pediatric patients [52] or breastfeeding mothers [53] prior to starting codeine.
Ethical Considerations of Testing
Even as genetic testing is becoming more widely accepted, many ethical questions have yet to be fully addressed. At the forefront is the concern that pharmacogenetics may exacerbate inequalities in the delivery of healthcare. Thus far, most debate surrounding genetic testing has been linked to genetic disorders and the potential impacts that knowledge of this information could have [54]. The use of pharmacogenetic tests to examine variation in treatment response raises a different set of ethical issues from other forms of genetic testing [54]. Expanding the use of genetic information could have consequences for both patients and their family members. Emerging research on genetic testing of opioid receptors may make it possible to identify those at high risk of opioid abuse and addiction [9]. Information obtained from pharmacogenetic testing could help to predict a patient’s susceptibility to certain diseases or the response of family members to particular drugs [55].
This leads to several ethical questions. Should health insurance companies or employers have access to this information? Will pharmacogenetic testing be mandatory in the future? With the availability of this information, would individuals be subject to higher health insurance premiums because they have the potential for a “poor response” to certain treatments? Moreover, where should the responsibility lie for obtaining pharmacogenetic testing? Should the tests be available for individuals to purchase online, over the counter? Or should they be available only through a PCP who is making a decision about prescribing a particular medication? If this information does guide a PCP’s decision, then what if that patient’s insurance disallows particular therapies?
Pharmacogenetic information can vary according to racial or ethnic origin. For instance, as described above, variations in the gene for the enzyme CYP2D6 are known to differ among racial groups [56]. What might be the implications of finding a genetic variant that influences a medicine’s response in a particular ethnic group? Among Ethiopian and Saudi Arabian populations, researchers found a high frequency of a genetic variant associated with increased CYP2D6 activity. In contrast, 7–10% of a white population possessed a genetic variant resulting in reduced activity of this enzyme [57].
Information like this has the potential to lead to the design of medications for a specific ethnic group or for an ethnic group most likely to be able to afford the medications [54]. As noted by Lipton [54], “There could be implications both for the conduct and design of research, and for the provision of tests and medicines. Will pharmacogenetics increase the likelihood of grouping of patients according to racial or ethnic groups for medical purposes? If so, what might be the ethical and social implications of such an outcome?”
These and other ethical questions will continue to arise as utilization of genetic testing becomes more sophisticated and thus more mainstream. Will the knowledge (or perceived knowledge) of genetic status change the way that patients are treated? A study of 134 chronic non-cancer pain patients found that physicians adjusted treatment plans for close to half of patients genotyped for pain perception-related COMT, and they perceived the genetic test results as consistent with patient pain levels in 85% of cases [58]. As such, these genetic tests carry significant weight. It is very concerning, therefore, to read case reports such as that by Zittel et al., who described a nurse who forged her genetic report to “confirm” her “dopa-responsive dystonia”, supporting her apparent Munchausen symptoms [59].
Many of these issues with regard to pharmacogenetics will have to be carefully addressed before the benefits and clinical applications of pharmacogenetics can be fully integrated into modern medicine. This will require healthcare professionals and policymakers to work together to continuously address issues regarding patient confidentiality, access to information, affordability, and research ethics in order to avoid such disparities.
Economic Considerations of Testing
Advances in pharmacogenetics have made the idea of “personalized medicine” more obtainable and provide a potential avenue for optimizing patient outcomes while reducing healthcare costs [60]. In cancer treatment, the use of genetic testing has become indispensable, improving outcomes, reducing side effects, and avoiding unnecessary testing [61]. In a review of the literature, 70% of 71 cardiac drugs studied had positive evidence of a varied response or adverse effect based on genetics. The authors stated that “considerable clinically actionable pharmacogenomic information for cardiovascular drugs exists, supporting the idea that consideration of such information when prescribing is warranted” [62]. However, the use of genetics in pain medicine has lagged these other fields.
