Abstract
Breakthrough pain is a transient exacerbation of pain that occurs either spontaneously, or in relation to a specific predictable or unpredictable trigger, despite relatively stable and adequately controlled background pain. Typically, breakthrough pain has a fast onset and short duration, and a significant impact on patients’ quality of life. Normal-release oral opioids are the traditional pharmacological approach for patients who are receiving an around the clock opioid regimen; however, their onset and duration of action may not be suitable for treating many breakthrough pains. Efforts to provide nonparenteral opioid formulations that could provide more rapid, and more effective, relief of breakthrough pain have led to the development of transmucosal opioid formulations including fentanyl sublingual spray (FSLS). This is a formulation of fentanyl available in doses of 100, 200, 400, 600, and 800 μg strengths approved for the management of breakthrough pain in adult cancer patients already receiving and who are tolerant to opioid therapy for their underlying persistent cancer pain. Published pharmacokinetic, efficacy, tolerability, and safety data suggest that FSLS has a valuable role to play in the symptomatic pharmacological management of breakthrough pain. The effective dose of FSLS is determined by titration according to the needs of the individual patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most patients with advanced cancer experience some degree of persistent background pain, the prevalence of which increases with disease progression, with rates of 30–40% during early disease, rising to 70–90% in advanced disease [1]. As pain assessment methods have evolved it has become increasingly clear that patients with cancer often report variations in their pain during the course of the day. Moreover, between 20% and 95% of patients also experience transitory exacerbation of pain, known as breakthrough pain [2]; the incidence varying according to the population surveyed and the definition of breakthrough pain used [2]. Breakthrough pain is associated with a significant negative impact on quality of life, yet surveys suggest that patients are not being treated optimally [3, 4]. In recent years a number of products specifically developed for the management of breakthrough pain have become available, most of which deliver fentanyl transmucosally. The aim of this paper is to review sublingual fentanyl spray, which is one of the most recent additions; other products have already been reviewed elsewhere [5, 6].
Definitions
Breakthrough pain is a transient exacerbation of pain that occurs either spontaneously, or in relation to a specific predictable or unpredictable trigger, despite relatively stable and adequately controlled background pain [7]. First described by Portenoy and Hagen in 1990 [8], the term has been used to describe a phenomenon whereby pain intensity suddenly increases to “break through” the background pain that is otherwise controlled by around the clock (ATC) medication.
Breakthrough pain has been variably defined in the literature. Some authors have proposed that breakthrough pain exists only when background pain is controlled [8]; others have suggested breakthrough pain may exist in patients with uncontrolled background pain and irrespective of analgesic regimen [4, 9]. These differences have led to difficulties comparing studies.
Given the importance of distinguishing breakthrough pain from uncontrolled background pain, it has been suggested that three questions would be helpful to distinguish between the two [7]:
-
Does the patient have background pain?
-
Is the background pain adequately controlled?
-
Does the patient have transient exacerbations of pain?
Characteristics
Breakthrough pain is heterogeneous and prevalent at all stages of disease, but appears most common in patients with advanced disease and poor performance status [4]. The characteristics of breakthrough pain vary from individual to individual, and may vary within an individual over time. Typically, the etiology and pathophysiology of the breakthrough pain are related to the background pain and the episodes are severe or excruciating in intensity, have a rapid onset (3–5 min to peak intensity), last for 15–30 min, and occur, on average, four times a day [8, 10–12].
Two subtypes of breakthrough pain have been described. First, incident pain, reported in 32–94% of patients [13, 14], may be predictable when precipitated by volitional factors (e.g., movement) or unpredictable when precipitated by non-volitional factors (e.g., bladder spasm). Incident pain has been shown to be a poor predictor of successful pharmacological therapy [14, 15]. Second, spontaneous pain, which has been reported in 28–45% of patients [8, 13], and occurs in the absence of a specific trigger. Spontaneous pain can occur randomly and unpredictably with little or no warning, making management difficult.
Some patients report pain that consistently occurs just before the next scheduled dose of ATC analgesia, so-called “end-of-dose” pain. This occurs either because the ATC analgesic dose is inadequate, or because the interval between administrations is too long. Although “end-of-dose” pain is sometimes included in the classification of breakthrough pain, it does not fit the definition given above, as background pain is not controlled.
Impact
Breakthrough pain has been shown to have significant physical, psychological, and economic burdens on both patients and their carers. Breakthrough pain is associated with decreased patient satisfaction [10, 12], decreased functioning, anxiety, and depression [10]. Furthermore, breakthrough pain can be a poor prognostic indicator [14, 16, 17], and can place additional burdens on the healthcare system (e.g., increases in emergency and medical visits, more hospital admissions, and longer stays) [18], and on patients with increased direct costs (e.g., prescriptions) and indirect costs (e.g., child care) [19].
