Abstract
Introduction
Neuropathic pain is a complex, chronic pain state that is usually accompanied by tissue injury. With neuropathic pain, the nerve fibers themselves may be damaged, dysfunctional, or injured.
Methods
A series of pharmacophoric hybrids of substituted aryl semicarbazides incorporated into a fused triazolo-thiadiazole nucleus were synthesized and evaluated for neuropathic pain activity. After the assessment of neurotoxicity and peripheral analgesic activity, the compounds were evaluated in two peripheral neuropathic pain models, the chronic constriction injury and partial sciatic nerve ligation, to assess their antiallodynic and antihyperalgesic potential.
Results
Selected compounds exhibiting promising efficacies (4b, 6a, and 7e) revealed median effective dose (ED50) values ranging from 7.62–28.71 mg/kg in four behavioral assays of allodynia and hyperalgesia (spontaneous pain, tactile allodynia, cold allodynia, and mechanical hyperalgesia). Studies carried out to assess the underlying mechanism revealed that compounds suppressed the inflammatory component of the neuropathic pain by inhibiting tumor necrosis factor (TNF)-alpha and preventing oxidative and nitrosative stress.
Conclusion
Using a hybrid design approach, the present study identified novel chemical compounds that could be a potential lead for the treatment of neuropathic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuropathic pain syndromes characterized by neuronal hyperexcitability in damaged areas of the peripheral or central nervous system involve complex pathophysiological processes [1]. The development of inflammatory microenvironment at the site of nerve injury and the release of inflammatory mediators, together with their coupled signaling pathways, contribute to the generation and maintenance of neuropathic pain [2, 3]. Following nerve injury, peripheral as well as central sensitization occurs [4, 5] with upregulation of tumor necrosis factor-alpha (TNF-alpha), a pro-inflammatory cytokine, and its receptors in Schwann cells, endothelial cells, and in the dorsal horn of the spinal cord and hippocampus [6–8]. TNF-alpha, a key mediator in the inflammation, activates T cells and macrophages, thereby initiating the innate immune response. Consequently, the release of other inflammatory cytokines, sympathomimetic amines, prostaglandins, and nitric oxide (NO) is stimulated, which are involved in sensitization of primary afferent nociceptors [5–8]. Activated microglia and pro-inflammatory cytokines also induce the generation of free radicals leading to oxidative and nitrosative stresses, which exaggerate pain states [9, 10]. Inhibiting TNF synthesis with thalidomide or treatment with anti-TNF neutralizing antibodies at the time of nerve injury blocks the development of hyperalgesia and allodynia in neuropathic animals [11, 12].
In recent years, the condensed bridgehead nitrogen heterocyclic system of triazolo-thiadiazole, which may be considered as the cyclic analog of thiosemicarbazide and biguanide has received considerable attention. A wide spectrum of biological activities, specifically anticonvulsant [13], analgesic [14], anxiolytic [15], and anti-inflammatory [16] properties has been reported for triazolo-thiadiazole in the literature. The 1,2,4-triazole core of the above fused system has gained considerable attention regarding its action against neuropathic pain acting through various targets. Many triazole-based P2X7 antagonists [17, 18] sodium channel blockers [19], and σ-receptor inhibitors [20] have been reported. The literature also reveals many 1,2,4-triazole-based cannabinoid modulators [21, 22] possessing antinociceptive efficacies.
The primary focus of our research has been on the design and synthesis of pharmacophoric hybrids of aryl semicarbazones to develop multifunctional leads useful in the treatment of neurological disorders such as epilepsy and neuropathic pain [23–26]. We have previously reported the cyclization of various aryl semicarbazones to 1,2,4-triazoles, which resulted in improved anticonvulsant activities [27]. Moreover, the literature reveals that acylthiosemicarbazides and their corresponding cyclized 1,3,4-thiadiazole derivatives possess anti-inflammatory [28, 29] and analgesic [30] activities.
In view of the above reports, the design and synthesis of pharmacophoric hybrids of aryl semicarbazides into triazolo-thiadiazole templates was accomplished followed by assessment of their antinociceptive potential and underlying mechanism of action. Various reports on the antinociceptive efficacy of 4-aminobutyric acid (GABA) and gabapentin [31] and our research on N-spiro GABA derivatives [32] prompted us to explore the structure–activity relationships of GABA and N-spiro GABA derivatives in the cyclized triazolo-thiadiazole template.
Materials and Methods
Chemistry
General
Melting points were measured in open capillary tubes on a Buchi 530 melting point apparatus (Buchi, Flawil, Switzerland) and are uncorrected. Proton nuclear magnetic resonance (1H-NMR) spectra were recorded for the compounds on a Bruker Avance (300 MHz) HMR machine (Bruker, Fällanden, Switzerland). Chemical shifts are reported in parts per million (ppm) using tetramethyl silane (TMS) as an internal standard. Mass spectra were measured with a Shimadzu GC–MS-QP5000 spectrophotometer. Elemental analyses (C, H, and N) were undertaken with a Perkin-Elmer model 240C analyzer, and all analyses were consistent with theoretical values (within ±0.4%) unless indicated. The homogeneity of the compounds was monitored by ascending thin-layer chromatography (TLC) on silicagel-G (Merck, Darmstadt, Germany) coated aluminum plates, visualized by iodine vapor and UV light.
General Scheme for the Synthesis of Potassium Dithiocarbazinate (2a–2e)
Substituted phenyl semicarbazide, 1a–1e (0.083 mol) was added to a solution of potassium hydroxide (0.125 mol) in methanol (50 mL) at 0–5°C under stirring. To this, carbon disulfide (0.025 mol) was added dropwise with constant stirring. The reaction mixture was stirred continuously for 12 h at room temperature. The precipitated potassium dithiocarbazinate salt was filtered, washed with anhydrous ether, and dried in a vacuum. The potassium salt thus obtained was used in the next step without further purification.
General Scheme for the Synthesis of 4-Amino-5-substituted-3-mercapto-(4H)-1,2,4-triazoles (3a–3e)
Potassium dithiocarbazinate derivatives, 2a–2e (0.02 mol) and hydrazine hydrate (99%, 0.04 mol) in water (25 mL) were refluxed for 10–15 h with occasional shaking. The reaction mixture was cooled to room temperature and diluted with cold water (10 mL). On acidification with dilute hydrochloric acid (HCl), a white precipitate resulted, which was filtered, washed with cold water, dried, and recrystallized from ethanol.
General Scheme for the Synthesis of 3,6-Disubstituted-[1, 2, 4]-triazolo-[3,4-b]-1,3,4-thiadiazoles (4a–43e, 5a–5e, 6a–6e, 7a–7e, 8a–8e)
An equimolar mixture (0.01 mol) of 4-amino-5-substituted-3-mercapto-(4H)-1,2,4-triazoles (3a–3e) and aromatic acids in phosphorous oxychloride (10 mL) were refluxed for 5 h. After the completion of the reaction, the reaction mixture was slowly poured into crushed ice with vigorous stirring and neutralized with sodium bicarbonate (NaHCO3). The precipitated solid was filtered, washed with cold water, and recrystallized from ethanol.