While pharmacogenetic tests are becoming more affordable, access is still limited, and the costs that are related to obtaining samples, as well as interpreting and counseling patients on results, still need to be accounted for. In a broader sense, as our testing becomes more precise and our data accumulate, the promise that these results could reduce the trial-and-error approach to medication prescribing and reduce the likelihood of hospitalizations due to adverse drug reactions could significantly impact the economics of healthcare [63].
Researchers at Harding University recently conducted a randomized controlled trial in a high-risk population of chronically ill polypharmacy patients aged 50 years and older who were admitted to home health care after an inpatient hospitalization. The trial was designed to add pharmacogenetic data in an integrated clinical information system compared to a standard drug information system. The data showed that readmissions were reduced by 52% (P = 0.007), emergency department (ED) visits by 42% (P = 0.045), and mortality by 85% (P = 0.05). The authors estimated a potential cost savings per patient of $4382 in just 60 days, based on Medicare average all-cause readmission and ED visit costs [64].
Greater precision in prescribing drugs could potentially streamline the costs associated with polypharmacy. In addition, the costs of developing new agents could be dramatically reduced with the use of pharmacogenetics, to about 60% of the $880 million on average currently spent in developing a drug [65].
As clinical utility and cost-effectiveness are still being debated, economics continues to be an important rate-limiting step in considering treatments and therapies, and will no doubt be a major factor in how pharmacogenetic testing is integrated into our current medical practice [66]. Furthermore, knowledge of which pharmacogenetic testing applications are appropriate in pain management may be used to tailor treatments and limit unnecessary costs as opposed to recommending global testing approaches [62].
The Ins and Outs of Testing
In current practice, when laboratory monitoring of patients taking pain medications is performed, it is largely through urine drug measurements. Most urine drug screens (UDS), especially physician office “point-of-service” (POS) dipsticks, will provide a positive versus negative result, but are fraught with false-positive and false-negative errors [67]. Quantitative urine drug toxicology (UDT) reports provide information on opioid metabolites, which can offer clues as to the genetic make-up of the patient [9].
Oral (saliva) drug sampling is becoming more prevalent and economically feasible [68]. The advantages of oral sampling include a low risk of tampering (since samples are taken under direct observation), its non-invasive nature, and easy sample collection. Drawbacks to oral collection are the shorter time that metabolized drugs remain in oral fluids compared to urine, and the lower efficiency in detecting certain drug use (e.g. marijuana).
The ratio of metabolites to the parent compound seen in the UDT can provide clues as to the genetic makeup of the patient. For instance, a patient taking hydrocodone who has very little hydromorphone in the urine might be genetically deficient in CYP2D6. However, this result might also be seen with a patient with normal CYP2D6 function who is also taking a CYP2D6 inhibitor. The combination of UDT and genetic testing can provide important insight into the phenotypical response of the patient to a medication.
Available Genetic Testing
Genetic testing is commonly performed with blood and saliva; however, even small amounts of cheek tissue from a buccal swab can now be used for genetic testing [69], with results showing accuracy comparable to that with serum samples [70]. Genetic testing can confirm the findings of the urine toxicology (poor CYP2D6 function in the above example), or it may show normal function, implying drug–drug interactions.
There are a variety of genetic panels available. Some look at only a few enzymes, typically CYP2C9, CYP2C19, CYP2D6, and VKOR1 (which is associated with warfarin levels). Other panels may include OPRM1, COMT, and ABCB1, as well as dopamine receptors and transporters, serotonin receptors and transporters, and a growing list of other alleles.
You’ve Tested; Now What?
As the use of polypharmacy increases, it is important to be able to appropriately utilize genetic testing in clinical practice. The following case will help illustrate how to properly interpret results and avoid prescribing medications that may be harmful or ineffective.
