Abstract
Introduction
Herpes zoster (HZ) can cause substantial patient morbidity and lead to large healthcare costs. However, the disease burden of HZ in Southeast Asia may be underestimated. This study aimed to estimate the public health burden of HZ and the impact of vaccinating adults aged ≥ 50 years old in five Southeast Asian countries (Indonesia, Malaysia, Philippines, Thailand, and Vietnam), with adjuvanted recombinant zoster vaccine (RZV) compared with no vaccination.
Methods
For each country, we adapted a static multicohort Markov model developed with a 1-year cycle length and lifetime horizon. Demographics were obtained from the World Health Organization, HZ incidence from a worldwide meta-regression reporting Asian-specific values, proportions of postherpetic neuralgia (PHN) and non-PHN complications from local/regional studies, and vaccine efficacy from a long-term follow-up trial. First-dose coverage and second-dose compliance were assumed to be 30% and 70%, respectively. A one-way deterministic sensitivity analysis (OWSA) and probabilistic sensitivity analysis (PSA) were performed to assess the robustness and uncertainty of inputs for each country.
Results
Without RZV, it was estimated that there would be a total of approximately 10 million HZ cases, 2.1 million PHN cases, and 1.4 million non-PHN complications in individuals aged ≥ 50 years included in the model. Introducing RZV under 30% coverage could avoid approximately 2.2 million (22%) HZ cases, almost 500,000 (21%) PHN cases, and around 300,000 (22%) non-PHN complications. OWSA showed that first-dose coverage and initial HZ incidence had the largest impact on the estimated number of HZ cases avoided. The number needed to vaccinate ranged from 15 to 21 to prevent one case of HZ and from 68 to 104 to prevent one case of PHN across each country.
Conclusions
This study demonstrated that there is substantial HZ disease burden in older adults for the five selected countries in Southeast Asia, negatively impacting national healthcare systems. Introducing RZV could potentially reduce this burden.
A graphical abstract is available with this article.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Herpes zoster (HZ) and its complications can cause substantial patient morbidity and lead to large healthcare costs; however, little is known about the disease burden of HZ in Southeast Asia. |
This study aimed to estimate the public health burden of HZ and the impact of vaccinating adults aged ≥ 50 years old in five Southeast Asian countries (Indonesia, Malaysia, Philippines, Thailand, and Vietnam), with adjuvanted recombinant zoster vaccine (RZV) compared with no vaccination. |
What was learned from the study? |
This study estimated that there is substantial HZ disease burden in older adults for the five selected countries in Southeast Asia. |
Introducing RZV under just 30% coverage could avoid approximately 2.2 million HZ cases, almost 500,000 postherpetic neuralgia cases, and around 300,000 non-postherpetic neuralgia complications. |
These results could help policymakers assess the potential value of introducing RZV for people aged ≥ 50 years in Southeast Asia, as well as inform future health economic research into the medical costs and healthcare resource utilization surrounding HZ. |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.25225775.
Introduction
Herpes zoster (HZ), commonly known as shingles, is caused by reactivation of the varicella-zoster virus (VZV) [1, 2]. It is characterized by a painful, unilateral, blistering rash [3]. HZ can have serious complications including postherpetic neuralgia (PHN), ophthalmic involvement, and neurological complications [2, 4]. The debilitating pain from PHN can last from several months to years [5].
The lifetime risk of HZ is estimated to be 30% in the general global population, increasing at 50 years old [6]. In the Asia–Pacific region, the estimated overall incidence rate of HZ is 3–10 per 1000 person-years, similar to worldwide incidence rates [7, 8]. Data related to the economic burden of HZ and its complications in Southeast Asia are sparse. In Thailand, the direct healthcare costs of HZ per patient were estimated to represent 1.1% of annual income per capita [9, 10]. Additionally, patients with HZ typically require increased assistance from caregivers. For example, a prospective cohort study conducted in Thailand found that caregivers of patients with HZ missed a median of 5 days of work in 6 months [9]. This highlights the societal burden of HZ, which, together with the resources required for HZ disease management, poses a substantial economic burden to healthcare systems [7, 11, 12].
In Asia, the number of people aged over 60 years is projected to reach one billion by 2035 [8]. Consequently, the frequency and burden of HZ is predicted to increase as waning T cell immunity, due to increasing age or immunosuppression, is a major risk factor for developing HZ [3, 13, 14]. This, together with historically limited implementation of adult immunization policies for HZ in the Asia–Pacific region [8], is likely to cause a large public health burden and lead to considerable economic costs in the near future [15].