6-(2-Aminoethyl)-N-(4-bromophenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (4a)
Yield: 64%; melting point (m.p.): 185°C; 1H NMR (DMSO-d6) δ: 2.01 (p, 2H), 2.63 (t, 2H), 2.84 (t, 2H), 4.78 (br s, 2H, D2O exchangeable), 6.91 (d, 2H), 7.13 (d, 2H), 8.24 (br s, NH, D2O exchangeable), 13C NMR δ 34.3, 41.8, 117.2, 119.4, 134.6, 139.2, 159.8, 168.8, 169.1: MS (ESI) 338.99 (MH)+. Anal. C11H11BrN6S (C, H, N).
6-(2-Aminoethyl)-N-(4-chlorophenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (4b)
Yield: 72%; m.p.: 192°C; 1H NMR (DMSO-d6) δ: 2.03 (p, 2H), 2.66 (t, 2H), 2.83 (t, 2H), 4.72 (br s, 2H, D2O exchangeable), 7.01 (d, 2H), 7.22 (d, 2H), 8.63 (br s, NH, D2O exchangeable), 13C NMR δ 34.2, 41.6, 122.2, 127.4, 129.6, 137.2, 157.8, 167.6, 168.2: MS (ESI) 295.05 (MH)+. Anal. C11H11ClN6S (C, H, N).
6-(2-Aminoethyl)-N-(2,4-dimethylphenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (4c)
Yield: 71%; m.p.: 178°C; 1H NMR (DMSO-d6) δ: 2.02 (p, 2H), 2.14 (s, 3H), 2.37 (s, 3H), 2.68 (t, 2H), 2.84 (t, 2H), 4.84 (br s, 2H, D2O exchangeable), 6.57 (d, 1H), 6.87–6.91 (m, 2H), 9.10 (br s, NH, D2O exchangeable), 13C NMR δ 17.2, 21.6, 34.1, 41.6, 116.3, 126.3, 128.1, 132.1, 137.2, 139.4, 157.3, 167.1, 168.2: MS (ESI) 289.12 (MH)+. Anal. C13H16N6S (C, H, N).
6-(2-Aminoethyl)-N-(2,5-dimethylphenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (4d)
Yield: 68%; m.p.: 152°C; 1H NMR (DMSO-d6) δ: 2.04 (p, 2H), 2.13 (s, 6H), 2.38 (s, 3H), 2.66 (t, 2H), 2.86 (t, 2H), 4.59 (br s, 2H, D2O exchangeable), 6.67–6.69 (m, 2H), 6.94 (d, 1H), 9.10 (br s, NH, D2O exchangeable), 13C NMR δ 17.2, 21.6, 34.1, 41.6, 115.3, 118.2, 126.1, 129.2, 136.1, 141.2, 157.2, 167.1, 168.1: MS (ESI) 289.12 (MH)+. Anal. C13H16N6S (C, H, N).
6-(2-Aminoethyl)-N-(2,6-dimethylphenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (4e)
Yield: 61%; m.p.: 144°C; 1H NMR (DMSO-d6) δ: 2.01 (p, 2H), 2.14 (s, 6H), 2.66 (t, 2H), 2.88 (t, 2H), 4.71 (br s, 2H, D2O exchangeable), 6.69 (t, 1H), 6.96 (d, 2H), 9.41 (br s, NH, D2O exchangeable), 13C NMR δ 17.8, 34.1, 41.6, 121.4, 128.2, 136.4, 139.2, 157.1, 167.2, 168.3: MS (ESI) 289.12 (MH)+. Anal. C13H16N6S (C, H, N).
N-(4-Bromophenyl)-6-(heptan-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (5a)
Yield: 69%; m.p.: 157°C; 1H NMR (DMSO-d6) δ: 0.93–1.10 (t, 6H), 1.35–1.40 (m, 4H), 1.56–1.62 (q, 4H), 2.66–2.68 (t, 1H), 6.94 (d, 2H), 7.16 (d, 2H), 8.43 (br s, 1H, D2O exchangeable), 13C NMR δ 14.2, 20.3, 38.3, 116.1, 118.2, 132.3, 137.2, 157.2, 167.2, 168.1: MS (ESI) 394.06 (MH)+. Anal. C16H20BrN5S (C, H, N).
N-(4-Chlorophenyl)-6-(heptan-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (5b)
Yield: 78%; m.p.: 171°C; 1H NMR (DMSO-d6) δ: 0.96–1.11 (t, 6H), 1.37–1.41 (m, 4H), 1.54–1.59 (q, 4H), 2.65–2.67 (t, 1H), 7.04 (d, 2H), 7.25 (d, 2H), 8.81 (br s, 1H, D2O exchangeable), 13C NMR δ 14.2, 20.3, 38.3, 122.7, 127.1, 129.5, 137.1, 157.2, 167.3, 168.2: MS (ESI) 350.11 (MH)+. Anal. C16H20ClN5S (C, H, N).
N-(2,4-Dimethylphenyl)-6-(heptan-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (5c)
Yield: 73%; m.p.: 153°C; 1H NMR (DMSO-d6) δ: 0.97–1.11 (t, 6H), 1.36–1.42 (m, 4H), 1.55–1.60 (q, 4H), 2.14 (s, 3H), 2.37 (s, 3H), 2.66–2.69 (t, 1H), 6.59 (d, 1H), 6.87–6.92 (m, 2H), 9.40 (br s, 1H, D2O exchangeable), 13C NMR δ 14.2, 17.3, 20.3, 21.1, 38.3, 116.3, 126.3, 128.2, 131.2, 137.2, 139.3, 157.3, 167.4, 168.1: MS (ESI) 344.19 (MH)+. Anal. C18H25N5S (C, H, N).
N-(2,5-Dimethylphenyl)-6-(heptan-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (5d)
Yield: 75%; m.p.: 138°C; 1H NMR (DMSO-d6) δ: 0.96–1.12 (t, 6H), 1.36–1.41 (m, 4H), 1.54–1.60 (q, 4H), 2.13 (s, 3H), 2.36 (s, 3H), 2.67–2.69 (t, 1H), 6.57–6.61 (m, 2H), 6.91 (d, 1H), 8.89 (br s, 1H, D2O exchangeable), 13C NMR δ 14.2, 17.3, 20.3, 21.1, 38.3, 115.2, 118.3, 126.1, 129.2, 136.2, 141.2, 157.3, 167.3, 168.1: MS (ESI) 344.19 (MH)+. Anal. C18H25N5S (C, H, N).
