Abstract
Introduction
Understanding antibiotic prescribing for uncomplicated urinary tract infection (uUTI) could help to optimize management. However, data on uUTI treatment patterns in the European Union are scarce. We used real-world data to evaluate adherence to antibiotic prescribing guidelines for femalepatients with uUTI in Germany.
Methods
This retrospective cohort study used anonymized German statutory health insurance claims data from the Wissenschaftliches Institut für Gesundheitsökonomie und Gesundheitssystemforschung from January 2013 to December 2019. Patients were female, aged ≥ 12 years, with an index uUTI diagnosis. Patient characteristics and treating physician specialties were examined overall and in sub-cohorts for recommended/non-recommended treatment (based on initial therapy adherence to German uUTI treatment guidelines) and optimal/sub-optimal outcome (based on a prescription of different antibiotics or a urinary tract infection-related episode).
Results
Overall, 144,645 uUTI cases in 124,971 patients were analyzed; 51,230 (35.4%) and 93,415 (64.6%) cases were assigned to the recommended/non-recommended treatment sub-cohorts, respectively. Clinically meaningful differences in age and comorbidities were observed between these sub-cohorts. Most cases had an optimal outcome (n = 122,823; 84.9%); of these, a higher proportion received antibiotics that were recommended but not as first-choice versus first-choice therapies as their initial treatment (58.6% vs. 35.3%). In the sub-optimal outcome cohort, 49.1% received antibiotics that were recommended but not as first-choice and 41.1% received first-choice therapies as their initial treatment. Most uUTIs were treated by general practitioners (GPs; 82.3%), followed by gynecologists (13.3%), and urologists (6.8%). Notably, 64.5% of initial therapy prescriptions filled by gynecologists and 32.1% by GPs were first-choice antibiotics.
Conclusion
A high proportion of prescribed treatments for the initial uUTI episode were not recommended by German uUTI guidelines as first-choice antibiotics. Prescribing adherence varied by physician specialty; specialists showed greater adherence to treatment guidelines versus GPs. This study provides a novel and multi-dimensional picture of uUTI treatment in Germany.
Plain Language Summary
Uncomplicated urinary tract infections are one of the most common infections in women. Doctors around the world use different types of antibiotics to treat people with uncomplicated urinary tract infections. We performed this study to find out more about how doctors in Germany use antibiotics to treat uncomplicated urinary tract infections. We looked at health records from female patients (aged 12+) in Germany. Overall, we examined 144,645 records. We found that around one in ten women use antibiotics to treat an uncomplicated urinary tract infection every year. We then checked to see if the doctors were giving people the right type of antibiotic, the right dose, and the right length of course. To do this, we checked against guidelines that were written by experts in Germany. We found that only one in three patients (35%) received treatment that met the guidelines. We also looked to see what differences there were between different types of doctors. For example, if general practitioners (family doctors) used different antibiotics to specialist doctors in hospitals. Four out of five patients (82%) were treated by general practitioners. We found that specialists were more likely to stick to the guidelines than general practitioners. Finally, we looked at how many patients recovered well after their first course of antibiotics. More than four out of five patients (80%) recovered well. Interestingly, more than half of the patients who had a good recovery (59%) received antibiotics that were not recommended by the guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Uncomplicated urinary tract infections (uUTIs) are among the most common bacterial infections in women; however, real-world data on uUTI treatment patterns in the European Union are scarce. |
We used anonymized statutory insurance claims data to evaluate the adherence to antibiotic prescribing guidelines overall and among different physician specialties for female patients with uUTI aged ≥ 12 years in Germany. |
Overall, 51,230 cases (35.4%) received recommended treatment (adherence to uUTI treatment guidelines) and 93,415 (64.6%) received non-recommended treatment (non-adherence to treatment guidelines); clinically meaningful differences between these groups were noted in terms of patient ages and comorbidities. |
Most uUTIs were treated by general practitioners (82.3%) and gynecologists (13.3%); gynecologists prescribed first-choice antibiotics for initial therapy in 64.5% of cases, while general practitioners did so for only 32.1% of cases. |
Many females with uUTIs in Germany receive initial treatment discordant with guidelines, including a high rate of antibiotics not recommended as for first-choice use. |
Introduction
Uncomplicated urinary tract infections (uUTIs) are among the most common bacterial infections experienced by women in the outpatient setting [1, 2]. There is a notable overlap in national and international guidelines for uUTI treatment, but there are also important differences regarding diagnosis and treatment recommendations [2,3,4,5]. Understanding the management approaches and prescribing practices of different physicians could help to optimize uUTI management.