There are different types of HZ vaccine—live attenuated or recombinant—both of which have demonstrated safety and efficacy in clinical trials [1, 8]. Live attenuated vaccines are generally not recommended for patients who are immunocompromised due to the risk of unchecked infection [7, 16]. As recombinant vaccines, such as recombinant zoster vaccine (RZV), are nonreplicating, they can be used for patients who are immunocompromised [1]. Despite effective vaccines being available and licensed to prevent HZ, few countries have implemented these vaccines into their national immunization programs [17]. In Southeast Asian countries, either live attenuated and/or recombinant HZ vaccines are currently available, with HZ vaccination being generally recommended to individuals ≥ 50 years old (Supplementary Table 1) [7]. However, these vaccines are currently only available privately and have not been implemented into national immunization programs.
The objectives of this study were firstly to estimate the public health burden of HZ and HZ-related complications; and secondly to evaluate the public health impact of RZV implementation among adults aged ≥ 50 years old in five Southeast Asian countries (Indonesia, Malaysia, Philippines, Thailand, and Vietnam).
Methods
Study Population
The population considered in this analysis was adults aged ≥ 50 years old in five countries in Southeast Asia: Indonesia, Malaysia, Philippines, Thailand, and Vietnam. These five countries are among the most populated in the region, and generally share similar socioeconomic and sociodemographic ranges [7].
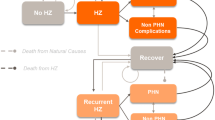
Model Design
A static multicohort Markov model, developed in Microsoft Excel [15, 18,19,20,21,22], was adapted to assess the public health burden of HZ and public health impact of RZV vaccination in the general population aged ≥ 50 years old in Southeast Asia. The model followed individuals from the year of vaccination and over their estimated remaining lifetime, with a cycle length set at 1 year. Two strategies were compared in each country: (1) no RZV and (2) vaccination with RZV.
HZ cases, PHN cases, and other non-PHN complications (classified as ocular, neurological, cutaneous, or other non-pain-related complications) were generated from the model scenario of no RZV to reflect the public health burden of HZ on a population level. HZ cases avoided, PHN cases avoided, and other non-PHN complications avoided by RZV were generated from the model scenario of vaccinating with RZV to reflect the absolute public health impact of RZV and were divided by the total cases to show the relative public health impact of introducing RZV.
Further details on the model design are provided in previous publications [15, 18,19,20,21,22].
Model Inputs
Demographics
The base population included adults aged ≥ 50 years old, stratified according to five age cohorts (50–59 years, 60–64 years, 65–69 years, 70–79 years, and 80+ years) residing in Indonesia, Malaysia, Philippines, Thailand, and Vietnam (Table 1). National population sizes for each country were taken from population pyramids reported in 2022 [23], and the annual probability of all-cause mortality was obtained from the World Health Organization (Supplementary Table 2) [24].
Epidemiology
Epidemiology inputs included HZ annual incidence, proportion of patients with PHN or other complications (classed as ocular, neurological, cutaneous, or other non-pain-related complications), recurrence rate of HZ and PHN, and case fatality rates of HZ.
Asian regional age-specific HZ incidence data were taken from a worldwide meta-regression study, which reported that geographic location, gender, and year of analysis had no statistically significant impact on HZ incidence [13]. Recurrence rates of HZ episodes were assumed to be the same as the first occurrence [25].
The proportions of HZ cases with PHN or non-PHN-related complications were selected from a pooled analysis of PHN risk among patients with HZ in North and South America and Asia (Canada, Brazil, Mexico, Argentina, Taiwan, South Korea, and Thailand) [26] and a literature review of HZ burden in the Asia–Pacific region (Australia, China, Hong Kong, India, Indonesia, Japan, Korea, Malaysia, New Zealand, Philippines, Singapore, Taiwan, Thailand, and Vietnam) [8], respectively (Table 1). Recurrent HZ cases were assumed to be associated with the same risk of developing PHN.
Case fatality rates were conservatively set at 0% as no credible sources were available and the impact of HZ on life expectancy was minor.
Vaccine Efficacy, Waning Rates, and Coverage
The assumed first-dose coverage for RSV was set at 30% [27], with a second-dose compliance rate of 70% [28]. A 2-month time window between two doses of RZV was assumed.