A former police officer with multiple work-related neck and low back injuries and surgeries presented as a new patient from another pain clinic. He was taking oxycodone controlled-release 80 mg four times daily, with morphine immediate-release 15 mg every 8–12 h for breakthrough pain, but still complained of pain scores of 8–9/10 with no evidence of sedation. At this time, the differential diagnosis included opioid hyperalgesia (increased pain due to the opioids themselves), diversion or drug-seeking, poor absorption, or poor drug conversion. POS urine testing (qualitative) was positive for opioids and oxycodone. UDT (quantitative) showed the following: oxycodone >6400, noroxycodone >6400, oxymorphone 145, and hydromorphone 57.
The high levels of oxycodone and morphine should have first triggered concerns that the pills had been scraped into the collecting cup, but the noroxycodone proved that the drug had been absorbed and metabolized by the liver. It is not uncommon to find small amounts hydromorphone in the urine of patients on high doses of morphine, though it should be <1% of the morphine dose. Most striking is the extremely small amount of the active metabolite oxymorphone. Thus the problem was not poor absorption or drug-seeking; it still could have been opioid hyperalgesia, but the most likely diagnosis was low CYP2D6 activity. However, the patient was also on fluoxetine, a very potent CYP2D6 inhibitor, so the question remained: was he genetically a PM or a normal metabolizer taking a potent inhibitor? If the fluoxetine was the culprit, changing antidepressants might help, but if he was a PM, it would be necessary to change the opioid.
Genetic testing confirmed poor CYP2D6 status, and the patient was transitioned to an extended-release and immediate-release hydromorphone, with good relief, since hydromorphone does not require CYP2D6 metabolism.
In this case, urine toxicology coupled with genetic testing provided both the diagnosis and appropriate treatment options.
Conclusion
Chronic pain is one of the most prevalent medical conditions, and pain medications are some of the most commonly prescribed drugs in the United States today. Unfortunately, there is wide variability in patient response to pain and to pain medications, which may be related to pain origin, pain sensitivity, cultural differences, weight, age, and prior use of opiates, as well as genetic polymorphisms. The risks of long-term opioid use include death from overdose and drug interactions; the use of more objective measures (e.g. urine levels, genetic testing) rather than subjective measures (pain scores) should aid in determining efficacy, identifying diversion, ensuring patient compliance with therapy, and guiding the management of complex patients.
Over time, genetic testing has become more accessible and less expensive. However, there are very serious and complex ethical and financial concerns regarding its use that must be addressed prior to widespread implementation of this tool. And, while the current data are intriguing, there is still no clear evidence that genetic testing—at least for the general population—is effective. It may be appropriate for certain patient populations (such as those with significant family history of adverse drug reactions, pediatric patients, and chronic opioid users) and for specific clinical situations (such as a family history of genetic polymorphisms, inadequate analgesia on a significant amount of pain medications, or aberrant UDS results). These tests may therefore offer unique information in the primary care setting that could aid in medical decision-making for the complex patient.
As noted by Reynolds et al. [12], with the knowledge of a patient’s potential for positive response to a given pain medicine, a physician is armed with critical information that can guide therapeutic decisions in real time. The incorporation of pharmacogenetic biomarkers holds promise as a means of assessing a patient’s risk of adverse events or likelihood of drug efficacy. Incorporation of such biomarkers is emerging at the forefront of personalized medicine, and has the potential to improve the utility and efficacy of current strategies and to guide the development of new approaches to pain management.
References
Hardt J, Jacobsen C, Goldberg J, Nickel R, Buchwald D. Prevalence of chronic pain in a representative sample in the United States. Pain Med. 2008;9:803–12.
Furlan AD, Reardon R, Weppler C. Opioids for chronic noncancer pain: a new Canadian practice guideline. Can Med Assoc J. 2010;182:923–30.
Kapur BM, Lala PK, Shaw JL. Pharmacogenetics of chronic pain management. Clin Biochem. 2014;47(13–14):1169–87.