Breakthrough pain is therefore a significant clinical challenge, and patients require fast and effective treatment to control the pain, improve quality of life, and increase their independence. The most common pharmacological management is with supplemental doses of oral opioids also known as “rescue medication.” A rapid onset of action and short duration of effect are among the key characteristics of an ideal rescue medication. The most appropriate route of administration for a rescue medication is dependent on the nature of the pain and the clinical profile of the patient and, at any given time, a patient with cancer may receive several pain medications using different administration routes to provide optimal analgesia. Although oral drug administration is usually preferred because it is convenient and usually inexpensive, the pharmacokinetic and pharmacodynamic profiles of many drugs delivered orally do not mirror closely the characteristics of breakthrough pain, resulting in only partially effective treatment and/or troublesome adverse effects [11]. In an effort to deliver more effective treatment of breakthrough pain ways of improving drug absorption have been explored.
Transmucosal Opioids
The recognized mismatch between the pharmacodynamics of oral and parenteral opioids and the typical time course of an episode of breakthrough pain, together with the inconvenience of parenteral administration, has led to a search for alternative drugs and drug delivery systems to improve the management of breakthrough pain. In this respect, opioid formulations that utilize the oral transmucosal (buccal and sublingual) and intranasal routes have emerged as effective options for the management of breakthrough pain [20].
These routes of administration also have the advantage that they utilize a highly vascular area, allowing rapid drug absorption, and circumvent or reduce absorption from the gastrointestinal tract, a particular advantage for patients who have difficulty swallowing or have a damaged or impaired gastrointestinal tract [21]. In addition, first-pass metabolism by the liver is avoided or reduced, which increases the proportion of the dose entering the systemic circulation, thereby allowing the amount of drug ingested to be minimized.
Sublingual Transmucosal Delivery
The oral mucosa is an attractive route for drug delivery as it is generally associated with more rapid absorption compared with the oral route. Fentanyl is a highly lipophilic opioid and, when placed in saliva under normal oral conditions, 80% of the administered dose remains nonionised allowing the drug to pass readily through the buccal mucosa, quickly cross the blood–brain barrier and enter the central nervous system [22].
The buccal and sublingual tissues are the primary focus for drug delivery via the oral mucosa because they are more permeable than the tissues in the other area of the mouth. The mucosa is easily accessible, convenient, noninvasive, and less threatening to patients compared to other routes of administration such as intravenous or intramuscular. Furthermore, it does not require technical equipment, expertise, preparation and supervision. The buccal mucosa is highly vascularized and therefore any drugs diffusing into the oral mucosa membranes have direct access to the systemic circulation via capillaries and venous drainage. Drugs are absorbed through the oral mucosa directly into the systemic circulation [21].
Methods
A Medline search was performed to identify the relevant literature. The search terms used included “breakthrough pain,” “incident pain,” and “episodic pain,” “sublingual,” and “fentanyl,” the database was searched up until November 2012, and limits used were human and English language. Additional papers were sought from the reference lists of the retrieved papers. The search identified one pivotal study. Further information was obtained from the US Food and Drug Administration website. Insys Pharmaceutical Inc. was contacted for additional information but none was received.
Fentanyl Sublingual Spray
Fentanyl sublingual spray (FSLS) is a sublingually administered formulation of fentanyl available in doses of 100, 200, 400, 600, and 800 μg strengths approved in the USA for the management of breakthrough pain in adult cancer patients already receiving and who are tolerant to opioid therapy for their underlying persistent cancer pain. Patients considered opioid tolerant are those who are taking ATC medicine consisting of at least 60 mg of oral morphine daily, at least 25 μg/h of transdermal fentanyl, at least 30 mg of oral oxycodone daily, at least 8 mg of oral hydromorphone daily, or an equianalgesic dose of another opioid daily for a week or longer.
Pharmacokinetics
Following the single dose administration of FSLS 400 μg, the mean absolute bioavailability of fentanyl compared to fentanyl citrate 100 μg intravenous injection was 76% as measured by AUC0–∞ and normalized for dose [23]. In an open-label study that compared the relative bioavailability of FSLS and oral transmucosal fentanyl citrate (OTFC) in 21 healthy adult subjects, the rate and extent of fentanyl absorption were considerably greater with FSLS (34% greater maximum plasma concentration [Cmax = 0.81 ng/mL for FSLS vs. 0.61 ng/mL for OTFC] and 36% greater systemic exposure [AUC0-∞ = 5.76 ng/mL/h for FSLS vs. 4.18 ng/mL/h for OTFC]) [22].