RZV vaccine efficacy rates against HZ and PHN were calculated on the basis of granular data taken from the ZOE-50 and ZOE-70 clinical studies, and the long-term follow-up (LTFU) study ZOE-LTFU (Table 1) [20, 29,30,31,32]. Vaccine efficacy for individuals receiving one dose of RZV was assumed to be 90.1% for individuals aged 50–69 and 69.5% for individuals aged ≥ 70 years, while efficacy in individuals receiving both doses was assumed to be 98.9% and 95.4%, respectively [20, 29,30,31,32]. Waning rates for individuals receiving both doses of RZV were age- and time-dependent: efficacy waned at 1.5% annually for individuals aged 50–69 years old, while efficacy waned at 2.3% for individuals aged ≥ 70 years old [29, 31].
For individuals receiving only one dose of RZV, waning rates were assumed to be the same as that of the live attenuated zoster vaccine (5.4% in the first 4 years post-vaccination and 5.1% in subsequent years) based on short-term and long-term persistence studies [33, 34]. This assumption was also used in a German public health impact study, where it was validated by an advisory board [20].
However, some adjustments for vaccine efficacy were made in the first 2 years post-vaccination. In the first year (first cycle of the model), an average vaccine efficacy of 2 months for individuals receiving a single dose of RZV, and 10 months for individuals receiving both doses were applied, as the time window between the two doses was assumed to be 2 months. In the second year, a half-cycle correction was applied to capture the full decline of efficacy from the completion of both doses until the end of the second year. In the subsequent years, age-dependent waning rates were used as described above.
Model Outputs
The numbers of events (HZ cases, PHN cases, and non-PHN complications) over the remaining lifetime of adults in each age cohort and overall adults aged ≥ 50 years old were reported for each country and summed to generate an overall estimate. The absolute numbers of events avoided with RZV vaccination were reported for the same cohort for their remaining lifetime and were divided by total number of events to generate relative cases avoided.
The number of individuals needed to vaccinate (NNV) to avoid one case of PHN was calculated using the following equation:
Sensitivity Analyses
A one-way deterministic sensitivity analysis (OWSA) was performed to assess the robustness and uncertainty of base case inputs for each country setting included in the study (Supplementary Table 3). Each model input was adjusted ± 20% or 95% confidence interval from the base case value to evaluate the relative impact on the number of HZ cases avoided from vaccination. A probabilistic sensitivity analysis (PSA) was also carried out to determine the impact of full uncertainty in the model inputs and the impact on the result estimates. A total of 1000 Monte Carlo simulations were performed, sampling input values from available probability distributions. A correlation coefficient of 0.5 was assumed for all age-specific incidence parameters.
Scenario Analyses
Scenario analyses were performed by altering model assumptions to explore the impact of vaccine coverage rates, second-dose compliance, and changing demographics or population size receiving the vaccine. One scenario applied demographics data from local statistics offices in Malaysia (applying projected population sizes in 2022 and natural mortality rates in 2018 from the Department of Statistics Malaysia) [35], Philippines (applying projected population sizes in 2022 and natural mortality rates in 2016 from the Philippine Statistics Authority) [36], and Thailand (applying projected population sizes in 2022 and natural mortality rates in 2012 from the National Statistic Office of Thailand) [37]. A second scenario analysis compared the best case scenario of first-dose coverage (80%) and second-dose compliance rates (95%) with worst case scenario of first-dose coverage (20%) and second-dose compliance (45%).
Ethics
The model was based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Base Case Results
HZ Cases, PHN Cases, and Non-PHN Complications
For all individuals aged ≥ 50 years included in the base case analysis of the model, without RZV, there would be total of approximately 10 million HZ cases (Indonesia 4,031,347; Malaysia 524,122; Philippines 1,333,625; Thailand 2,496,571; Vietnam 1,817,876), 2 million PHN cases (Indonesia 805,893; Malaysia 109,102; Philippines 271,636; Thailand 565,526; Vietnam 379,158), and 1 million non-PHN complications (Indonesia 546,840; Malaysia 71,096; Philippines 180,902; Thailand 338,653; Vietnam 246,590) (Fig. 1).