N-(2,6-Dimethylphenyl)-6-(heptan-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (5e)
Yield: 80%; m.p.: 129°C; 1H NMR (DMSO-d6) δ: 0.95–1.12 (t, 6H), 1.36–1.42 (m, 4H), 1.56–1.61 (q, 4H), 2.15 (s, 6H), 2.64–2.67 (t, 1H), 6.67 (t, 1H), 6.98 (d, 2H), 9.41 (br s, 1H, D2O exchangeable), 13C NMR δ 14.2, 17.3, 20.3, 38.3, 121.1, 128.3, 136.2, 137.5, 157.2, 167.2, 168.1: MS (ESI) 344.18 (MH)+. Anal. C18H25N5S (C, H, N).
N-(4-Bromophenyl)-6-(pyridin-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (6a)
Yield: 81%; m.p.: 203°C; 1H NMR (DMSO-d6) δ: 6.94 (d, 2H), 7.13 (d, 2H), 7.89 (d, 2H), 8.45 (d, 2H), 8.91 (br s, 1H, D2O exchangeable, 13C NMR δ 116.3, 118.3, 121.2, 132.4, 137.1, 143.1, 143.6, 149.2, 157.3, 167.4: MS (ESI) 372.98 (MH)+. Anal. C14H9BrN6S (C, H, N).
N-(4-chlorophenyl)-6-(pyridin-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (6b)
Yield: 65%; m.p.: 216°C; 1H NMR (DMSO-d6) δ: 7.02 (d, 2H), 7.23 (d, 2H), 7.90(d, 2H), 8.46 (d, 2H), 8.95 (br s, 1H, D2O exchangeable), 13C NMR δ 121.2, 122.1, 127.3, 129.2, 137.1, 143.1, 143.6, 149.2, 157.3, 167.4: MS (ESI) 329.03 (MH)+. Anal. C14H9ClN6S (C, H, N).
N-(2,4-Dimethylphenyl)-6-(pyridin-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (6c)
Yield: 62%; m.p.: 192°C; 1H NMR (DMSO-d6) δ: 2.14 (s, 3H), 2.36 (s, 3H), 6.58 (d, 1H), 6.88–6.94 (m, 2H), 7.91 (d, 2H), 8.54 (d, 2H), 9.12 (br s, D2O exchangeable, 1H), 13C NMR δ 17.3, 21.1, 116.3, 121.2, 126.1, 128.1, 131.3, 137.2, 139.3, 143.0, 143.5, 149.1, 157.1, 167.2: MS (ESI) 323.10 (MH)+. Anal. C16H14N6S (C, H, N).
N-(2,5-Dimethylphenyl)-6-(pyridin-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (6d)
Yield: 68%; m.p.: 183°C; 1H NMR (DMSO-d6) δ: 2.13 (s, 3H), 2.37 (s, 3H), 6.66–6.71 (m, 2H), 6.90 (d, 2H), 5.64 (br s, D2O exchangeable, 1H), 7.92 (d, 2H), 8.45 (d, 2H), 13C NMR δ 17.3, 21.1, 115.2, 118.3, 121.4, 126.1, 129.2, 136.2, 141.2, 143.1, 143.6, 149.2, 157.2, 167.1: MS (ESI) 323.10 (MH)+. Anal. C16H14N6S (C, H, N).
N-(2,6-Dimethylphenyl)-6-(pyridin-4-yl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (6e)
Yield: 70%; m.p.: 161°C; 1H NMR (DMSO-d6) δ: 2.15 (s, 6H), 6.65 (t, 1H), 6.96 (d, 2H), 7.91 (d, 2H), 8.47 (d, 2H), 9.21 (br s, D2O exchangeable, 1H), 13C NMR δ 17.3, 121.1, 128.3, 136.2, 137.5, 143.1, 143.4, 149.1, 157.3, 167.4: MS (ESI) 323.10 (MH)+. Anal. C16H14N6S (C, H, N).
N-(4-Bromophenyl)-6-(4-nitrophenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (7a)
Yield: 68%; m.p.: 199°C; 1H NMR (DMSO-d6) δ: 6.93 (d, 2H), 7.14 (d, 2H), 7.81 (d, 2H), 8.08 (d, 2H), 9.71 (br s, D2O exchangeable, 1H), 13C NMR δ 116.1, 118.2, 124.3, 128.1, 132.3, 137.1, 139.2, 143.2, 147.4, 157.3, 167.3: MS (ESI) 416.97 (MH)+. Anal. C15H9BrN6O2S (C, H, N).
N-(4-Chlorophenyl)-6-(4-nitrophenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazole-3-amine (7b)
Yield: 69%; m.p.: 207°C; 1H NMR (DMSO-d6) δ: 7.01 (d, 2H), 7.25 (d, 2H), 7.83 (d, 2H), 8.10 (d, 2H), 9.12 (br s, D2O exchangeable, 1H), 13C NMR δ 122.7, 124.3, 127.1, 128.1, 129.5, 137.1, 139.2, 143.2, 147.4, 157.0, 167.1: MS (ESI) 373.02 (MH)+. Anal. C15H9ClN6O2S (C, H, N).
N-(2,4-Dimethylphenyl)-6-(4-nitrophenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (7c)
Yield: 77%; m.p.: 176°C; 1H NMR (DMSO-d6) δ: 2.13 (s, 3H), 2.34 (s, 3H), 6.56 (d, 1H), 6.87–6.92 (m, 2H) 7.81 (d, 2H), 8.10 (d, 2H), 8.76 (br s, D2O exchangeable, 1H), 13C NMR δ 17.3, 21.1, 116.3, 124.2, 126.1, 128.1, 128.6, 131.3, 137.2, 139.3, 139.4, 143.1, 147.1, 157.3, 167.1: MS (ESI) 367.09 (MH)+. Anal. C17H14N6O2S (C, H, N).
N-(2,5-Dimethylphenyl)-6-(4-nitrophenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (7d)
Yield: 73%; m.p.: 162°C; 1H NMR (DMSO-d6) δ: 2.14 (s, 3H), 2.35 (s, 3H), 6.66–6.70 (m, 2H), 6.90 (d, 2H), 7.81 (d, 2H), 8.09 (d, 2H), 9.71 (br s, D2O exchangeable, 1H), 13C NMR δ 17.3, 21.1, 115.1, 118.2, 124.4, 126.3, 128.1, 129.0, 136.1, 139.6, 141.2, 143.1, 147.4, 157.1, 167.2: MS (ESI) 367.09 (MH)+. Anal. C17H14N6O2S (C, H, N).