The various medical specialties involved in uUTI management, including urologists, gynecologists, and family and internal medicine physicians, demonstrate different approaches to treatment and varying levels of concordance with guidelines [6]. Treatment decisions that do not align with guidelines can be driven by low levels of reliance on guidelines, but can also occur when physicians alter their antibiotic prescribing (i.e., longer duration and/or broader spectrum) to account for patient factors such as older age, presence of diabetes, and urinary tract infection (UTI) recurrence [7].
Empiric therapy for uUTIs should be tailored to the current distribution and regional susceptibility of pathogens to ensure an optimal outcome. Ny et al. [8] reported single-drug resistance rates among German outpatient UTI isolates as follows: amoxicillin/clavulanic acid (32.9%); trimethoprim (18.4%); trimethoprim/sulfamethoxazole (16.1%); ciprofloxacin (6.1%); cefuroxime, ceftazidime, and cefotaxime (4.3–7.2%); fosfomycin (1.1%); and nitrofurantoin (0.4%). The rate [95% confidence interval (CI)] of resistant and intermediate E. coli isolates from outpatient UTIs was 7.9% (4.7–12.4%) for extended-spectrum beta-lactamase positive (ESBL+), 7.0% (4.4–10.7%) for multi-drug resistance (MDR), 3.7% (1.6–7.2%) for ESBL+ ciprofloxacin resistance, and 1.9% (0.5–4.7%) for ESBL+ ciprofloxacin plus gentamicin resistance. While single-drug resistance rates show that there are antibiotic options available to most patients with uUTI in Germany, the MDR and ESBL+ rates suggest that there is an unmet need regarding available treatment options in outpatients with MDR/ESBL+ E. coli uropathogens.
Data on treatment patterns for uUTIs in the European Union are scarce; however, one study has analyzed uUTI treatment patterns in Germany using real-world data [9]. Our study used insurance claims data to evaluate adherence to antibiotic prescribing for female patients with uUTIs in Germany per German uUTI guidelines [10, 11]. We also assessed various patient and treatment factors for sub-populations, including the adherence of index treatment to German guidelines and optimal versus sub-optimal outcome (based on if patients were prescribed different antibiotics or had a UTI-related episode).
Methods
Study Design
This retrospective cohort study used anonymized German statutory health insurance claims data from the Wissenschaftliches Institut für Gesundheitsökonomie und Gesundheitssystem-forschung (WIG2, Scientific Institute for Health Economics and Health System Research, Leipzig, Germany) benchmark database from January 1, 2012 to December 31, 2019. Patient cases were followed longitudinally, and required a baseline period of 12 months prior to the index date to identify patients with recurrent uUTI and other baseline characteristics, plus a follow-up period of 12 months after the index date.
Exact prescription dates were available for each patient. However, uUTI diagnoses were recorded quarterly. Therefore, the index date for each uUTI episode was defined as the date of the first antibiotic prescription linked to a uUTI diagnosis. To ensure that the prescription was for the uUTI and not for a different infection, uUTI diagnosis and antibiotic prescription were required to be linked via physician and office ID, and patients with other infections in the index and preceding quarter were excluded. The index episode covered the 28 days following the index date, and could be prolonged for another 28 days in the event of switching antibiotics (including to intravenous antibiotics), a UTI-related emergency department (ED) visit or hospitalization, or disease progression (ED or inpatient diagnosis of acute pyelonephritis, bacteremia, or sepsis).