Introducing RZV under 30% coverage could avoid approximately 2 million (22%) HZ cases (Indonesia 904,399; Malaysia 115,274; Philippines 297,990; Thailand 513,903; Vietnam 398,679), almost 500,000 (21%) PHN cases (Indonesia 175,943; Malaysia 23,312; Philippines 59,018; Thailand 111,976; Vietnam 80,646), and around 300,000 (22%) non-PHN complications (Indonesia 122,679; Malaysia 15,637; Philippines 40,421; Thailand 69,709; Vietnam 54,080). The highest numbers of HZ cases, PHN cases, and non-PHN complications in the no vaccination scenario were located in Indonesia, mainly because of the large population sizes, followed by Thailand and Vietnam (Table 2). Consistent with this, RZV could prevent the highest number of HZ cases, PHN cases, and non-PHN complications in Indonesia, followed by Thailand and Vietnam (Fig. 1). The majority HZ, PHN, and non-PHN complication cases, and the majority of cases avoided, occurred in the cohorts aged 50–59, followed by 60–64 years old (see more details in Supplementary Table 4).
When non-PHN HZ-related complications were further stratified into neurological, cutaneous, and other non-pain-related complications, the greatest numbers of avoided complications were cutaneous (151,374 cases), followed by ocular (111,008 cases).
Numbers Needed to Vaccinate
NNV ranged from 15 to 21 to prevent one case of HZ and from 68 to 104 to prevent one case of PHN across each country included in the analysis, with the lowest NNV for HZ and PHN reported in Thailand, followed by Vietnam and Malaysia (Figs. 2 and 3). When stratified by age, the 50–59 years age cohort had the lowest NNV to prevent HZ and 60–64 years age cohort had the lowest NNV to prevent one case of PHN.
Sensitivity Analyses
In the OWSA, the inputs with the largest impact on the number of HZ cases avoided included first-dose coverage, initial HZ incidence, and waning of vaccine efficacy (Fig. 4).
In the PSA with 1000 iterations, 90% of simulations showed reductions of ≥ 1,200,000, ≥ 140,000, ≥ 360,000, ≥ 600,000, and ≥ 490,000 cases when compared with no vaccination in Indonesia, Malaysia, Philippines, Thailand, and Vietnam, respectively (Fig. 5).
Scenario Analyses
Results from the scenario analyses are presented in Fig. 6.
The first scenario indicated that the most up-to-date demographic inputs from local statistics offices projected higher HZ public health burden and higher RZV public health impact than the base case. Increases of avoided HZ cases were observed in the countries with available data (80% in Malaysia, 116% in Philippines, and 50% in Thailand).
The second scenario indicated that improving first-dose coverage from 30% to 80% and second-dose compliance from 70% to 95% would result in more than two times higher numbers of HZ cases avoided (200% in Indonesia, 202% in Malaysia, 200% in Philippines, 207% in Thailand, and 202% in Vietnam). When the first-dose coverage was reduced from 30% to 20% and the second-dose compliance from 70% to 45%, HZ vaccination could prevent 58.39% of HZ cases in Indonesia, 57.94% of HZ cases in Malaysia, 58.34% of HZ cases in Philippines, 56.62% of HZ cases in Thailand, and 57.89% of HZ cases in Vietnam.
Discussion
Modelling the remaining lifetime risk of HZ and its complications with a multicohort approach allows for disease projections to be made on outcomes that are limited or difficult to obtain in real-world evidence. To the best of the authors’ knowledge, this is the first study to assess the potential burden of HZ and the public health impact of RZV in Southeast Asia.
Overall, this study estimated that HZ is likely to be a substantial public health burden in the remaining lifetime of adults aged ≥ 50 years in Indonesia, Malaysia, Philippines, Thailand, and Vietnam. The introduction of RZV among these populations, with just 30% first-dose coverage, could avoid approximately 22% of cases of HZ, PHN, and non-PHN complications in the region. The public health benefit of RZV would also increase in line with increasing coverage rates over time.
It was also predicted that over the course of their remaining lifetimes, the youngest cohort (50–59 years old) would have the greatest lifetime burden of HZ without vaccination and would avoid the greatest number of HZ cases with vaccination. This may be due to the youngest cohort having the largest sample size, but also a result of the relatively longer life expectancy. This is supported by a study conducted in South America (Argentina, Brazil, Mexico, Chile, and Colombia) that also concluded that the optimal age for vaccination would be 50 or 60 years [38]. Additionally, a recent modelling study conducted in Beijing, China found that vaccination of a 50–59-year-old cohort led to the greatest number of avoided cases and could have a greater effect on case avoidance of HZ, PHN, and other complications versus vaccinating older cohorts [15].