N-(2,6-Dimethylphenyl)-6-(4-nitrophenyl)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-3-amine (7e)
Yield: 71%; m.p.: 151°C; 1H NMR (DMSO-d6) δ: 2.16 (s, 6H), 6.65 (t, 1H), 6.96 (d, 2H), 7.82 (d, 2H), 8.03 (d, 2H), 9.65 (br s, D2O exchangeable, 1H), δ 17.3, 121.1, 124.4, 128.3, 136.2, 137.5, 139.2, 143.1, 147.4, 157.3, 167.3: MS (ESI) 367.09 (MH)+. Anal. C17H14N6O2S (C, H, N).
3-(3-(3-(4-Bromophenylamino)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-6-yl)propyl)-3-azaspiro[5.5]undecane-2,4-dione (8a)
Yield: 80%; m.p.: 174°C; 1H NMR (DMSO-d6) δ: 1.42–1.53 (m, 10H), 2.08–2.17 (m, 6H), 2.91 (t, 2H), 3.01 (t, 2H), 6.92 (d, 2H), 7.13 (d, 2H), 9.32 (br s, D2O exchangeable, 1H), 13C NMR δ 15.3, 20.4, 25.1, 26.2, 39.1, 41.2, 41.4, 116.1, 118.2, 132.3, 137.2, 157.1, 167.1, 168.2, 171.3: MS (ESI) 517.09 (MH)+. Anal. C22H25BrN6O2S (C, H, N).
3-(3-(3-(4-Chlorophenylamino)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-6-yl)propyl)-3-aza spiro[5.5]undecane-2,4-dione (8b)
Yield: 75%; m.p.: 183°C; 1H NMR (DMSO-d6) δ: 1.42–1.53 (m, 10H), 2.08–2.15 (m, 6H), 2.94 (t, 2H), 3.02 (t, 2H), 7.02 (d, 2H), 7.22 (d, 2H), 9.08 (br s, D2O exchangeable, 1H), 13C NMR δ 15.3, 20.4, 25.1, 26.1, 39.3, 41.2, 41.3, 122.0, 127.4, 129.1, 137.2, 157.0, 167.4, 168.1, 171.3: MS (ESI) 473.14 (MH)+. Anal. C22H25ClN6O2S (C, H, N).
3-(3-(3-(2,4-Dimethylphenylamino)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-6-yl)propyl)-3- azaspiro[5.5]undecane-2,4-dione (8c)
Yield: 74%; m.p.: 159°C; 1H NMR (DMSO-d6) δ: 1.43–1.54 (m, 10H), 2.09–2.17 (m, 9H), 2.35 (t, 3H), 2.92 (t, 2H), 3.02 (t, 2H), 6.59 (d, 1H), 6.88–6.93 (m, 2H), 9.63 (br s, D2O exchangeable, 1H), 13C NMR δ 15.1, 17.5, 20.1, 21.2, 25.3, 26.1, 39.2, 41.1, 41.4, 116.1, 126.2, 128.2, 131.3, 137.1, 139.3, 157.1, 167.2, 168.1, 171.4: MS (ESI) 467.21 (MH)+. Anal. C24H30N6O2S (C, H, N).
3-(3-(3-(2,5-Dimethylphenylamino)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-6-yl)propyl)- 3-azaspiro[5.5]undecane-2,4-dione (8d)
Yield: 75%; m.p.: 141°C; 1H NMR (DMSO-d6) δ: 1.43–1.53 (m, 10H), 2.08–2.15 (m, 9H), 2.35 (s, 3H), 2.91 (t, 2H), 3.03 (t, 2H), 6.65–6.69 (m, 2H), 6.89 (d, 2H), 9.64 (br s, D2O exchangeable, 1H), 13C NMR δ 15.3, 17.4, 20.3, 21.1, 25.1, 26.2, 39.1, 41.2, 41.4, 115.1, 118.2, 126.1, 129.2, 136.3, 141.1, 157.3, 167.1, 168.2, 171.2: MS (ESI) 467.21 (MH)+. Anal. C24H30N6O2S (C, H, N).
3-(3-(3-(2,6-Dimethylphenylamino)-[1, 2, 4]triazolo[3,4-b][1, 3, 4]thiadiazol-6-yl)propyl)-3-azaspiro[5.5]undecane-2,4-dione (8e)
Yield: 72%; m.p.: 124°C; 1H NMR (DMSO-d6) δ: 1.42–1.54 (m, 10H), 2.07–2.17 (m, 6H), 2.25 (s, 6H), 2.93 (t, 2H), 3.02 (t, 2H), 6.66 (t, 1H), 6.97 (d, 2H), 9.62 (br s, D2O exchangeable, 1H), 13C NMR δ 15.1, 17.3, 20.1, 25.1, 26.1, 39.2, 41.1, 41.5, 121.2, 128.2, 129.1, 136.4, 137.2, 157.2, 167.2, 168.1, 171.1: MS (ESI) 467.21 (MH)+. Anal. C24H30N6O2S (C, H, N).
Pharmacology
Swiss albino mice (either sex) with weights ranging from 20–25 g were used for the assessment of neurotoxicity, acetic acid-induced writhing, and formalin-induced flinching model. Wistar rats of either sex (200–250 g) were used for the inflammatory and neuropathic pain models. All experiments were approved by the Institutional Animal Ethics Committee. Animals were housed six (mice) and four (rats) per cage at constant temperature under a 12 h light/dark cycle (lights on at 7:00 am), with food and water ad libitum.
Motor Impairment
Minimal motor impairment was measured in mice by the rotarod test. The mice were trained to stay on an accelerating rotarod that rotates at 10 revolutions per minute. The rod diameter was 3.2 cm. Neurotoxicity was indicated by the inability of the animal to maintain equilibrium on the rod for at least 1 min in each of the three trials [33].
Acetic Acid-Induced Writhing
Writhing was induced in a group of mice by an intraperitoneal injection of 0.1 mL of 2% (v/v) acetic acid. Test group mice received acetic acid 30 min after the administration of test compounds. The number of writhings occurring for a period of 30 min was recorded. For scoring purposes, a writhe was indicated by stretching of the abdomen with simultaneous stretching of at least one hind limb. The percentage inhibition of the writhing response was calculated [34].
Formalin-Induced Flinching
The test involved intraplantar injection of 25 μL of 1% formalin into the hind paw of mice, which resulted in flinches in the paw in the early phase (0–5 min) and the late phase (10–30 min) [35]. Time spent in paw licking and biting was monitored in each 5 min and calculated for both the phases. Test compounds were administered 30 min before the experiment.