The study complied with all applicable laws regarding subject privacy. Study results are presented as aggregate analyses that do not allow for subject identification, thus informed consent and ethics committee and Institutional Review Board approvals were not required. This study was conducted in accordance with the protocols and consensus ethical principles derived from international guidelines including the Declaration of Helsinki and Council for International Organizations of Medical Sciences International Ethical Guidelines, International Council on Harmonization Good Clinical Practice Guidelines, and applicable laws and regulations. Permission was granted to access the databases utilised in this study.
Study Population
Female patients aged ≥ 12 years with an index UTI diagnosis in the ED or outpatient setting were included if they had ≥ 12 months of continuous health insurance data before and after the index date and had received one or more oral antibiotic prescription.
UTI diagnosis was judged via German Modification of the International Classification of Diagnoses 10th edition (ICD-10-GM) codes for acute cystitis (N30.0), unspecified cystitis (N30.9), and unspecified UTI (N39.0). The dataset captured whether or not a urine culture was performed; however, as the laboratory results were not relevant for reimbursement, test results were not included in the statutory health insurance German claims dataset and, therefore, could not be used to confirm uUTI diagnosis in this analysis.
To exclude complicated UTIs (cUTIs), cases with anatomical or functional abnormality of the urinary tract, urological procedures, or complicating comorbidities (cancer, human immunodeficiency viruses/acquired immunodeficiency syndrome, immunosuppression, multiple sclerosis, organ transplant, and uncontrolled diabetes) within the index quarter or two preceding quarters were excluded. Other exclusions for cUTI were as follows: prescription of intravenous antibiotics within 5 days of a prescription of oral antibiotics for uUTI; inpatient visit within the 3 months before and 2 days after the index date; prescription of immunosuppressive medications or receipt of chemotherapy within the 6 months before and 1 month after the index date; or pregnancy within the index quarter or two preceding quarters.
Study Outcomes and Data Analysis
We analyzed patients’ baseline demographic and clinical characteristics; whether the initial uUTI treatment received was aligned with first-choice therapy, not recommended as first-choice but still recommended, or not recommended per 2017 German Clinical guidelines of uUTI [11]; and the specialty of the treating physician consulted. Analyses were conducted in the overall incident uUTI population and in four sub-cohorts: cases that received recommended or non-recommended treatment, and cases that experienced an optimal or sub-optimal outcome. The definitions of recommended versus non-recommended treatment and optimal versus sub-optimal outcome are summarized in Table 1.
We estimated the prevalence of UTIs and uUTIs in Germany, and the incidence of uUTIs treated with antibiotics among female patients by age group (≥ 12 to < 18 years vs. ≥ 18 to ≤ 65 years) and region (North, East, South, or West). Prevalence in the study population was estimated based on diagnosis codes and standardized by age and gender to the entire population covered by the German statutory health insurance using KM6-statistics [12]. Incidence was calculated as the number of episodes per-patient per-year (PPPY).
Additional analyses were performed to assess risk factors for disease progression, plus healthcare resource utilization and associated costs in this patient group. These have been included in the Supplementary Materials.
Statistical Analyses
Standardized differences (STDs) were calculated to identify any meaningful differences in key baseline characteristics, treatment received (first-choice, not recommended as first-choice but still recommended, not recommended), and physician specialty between recommended/non-recommended treatment sub-cohorts and between optimal/sub-optimal outcome sub-cohorts. STDs > 10% were considered clinically meaningful.
Results
Study Population
A total of 144,645 uUTI cases in 124,971 patients were analyzed. uUTI cases were highest among 16- to 29-year-olds (27.7%), followed by 50- to 64-year-olds (21.1%; Table 2). Almost half of the cases occurred in women located in the West region of Germany (44.6%). Most women had a comorbidity index score of 0 (71.6%; Table 2).