Steimer W, Müller B, Leucht S, Kissling W. Pharmacogenetics: a new diagnostic tool in the management of antidepressive drug therapy. Clin Chim Acta. 2001;308(1–2):33–41.
Stamer UM, Stuber F. Genetic factors in pain and its treatment. Curr Opin Anaesthesiol. 2007;20:478–84.
CDC/NCHS National Ambulatory Medical Care Survey: 2010 Summary Tables Atlanta, GA: Centers for Disease Control and Prevention https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed 12/15/16.
Mills R, Voora D, Peyser B, Haga S. Delivering pharmacogenetic testing in a primary care setting. Pharmgenom Pers Med. 2013;6:105–12.
Trescot AM, Faynboym S. A review of the role of genetic testing in pain medicine. Pain Physician. 2014;17:425–45.
Trescot AM. Genetics and implications in perioperative analgesia. Best Pract Res Clin Anaesthesiol. 2014;28(2):1153–66.
Yang Z, Arheart KL, Morris R, et al. CYP2D6 poor metabolizer genotype and smoking predict severe postoperative pain in female patients on arrival to the recovery room. Pain Med. 2012;13:604–9.
Kadiev E, Patel V, Rad P, et al. Role of pharmacogenetics in variable response to drugs: focus on opioids. Expert Opin Drug Metab Toxicol. 2008;41(1):77–91.
Reynolds KK, Ramey-Hartung B, Jortani SA. The value of CYP2D6 and OPRM1 pharmacogenetic testing for opioid therapy. Clin Lab Med. 2008;28(4):581–98.
Reyes-Gibby CC, Shete S, Rakvag T, et al. Exploring joint effects of genes and the clinical efficacy of morphine for cancer pain: OPRM1 and COMT gene. Pain. 2007;130:25–30.
Klepstad P. Genetic variability and opioid efficacy. Curr Anaesth Crit Care. 2007;18:149–56.
Samer CF, Daali Y, Wagner M, et al. Genetic polymorphisms and drug interactions modulating CYP2D6 and CYP3A activities have a major effect on oxycodone analgesic efficacy and safety. Br J Pharmacol. 2010;160:919–30.
Crist RC, Berrettini WH. Pharmacogenetics of OPRM1. Pharmacol Biochem Behav. 2014;123:25–33.
Trescot AM. Genetic testing in pain medicine. Pain Med News. 2013:1–8.
Kirchcheiner J, Schmidt H, Tzvetkov M, Keulen JT, Lotsch J, Roots I, Brockmoller J. Pharmacokinetics of codeine and its metabolite morphine in ultra rapid metabolizers due to CYP2D6 duplication. Pharmacogenom J. 2007;7:257–65.
Kaplan HL, Busto UE, Baylon GJ, Cheung SW, Otton SV, Somer G, Sellers EM. Inhibition of cytochrome P450 2D6 metabolism of hydrocodone to hydromorphone does not importantly affect abuse liability. J Pharm Exp Ther. 1997;281(1):103–8
Grond S, Sablotzki A. Clinical pharmacology of tramadol. Clin Pharmacokinet. 2004;43(13):879–923.
Paar WD, Poche S, Gerloff J, Dengler HJ. Polymorphic CYP2D6 mediates O-demethylation of the opioid analgesic tramadol. Eur J Clin Pharmacol. 1997;53:235–9.
Trescot AM, Datta S, Lee M, Hansen H. Opioid pharmacology. Pain Physician. 2008;11(Opioid Special Issue):S133–53.
Barakat NH, Atayee RS, Best BM, Pesce AJ. Relationship between the concentration of hydrocodone and its conversion to hydromorphone in chronic pain patients using urinary excretion data. J Anal Toxicol. 2012;36(4):257–64.
VanderVaart S, Berger H, Sistonen J, Madadi P, Matok I, Gijsen VM, et al. CYP2D6 polymorphisms and codeine analgesia in postpartum pain management: a pilot study. Ther Drug Monit. 2011;33(4):425–32.
