Abstract
Introduction
Limited studies have evaluated the association between Clostridium difficile infection (CDI) and the duration of proton pump inhibitor (PPI) or histamine H2-receptor blocker (H2RA) use and provided a cutoff duration for PPI or H2RA use to mitigate a substantially increased risk of CDI. We aimed to evaluate these associations in hospitalized patients using a nationwide insurance claims database.
Methods
We conducted a nested case–control study to identify cases with a first ever record of CDI in a study cohort undergoing PPI or H2RA therapy from the National Health Insurance Database from 2012 to 2018. Each case was matched with one control by age, sex, and calendar year. We used conditional logistic regression to estimate the sensitivity, specificity, and area under the receiver operating characteristic curve (AUC ROC). Youden’s J statistic was used to identify the optimal cutoff duration in days for PPI or H2RA use.
Results
In the main analysis, the AUC ROC was 0.64 (95% CI 0.63–0.66) and optimal cutoff duration was 15 days for PPI users. The AUC ROC was 0.63 (95% CI 0.62–0.64) and optimal cutoff duration was 16 days for H2RA users. In the sensitivity analyses, the results were similar to those of the main analysis, and the optimal cutoff duration was in the range of 14–15 days.
Conclusions
The optimal cutoff duration for PPI and H2RA use was about 2 weeks. It is necessary to be cautious regarding the risk of CDI in patients taking PPIs or H2RAs for longer than 2 weeks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
PPIs or H2RAs are commonly prescribed to prevent gastrointestinal bleeding or stress ulcers in hospitalized patients. However, the FDA has issued a warning that PPIs may be associated with an increased risk of Clostridium difficile-associated diarrhea. |
Although several studies have suggested an association between the risk of CDI and the use of PPIs or H2RAs, few studies have evaluated the association between the risk of CDI and the duration of PPI or H2RA therapy in a well-defined nationwide population-based cohort study. |
This study was the first to use Youden’s J statistic to estimate the cutoff duration of PPIs or H2RAs use to evaluate an increased risk of CDI. |
What was learned from the study? |
This study showed that the risk of CDI is significantly increased when PPIs or H2RAs are used continuously for more than 14 days. |
On the basis of our findings, we consider physicians need to be aware of the risk of CDI in patients receiving PPI or H2RA treatment for more than 14 days. |
Introduction
Clostridium difficile is one of the common causes of nosocomial infection in hospitals and is associated with high morbidity and mortality [1,2,3]. Clinical signs and symptoms of C. difficile infection (CDI) include severe to life-threatening diarrhea and colitis. Thus, the Centers for Disease Control and Prevention has categorized CDI as an urgent threat to public health, and this infection should be monitored and prevented [4]. Hospital-acquired CDI usually results from alteration of the normal gut flora owing to recent antibiotic exposure in susceptible populations [5, 6]. In addition, older age, hospitalization, high severity of underlying diseases, long length of hospital stay, and use of acid suppressant medications are considered risk factors for CDI [6, 7].
Acid suppressant medications such as proton pump inhibitors (PPIs) or histamine H2-receptor blockers (H2RAs) are commonly prescribed for prophylaxis of gastrointestinal bleeding or stress ulcer prevention in hospitalized patients [8, 9]. Although no randomized controlled trials have examined the safety of PPIs or H2RAs in relation to CDI, it is worthy of note that the US Food and Drug Administration (FDA) has issued a warning suggesting that PPIs may be associated with an increased risk of C. difficile-associated diarrhea [10]. A meta-analysis including 56 studies and a large number of patients indicated a significantly increased risk of CDI in PPI users as compared with non-PPI users (OR 1.99, 95% CI 1.73–2.30) [11]. An observational cohort study included outpatient-based patients and evaluated the risk of CDI among patients receiving PPI or H2RA therapy, and showed a significantly increased risk of CDI among the patients taking PPIs or H2RAs as compared with the matched controls [12].