Dose proportionality of 100, 200, 400, 600, and 800 μg strengths of FSLS has been evaluated in a crossover study in healthy subjects [23]. Both the Cmax (0.20, 0.38, 0.80, 1.17, and 1.61 ng/mL, respectively) and AUC0-∞ (1.25, 2.48, 5.34, 7.45, and 10.38 ng/mL/h, respectively) values increased in a dose-dependent manner that was approximately proportional to the FSLS doses administered [23].
The effect of Grades 1 and 2 mucositis on the pharmacokinetics of FSLS was studied in a group of cancer patients with mucositis (n = 7 for Grade 1 and n = 2 for Grade 2) and without mucositis (n = 8). A single 100 μg dose was administered. Cancer patients with Grade 1 mucositis compared to patients without mucositis exhibited 73% greater Cmax (0.45 vs. 0.26 ng/mL) and 52% greater AUClast (1.38 vs. 0.91 ng/mL/h) values. The two cancer patients with Grade 2 mucositis had four and sevenfold higher Cmax and more than threefold higher AUClast values compared to patients without mucositis [23].
Efficacy
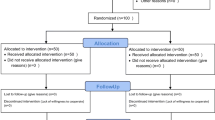
The efficacy of FSLS was investigated in a double-blind, placebo-controlled, crossover study in opioid-tolerant adults with cancer and breakthrough pain [24]. Patients received FSLS from 100 μg per dose to 1,600 μg per dose. The study began with an open-label dose titration period followed by a double-blind treatment period. The goal of titration was to find the dose of FSLS that provided adequate analgesia with acceptable side effects. Once a successful dose was established, patients were enrolled into the double-blind period and randomly assigned to a sequence of 10 treatments; seven with FSLS and three with placebo. The subjects assessed pain intensity on a 100 mm visual analog scale that rated the pain as 0 = none to 100 = worst possible pain. With each episode of breakthrough pain, pain intensity was assessed first and then treatment was administered. Pain intensity (0–100) was then measured at 5, 10, 15, 30, 45, and 60 min after the start of administration. The primary endpoint was the summed pain intensity difference from baseline to 30 min after dosing (SPID30).
Out of 130 patients who entered the titration phase, 98 (75%) were able to titrate to a dose of FSLS that adequately reduced pain with tolerable side effects and entered into the double-blind period; 79 patients completed all 10 doses of blinded study drug [24]. The median effective dose was 800 μg, and 58.2% of patients attained an effective dose between 800 and 1,600 μg. Comparison of FSLS and placebo showed that FSLS was statistically superior in reducing pain intensity using the primary outcome SPID30 (Fig. 1). Furthermore, secondary efficacy analyses including total pain relief and patient global evaluation of study medication at 30 min also favored FSLS. Moreover, rescue medication was used by patients during 28% of episodes treated by placebo compared to 10% of episodes treated with FSLS.
Mean summed pain intensity difference ± SE for fentanyl sublingual spray (FSLS) and placebo at each time point [23]
Safety and Tolerability
The safety of FSLS has been evaluated in a total of 359 patients including patients from the efficacy study and patients from an open-label safety study lasting up to 90 days that rolled patients over from the efficacy study and enrolled new patients [23]. During the efficacy study the most commonly reported adverse effects during titration were nausea (13%), somnolence (8.5%), dizziness (7.7%), and vomiting (7.7%), and during the efficacy phase nausea (7.1%), hyperhidrosis (5.1%), and peripheral edema (5.1%); the majority mild or moderate in intensity. Application site irritation occurred in three patients (2.3%) during the titration period; this adverse event led to study discontinuation in one patient.
Safety data from a long-term extension study showed that the average duration of therapy in the open-label study was 66 days [23]. The maximum duration of therapy was 149 days. The dose range studied in these trials ranged from 100 μg per dose to 1,600 μg per dose. The most commonly observed adverse reactions seen with FSLS are typical opioid side effects such as nausea, vomiting, somnolence, and constipation. The most common adverse reaction leading to discontinuation of FSLS was nausea.
The risk of respiratory depression is often associated with opioids and usually considered more likely with the short-acting formulations, although in clinical practice provided the drug is used in accordance with the label, respiratory depression is seldom a problem. Moreover, in the safety and tolerability data there were no cases of respiratory depression associated with the use of FSLS.