Prevalence and Incidence of uUTI
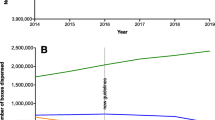
The year-wise overall prevalence of UTI per 100,000 women ranged from 10,982 (95% CI 10,929–11,036) in 2019 to 11,692 (95% CI 10,929–11,036) in 2014. The prevalence of UTI per age and region is shown in Fig. 1. The estimated overall prevalence of uUTI per 100,000 women ranged from 2995 (95% CI 2966–3024) in 2019 to 3204 (95% CI 3175–3233) in 2014. After excluding potential cUTI cases to generate a population of patients with uUTI, the prevalence of uUTI is reduced to around 30% of the values for UTI prevalence.
The incidence of uUTI treated with antibiotics generally decreased over time, starting at 0.0652 (95% CI 0.0645–0.0659) episodes PPPY in 2013 and falling to 0.0558 (95% CI 0.0551–0.0564) PPPY in 2019. Regional incidence rates were higher in the North (0.069 PPPY in 2013 to 0.058 PPPY in 2019) and West (0.071 PPPY in 2013 to 0.06 in 2019) of Germany than the South (0.064 PPPY in 2013 to 0.056 PPPY in 2019) and East (0.058 PPPY in 2013 to 0.047 PPPY in 2019).
Antibiotic Prescribing Patterns
According to recommendations issued in the German uUTI guidelines [10], 51,230 cases (35.4%) were assigned to the recommended treatment cohort and 93,415 cases (64.6%) were assigned to the non-recommended treatment cohort (Table 3). There was a higher proportion of younger patients (16–29 years) in the recommended treatment cohort versus non-recommended treatment cohort (32.2% vs. 25.3%) and, correspondingly, a higher proportion of older patients (≥ 65 years) in the non-recommended treatment cohort versus recommended treatment cohort (18.3% vs. 13.1%). Differences between the recommended and non-recommended treatment cohorts that were considered clinically meaningful were age (STD 20.8) and Comorbidity Index Score (STD 10.6). Most patients were from western Germany (44.6%); proportions of patients treated as recommended (42.9%) and non-recommended (45.5%) were consistent across all regions.
Most cases (n = 122,823; 84.9%) experienced an optimal outcome versus a sub-optimal outcome (n = 21,822; 15.1%; Table 3). Within the recommended treatment group, 42,437 cases (82.8%) experienced an optimal outcome and 8793 (17.2%) experienced a sub-optimal outcome; in the non-recommended treatment group, these numbers were 80,386 (86.1%) and 13,029 (13.9%), respectively. A higher proportion of therapies recommended but not as first-choice versus first-choice therapies were prescribed as initial therapy among cases with an optimal outcome (58.6% vs. 35.3%, respectively) compared with the sub-optimal outcome cohort (49.1% vs. 41.1%; Table 3).
Physician Specialty
Most uUTI cases were diagnosed and treated by general practitioners (GPs; 82.3%), followed by gynecologists (13.3%), and urologists (6.8%) (Table 3). Notably, 32.1% of prescriptions filled by GPs for the initial uUTI episode were first-choice antibiotics, versus 64.5% of those filled by gynecologists; 61.3% of prescriptions filled by GPs for initial therapies were recommended but not as first-choice antibiotics versus 29.7% of those filled by gynecologists. The remaining prescriptions were filled by internists, urologists, and physicians with unknown or other specialties.
Index uUTI Treatment
First-choice antibiotics were prescribed as initial therapy in 36.2% of all index episodes and recommended but not as first-choice antibiotics were prescribed as initial therapy in 57.1% (Table 3). The most commonly prescribed initial therapy was fosfomycin (30.4%), a recommended first-choice antibiotic. Ciprofloxacin (recommended but not as first-choice) and sulfamethoxazole/trimethoprim (recommended but not as first-choice antibiotic) were the next most common initial therapies (27.0% and 19.9%, respectively) (Table 4). All other antibiotics were prescribed as initial treatment in < 4% of index episodes. The most frequently prescribed antibiotics in the recommended treatment cohort were fosfomycin (85.1%), trimethoprim (6.6%), and nitrofurantoin (6.6%). Within the non-recommended treatment cohort, the most frequently prescribed antibiotics were ciprofloxacin (41.9%), sulfamethoxazole/trimethoprim (30.9%), and norfloxacin (5.8%). The most frequently prescribed antibiotic in the optimal outcome group was fosfomycin (29.8%), followed by ciprofloxacin (28.1%), and sulfamethoxazole/trimethoprim (20.1%). In the sub-optimal outcome group, the most frequently prescribed antibiotic was fosfomycin (33.7%); ciprofloxacin and sulfamethoxazole/trimethoprim were less frequently prescribed (21.3% and 18.9%, respectively).