Although several studies have indicated an association between the risk of CDI and use of PPIs or H2RAs, not all patients develop CDI after receiving PPI or H2RA therapy. Thus, we considered that the duration of PPI or H2RA therapy could be an important factor affecting CDI development. However, limited studies have examined the association between risk of CDI and duration of PPI or H2RA therapy and indicated the threshold for the duration of PPI or H2RA use at which there is a significantly increased risk of CDI. Thus, the objective of this study was to evaluate the association between risk of CDI and duration of PPI or H2RA therapy and estimate the optimal cutoff duration for PPI or H2RA use using a nationwide population-based database.
Materials and Methods
Data Sources
The National Health Insurance Database (NHID) was used in this study. The NHID and Cause of Death database were provided and authorized access by the Health and Welfare Data Science Center, Ministry of Health and Welfare, Taiwan. These databases provide person-level information through personal identification number linkage [13]. The NHID is populated from a universal single-payer healthcare program that covers 99% of Taiwan’s population. It is composed of a registry of beneficiaries, ambulatory care claims, inpatient claims, and prescription dispensing claims of pharmacies. Each claim contains a diagnosis code according to the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM, up to December 31, 2015) and Tenth Edition (ICD-10-CM, after January 1, 2016). In addition, medications, laboratory tests, and surgeries are recorded with National Health Insurance codes. For details of the NHID, refer to Hsieh et al. [13].
Design, Setting, and Study Cohort
We conducted a nested case–control study [14] to investigate the association between CDI and duration of PPI or H2RA use in hospitalized patients. The study cohort was identified as patients with a first admission who began to use PPIs or H2RAs in the NHID from 2012 to 2018. Patients were excluded if they were aged under 20 years, had a history of PPI or H2RA prescription during a 180-day period prior to the admission date, had a diagnosis of peptic ulcer (ICD-10-CM codes K25–K28), had acquired immunodeficiency syndrome (ICD-10-CM codes B20–B22, B24), or were pregnant (O00-O99, O9A). A length of stay (LOS) longer than 90 days was considered excessive, and as these patients could have a greater illness severity or other critical issues they were excluded from our study cohort (Fig. 1).
Follow-up and Covariates
The duration of follow-up was based on PPI or H2RA exposure days in an “as treated” way. The exposure days to PPIs or H2RAs began on the date of the first prescription filling and was censored at the date of discontinuation, switching, death, occurrence of CDI, discharge from hospital, or the end of the study period after the first prescription, whichever came first. Discontinuation was defined as patients who stopped receiving PPIs or H2RAs within 7 days after the date of the last prescription. Baseline variables were constructed from the NHID during the 180-day pre-admission period. Comorbidities and co-medications were assessed according to the Charlson comorbidity index (CCI) [15], and CCI scores were calculated in this study. Information regarding the antibiotic use in our study, it was measured as a co-medication during the 2-week pre-admission period and was considered as a baseline variable in our analysis. The date of incident CDI was defined as the index date. Details of the baseline variables are presented in Table 1 and in Supplemental Table 1 in the supplementary data.
Cases and Controls
According to the nested case–control study, the source population was our study cohort of hospitalized patients who were prescribed a PPI or H2RA for treatment. We then followed these patients, and if a patient had CDI during the PPI or H2RA exposure period, it was considered a case. Patients with CDI in this study were considered to be those who received metronidazole, fidaxomicin, or vancomycin orally for treatment for at least 7 days [16]. If a patient becomes a case, we would randomly select a patient who did not have CDI at that time from the source population and matched by age, sex, and calendar year of entry into the cohort according to incidence density sampling as a control until the end of follow-up during the PPI or H2RA exposure period. The final case and control groups were matched to a case on a 1:1 basis for age, sex, and calendar year of cohort entry. The nested case–control study design in this study is shown in Supplemental Fig. 1.
Sensitivity Analysis
To confirm that our results were not biased by misclassification of CDI, we performed two sensitivity analyses. First, we restricted our study cohort to between 2017 and 2018, and cases were defined as patients with records of CDI testing or diagnosis of CDI (ICD-10-CM codes 8.45, A04.7) in addition to metronidazole, fidaxomicin or vancomycin oral treatment for at least 7 days. The C. difficile GDH Ag rapid test and C. difficile toxin A/B rapid test have been reimbursed by the National Health Insurance program since 2017. We therefore used a strict definition to identify patients with CDI and performed the analysis again. Second, in order to avoid community-acquired infection, we excluded patients who had CDI within 3 days between admission date and index date and performed the analysis again.