Liukas A, Hagelberg NM, Kuusniemi K, Neuvonen PJ, Olkkola KT. Inhibition of cytochrome P450 3A by clarithromycin uniformly affects the pharmacokinetics and pharmacodynamics of oxycodone in young and elderly volunteers. J Clin Psychopharmacol. 2011;31(3):302–8.
Iribarne C, Berthou F, Baird S, Dreano Y, Picart D, Bail JP, et al. Involvement of cytochrome P450 3A4 enzyme in the N-demethylation of methadone in human liver microsomes. Chem Res Toxicol. 1996;9(2):365–73.
Totah RA, Sheffels P, Roberts T, Whittington D, Thummel K, Kharasch ED. Role of CYP2B6 in stereoselective human methadone metabolism. Anesthesiology. 2008;108(3):363–74.
Levran O, Peles E, Hamon S, Randesi M, Adelson M, Kreek MJ. CYP2B6 SNPs are associated with methadone dose required for effective treatment of opioid addiction. Addict Biol. 2011;18(4):709–16.
Kirchheiner J, Nickchen K, Bauer M, Wong ML, Licinio J, Roots I, et al. Pharmacogenetics of antidepressants and antipsychotics: the contribution of allelic variations to the phenotype of drug response. Mol Psychiatry. 2004;9(5):442–73.
Hesse LM, Venkatakrishnan K, Court MH, von Moltke LL, Duan SX, Shader RI, et al. CYP2B6 mediates the in vitro hydroxylation of bupropion: potential drug interactions with other antidepressants. Drug Metab Dispos. 2000;28(10):1176–83.
Zanger UM, Klein K. Pharmacogenetics of cytochrome P450 2B6 (CYP2B6): advances on polymorphisms, mechanisms, and clinical relevance. Front Genet. 2013;4:24.
Hesse LM, von Moltke LL, Shader RI, Greenblatt DJ. Ritonavir, efavirenz, and nelfinavir inhibit CYP2B6 activity in vitro: potential drug interactions with bupropion. Drug Metab Dispos. 2001;29(2):100–2.
Basile VS, Ozdemir V, Masellis M, Walker ML, Meltzer HY, Lieberman JA, et al. A functional polymorphism of the cytochrome P450 1A2 (CYP1A2) gene: association with tardive dyskinesia in schizophrenia. Mol Psychiatry. 2000;5(4):410–7.
Kalow W, Tang BK. Use of caffeine metabolite ratios to explore CYP1A2 and xanthine oxidase activities. Clin Pharmacol Ther. 1991;50(5 Pt 1):508–19.
Anderson GD, Chan LN. Pharmacokinetic drug interactions with tobacco, cannabinoids and smoking cessation products. Clin Pharmacokinet. 2016;55(11):1353–68.
Rodenburg EM, Eijgelsheim M, Geleijnse JM, Amin N, van Duijn CM, Hofman A, et al. CYP1A2 and coffee intake and the modifying effect of sex, age, and smoking. Am J Clin Nutr. 2012;96(1):182–7.
Jalil NJ, Bannur Z, Derahman A, Maskon O, Darinah N, Hamidi H, et al. The Implication of the Polymorphisms of COX-1, UGT1A6, and CYP2C9 among Cardiovascular Disease (CVD) Patients Treated with Aspirin. J Pharm Pharm Sci Publ Can Soc Pharm Sci (Société canadienne des sciences pharmaceutiques). 2015;18(3):474–83.
Xia MM, Wang L, Pan PP, Wang HY, Chen MC, Chen Y, et al. The role of CYP2C9 genetic polymorphisms in the oxidative metabolism of diclofenac in vitro. Pharmazie. 2014;69(12):898–903.
Garcia-Martin E, Martinez C, Ladero JM, Gamito FJ, Agundez JA. High frequency of mutations related to impaired CYP2C9 metabolism in a Caucasian population. Eur J Clin Pharmacol. 2001;57(1):47–9.