Discussion
This study describes uUTI treatment in a large female population in Germany. Most patients received antibiotic treatment that was non-concordant with German treatment guidelines. Compared with the non-recommended treatment sub-cohort, patients who received recommended treatment tended to be younger and have less impact of comorbidities. Adherence to treatment guidelines varied by physician specialty. GPs were markedly more likely to prescribe a treatment that was non-concordant with the guidelines compared with specialist physicians.
Most patients (85%) had optimal outcomes, defined by the absence of additional antibiotic prescriptions and no indication of a worsening of uUTI. Interestingly, we observed among patients who had optimal outcomes, a higher proportion received antibiotics recommended but not as first-choice (59%) for the initial uUTI episode compared with first-choice therapies (35%); this pattern was observed to a lesser extent in the sub-optimal outcome cohort (49% received recommended but not as first-choice therapies, 41% received first-choice therapies). This unexpected result may speak to the challenges of empirical prescribing in the context of rising antimicrobial resistance in the community.
Antibiotic Prescribing Patterns
Overall, the most frequently prescribed antibiotic for initial uUTI treatment was fosfomycin (30.4%), which is recommended for first-choice therapy per German clinical practice guidelines, followed by ciprofloxacin (27.0%) and sulfamethoxazole/trimethoprim (19.9%). Sulfamethoxazole/trimethoprim and ciprofloxacin treatment are not recommended for first-choice uUTI therapy in Germany but are still recommended [11]. However, despite the guidance provided, a recent survey highlighted fosfomycin and sulfamethoxazole/trimethoprim as the preferred first-choice treatment choices among German physicians, chosen by 61% and 50% of 100 respondents, respectively [13]. Ciprofloxacin was the most commonly selected option following treatment failure (45%) [13]. In the current study, ciprofloxacin was the second most frequently prescribed antibiotic for first-choice treatment, with fluoroquinolone-class therapies accounting for 37% of all antibiotic prescriptions. An analysis of German health insurance data from 2015 to 2019 demonstrated movement towards more guideline-adherent prescribing practices, but with room for improvement regarding the use of antibiotics not recommended as first-choice therapies [14]. The discussion on the relevance of the recommended first-line drugs when second-line antibiotics are more effective is the dilemma for any guideline committee; ciprofloxacin (or other fluoroquinolones) are known to be effective for UTI [15], but they are also most prone to resistance [14]. However, if the diagnosis of UTI is not often validated and therefore treatment not administered for an actual infection, it may be preferable to use a less resistance-prone antibiotic for empiric first-line treatment. The resistance levels in Germany in E. coli for fluoroquinolones and sulfamethoxazole/trimethoprim points in the direction, that they should not be recommended as first-line empiric treatment [15].
Physician Specialty
Most uUTI cases were diagnosed by GPs (fewer cases were diagnosed by gynecologists and urologists), and 64.6% of cases were treated with non-recommended initial therapies. GPs prescribed first-choice antibiotics in just 32% of cases and were found to provide non-recommended treatment to 68% of cases overall. Conversely, gynecologists prescribed mostly first-choice antibiotics and complied with guidelines in 60% of cases. High rates of non-recommended antibiotic prescribing are not unexpected, and they are not limited to Germany. Retrospective database studies of female patients with uUTI in the US have shown similar trends of guideline non-compliant antibiotic prescribing [16, 17]. One such study demonstrated a 45% rate of fluoroquinolone prescribing as first-choice, which fell by just 3% after guidelines were released, indicating a minimal impact of clinical guidance on prescribing behaviors [16]. High rates of guideline non-compliant antibiotic prescribing may contribute to antimicrobial resistance and potentially sub-optimal patient care [15, 18,19,20].