Statistical Analysis
Descriptive statistics were used to characterize case and control characteristics. Continuous variables were described as means with standard deviations (SD), and categorical variables by numbers and proportions. The standardized mean difference (SMD) was used to characterize the differences in baseline characteristics between the case and control groups. We used univariable conditional logistic regressions to estimate the sensitivity, specificity, and area under the receiver operating characteristic curve (AUC ROC) for CDI associated with duration of PPI or H2RA use, respectively. Youden’s J statistic was used to identify the optimal cutoff duration for the length of PPI or H2RA use. According to the results of Youden’s J statistic, we stratified the duration of PPI or H2RA use into shorter cutoff duration and longer cutoff duration groups, and the adjusted odds ratios (aORs) were estimated to compare the risk of CDI in patients using PPIs and H2RAs for shorter or longer cutoff durations by multivariable conditional logistic regression. An example of estimating odds ratios is shown in Supplemental Table 2.
Results
The 6933 cases were matched to 6933 controls. The mean age was approximately 65 years in the cases and controls. The cases were more likely to use PPIs or H2RAs for a longer duration (mean 19.72 days; SD 15.99 days) as compared with the controls (mean 12.34 days; SD 10.09 days). In addition, the cases had the propensity to have a higher proportion of baseline antibiotic use (28.8%) as compared with the controls (11.4%). The details of baseline characteristics are shown in Table 1.
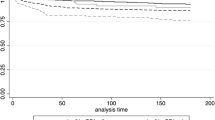
Table 2 lists the optimal cutoff values, AUC ROC, sensitivity, and specificity of the duration of PPI and H2RA use in discriminating the occurrence of CDI. In PPI users, the AUC ROC was 0.64 (95% CI 0.63–0.66), sensitivity was 0.57 (95% CI 0.56–0.58), and specificity was 0.73 (95% CI 0.72–0.74). The optimal cutoff duration was 15 days. In H2RA users, the AUC ROC was 0.63 (95% CI 0.62–0.64), sensitivity was 0.59 (95% CI 0.58–0.60), and specificity was 0.70 (95% CI 0.69–0.71). The optimal cutoff duration was 16 days. For sensitivity analyses, the optimal cutoff duration was in the range of 14–15 days for PPIs and H2RAs. Taking these results regarding the optimal cutoff duration together, it was indicated that around 14 days could be the optimal cutoff duration for PPI and H2RA use. Therefore, we stratified the duration of PPI and H2RA use into two groups, shorter than 14 days (≤ 14 days) and longer than 14 days (> 14 days), and compared the risk of CDI with PPI and H2RA use for shorter or longer than 14 days.
Table 3 shows an increased risk of CDI in PPI and H2RA users. Compared with H2RAs, PPIs led to an increased risk of CDI (aOR 1.31, 95% CI 1.22–1.4) after adjustment for comorbidities and co-medications. Patients who use PPIs or H2RAs for more than 14 days could be at increased risk of CDI (aOR 4.27, 95% CI 3.95–4.6) as compared with patients who take the medications for fewer than 14 days. Compared with patients who use H2RAs for fewer than 14 days, patients who use H2RAs for more than 14 days could have an increased risk of CDI (aOR 4.19, 95% CI 3.77–4.65), and the same applies to patients who use PPIs for more than 14 days (aOR 5.38, 95% CI 4.84–5.99). The sensitivity analyses showed similar results to the main analysis.