Scordo MG, Aklillu E, Yasar U, Dahl ML, Spina E, Ingelman-Sundberg M. Genetic polymorphism of cytochrome P450 2C9 in a Caucasian and a black African population. Br J Clin Pharmacol. 2001;52(4):447–50.
Kim YM, Yoo SH, Kang RY, Kim MJ, Bae YY, Lee YK, et al. Identifying drugs needing pharmacogenetic monitoring in a Korean hospital. Am J Health Syst Pharm AJHP. 2007;64(2):166–75.
Klieber M, Oberacher H, Hofstaetter S, Beer B, Neururer M, Amann A, et al. CYP2C19 phenoconversion by routinely prescribed proton pump inhibitors omeprazole and esomeprazole: clinical implications for personalized medicine. J Pharmacol Exp Ther. 2015;354(3):426–30.
Sim SC, Risinger C, Dahl ML, Aklillu E, Christensen M, Bertilsson L, et al. A common novel CYP2C19 gene variant causes ultrarapid drug metabolism relevant for the drug response to proton pump inhibitors and antidepressants. Clin Pharmacol Ther. 2006;79(1):103–13.
Smith HS. The metabolism of opioid agents and the clinical impact of their active metabolites. Clin J Pain. 2011;27(9):824–38.
Crist RC, Berrettini WH. Pharmacogenetics of OPRM1. Pharmacol Biochem Behav. 2014;123:25–33.
Guillot CR, Fanning JR, Liang T, Berman ME. COMT associations with disordered gambling and drinking measures. Journal of gambling studies/co-sponsored by the National Council on Problem Gambling and Institute for the Study of Gambling and Commercial Gaming. 2014.
Agarin T, Trescot AM, Agarin A, Lesanics D, Decastro C. Reducing opioid analgesic deaths in America: what health providers can do. Pain Physician. 2015;18(3):E307–22.
Campa D, Gioia A, Tomei A, Poli P, Barale R. Association of ABCB1/MDR1 and OPRM1 gene polymorphisms with morphine pain relief. Clin Pharmacol Ther. 2008;83(4):559–66.
Laugesen S, Enggaard TP, Pedersen RS, Sindrup SH, Brosen K. Paroxetine, a cytochrome P450 2D6 inhibitor, diminishes the stereoselective O-demethylation and reduces the hypoalgesic effect of tramadol. Clin Pharmacol Ther. 2005;77(4):312–23.
Skinner MH, Kuan HY, Pan A, et al. Duloxetine is both an inhibitor and a substrate of cytochrome P450 2D6 in healthy volunteers. Clin Pharmacol Ther. 2003;73(3):170–7.
Verbeurgt P, Mamiya T, Oesterheld J. How common are drug and gene interactions? Prevalence in a sample of 1143 patients with CYP2C9, CYP2C19 and CYP2D6 genotyping. Pharmacogenomics. 2014;15(5):655–65.
Madadi P, Amstutz U, Rieder M, et al. Clinical practice guideline: CYP2D6 genotyping for safe and efficacious codeine therapy. J Popul Therap Clin Pharm (Journal de la therapeutique des populations et de la pharamcologie clinique). 2013;20(3):e369–96.
Madadi P, Ciszkowski C, Gaedigk A, et al. Genetic transmission of cytochrome P450 2D6 (CYP2D6) ultrarapid metabolism: implications for breastfeeding women taking codeine. Curr Drug Saf. 2011;6(1):36–9.
Lipton P. Pharmacogenetics: the ethical issues. Pharmacogenom J. 2003;3:14–6.
Barash, CI. Ethical Issues in Pharmacogenetics. Action Bioscience. April 2013. http://www.actionbioscience.org/biotechnology/ethical_issues_in_pharmacogenetics.html. Accessed 12/15/16.