The clinical trials of FSLS were designed to evaluate safety and efficacy in treating breakthrough cancer pain; all patients were also taking concomitant opioids, such as sustained-release morphine or transdermal fentanyl, for their persistent cancer pain. Therefore, the adverse events data reflect the effects of study drug, but also reflect that this was a population with active cancer causing pain, taking ATC opioids and many other medications.
Clinical Application of Sublingual Fentanyl
Fentanyl sublingual spray should only be administered to adult patients already taking at least 60 mg oral morphine per day or equivalent alternative ATC opioid for a week or longer [25]. Each FSLS carton contains individual blister packages containing single spray units of FSLS, a supply of small white disposal bags for disposing of used FSLS units, a medication guide, and a package insert. FSLS is supplied in individually sealed blister packages that should be opened with scissors immediately before product use. The patient should carefully spray the contents of the unit into his or her mouth underneath the tongue.
The spray unit must be disposed of in used unit dose systems immediately after use, and any unneeded unit dose systems remaining from a prescription as soon as they are no longer needed. Consumed units represent a special risk because they are no longer protected by the child-resistant blister package, yet may contain enough medicine to be fatal to a child. A disposal bottle is provided with every carton dispensed. This container is to be used by patients or their caregivers to dispose of the contents of any unneeded unit dose systems when they are no longer needed.
Titration
Fentanyl sublingual spray should be individually titrated to a dose that provides adequate analgesia and minimizes side effects (Fig. 2; Table 1). The initial dose of FSLS to treat episodes of breakthrough cancer pain is always 100 μg [25]. From this initial dose, the dose should be titrated through steps of 200, 400, 600, 800, 1,200, and 1,600 μg to provide adequate analgesia using a single FSLS dose per breakthrough cancer pain episode with tolerable side effects. For each breakthrough pain episode treated, if pain is not relieved after 30 min, patients may take one additional dose of the same strength for that episode. Therefore, the maximum of two doses of FSLS is recommended for any breakthrough pain episode. Patients should wait at least 4 h before treating another episode of breakthrough pain with FSLS. FSLS is not bioequivalent with other fentanyl products and therefore patients should not be converted on a microgram per microgram basis from other fentanyl products.
Fentanyl sublingual spray titration process [23]
Maintenance
Once titrated to a dose that provides adequate pain relief and tolerable side effects, patients should generally use one FSLS dose of the appropriate strength per breakthrough pain episode.
On those occasions when the breakthrough pain episode is not relieved within 30 min after administration of the FSLS dose, the patient may take one additional dose using the same strength for that episode. Patients should wait at least 4 h before treating another episode of breakthrough pain with FSLS. Once a successful dose has been found, patients should limit consumption to four or fewer doses per day. Dosage adjustment of FSLS may be required in some patients in order to continue to provide adequate relief of breakthrough pain. If signs of excessive opioid effects appear following administration of a single FSLS dose, subsequent doses should be decreased.
Generally, only increase the FSLS dose when a single administration of the current dose fails to treat the breakthrough pain episode adequately for several consecutive episodes. If the patient experiences greater than four breakthrough pain episodes per day, the dose of the maintenance (ATC) opioid used for persistent pain should be re-evaluated. In addition, if pain worsens, re-evaluate the patient for changes in the underlying pain condition.
Contraindications
Fentanyl sublingual spray is contraindicated in opioid-naive patients, in the management of acute or postoperative pain including headache/migraine, and in patients with known intolerance or hypersensitivity to any of its components or the drug fentanyl.
Cost
When considering costs, the transmucosal fentanyl preparations are usually compared to oral opioids, the latter being considerably cheaper. Although oral opioids may be helpful for some breakthrough pains, particularly those with a slow onset and long duration, they are not suited to most of them [2]. The use of transmucosal opioids is therefore based on an assessment of the presenting breakthrough pain and used when oral opioids are, or are likely to be, ineffective. If there is any doubt, a therapeutic trial of an oral opioid may help before switching to the transmucosal route.
Conclusions
Breakthrough pain has been shown to occur commonly in patients with cancer, and is often of sudden onset, short duration, and is severe or excruciating and short lasting, making management difficult. The ideal treatment for breakthrough pain should match the clinical and dynamic profile of breakthrough pain. FSLS is indicated for the management of breakthrough pain in patients with cancer who are already receiving opioid therapy for their background cancer pain. The pharmacokinetic, efficacy, tolerability and safety profile of FSLS suggest that it has a valuable role to play in the symptomatic pharmacological management of breakthrough pain. The effective dose of FSLS is determined by titration according to the needs of the individual patient.