The outcome of the index episode was optimal in approximately 85% of cases, with comparable rates of optimal outcomes between the recommended treatment and non-recommended treatment cohorts (83% vs. 86%, respectively). Considering the high number of recommended prescriptions from gynecologists, this finding may be a result of complicating factors treated by specialists rather than GPs.
Limitations
This study was not without its limitations. First, given that empiric therapy was recommended by the German guidelines, it is possible that in some cases cultures were performed before therapy and the results of the cultures would impact the choice of therapy. These cases would differ from those experienced by the overall uUTI population, and the decision to deviate from the guidelines was not documented. However, while prescriptions were not directly linked to a diagnosis, it could be linked to the diagnosing physician by matching the unique ID of a physician involved in outpatient care to the ID of the physician who prescribed the antibiotics. In addition, one study found that the use of urine culture and susceptibility testing for guiding initial therapy for uUTI differed depending on physician and was more commonly used for initial therapy in the US (33–78%) versus Germany (9–50%) [13]. It is therefore likely that not all diagnoses were based on cultures. Another study found that symptoms of UTI do not necessarily equate to a culture-based UTI diagnosis [21]. Furthermore, it may be that, among the 85% of people who responded to antibiotic treatment, some may have had a false-positive UTI diagnosis. Similarly, sub-optimal outcome was defined as a switch in medication or documented ED or inpatient visit. As clinical and laboratory data were not available, the correlation of culture results with a switch in therapy could not be confirmed and non-recommended therapy may have been overestimated. Treatment with antibiotics not recommended as first-choice therapy could not be differentiated due to lacking information on antibiotic allergy and intolerance; this information could justify the use of an antibiotic not recommended as first-choice therapy in cases with limited treatment options.
On the other hand, services and prescriptions are documented with an exact date, the latter with a date of prescription and dispensing; however, prescriptions are not directly linked to a diagnosis, but by matching the unique ID of a physician involved in a case of outpatient care to the ID of the physician who prescribed the antibiotic. This could have led to misclassification if other infections requiring antibiotic treatment were diagnosed by the same physician. To avoid this misclassification, cases with other acute infections were excluded. Requiring linkage of diagnosis and prescription enabled the date of uUTI diagnosis, and thus the index date, to be extracted. It was presumed that any prescription was paralleled by a diagnosis, and cases with prescriptions that lacked an associated diagnosis were ignored.
It is also important to consider the limitations inherent to observational retrospective studies using claims data. Claims data can only demonstrate association and not causality, and the data described in this study were collected for the purpose of payment, not research. In addition, there was no precise method of identifying patients with uUTI using statutory health insurance claims data. Therefore, the epidemiological parameters were approximated by selecting adolescent and adult female patients with UTI diagnoses compatible with uUTI and excluding patients with indications of cUTI. The presence of a diagnosis code on a medical claim was also not positive proof of disease, as the diagnosis code may be incorrectly coded or imprecise. Information on outcomes such as treatment failure were not available and claims for filled prescriptions did not indicate whether the medication was taken as prescribed. Dates for diagnoses are not available in German claims data, which prevented the evaluation of treatment and outcomes over time and led to the exclusion of more cases than necessary (due to an inability to exclude in a temporally precise manner). The records used will have underestimated the true number of outpatient visits and the number of cases with progression; these cases were likely excluded as unrelated infections. The exclusion of unrelated infections was necessary, however, as it minimized the potential for misclassification of other infections diagnosed by the same physician and facilitated extraction of the index date for each patient.
Conclusions
In this study of women diagnosed with uUTIs in Germany, a considerable proportion received treatment discordant with current German guidelines [10], with different treatment approaches from different medical specialists. Prescription of antibiotics recommended but not as first-choice therapies as initial treatment for uUTI was common, and guideline adherence differed between physician specialties, with gynecologists adhering to prescribing recommendations more than GPs. The study of patient and treatment factors, as well as adherence to antibiotic prescribing provides a novel and multi-dimensional picture of uUTI treatment in Germany.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to data protection aspects.