Unilateral Mononeuropathy: Chronic Constriction Nerve Injury Model
Unilateral mononeuropathy was produced in rats using the chronic constriction injury (CCI) model performed essentially as described by Bennett and Xie [36]. The rats were anesthetized with an intraperitoneal dose of ketamine (55 mg/kg) and xylazine (5 mg/kg) with additional doses of the anesthetic given as needed. Under aseptic conditions, a 3 cm incision was made on the lateral aspect of the left hind limb at the mid-thigh level. The left paraspinal muscles were then separated from the spinous processes and the common left sciatic nerve was exposed just above the trifurcation point. Four loose ligatures were made with a 4-0 braided silk suture around the sciatic nerve with about 1-mm spacing. The wound was then closed by suturing the muscle using chromic catgut with a continuous suture pattern. Finally, the skin was closed using silk thread with horizontal-mattress suture pattern.
Induction of Peripheral Mononeuropathy: Partial Sciatic Nerve Ligation Model
As described by Seltzer et al. [37], in anesthetized rats, the left sciatic nerve was exposed at mid-thigh level through a small incision, cleared of adhering muscle tissue, and one-half of the nerve thickness was tightly ligated using 7.0 silk suture. The wound was closed and dusted with neomycin powder. The animals were then transferred to their home cages and left for recovery.
Sensory Testing Using Nociceptive Assays
Compounds (100 mg/kg, i.p.) were administered at t = 0, in 30% (v/v) PEG 400. The control group of rats received only the vehicle. Gabapentin (100 mg/kg, i.p.) was used as a positive control. Paw withdrawal duration (PWD) was assessed in spontaneous pain and cold allodynia, and paw withdrawal threshold (PWT) was assessed in tactile allodynia and mechanical hyperalgesia. Percentage reversal in spontaneous pain, allodynia, or hyperalgesia was calculated for each animal as defined below [38],
Carrageenan-Induced Paw Edema and Quantification of TNF-alpha
Paw edema was induced in Wistar rats by intra-plantar injection of 50 μl of 2% carrageenan (λ-carrageenan, type IV, Sigma-Aldrich Company Ltd, Dorset, UK) diluted in saline. The volume of the paw edema (mL) was determined at 0, 60, 120, and 180 min using a water plethysmometer (Ugo Basile, Varese, Italy). Indomethacin (10 mg/kg, i.p.) was used as a positive control [39]. The percentage protection against inflammation was calculated as: Vc − Vd/Vc × 100, where Vc is the increase in paw volume in the absence of the test compound (control) and Vd is the increase of paw volume after administration of the test compound.
For the measurement of TNF-alpha, whole right hind paws were collected at the third hour after carrageenan injection. After rinsing with ice-cold normal saline, they were homogenized at 4°C, and the homogenate was centrifuged at 12,000 rpm for 5 min. The supernatant obtained was assayed using a TNF-alpha enzyme-linked immunosorbant assay (ELISA) kit [40].
Estimation of Total Nitrite/Nitrate
On day 9 post-CCI, after 2 h of administration of test compounds, the total nitrate/nitrite in the brain and sciatic nerve was estimated according to the reported procedure [9]. The method involved reduction of nitrate to nitrite followed by calorimetric estimation using Griess’s reagent. The concentration of nitrite in the supernatant was calculated using a standard curve and expressed as a percentage of the control.
2,2-Diphenyl-1-picrylhydrazyl Assay
A solution of 2,2-diphenyl-1-picrylhydrazyl (DPPH) was prepared by dissolving 5 mg DPPH in 2 mL methanol, and the solution was kept in the dark at 4°C. Varying concentrations of test compounds (200 μL) were taken in a 96-well microplate. Then, 5 μL methanolic DPPH solution (final concentration 300 μM) was added to each well. After 20 min incubation, absorbance of the solution was read using an ELISA plate reader (EL340 Biokinetic reader, Bio-Tek Instrumentation, CA, USA) at a wavelength of 517 nm. A methanolic solution of DPPH served as a control. A dose–response curve was plotted to determine the half maximal inhibitory concentration (IC50) values. All tests and analyses were run in triplicate and averaged [41]. Percentage scavenging was calculated according to the following equation.
Results
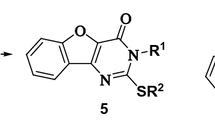
With the aim of synthesizing pharmacophoric hybrids of chemical entities with proven antinociceptive properties, the synthesis of various substituted phenyl semicarbazides (1a–1e), was accomplished from substituted anilines via urea formation as per our previously reported procedure [26]. Upon treatment with carbon disulfide in the presence of potassium hydroxide in ethanol, substituted phenyl semicarbazides gave the potassium salt of the corresponding 4-dithiocarbamate derivatives (2a–2e), which underwent ring closure with an excess of hydrazine hydrate to give 4-amino-3-substituted-5-mercapto-(4H)-1,2,4-triazoles (3a–3e). Resultant triazoles were further converted to 1,2,4-triazolo-[3,4-b]-1,3,4-thiadiazoles (4a–4e, 5a–5e, 6a–6e, 7a–7e, 8a–8e) via a one-pot reaction by condensation with various acids in the presence of phosphorous oxychloride as outlined in Fig. 1. The synthesis of N-spiro GABA (8a–8e) was accomplished as reported in our earlier work [32]. The structures of the synthesized compounds were characterized by both spectral and elemental analysis, and the data were within ±0.4% of the theoretical values.
Following assessment of neurotoxicity of the synthesized compounds by rotarod (data not shown), the non-neurotoxic compounds were further evaluated in acetic acid-induced writhing and formalin-induced flinching models (Table 1). The acetic acid-induced writhing model is a chemical pain test used to evaluate acute antinociceptive function, whereas the formalin model is a tonic inflammatory pain model used to distinguish peripherally and centrally acting compounds. It is characterized by two phases: first phase (0–5 min) occurs due to direct stimulation of nociceptors (C-fibers), whereas the second phase (10–30 min) results following the development of a localized inflammatory response along with activation of N-methyl-d-aspartate (NMDA) and non-NMDA receptors and nitric oxide production [42, 43]. All tested compounds, except 6e, suppressed the acetic acid-induced writhing response significantly (P < 0.01) in comparison with the control (Table 1). The standard drug, indomethacin, exhibited the highest percentage inhibition (96.1%). In the formalin-induced flinching model, all of the compounds showed significant suppression in both phases, with the exception of compounds 4a, 4d, 6d, 6e, 7c, and 8d, which were effective only in the second phase of the formalin assay. Indomethacin (72.1%) significantly reversed flinching responses in the second phase of the formalin assay. The triazolo-thiadiazoles were further evaluated in two well-established peripheral neuropathic pain models: the CCI and the partial sciatic nerve ligation (PSNL) model. In the CCI model, the left sciatic nerve proximal to the trifurcation point was constricted with four loose ligatures using 4-0 braided silk thread [36]. In the PSNL model, left sciatic nerve was exposed at mid-thigh level and one-half of the nerve thickness was tightly ligated using 7.0 silk sutures [37]. Four nociceptive assays with the aim of determining the severity of behavioral neuropathic responses, namely allodynia and hyperalgesia, were performed. The assays involved measurement of the degree of spontaneous (ongoing) pain and tests of hind limb withdrawal to cold and mechanical stimuli (tactile allodynia, cold allodynia, and mechanical hyperalgesia). A minimum of 10 min separated the testing procedures to reduce the influence of prior nociceptive testing. All animals included in the study showed altered sensory responses in all the four behavioral nociceptive tests, 9 days post-surgery. The sham-operated animals showed no significant difference from the preoperative baseline sensory response values. Percentage reversal in spontaneous pain, tactile allodynia, cold allodynia, and mechanical hyperalgesia was assessed day 9 post-surgery.