References
Schrijvers D. Pain control in cancer: recent findings and trends. Ann Oncol. 2007;18(Suppl. 9):ix37–42.
Zeppetella G. Breakthrough pain in cancer patients. Clin Oncol. 2011;23:393–8.
Breivik H, Cherny N, Collett B, et al. Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol. 2009;20:1420–33.
Caraceni A, Martini C, Zecca E, et al. Breakthrough pain characteristics and syndromes in patients with cancer pain. An international survey. Palliat Med. 2004;18:177–83.
Mercadante S. Pharmacotherapy for breakthrough cancer pain. Drugs. 2012;72:181–90.
Smith H. A comprehensive review of rapid-onset opioids for breakthrough pain. CNS Drugs. 2012;26:509–35.
Davies AN, Dickman A, Reid C, Stevens AM, Zeppetella G. The management of cancer-related breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. Eur J Pain. 2009;13:331–8.
Portenoy RK, Hagen NA. Breakthrough pain: definition, prevalence and characteristics. Pain. 1990;41:273–81.
Petzke F, Radbruch L, Zech D, et al. Temporal presentation of chronic cancer pain: transitory pains on admission to a multidisciplinary pain clinic. J Pain Symptom Manage. 1999;17:391–401.
Portenoy RK, Payne D, Jacobsen P. Breakthrough pain: characteristics and impact in patients with cancer pain. Pain. 1999;81:129–34.
Bennett D, Burton AW, Fishman S, et al. Consensus panel recommendations for the assessment and management of breakthrough pain. Part 2. Management. P & T. 2005;30:354–61.
Zeppetella G, O’Doherty CA, Collins S. Prevalence and characteristics of breakthrough pain in cancer patients admitted to a hospice. J Pain Symptom Manage. 2000;20:87–92.
Swanwick M, Haworth M, Lennard RF. The prevalence of episodic pain in cancer: a survey of hospice patients on admission. Palliat Med. 2001;15:9–18.
Mercadante S, Maddaloni S, Roccella S, Salvaggio L. Predictive factors in advanced cancer pain treated only by analgesics. Pain. 1992;50:151–5.
Bruera E, Scholler T, Wenk R, et al. A prospective multicentre assessment of the Edmonton staging system for cancer pain. J Pain Symptom Manage. 1995;10:348–55.
Bruera E, Fainsinger R, MacEachern T, et al. The use of methylphenidate in patients with incident cancer pain receiving regular opiates: a preliminary report. Pain. 1992;50:75–7.
Hwang SS, Chang VT, Kasimis B. Cancer breakthrough pain characteristics and responses to treatment at a VA medical center. Pain. 2003;101:55–64.
Fortner BV, Okon TA, Portenoy RK. A survey of pain-related hospitalizations, emergency department visits, and physician office visits reported by cancer patients with and without history of breakthrough pain. J Pain. 2002;3:38–44.
Fortner BV, Demarco G, Irving G, et al. Description and predictors of direct and indirect costs of pain reported by cancer patients. J Pain Symptom Manage. 2003;25:9–18.
Zeppetella G. Opioids for the management of breakthrough cancer pain in adults: a systematic review undertaken as part of an EPCRC opioid guidelines project. Palliat Med. 2011;25:516–24.
Patel VF, Liu F, Brown MB. Advances in oral transmucosal drug delivery. J Control Release. 2011;153:106–16.
Zhang H, Zhang J, Streisand JB. Oral mucosal drug delivery: clinical pharmacokinetics and therapeutic applications. Clin Pharmacokinet. 2002;41:661–80.
Medication Guide—Fentanyl sublingual spray. Food and Drug Administration web site. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM287863.pdf. Accessed Feb 5 2013.
Rauck R, Reynolds L, Geach J, et al. Efficacy and safety of fentanyl sublingual spray for the treatment of breakthrough cancer pain: a randomized, double-blind, placebo-controlled study. Curr Med Res Opin. 2012;28:859–70.
Highlights of Prescribing Information. Food and Drug Administration web site. www.accessdata.fda.gov/drugsatfda_docs/label/2012/202788s000lbl.pdf. Accessed Feb 5 2013.
Acknowledgments
Dr. Zeppetella is the guarantor for this article, and takes responsibility for the integrity of the work as a whole. No external funding was received for this manuscript, which was provided independently of the pharmaceutical industry.
Conflict of interest
Dr. Zeppetella declares he has no conflicts of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Zeppetella, G. Fentanyl Sublingual Spray for Breakthrough Pain in Cancer Patients. Pain Ther 2, 1–9 (2013). https://doi.org/10.1007/s40122-013-0008-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-013-0008-9