References
Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary tract infections. Ther Adv Urol. 2019;11:1756287219832172. https://doi.org/10.1177/1756287219832172.
Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5):e103–20. https://doi.org/10.1093/cid/ciq257.
Naber KG, Bonkat G, Wagenlehner FME. The EAU and AUA/CUA/SUFU guidelines on recurrent urinary tract infections: what is the difference? Eur Urol. 2020;78(5):645–6. https://doi.org/10.1016/j.eururo.2020.06.032.
Hummers-Pradier E, Ohse AM, Koch M, Heizmann WR, Kochen MM. Management of urinary tract infections in female general practice patients. Fam Pract. 2005;22(1):71–7. https://doi.org/10.1093/fampra/cmh720.
Bonkat G. European Association of Urology guidelines: Urological infections 2021. https://uroweb.org/guidelines/urological-infections/chapter/the-guideline. Accessed 24 May 2023.
Kikuchi JY, Banaag A, Koehlmoos TP. Antibiotic prescribing patterns and guideline concordance for uncomplicated urinary tract infections among adult women in the US military health system. JAMA Netw Open. 2022;5(8): e2225730. https://doi.org/10.1001/jamanetworkopen.2022.25730.
Grigoryan L, Nash S, Zoorob R, et al. Qualitative analysis of primary care provider prescribing decisions for urinary tract infections. Antibiotics (Basel). 2019;8(2):84. https://doi.org/10.3390/antibiotics8020084.
Ny S, Edquist P, Dumpis U, et al. Antimicrobial resistance of Escherichia coli isolates from outpatient urinary tract infections in women in six European countries including Russia. J Glob Antimicrob Resist. 2019;17:25–34. https://doi.org/10.1016/j.jgar.2018.11.004.
Naber KG, Wagenlehner F, Kresken M, et al. Escherichia coli resistance, treatment patterns and clinical outcomes among females with uUTI in Germany: a retrospective physician-based chart review study. Sci Rep. 2023;13(1):12077.
AWMF. Epidemiology, diagnosis, therapy, prevention and management of uncomplicated, bacterial, community-acquired urinary tract infections in adult patients. https://register.awmf.org/assets/guidelines/043-044l_S3_Harnwegsinfektionen_2017-05.pdf. Accessed 09 Oct 2023.
Kranz J, Schmidt S, Lebert C, et al. The 2017 update of the German clinical guideline on epidemiology, diagnostics, therapy, prevention, and management of uncomplicated urinary tract infections in adult patients: part 1. Urol Int. 2018;100(3):263–70.
BMG. Members and insured persons of the statutory health insurance (GKV). https://www.bundesgesundheitsministerium.de/themen/krankenversicherung/zahlen-und-fakten-zur-krankenversicherung/mitglieder-und-versicherte.html. Accessed 26 Sept 2023.
O’Brien M, Marijam A, Mitrani-Gold FS, Terry L, Taylor-Stokes G, Joshi AV. Unmet needs in uncomplicated urinary tract infection in the United States and Germany: a physician survey. BMC Infect Dis. 2023;23(1):281. https://doi.org/10.1186/s12879-023-08207-x.
Schmiemann G, Hoffmann F, Hamprecht A, Jobski K. Patterns and trends of antibacterial treatment in patients with urinary tract infections, 2015–2019: an analysis of health insurance data. BMC Prim Care. 2022;23(1):204. https://doi.org/10.1186/s12875-022-01816-6.
Gupta K. Emerging antibiotic resistance in urinary tract pathogens. Infect Dis Clin North Am. 2003;17(2):243–59. https://doi.org/10.1016/s0891-5520(03)00006-0.
Durkin MJ, Keller M, Butler AM, et al. An assessment of inappropriate antibiotic use and guideline adherence for uncomplicated urinary tract infections. Open Forum Infect Dis. 2018;5(9):ofy198. https://doi.org/10.1093/ofid/ofy198.
Moon RC, Marijam A, Mitrani-Gold FS, et al. Treatment patterns, healthcare resource use, and costs associated with uncomplicated urinary tract infection among female patients in the United States. PLoS ONE. 2022;17(11): e0277713. https://doi.org/10.1371/journal.pone.0277713.