In the CCI model (Fig. 2), compounds 4b, 6a, and 7e completely reversed the spontaneous pain response throughout the time period of testing (0.5–2.0 h) similar to gabapentin. Compounds 7a and 8b were effective only up to 0.5 h, whereas compounds 4a, 4e, 7b, and 8e were effective up to 1 h. The onset of action of compound 7c was at 1 h. Other compounds were ineffective in this test. Three compounds, 4b, 6a, and 7e, were effective in attenuating the tactile allodynia throughout the 2 h experiment similar to gabapentin. Compound 4a was effective only up to 0.5 h of the experiment whereas compounds 4e, 8b, and 8e were effective up to 1 h. All other compounds were ineffective in this test. In the cold allodynia produced in CCI rats, significant reversal of paw withdrawal durations was observed at all timepoints by the administration of compounds 4b and 7e. Gabapentin was also found to be effective at all the timepoints. Compound 6b was effective only up to 0.5 h whereas compounds 4a, 6a, 7c, 8c, and 8e were effective up to 1 h of the experiment. Mechanical hyperalgesia was significantly attenuated at all the timepoints by 4b and 6a similar to gabapentin. Compounds 7b and 8e were effective only up to 0.5 h, whereas compounds 4e, 5a, 7e, and 8c were effective until 1 h. Compound 6c exhibited irregular activity pattern.
Efficacy of compounds in spontaneous pain (a), tactile allodynia (b), cold allodynia (c), and mechanical hyperalgesia (d) in chronic constriction injury rats. Each value represents the percent reversal (mean ± SEM) in spontaneous pain, tactile allodynia, cold allodynia, and mechanical hyperalgesia of four rats. Asterisk denotes a significant value, in comparison to their respective vehicle control at P < 0.05 (one-way analysis of variance [ANOVA], followed by post hoc Dunnet test)
Overall, it appears that in the CCI model of neuropathic pain compounds that showed promising results include 4b, 6a, 7e, and 8e, which were effective in four tests; 4a and 4e, effective in three tests; and 7b, 7c, 8b, and 8c, effective in two tests.
In the PSNL model (Fig. 3), the paw withdrawal durations due to spontaneous ongoing pain were significantly reduced by compounds 4b, 6a, and 7e throughout the experiment, similar to gabapentin. The compounds 7c and 8e were effective up to 0.5 h of the experiment, whereas compounds 4a, 4e, and 8b exhibited activity up to 1 h. The tactile allodynia produced in the PSNL model was effectively reversed by compounds 4b and 6a at all the timepoints, similar to gabapentin. Compound 4a was effective only up to 0.5 h of the experiment, whereas compounds 4e, 7e, 8b, 8c, and 8e were effective up to 1 h of the experiment. The onset of action for compound 6b was at 1 h. Cold allodynia produced in the PSNL model was completely reversed by compounds 4b, 6a, and 7e. Compounds 6b and 6d were effective only up to 0.5 h of the experiment, whereas compounds 4a, 4e, 6c, 8c, and 8e were effective up to 1 h of the experiment. Compounds 4b, 7b, and 7e significantly reversed mechanical hyperalgesia at all the timepoints, similar to gabapentin. Compounds 6a, 7a, and 8c were effective in first 1 h of the experiment. Compound 7c exhibited irregular activity. Overall, it appears, in the PSNL model, compounds that exhibited promising results included 4b, 6a, and 7e, which were effective in four tests; 4a, 4e, and 8a, effective in three tests; and 6b, 7c, 8b, and 8c, effective in two tests.
Efficacy of compounds in spontaneous pain (a), tactile allodynia (b), cold allodynia (c), and mechanical hyperalgesia (d) in partial sciatic nerve ligation rats. Each value represents the percent reversal (mean ± SEM) in spontaneous pain, tactile allodynia, cold allodynia, and mechanical hyperalgesia of four rats. Asterisk denotes a significant value, in comparison to their respective vehicle control at P < 0.05 (one-way analysis of variance [ANOVA], followed by post hoc Dunnet test)
Compounds exhibiting more than 90% reversal in one or more of the nociceptive assays (4b, 6a, and 7e) were taken further for ED50 studies (Table 2). In the CCI model, compound 6a reversed spontaneous pain with an ED50 value of 13.92 mg/kg at 0.5 h. Compound 4b reversed tactile and cold allodynia with an ED50 value of 7.62 and 16.92 mg/kg at 0.5 and 1 h, respectively. Compound 7e reversed mechanical hyperalgesia with an ED50 value of 12.94 mg/kg at 0.5 h. In the PSNL model, compound 4b reversed spontaneous pain and tactile allodynia with an ED50 value of 14.91 and 13.95 mg/kg at 0.5 and 1 h, respectively. In cold allodynia and mechanical hyperalgesia, compound 6a was the most effective compound with an ED50 value of 21.91 and 28.10 mg/kg at 0.5 and 1 h, respectively.
The significant reversal exhibited by most of the test compounds in acetic acid-induced writhing model supported their role as peripherally acting analgesics. Significant suppression of flinching observed in both the phases of formalin assay (Table 1) suggested the mediation of anti-inflammatory pathways. The carrageenan-induced paw edema model was used to investigate the probable role of the selective compounds (4b, 6a, and 7e) in the inhibition of inflammatory mediators. A significant reduction in edema was observed for compounds 4b, 6a, and 7e at all the timepoints (Table 3). TNF-α levels quantified in the carrageeenan injected paw were also found to be inhibited by compounds 4b, 6a, and 7e. As a result, there was inhibition of keratinocyte chemokines (KC), leading to subsequent inhibition of interleukin-1beta, prostanoids, and sympathomimetic amines, as evidenced by reduction of edema [44]. The occurrence of nitrosative stress following nerve injury as evident by the significant increase in nitrite and nitrate levels in both the brains and sciatic nerves of the rats, led us to estimate the levels of nitrite, a metabolite of nitrate in the brain and sciatic nerve of CCI rats using Griess’s reagent. Also, the free-radical scavenging activity of the compounds was assessed spectrophotometrically via the DPPH assay. No significant reduction of nitrite in the brain of CCI rats was found when compared to vehicle-treated animals for compounds 4b, 6a, and 7e. However, a significant reduction was observed in the sciatic nerve of the CCI animals when compared to the vehicle-treated group for 4b, 6a, and 7e. The results indicate the inhibition of local NO at the site of nerve injury. The compounds (4b, 6a, and 7e) were found to exhibit free-radical scavenging abilities in the DPPH assay, thereby acting by reducing oxidative stress (Table 4).