The robustness of the base case analysis was proved when comparing with the PSA and scenario analysis. In the PSA, 90% of simulations showed reductions of ≥ 140,000, ≥ 360,000, ≥ 490,000, ≥ 600,000, and ≥ 1,200,000 HZ cases when compared with no vaccination in Malaysia, Philippines, Vietnam, Thailand, and Indonesia, respectively. The alternative demographic inputs in the scenario analysis also projected a significantly higher HZ disease burden and higher RZV benefit. However, to increase the comparability between countries, conservative estimates from standardized sources were applied in the base case analysis.
The coverage and compliance rates of RZV applied in the base case analysis of this study were among the most conservative in published public health impact of RZV modelling studies [19, 21]. The second scenario analysis assessing best and worst case scenarios of HZ coverage and compliance showed that improving first-dose coverage and second-dose compliance would result in higher numbers of HZ cases avoided. In addition to this, the current analysis conservatively assumed that recurrence rates of HZ episodes were the same as the first occurrence. However, a study conducted by Yawn et al. highlighted that recurrence rates were much higher than initial incidence rates [25]. Therefore, the number of HZ and PHN cases prevented by RZV could be higher.
Despite the robust base case data produced in this analysis, there are several limitations, many of which are related to the large number of assumptions applied to the model. Firstly, country- and age-specific data were not always available for inputting into the model. For example, regional data from Asia were taken from a worldwide meta-regression study for HZ incidence because of a lack of robust local data [13]. However, as a result of the similarities in the burden of HZ between the countries in Asia [13], this meta-regression was the most up to date and robust source and the relative percentages should be pertinent to other countries in Southeast Asia. A recently published systematic literature review found that there is no significant difference in HZ incidence between countries worldwide and therefore the regional data can be generalized to the countries in this study [3]. The lack of robust local data regarding HZ epidemiology and the costs and healthcare resource utilization of HZ in Southeast Asia demonstrates that there are gaps in the research that need to be further investigated to truly reflect the burden of HZ in this region. Also, while vaccine efficacy and waning rates were based on randomized controlled trials, the values beyond 8 years are unknown [20, 29,30,31,32]. However, the model extrapolated a linear decline in efficacy, and set an age limit of 100 years for the cohorts, which prevented overestimation of vaccine benefit and disease burden over the modelling time horizon.
Among the general population, there may be some individuals with comorbidities, including diabetes and coronary heart disease, and some who are immunocompromised, which are significant risk factors for HZ infection [13, 14]. This was not considered in the model for simplicity, since immunosuppressive conditions may not persist for the entirety of a patient’s remaining lifetime, and the risk of developing HZ may be affected if a patient’s condition improves with treatment. A different model structure would therefore be required to account for the duration of immunosuppression and the change in HZ risk over the remaining lifetime of patients with immunosuppressive conditions, in order to accurately estimate the public health impact of RZV in immunocompromised adults in Southeast Asia.
Lastly, this analysis employed a static multicohort Markov model, which allowed for the consideration of the long-term benefits of RZV. However, as the potential effect of RZV on the severity of HZ and PHN and the economic savings by preventing diseases and social psychological value were not accounted for [39], the overall value of RZV may have been underestimated.
Overall, this study provides strong evidence of the burden of HZ in Southeast Asia, as well as the benefit RZV could bring to alleviate the occurrence of HZ and its related complications in the region. It is likely that the HZ public health burden is underestimated in the region because of passive surveillance techniques and a lack of national surveillance, as well as the fact that HZ is not a mandatory notifiable disease [7, 40]. A study conducted to assess public awareness of HZ found that there is globally poor knowledge of HZ, with 53% of responders who had never experienced HZ in the Asia–Pacific region (n = 1470) having “little knowledge” of the disease [40]. Disease awareness is important in order to improve prevention of HZ. This study highlighted that as HZ causes significant morbidity rather than high mortality, the burden is likely to increase with ageing populations; thus preventative strategies such as vaccination will be key to reduce the burden of HZ [40].