Avorn J, Solomon DH. Cultural and economic factors that (mis)shape antibiotic use: the nonpharmacologic basis of therapeutics. Ann Intern Med. 2000;133(2):128–35. https://doi.org/10.7326/0003-4819-133-2-200007180-00012.
Cassini A, Plachouras D, Monnet DL. Attributable deaths caused by infections with antibiotic-resistant bacteria in France: Authors’ reply. Lancet Infect Dis. 2019;19(2):129–30. https://doi.org/10.1016/S1473-3099(19)30004-0.
Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096. https://doi.org/10.1136/bmj.c2096.
Bai AD, Bonares MJ, Thrall S, Bell CM, Morris AM. Presence of urinary symptoms in bacteremic urinary tract infection: a retrospective cohort study of Escherichia coli bacteremia. BMC Infect Dis. 2020;20(1):1–10. https://doi.org/10.1186/s12879-020-05499-1.
Medical Writing/Editorial Assistance
Medical writing support for the development of this manuscript, under the guidance of the authors, was provided by Hayley Sharpe, PhD, of Ashfield MedComms, an Inizio company, and funded by GSK.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
This study, including study design, data collection, analysis, and interpretation, medical writing and submission support for the manuscript, and the journal’s rapid service fee was funded by GSK (study 214846).
Author information
Authors and Affiliations
Contributions
Axel Krinner: conceptualization, formal analysis and investigation, methodology, project administration, writing – review & editing. Michael Schultze: conceptualization, methodology, project administration, writing – review & editing. Alen Marijam: conceptualization, formal analysis, methodology, writing – review & editing. Marc Pignot: conceptualization, formal analysis and investigation, methodology, project administration, writing – review & editing. Nils Kossack: conceptualization, formal analysis and investigation, methodology, project administration, writing – review & editing. Fanny S. Mitrani-Gold: conceptualization, formal analysis, methodology, writing – review & editing. Ashish V. Joshi: conceptualization, formal analysis, methodology, writing – review & editing.
Corresponding author
Ethics declarations
Conflict of Interest
Axel Krinner is an employee of WIG2 which received funding from GSK to conduct this study. Michael Schultze is an employee of ZEG Berlin which received funding from GSK to conduct this study. Alen Marijam is an employee of and shareholder in GSK. Marc Pignot is an employee of ZEG Berlin which received funding from GSK to conduct this study. Nils Kossack is an employee of WIG2 which received funding from GSK to conduct this study. Fanny S. Mitrani-Gold is an employee of and shareholder in GSK. Ashish V. Joshi is an employee of and shareholder in GSK.
Ethical Approval
The study complied with all applicable laws regarding subject privacy. Study results are presented as aggregate analyses that do not allow for subject identification, thus informed consent and ethics committee and Institutional Review Board approvals were not required. This study was conducted in accordance with the protocols and consensus ethical principles derived from international guidelines including the Declaration of Helsinki and Council for International Organizations of Medical Sciences International Ethical Guidelines, International Council on Harmonization Good Clinical Practice Guidelines, and applicable laws and regulations. Permission was granted to access the databases utilised in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentation: Some of the material discussed in this manuscript was presented at European Congress of Clinical Microbiology & Infectious Diseases (ECCMID 2023, Copenhagen, Denmark) meeting; Schultze et al. (2023) “Patterns and adherence to treatment guidelines by physician specialty in uncomplicated urinary tract infection treatment among female patients in Germany: a retrospective real world study” and “Recurrence, healthcare resource use, and costs in the treatment of uncomplicated urinary tract infection in female patients in Germany”.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-Non Commercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Krinner, A., Schultze, M., Marijam, A. et al. Treatment Patterns and Adherence to Guidelines for Uncomplicated Urinary Tract Infection in Germany: A Retrospective Cohort Study. Infect Dis Ther 13, 1487–1500 (2024). https://doi.org/10.1007/s40121-024-00973-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-024-00973-8