Discussion
In this study, the results showed that PPIs increased the risk of CDI as compared with H2RAs in a hospital cohort, which was consistent with previous studies [12, 17]. In addition, we further examined the association between CDI occurrence and duration of PPI and H2RA use. A longer duration of PPI or H2RA use significantly increased the risk of CDI, and the threshold for a substantial increase in the risk of CDI was about 14 days for both medications. Therefore, patients who use PPIs or H2RAs for longer than 2 weeks could be at increased risk of CDI as compared with patients who use these medications for less than 2 weeks, and the greatest risk is in patients who undergo PPI treatment for longer than 2 weeks. In baseline characteristics, we found that the case group had a higher proportion of baseline antibiotic use compared with controls. The possible explanation is that more people in the case group in our study had diabetes compared with the control group, which may lead to a higher risk of infection. Previous studies [18, 19] have suggested that hyperglycemia and poor glycemic control may induce immune dysfunction, affecting chronic inflammatory processes and leading to diabetes mellitus-associated susceptibility to infection. This could explain why the case group (hospitalized patients with CDI) had more records of antibiotic use in the pre-admission period. To reduce the effect of confounding due to baseline antibiotic use, we use conditional logistic regression to adjust for the confounders to reduce bias.
Although no randomized controlled trial has evaluated the safety of PPIs or H2RAs, several studies have shown an association between the risk of CDI and PPI or H2RA use. A systematic review included 12 observational studies and found an increased risk of the need to take antisecretory agents in patients with CDI. Furthermore, there was a greater risk for PPIs (OR 1.96, 95% CI 1.28–3.00) as compared with H2RAs (OR 1.40, 95% CI 0.85–2.29) [20]. Another systematic review and meta-analysis included 12 observational studies and reported the hospital-acquired CDI occurrence following H2RA and PPI use for the prevention and treatment of stress gastric ulcers. Similar to a previous study, it was found that PPIs led to a greater CDI risk than H2RAs (OR 1.39, 95% CI 1.15–1.67) [17].
Gastric acid is one of the protective mechanisms against enteral infection, including CDI. Gastric acid suppression may affect indigenous microbiota, causing less diversity among gut bacteria and an increased risk of infections such as C. difficile [21]. In addition, C. difficile spores are unable to sporulate at a low gastric pH; a high gastric pH is better for the sporulation and germination of vegetative forms of the bacterium [22]. These in vitro studies may explain the high occurrence of CDI in patients receiving PPIs or H2RAs.
Compared with H2RAs, PPIs have shown a more potent gastric acid suppression ability and are more effective as a treatment for peptic ulcer disease (PUD), severe gastroesophageal reflux disease (GERD), Zollinger-Ellison syndrome, and upper gastrointestinal bleeding [23]. Thus, it may be reasonable that PPIs are more likely to increase the risk of CDI as compared with H2RAs according to the effectiveness of gastric acid suppression. A large cohort study indicated a positive association between the risk of CDI and the intensity of gastric acid suppression. The highest risk was in patients receiving frequent PPI therapy, followed by those receiving daily PPIs, H2RAs, and those not receiving gastric acid suppressive therapy [24]. The FDA and Canadian Agency for Drugs and Technologies in Health (CADTH) issued warnings stating that the use of PPIs may be associated with an increased risk of CDI [10, 25] and recommended the lowest dose and shortest duration be employed in patients undergoing treatment with PPIs. However, a suggested duration of PPI or H2RA use was lacking, and there are no recommendations in the current guidelines.
Despite the duration of PPI and H2RA use being an important risk factor for CDI [6, 7], it has varied in previous studies. A meta-analysis included 60 studies and evaluated the association between PPI use and recurrent CDI. Only five studies revealed information regarding the duration of PPI use, which ranged from 3 days to 1 month [26]. To our knowledge, the current study was the first to evaluate the optimal cutoff duration for PPI and H2RA therapy and provide information regarding the threshold for a substantial increase in the risk of CDI using a real-world nationwide database. The results indicated that the optimal cutoff duration for PPI and H2RA use was 14 days. Our findings provided real-world evidence regarding PPI and H2RA use for prophylaxis in hospitalized patients.