Vaccination can provide direct protection against HZ, as well as providing substantial savings to healthcare systems by preventing illness and long-term complications [41]. In addition, implementation of HZ vaccination into national immunization programs would allow all socioeconomic groups to have access to vaccination, aiding the reduction of health inequity [42]. The broad value that vaccination brings on the individual, societal, and national level is well recognized in the literature [43, 44]. However, some studies suggest that adult vaccination is severely undervalued by the public [45]. This study highlighted the health benefit that vaccination could bring to older adults in Southeast Asia, even with just 30% first-dose coverage.
Conclusion
This study revealed that there could be approximately 10.2 million cases of HZ during the remaining lifetimes of those aged ≥ 50 years Indonesia, Malaysia, Philippines, Thailand, and Vietnam, with many cases resulting in serious, painful complications including PHN (2.1 million cases). Introducing RSV vaccination for older adults with just 30% first-dose coverage could substantially reduce disease burden in all countries assessed, with 2.2 million HZ cases and approximately 500,000 PHN cases being avoided. Furthermore, as a conservative estimate was used for vaccine coverage and compliance rates, the true number of HZ and PHN cases avoided by introducing RZV could be even higher. These results could help policymakers assess the potential value of introducing RZV for people aged ≥ 50 years in Southeast Asia, as well as inform future health economic research into the medical costs and healthcare resource utilization surrounding HZ, and the impact RZV may bring to the region. These results will also aid in the development of well-designed and accurately communicated vaccination campaigns, improving understanding and positive awareness of RZV, which may improve vaccine uptake.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
References
Patil A, Goldust M, Wollina U. Herpes zoster: a review of clinical manifestations and management. Viruses. 2022;14(2):192.
Hope-Simpson RE. The nature of herpes zoster: a long-term study and a new hypothesis. Proc R Soc Med. 1965;58(1):9–20.
van Oorschot D, Vroling H, Bunge E, et al. A systematic literature review of herpes zoster incidence worldwide. Hum Vaccin Immunother. 2021;17(6):1714–32.
Harbecke R, Cohen JI, Oxman MN. Herpes zoster vaccines. J Infect Dis. 2021;224(12 Suppl 2):S429–42.
Johnson RW, Bouhassira D, Kassianos G, et al. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med. 2010;8(1):37.
Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4(6):e004833.
San Martin P, Aunhachoke K, Batac MCF, et al. Systematic literature review of herpes zoster disease burden in Southeast Asia. Infect Dis Ther. 2023;12(6):1553–78.
Chen LK, Arai H, Chen LY, et al. Looking back to move forward: a twenty-year audit of herpes zoster in Asia-Pacific. BMC Infect Dis. 2017;17(1):213.
Aunhachoke K, Bussaratid V, Chirachanakul P, et al. Measuring herpes zoster, zoster-associated pain, post-herpetic neuralgia-associated loss of quality of life, and healthcare utilization and costs in Thailand. Int J Dermatol. 2011;50(4):428–35.
Chayangsu O, Jiamton S, Leeyaphan C, et al. Willingness to pay, quality of life, and knowledge on herpes zoster among Thai patients prior zoster vaccine era. Southeast Asian J Trop Med Public Health. 2016;47(6):1183–91.
White RR, Lenhart G, Singhal PK, et al. Incremental 1-year medical resource utilization and costs for patients with herpes zoster from a set of US health plans. Pharmacoeconomics. 2009;27(9):781–92.
Yawn BP, Itzler RF, Wollan PC, et al. Health care utilization and cost burden of herpes zoster in a community population. Mayo Clin Proc. 2009;84(9):787–94.
Curran D, Callegaro A, Fahrbach K, et al. Meta-regression of herpes zoster incidence worldwide. Infect Dis Ther. 2022;11(1):389–403.
Cohen JI. Clinical practice: herpes zoster. N Engl J Med. 2013;369(3):255–63.
Lee C, Jiang N, Tang H, et al. Potential public health impact of the adjuvanted recombinant zoster vaccine among people aged 50 years and older in Beijing. Hum Vaccin Immunother. 2021;17(10):3735–46.
National Center for Immunization and Respiratory Diseases. Contraindications and precautions: general best practice guidelines for immunization. 2023. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html. Accessed 13 Nov 2023.
Pan CX, Lee MS, Nambudiri VE. Global herpes zoster incidence, burden of disease, and vaccine availability: a narrative review. Ther Adv Vaccines Immunother. 2022;10:25151355221084535.