Discussion
The results obtained in the nociceptive assays provide an insight into the structure–activity relationships of the triazolo-thiadiazoles. Functionalization of the aryl ring of the semicarbazide fragment forming triazolo-thiadiazoles with dimethyl substitutions resulted in variable antinociceptive efficacy. Compounds having a 2,4-dimethyl substituted aryl semicarbazide fragment (6c, 7c, and 8c) reversed one or more nociceptive parameters in both CCI and PSNL animals. Introduction of a 2,5-dimethyl substituted aryl ring proved to be detrimental for the antinociceptive efficacy in both CCI and PSNL animals. Only one compound, 6d, was found to be effective against cold allodynia in PSNL animals. The introduction of electron-releasing 2,6-dimethyl substitutions (4e, 7e, and 8e) resulted in significant attenuation of one or more nociceptive parameters in neuropathic animals. Introduction of an electron-withdrawing halogen (bromo) para to the aryl ring resulted in significant activity against one or more nociceptive assays. Compounds 4a, 5a, 6a, and 7a were effective in CCI animals, whereas compounds 4a, 6a, 7a, and 8a were found to be effective in one or more nociceptive parameters in PSNL animals. Compounds with para chloro-substituted aryl rings (4b, 6b, 7b, and 8b) resulted in significant attenuation of one or more nociceptive parameters in neuropathic animals.
Accounting for the nociceptive efficacies observed for triazolo-thiadiazoles in the neuropathic pain models, it can be generalized that unlike 2-propylpentanyl substitution at the R2 position (5a–5e), 2-aminobutanyl substitution (4a, 4b, and 4e) at the R2 position was beneficial for nociceptive efficacy. Aryl substitution with a 4-nitobenzyl group (6a–6d) and heteroaryl substitution with an isonicotinyl group (7a, 7b, 7c, and 7e) resulted in significant attenuation of nociceptive parameters. N-spiro GABA substitution (8a, 8b, 8c, and 8e) also proved to be additive for antinociceptive efficacy.
In conclusion, utilizing a pharmacophoric hybrid approach, a series of structurally novel triazolo-thiadiazoles derivatives were synthesized and evaluated for acute antinociceptive, antiallodynic, and antihyperalgesic potential. In the carrageenan-induced paw edema model, in which there is a pronounced local TNF-alpha response, compounds 4b, 6a, and 7e significantly inhibited paw swelling as well as localized TNF-alpha levels in the paw, thereby suppressing the inflammatory component of neuropathic pain. The neuroprotection exhibited by compounds 4b, 6a, and 7e is also associated with their free-radical scavenging abilities and subsequent attenuation of oxidative and nitrosative stresses.
References
Yogeeswari Y, Ragavendran JV, Sriram D. Neuropathic pain: strategies in drug discovery and treatment. Expert Opin Drug Discov. 2007;2:169–84.
Sommer C, Galbraith JA, Heckman HM, Myers RR. Pathology of experimental compression neuropathy producing hyperesthesia. J Neuropathol Exp Neurol. 1993;52:223–33.
Frisen J, Risling M, Fried K. Distribution and axonal relations of macrophages in a neuroma. Neuroscience. 1993;55:1003–13.
Cunha FQ, Poole S, Lorenzetti B, Ferreira SH. The pivotal role of tumour necrosis factor alpha in the development of inflammatory hyperalgesia. Br J Pharmacol. 1992;107:660–4.
Woolf CJ, Allchorne A, Safieh-Garabedian B, Poole S. Cytokines, nerve growth factor and inflammatory hyperalgesia: the contribution of tumour necrosis factor alpha. Br J Pharmacol. 1997;121:417–24.
Shubayev VI, Myers RR. Upregulation and interaction of TNFalpha and gelatinases A and B in painful peripheral nerve injury. Brain Res. 2000;855:83–9.
Wagner R, Myers RR. Schwann cells produce tumor necrosis factor alpha: expression in injured and non-injured nerves. Neuroscience. 1996;73:625–9.
Ignatowski TA, Covey WC, Knight PR, Severin CM, Nickola TJ, Spengler RN. Brain-derived TNFalpha mediates neuropathic pain. Brain Res. 1999;841:70–7.
Padi SS, Kulkarni SK. Minocycline prevents the development of neuropathic pain, but not acute pain: possible anti-inflammatory and antioxidant mechanisms. Eur J Pharmacol. 2008;601:79–87.
Naik AK, Tandan SK, Dudhgaonkar SP, et al. Role of oxidative stress in pathophysiology of peripheral neuropathy and modulation by N-acetyl-l-cysteine in rats. Eur J Pain. 2006;10:573–9.
Sommer C, Marziniak M, Myers RR. The effect of thalidomide treatment on vascular pathology and hyperalgesia caused by chronic constriction injury of rat nerve. Pain. 1998;74:83–91.
Sommer C, Lindenlaub T, Teuteberg P, Schäfers M, Hartung T, Toyka KV. Anti-TNF-neutralizing antibodies reduce pain-related behavior in two different mouse models of painful mononeuropathy. Brain Res. 2001;913:86–9.
Chapleo CB, Myers PL, Smith AC, Tulloch IF, Turner S, Walter DS. Substituted 1,3,4-thiadiazoles with anticonvulsant activity. 3. Guanidines. J Med Chem. 1987;30:951–4.
Schenone S, Brullo C, Bruno O, et al. New 1,3,4-thiadiazole derivatives endowed with analgesic and anti-inflammatory activities. Bioorg Med Chem. 2006;14:1698–705.
Clerici F, Pocar D, Guido M, Loche A, Perlini V, Brufani M. Synthesis of 2-amino-5-sulfanyl-1,3,4-thiadiazole derivatives and evaluation of their antidepressant and anxiolytic activity. J Med Chem. 2001;44:931–6.
Boschelli DH, Connor DT, Bornemeier DA, et al. 1,3,4-Oxadiazole, 1,3,4-thiadiazole, and 1,2,4-triazole analogs of the fenamates: in vitro inhibition of cyclooxygenase and 5-lipoxygenase activities. J Med Chem. 1993;36:1802–10.
Carroll WA, Kalvin DM, Perez Medrano A, et al. Novel and potent 3-(2,3-dichlorophenyl)-4-(benzyl)-4H-1,2,4-triazole P2X7 antagonists. Bioorg Med Chem Lett. 2007;17:4044–8.