This study has strengths related to the healthcare and health insurance systems of Taiwan. The Taiwanese National Health Insurance Database is derived from a universal and mandatory health insurance program in Taiwan that covers 99% of the entire population. Therefore, it allows researchers to construct a nationwide cohort of patients with negligible loss of follow-up. The use of claims data for pharmacoepidemiological study has inherent limitations. First, we considered patients who received metronidazole, fidaxomicin, or vancomycin oral treatment for at least 7 days as the CDI cohort, which might have resulted in misclassification between cases and controls. In order to reduce bias, we performed sensitivity analyses to identify cases using a strict definition, including records of CDI rapid testing, diagnosis of CDI, and exclusion of patients suspected of community-acquired infection. Similar results were obtained to those of the main analysis. The effects of misclassification were therefore minimized. Second, other confounding factors, such as disease severity, health behaviors, and strains, were not available in the claims data, which may have led to slight overestimation in our results.
Conclusion
In this study, we found that a longer duration of use of PPIs and H2RAs could increase the risk of CDI in hospitalized patients. In addition, the results showed the optimal cutoff duration for PPI and H2RA use to be 14 days. Therefore, we suggest that physicians need to pay attention to the risk of CDI in patients receiving PPI or H2RA treatment for more than 14 days.
Data Availability
The data supporting our observational study were from National Health Insurance Database. Regarding Taiwanese “Personal Information Protection Act” and governmental regulation, the data with individual information cannot be released. We only can provide aggregated data without individual information for materials.
References
Ramaswamy R, Grover H, Corpuz M, Daniels P, Pikhumoni C. Prognostic criteria in Clostridium difficile colitis. Am J Gastroenterol. 1996;91(3):460–4.
Kyne L, Hamel MB, Polavaram R, Kelly CP. Health care costs and mortality associated with nosocomial diarrhea due to Clostridium difficile. Clin Infect Dis. 2002;34(3):346–53.
Kenneally C, Rosini JM, Skrupky LP, et al. Analysis of 30-day mortality for Clostridium difficile-associated disease in the icu setting. Chest. 2007;132(2):418–24.
CDC. 2019 AR threats report. https://www.cdc.gov/drugresistance/biggest-threats.html#cdiff. https://doi.org/10.15620/cdc:82532. Accessed 5 Jan 2024
Shrestha A, Kalapurayil M, Bailey J, Deol H, Singh R, Surani S. Examining risk of C difficile infection with use of proton pump inhibitor vs H2 receptor antagonist. Chest. 2018;154(4):374A.
Czepiel J, Dróżdż M, Pituch H, et al. Clostridium difficile infection: review. Eur J Clin Microbiol Infect Dis. 2019;38(7):1211–21.
Bignardi GE. Risk factors for Clostridium difficile infection. J Hosp Infect. 1998;40(1):1–15.
Tariq R, Singh S, Gupta A, Pardi DS, Khanna S. Association of gastric acid suppression with recurrent Clostridium difficile infection: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(6):784–91.
Al-Aly Z, Maddukuri G, Xie Y. Proton pump inhibitors and the kidney: implications of current evidence for clinical practice and when and how to deprescribe. Am J Kidney Dis. 2020;75(4):497–507.
FDA drug safety communication: Clostridium difficile associated diarrhea can be associated with stomach acid drugs known as proton pump inhibitors (PPIs). https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-clostridium-difficile-associated-diarrhea-can-be-associated-stomach. Accessed 5 Jan 2024
Trifan A, Stanciu C, Girleanu I, et al. Proton pump inhibitors therapy and risk of Clostridium difficile infection: systematic review and meta-analysis. World J Gastroenterol. 2017;23(35):6500–15.
Seo SI, You SC, Park CH, et al. Comparative risk of Clostridium difficile infection between proton pump inhibitors and histamine-2 receptor antagonists: a 15-year hospital cohort study using a common data model. J Gastroenterol Hepatol. 2020;35(8):1325–30.
Hsieh CY, Su CC, Shao SC, et al. Taiwan’s national health insurance research database: past and future. Clin Epidemiol. 2019;11:349–58.
Ernster VL. Nested case-control studies. Prev Med. 1994;23(5):587–90.
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–94.