Watanabe D, Mizukami A, Holl K, et al. The potential public health impact of herpes zoster vaccination of people aged ≥ 50 years in Japan: results of a Markov model analysis. Dermatol Ther (Heidelb). 2018;8(2):269–84.
van Oorschot DAM, Hunjan M, Bracke B, et al. Public health impact model estimating the impact of introducing an adjuvanted recombinant zoster vaccine into the UK universal mass vaccination programme. BMJ Open. 2019;9(5):e025553.
Curran D, Van Oorschot D, Varghese L, et al. Assessment of the potential public health impact of herpes zoster vaccination in Germany. Hum Vaccin Immunother. 2017;13(10):2213–21.
McGirr A, Van Oorschot D, Widenmaier R, et al. Public health impact and cost-effectiveness of non-live adjuvanted recombinant zoster vaccine in Canadian adults. Appl Health Econ Health Policy. 2019;17(5):723–32.
Volpi A, Boccalini S, Dari S, et al. The potential public health impact of herpes zoster vaccination in the 65 years of age cohort in Italy. Hum Vaccin Immunother. 2020;16(2):327–34.
PopulationPyramid.net. Population pyramids of the world from 1950 to 2100. 2022. https://www.populationpyramid.net/. Accessed 19 Aug 2022.
World Health Organization. Life tables by country 2019. https://apps.who.int/gho/data/node.searo.LIFECOUNTRY?lang=en. Accessed 19 Aug 2022.
Yawn BP, Wollan PC, Kurland MJ, et al. Herpes zoster recurrences more frequent than previously reported. Mayo Clin Proc. 2011;86(2):88–93.
Kawai K, Rampakakis E, Tsai TF, et al. Predictors of postherpetic neuralgia in patients with herpes zoster: a pooled analysis of prospective cohort studies from North and Latin America and Asia. Int J Infect Dis. 2015;34:126–31.
Williams WW, Lu PJ, O'Halloran A. Surveillance of vaccination coverage among adult populations—United States, 2015. MMWR Surveill Summ. 2017;66(11):1–28.
LaMori J, Feng X, Pericone CD, et al. Real-world evidence on adherence and completion of the two-dose recombinant zoster vaccine and associated factors in U.S. adults, 2017–2021. Vaccine. 2022;40(15):2266–73.
Boutry C, Hastie A, Diez-Domingo J, et al. The adjuvanted recombinant zoster vaccine confers long-term protection against herpes zoster: interim results of an extension study of the pivotal phase 3 clinical trials ZOE-50 and ZOE-70. Clin Infect Dis. 2022;74(8):1459–67.
Cunningham AL, Lal H, Kovac M, et al. Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N Engl J Med. 2016;375(11):1019–32.
Curran D, Van Oorschot D, Matthews S, et al. Long-term efficacy data for the recombinant zoster vaccine: impact on public health and cost effectiveness in Germany. Hum Vaccin Immunother. 2021;17(12):5296–303.
Lal H, Cunningham AL, Godeaux O, et al. Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N Engl J Med. 2015;372(22):2087–96.
Morrison VA, Johnson GR, Schmader KE, et al. Long-term persistence of zoster vaccine efficacy. Clin Infect Dis. 2015;60(6):900–9.
Schmader KE, Oxman MN, Levin MJ, et al. Persistence of the efficacy of zoster vaccine in the shingles prevention study and the short-term persistence substudy. Clin Infect Dis. 2012;55(10):1320–8.
Department of Statistics Malaysia. Statistics on demand, open data, population and demography. 2022. https://www.dosm.gov.my/v1/index.php?r=column3/accordion&menu_id=amZNeW9vTXRydTFwTXAxSmdDL1J4dz09. Accessed 19 Aug 2022.
Philippines Statistics Authority. OpenSTAT, population and migration. 2022. https://openstat.psa.gov.ph/Database/Population-and-Migration. Accessed 19 Aug 2022.
National Statistics Office Thailand. Number of population by age; number of death by age. 2023. https://stat.bora.dopa.go.th/stat/statnew/statMONTH/statmonth/#/displayData. Accessed 02 Feb 2023.
Han R, Gomez JA, de Veras B, et al. How large could the public health impact of introducing recombinant zoster vaccination for people aged ≥50 years in five Latin American countries be? Hum Vaccin Immunother. 2023;19(1):2164144.
Syed YY. Recombinant zoster vaccine (Shingrix®): a review in herpes zoster. Drugs Aging. 2018;35(12):1031–40.