Florjancic AS, Peddi S, Perez Medrano A, et al. Synthesis and in vitro activity of 1-(2,3-dichlorophenyl)-N-(pyridin-3-ylmethyl)-1H-1,2,4-triazol-5-amine and 4-(2,3-dichlorophenyl)-N-(pyridin-3-ylmethyl)-4H-1,2,4-triazol-3-amine P2X7 antagonists. Bioorg Med Chem Lett. 2008;18:2089–92.
Chakravarty PK, Zuegner LL, Parsons WH, et al. Biaryl substituted triazoles as sodium channel blockers. US Patent 7,572,822.
Alberto DZ, Nadine J, Maria Pillar GJ, Maria Rosa CA, Jose CM. 1,2,4-Triazole derivatives as sigma receptor inhibitors. European Patent 1,921,073.
Jagerovic N, Hernandez-Folgado L, Alkorta I, et al. Discovery of 5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-3-hexyl-1 h-1,2,4-triazole, a novel in vivo cannabinoid antagonist containing a 1,2,4-triazole motif. J Med Chem. 2004;47:2939–42.
Lange JH, van Stuivenberg HH, Coolen HK, et al. Bioisosteric replacements of the pyrazole moiety of rimonabant: synthesis, biological properties, and molecular modeling investigations of thiazoles, triazoles, and imidazoles as potent and selective CB1 cannabinoid receptor antagonists. J Med Chem. 2005;48:1823–38.
Yogeeswari P, Ragavendran JV, Sriram D, et al. Discovery of 4-aminobutyric acid derivatives possessing anticonvulsant and antinociceptive activities: a hybrid pharmacophore approach. J Med Chem. 2007;50:2459–67.
Yogeeswari P, Sriram D, Thirumurugan R, et al. Discovery of N-(2,6-dimethylphenyl)-substituted semicarbazones as anticonvulsants: hybrid pharmacophore-based design. J Med Chem. 2005;48:6202–11.
Yogeeswari P, Sriram D, Saxena A, Thirumurugan R, Stables J. 2,4-Dimethoxyphenylsemicarbazones with anticonvulsant activity against three animal models of seizures: synthesis and pharmacological evaluation. Bioorg Med Chem. 2006;14:3106–12.
Yogeeswari P, Sriram D, Mehta S, et al. Anticonvulsant and neurotoxicity evaluation of some 6-substituted benzothiazolyl-2-thiosemicarbazones. Farmaco. 2005;60:1–5.
Shalini M, Yogeeswari P, Sriram D, Stables JP. Cyclization of the semicarbazone template of aryl semicarbazones: synthesis and anticonvulsant activity of 4,5-diphenyl-2H-1,2,4-triazol-3(4H)-one. Biomed Pharmacother. 2009;63:187–93.
Song Y, Connor DT, Sercel AD, et al. Synthesis, structure-activity relationships, and in vivo evaluations of substituted di-tert-butylphenols as a novel class of potent, selective, and orally active cyclooxygenase-2 inhibitors. 2. 1,3,4- and 1,2,4-thiadiazole series. J Med Chem. 1999;42:1161–9.
Palaska E, Sahin G, Kelicen P, Durlu NT, Altinok G. Synthesis and anti-inflammatory activity of 1-acylthiosemicarbazides, 1,3,4-oxadiazoles, 1,3,4-thiadiazoles and 1,2,4-triazole-3-thiones. Farmaco. 2002;57:101–7.
Amir M, Shikha K. Synthesis and anti-inflammatory, analgesic, ulcerogenic and lipid peroxidation activities of some new 2-[(2,6-dichloroanilino) phenyl]acetic acid derivatives. Eur J Med Chem. 2004;39:535–45.
Receveur JM, Bryans JS, Field MJ, Singh L, Horwell DC. Synthesis and biological evaluation of conformationally restricted gabapentin analogues. Bioorg Med Chem Lett. 1999;9:2329–34.
Yogeeswari P, Sriram D, Reddy ASK, Semwal A, Mishra R. Newer 4-aminobutyric acid derivatives for the treatment of epilepsy and neuropathic pain. Indian Patent Application No. 1138/CHE/2009 A (18/5/2009).
Dunham NW, Miya TA. A note on a simple apparatus for detecting neurological deficit in rats and mice. J Am Pharm Assoc Sci Eds. 1957;46:208–9.
Siegmund EA, Cadmus RA, Lu G. A method for evaluating both nonnarcotic and narcotic analgesics. Proc Soc Exp Biol. 1957;95:729–31.
Hunskaar S, Hole K. The formalin test in mice: dissociation between inflammatory and non-inflammatory pain. Pain. 1987;30:103–14.
Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. 1988;33:87–107.
Seltzer Z, Dubner R, Shir Y. A novel behavioral model of neuropathic pain disorders produced in rats by partial sciatic nerve injury. Pain. 1990;43:205–18.
Garth T, Whiteside JH, Jamie B, et al. Pharmacological characterisation of a rat model of incisional pain. Br J Pharmacol. 2004;141:85–91.
Harris JM, Spencer PS. A modified plethysmographic apparatus for recording volume changes in the rat paw. J Pharm Pharmacol. 1962;14:464–6.
Sekut L, Yarnall D, Stimpson SA, et al. Anti-inflammatory activity of phosphodiesterase (PDE)-IV inhibitors in acute and chronic models of inflammation. Clin Exp Immunol. 1995;100:126–32.
Mellors A, Tappel AL. The inhibition of mitochondrial peroxidation by ubiquinone and ubiquinol. J Biol Chem. 1966;241:4353–6.
Coderre TJ, Melzack RJ. The contribution of excitatory amino acids to central sensitization and persistent nociception after formalin-induced tissue injury. J Neurosci. 1992;12:3665–70.
Okuda K, Sakurada C, Takahashi M, Yamada T, Sakurada T. Characterization of nociceptive responses and spinal releases of nitric oxide metabolites and glutamate evoked by different concentrations of formalin in rats. Pain. 2001;92:107–15.
Da Silva KA, Manjavachi MN, Paszcuk AF, et al. Plant derived alkaloid (-)-cassine induces anti-inflammatory and anti-hyperalgesics effects in both acute and chronic inflammatory and neuropathic pain models. Neuropharmacology. 2011;62:967–77.
Acknowledgments
P. Yogeeswari is the guarantor for this article, and takes responsibility for the integrity of the work as a whole.
Conflict of interest
The authors declare that they have no conflicts of interest and received no funding for this study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Sharma, M., Deekshith, V., Semwal, A. et al. Discovery of Fused Triazolo-thiadiazoles as Inhibitors of TNF-alpha: Pharmacophore Hybridization for Treatment of Neuropathic Pain. Pain Ther 1, 3 (2012). https://doi.org/10.1007/s40122-012-0003-6
Received:
Published:
DOI: https://doi.org/10.1007/s40122-012-0003-6