Genetic Alliance; The New York-Mid-Atlantic Consortium for Genetic and Newborn Screening Services. Understanding Genetics: a New York, Mid-Atlantic Guide for Patients and Health Professionals. Washington (DC): Genetic Alliance; 2009 Jul 8. APPENDIX Q, National Coalition for Health Professional Education in Genetics (NCHPEG): Principles of Genetics for Health Professionals. Available from: https://www.ncbi.nlm.nih.gov/books/NBK115543/. Accessed 12/15/16.
Weber W. Pharmacogenetics. Oxford: Oxford Press; 1997.
Sharma M, Kantorovich S, Lee C, Anand N, Blanchard J, Fung ET, et al. An observational study of the impact of genetic testing for pain perception in the clinical management of chronic non-cancer pain. J Psychiatr Res. 2017;89:65–72.
Zittel S, Lohmann K, Bauer P, Klein C, Munchau A. Munchausen syndrome by genetics: next-generation challenges for clinicians. Neurology. 2017;88(10):1000–1.
Vogenberg FR, Barash CI, Pursel M. Personalized medicine Part 3: Challenges facing health care plans in implementing coverage for policies for pharmacogenomic and genetic testing. 2010; 35(12):670–75.
Lehmann-Che J, Poirot B, Boyer JC, Evrard A. Cancer genomics guide clinical practice in personalized medicine. Therapie. 2017. doi:10.1016/j.therap.2016.09.015.
Kaufman AL, Spitz J, Jacobs M, Sorrentino M, Yuen S, Danahey K, Saner D, Klein TE, Altman RB, Ratain MJ, O'Donnell PH. Evidence for clinical implementation of pharmacogenomics in cardiac drugs. Mayo Clin Proc. 2015;90(6):716–29.
Wu AC, Fuhlbrigge AL. Economic evaluation of pharmacogenetic tests. Clin Pharmacol Ther. 2008;84(2):272–4.
Elliott LS, Henderson JC, Neradilek MB, Moyer NA, Ashcraft KC, Thirumaran RK. Clinical impact of pharmacogenic profiling with a clinical decision support tool in polypharmacy home health patients: A prospective pilot randomized controlled trial. PLoS One. 2017;12(2):a0170905.
Tollman P, Guy P, Altshuler J, et al. A Revolution in R&D. How genomics and genetics are transforming the biopharmaceutical industry. Boston: Boston Consulting Group; 2001.
Lesko LJ, Zineh I, Huang SM. What is clinical utility and why should we care? Clin Pharmacol Ther. 2010;88(6):729–33.
Moeller KE, Lee KC, Kissak JC. Urine drug screening: practical guide for clinicians. Mayo Clin Proc. 2008;83:66–76.
Drummer OH. Drug testing in oral fluid. Clin Biochem Rev. 2006;27(3):147–59.
McMichael GL, Gibson CS, O’Callaghan ME, et al. DNA from buccal swabs suitable for high-throughput SNP multiplex analysis. J Biomol Tech. 2009;20(5):232–5.
Belmonte I, Barrecheguren M, Esquinas C, Rodriguez E, Miravitlles M, Rodriguez-Frias F. Genetic diagnosis of alpha1-antitrypsin deficiency using DNA from buccal swab and serum samples. Clin Chem Lab Med. 2017.
Acknowledgements
No funding or sponsorship was received for the publication of this article.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as whole, and have given final approval for the version to be published.
Disclosures
Dr. Deepti Agarwal and Dr. Mercy Udoji declare that they have no conflict of interest to disclose. Dr. Andrea Trescot is the medical director of Pinnacle Lab Services.
Compliance with Ethics Guidelines
This article is based on previously conducted studies, and does not involve any studies of human or animal subjects performed by any of the authors.
Data Availability
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/5708F0606FE96946.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Agarwal, D., Udoji, M.A. & Trescot, A. Genetic Testing for Opioid Pain Management: A Primer. Pain Ther 6, 93–105 (2017). https://doi.org/10.1007/s40122-017-0069-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-017-0069-2