Paek E, Johnson R. Public awareness and knowledge of herpes zoster: results of a global survey. Gerontology. 2009;56(1):20–31.
Largeron N, Lévy P, Wasem J, et al. Role of vaccination in the sustainability of healthcare systems. J Mark Access Health Policy. 2015;3. https://doi.org/10.3402/jmahp.v3.27043
Hinman AR, McKinlay MA. Immunization equity. Am J Prev Med. 2015;49(6 Suppl 4):S399–405.
Beck E, Biundo E, Devlin N, et al. Capturing the value of vaccination within health technology assessment and health economics: literature review and novel conceptual framework. Vaccine. 2022;40(30):4008–16.
Postma M, Biundo E, Chicoye A, et al. Capturing the value of vaccination within health technology assessment and health economics: country analysis and priority value concepts. Vaccine. 2022;40(30):3999–4007.
Nowak GJ, Shen AK, Schwartz JL. Using campaigns to improve perceptions of the value of adult vaccination in the United States: health communication considerations and insights. Vaccine. 2017;35(42):5543–50.
Medical Writing/Editorial Assistance
The authors thank Costello Medical for editorial assistance and publication coordination, on behalf of GSK, and acknowledge Chloe Foulds, Costello Medical, UK for medical writing and editorial assistance based on authors’ input and direction.
Funding
This study was sponsored by GSK (Study identifier eTrack VEO-000513). Support for third-party writing assistance for this article was funded by GSK in accordance with Good Publication Practice (GPP 2022) guidelines (https://www.ismpp.org/gpp-2022). Funding of the Rapid Service Fee was provided by the study sponsor.
Author information
Authors and Affiliations
Contributions
Substantial contributions to study conception and design: Ru Han, Peter San Martin, Nurilign Ahmed, Adriana Guzman-Holst, Ahmed Mohy, Thatiana Pinto, Bruna de Veras, Jorge A. Gomez, Gyneth Lourdes Bibera, Désirée A. M. van Oorschot; substantial contributions to analysis and interpretation of the data: Ru Han, Peter San Martin, Nurilign Ahmed, Adriana Guzman-Holst, Ahmed Mohy, Thatiana Pinto, Bruna de Veras, Jorge A. Gomez, Gyneth Lourdes Bibera, Désirée A. M. van Oorschot; drafting the article or revising it critically for important intellectual content: Ru Han, Peter San Martin, Nurilign Ahmed, Adriana Guzman-Holst, Ahmed Mohy, Thatiana Pinto, Bruna de Veras, Jorge A. Gomez, Gyneth Lourdes Bibera, Désirée A. M. van Oorschot; final approval of the version of the article to be published: Ru Han, Peter San Martin, Nurilign Ahmed, Adriana Guzman-Holst, Ahmed Mohy, Thatiana Pinto, Bruna de Veras, Jorge A. Gomez, Gyneth Lourdes Bibera, Désirée A. M. van Oorschot. The authors acknowledge Bussakorn Mahakkanukrauh (GSK, Thailand), Minh Nguyen (GSK, Vietnam), Olakunle Oladehin (GSK, Malaysia), Thanabalan Fonseka (GSK, Malaysia), Li Ling Tan (GSK, Malaysia), and Deliana Permatasari (GSK, Indonesia) for contributions to the study. The authors also acknowledge Bella Dragova-Maurin (GSK, Belgium) for publication management.
Corresponding author
Ethics declarations
Conflict of Interest
Ru Han, Peter San Martin, Thatiana Pinto, Bruna de Veras, Gyneth Lourdes Bibera: Employees of GSK; Nurlign Ahmed, Adriana Guzman-Holst, Ahmed Mohy, Jorge A. Gomez, Désirée A. M. van Oorschot: Employees and shareholders of GSK.
Ethical Approval
This model is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentation: Some of the data included in this manuscript were presented in an oral presentation at the Asian Vaccine Conference 2023, held in Cebu, Philippines on November 8–11, 2023.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Han, R., San Martin, P., Ahmed, N. et al. Modelling the Public Health Burden of Herpes Zoster and the Impact of Adjuvanted Recombinant Zoster Vaccine in Five Selected Countries in Southeast Asia. Infect Dis Ther 13, 761–778 (2024). https://doi.org/10.1007/s40121-024-00945-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-024-00945-y