Kimura T, Stanhope S, Sugitani T. Clostridioides (Clostridium) difficile infection in Japanese hospitals 2008–2017: a real-world nationwide analysis of treatment pattern, incidence and testing density. J Infect Chemother. 2020;26(5):438–43.
Azab M, Doo L, Doo DH, et al. Comparison of the hospital-acquired Clostridium difficile infection risk of using proton pump inhibitors versus histamine-2 receptor antagonists for prophylaxis and treatment of stress ulcers: a systematic review and meta-analysis. Gut liver. 2017;11(6):781–8.
Kim EJ, Ha KH, Kim DJ, Choi YH. Diabetes and the risk of infection: a national cohort study. Diabetes Metab J. 2019;43(6):804–14.
Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr Diabetes Rev. 2020;16(5):442–9.
Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol. 2007;102(9):2047–56.
Romero R, Hassan SS, Gajer P, et al. The composition and stability of the vaginal microbiota of normal pregnant women is different from that of non-pregnant women. Microbiome. 2014;2(1):4.
Tawam D, Baladi M, Jungsuwadee P, Earl G, Han J. The positive association between proton pump inhibitors and Clostridium difficile infection. Innov Pharm. 2021;12(1):10.24926
Herszényi L, Bakucz T, Barabás L, Tulassay Z. Pharmacological approach to gastric acid suppression: past, present, and future. Dig Dis. 2020;38(2):104–11.
Howell MD, Novack V, Grgurich P, et al. Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Arch Intern Med. 2010;170(9):784–90.
Summary safety review - proton pump inhibitors - assessing the potential risk of Clostridium difficile infection. https://www.canada.ca/en/health-canada/services/drugs-health-products/medeffect-canada/safety-reviews/summary-safety-review-proton-pump-inhibitors-assessing-potential-risk-clostridium-infection.html. Accessed 5 Jan 2024
D’Silva KM, Mehta R, Mitchell M, et al. Proton pump inhibitor use and risk for recurrent clostridioides difficile infection: a systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(5):697–703.
Acknowledgements
This research was supported by National Cheng Kung University Hospital, Tainan, Taiwan. We are grateful to the administrative and technical services provided by the Health Data Science Center and Bioinformatics Group of the Smart Healthcare Solution in National Cheng Kung University Hospital.
Funding
This study and the journal’s Rapid Service Fee was supported by a grant from the National Cheng Kung University Hospital, Tainan, Taiwan [grant number NCKUH-10905021 and NCKUH-11007021].
Author information
Authors and Affiliations
Contributions
Study concept and design: Chien-Huei Huang, Yung-Hsin Tseng, Wen-Shan Tsai and Chien-Chou Su. Acquisition of data: Yea-Huei Kao Yang. Analysis and interpretation of data: Yu-Ching Chang, Yi-Hsuan Liu, Chien-Chou Su and Ching-Lan Cheng. Drafting of the manuscript: Chien-Huei Huang, Yung-Hsin Tseng, Wen-Shan Tsai and Chien-Chou Su. Critical revision of the manuscript for important intellectual content: Chien-Chou Su and Ching-Lan Cheng.
Corresponding authors
Ethics declarations
Disclosures
Chien-Huei Huang, Yung-Hsin Tseng, Wen-Shan Tsai and Chien-Chou Su, Ching-Lan Cheng, Yea-Huei Kao Yang, Yu-Ching Chang, and Yi-Hsuan Liu declare there are no conflicts of interest with respect to this research study and paper.
Ethical Approval and Informed Consent
The research protocol was approved by the Institutional Review Board of National Cheng Kung University Hospital (A-EX-109-039). This study employed de-identified secondary data from National Insurance Database (NHID) and thus was exempted from informed consent.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Huang, CH., Tseng, YH., Tsai, WS. et al. Association Between Risk of Clostridium difficile Infection and Duration of Proton Pump Inhibitor or H2-Receptor Antagonist Use in Hospitalized Patients. Infect Dis Ther 13, 373–383 (2024). https://doi.org/10.1007/s40121-024-00922-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-024-00922-5